The Role of Autologous Platelet Concentrates as a Local Antibiotic Delivery System: A Systematic Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Literature Search
2.2. Data Extraction
3. Results
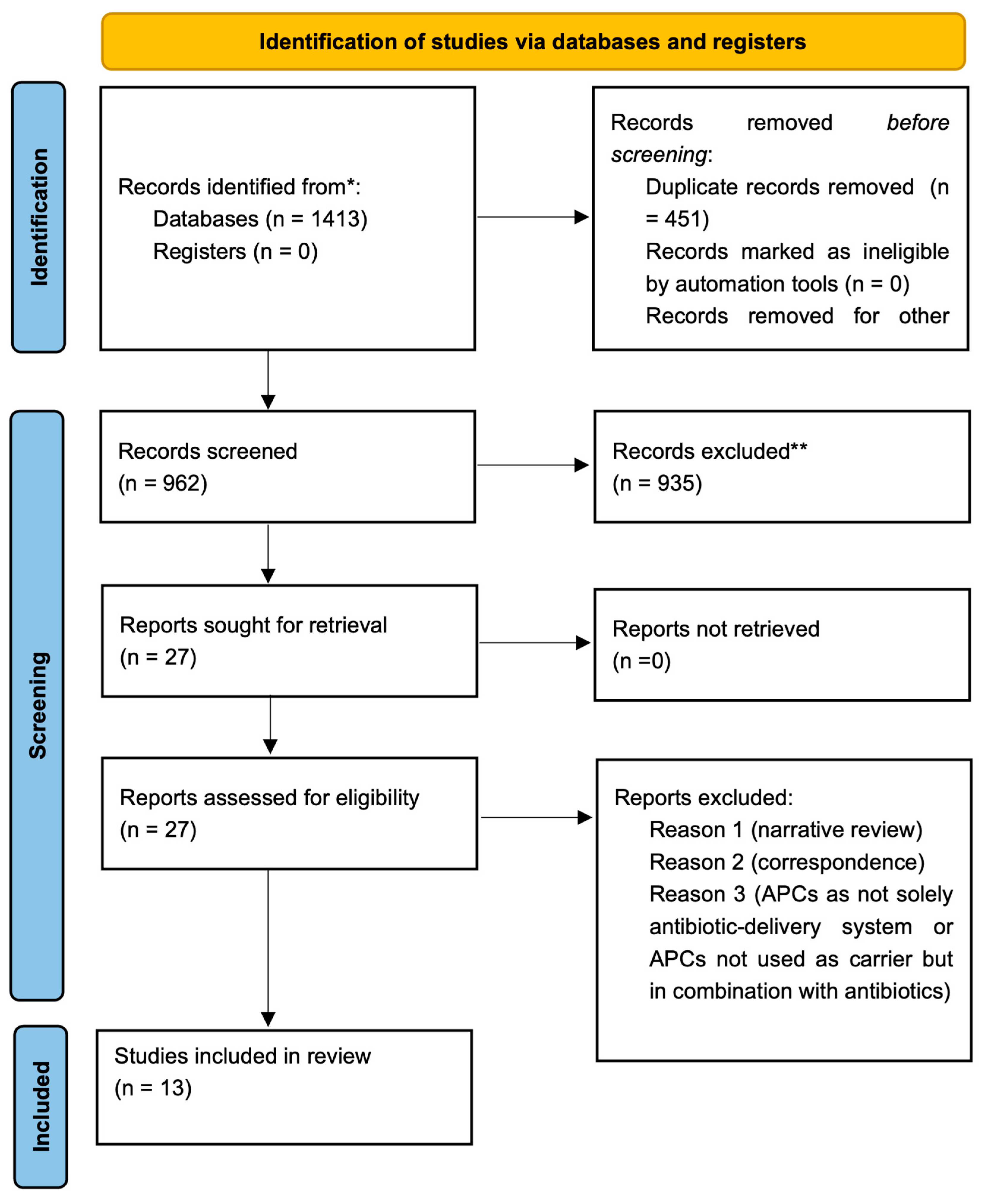
3.1. Selection of Studies
3.2. In Vitro Studies
3.2.1. Antibiotic Loading Capacity of APC
3.2.2. Release Kinetics of Antibiotic
3.2.3. Antibacterial Effects of Loaded APCs
3.2.4. Mutual Interaction: Antibiotics’ Impact on APC Structures and Vice Versa
3.3. In Vivo Studies
4. Discussion
4.1. Clinical Relevance
4.2. Limits, Strengths, and Future Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Ajulo, S.; Awosile, B. Global antimicrobial resistance and use surveillance system (GLASS 2022): Investigating the relationship between antimicrobial resistance and antimicrobial consumption data across the participating countries. PLoS ONE 2024, 19, e0297921. [Google Scholar] [CrossRef] [PubMed]
- Murugaiyan, J.; Kumar, P.A.; Rao, G.S.; Iskeqandar, K.; Hawser, S.; Hays, J.P.; Mohsen, Y.; Adukkadukkam, S.; Awuah, W.A.; Jose, R.A.M.; et al. Progress in Alternative Strategies to Combat Antimicrobial Resistance: Focus on Antibiotics. Antibiotics 2022, 11, 200. [Google Scholar] [CrossRef]
- Signorini, L.; Marenzi, G.; Facente, A.; Marrelli, B.; Marano, R.M.; Valletta, A.; Pacifici, L.; Gasparro, R.; Sammartino, G.; Severino, M. Critical Overview on Pure Chitosan-based Scaffolds for Bone Tissue Engineering: Clinical insights in Dentistry. Int. J. Med. Sci. 2023, 20, 1527–1534. [Google Scholar] [CrossRef] [PubMed]
- Ahangar, P.; Li, J.; Nkindi, L.S.; Mohammadrezaee, Z.; Cooke, M.E.; Martineau, P.A.; Weber, M.H.; Saade, E.; Nateghi, N.; Rosenzweig, D.H. A Nanoporous 3D-Printed Scaffold for Local Antibiotic Delivery. Micromachines 2023, 15, 83. [Google Scholar] [CrossRef] [PubMed]
- Laubach, J.M.; Sani, R.K. Thermophilic Exopolysaccharide Films: A Potential Device for Local Antibiotic Delivery. Pharmaceutics 2023, 15, 557. [Google Scholar] [CrossRef] [PubMed]
- Nimal, T.R.; Baranwal, G.; Bavya, M.C.; Biswas, R.; Jayakumar, R. Anti-staphylococcal Activity of Injectable Nano Tigecycline/Chitosan-PRP Composite Hydrogel Using Drosophila melanogaster Model for Infectious Wounds. ACS Appl. Mater. Interfaces 2016, 8, 22074–22083. [Google Scholar] [CrossRef]
- Wei, S.; Xu, P.; Yao, Z.; Cui, X.; Lei, X.; Li, L.; Dong, Y.; Zhu, W.; Guo, R.; Cheng, B. A composite hydrogel with co-delivery of antimicrobial peptides and platelet-rich plasma to enhance healing of infected wounds in diabetes. Acta Biomater. 2021, 124, 205–218. [Google Scholar] [CrossRef]
- Wassif, R.K.; Elkayal, M.; Shamma, R.N.; Elkheshen, S.A. Recent advances in the local antibiotics delivery systems for management of osteomyelitis. Drug Deliv. 2021, 28, 2392–2414. [Google Scholar] [CrossRef]
- D’Esposito, V.; Lecce, M.; Marenzi, G.; Cabaro, S.; Ambrosio, M.R.; Sammartino, G.; Misso, S.; Migliaccio, T.; Liguoro, P.; Oriente, F.; et al. Platelet-rich plasma counteracts detrimental effect of high-glucose concentrations on mesenchymal stem cells from Bichat fat pad. J. Tissue Eng. Regen. Med. 2020, 14, 701–713. [Google Scholar] [CrossRef]
- Gasparro, R.; Qorri, E.; Valletta, A.; Masucci, M.; Sammartino, P.; Amato, A.; Marenzi, G. Non-Transfusional Hemocomponents: From Biology to the Clinic—A Literature Review. Bioengineering 2018, 5, 27. [Google Scholar] [CrossRef]
- Gasparro, R.; Sammartino, G.; Mariniello, M.; di Lauro, A.E.; Spagnuolo, G.; Marenzi, G. Treatment of periodontal pockets at the distal aspect of mandibular second molar after surgical removal of impacted third molar and application of L-PRF: A split-mouth randomized clinical trial. Quintessence Int. 2020, 51, 204–211. [Google Scholar] [PubMed]
- Intravia, J.; Allen, D.A.; Durant, T.J.; McCarthy, M.B.; Russell, R.; Beitzel, K.; Cote, M.P.; Dias, F.; Mazzocca, A.D. In vitro evaluation of the anti-bacterial effect of two preparations of platelet rich plasma compared with cefazolin and whole blood. Muscles Ligaments Tendons J. 2014, 4, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Ozcan, M.; Kabaklı, S.C.; Alkaya, B.; Isler, S.C.; Turer, O.U.; Oksuz, H.; Haytac, M.C. The impact of local and systemic penicillin on antimicrobial properties and growth factor release in platelet-rich fibrin: In vitro study. Clin. Oral Investig. 2023, 28, 61. [Google Scholar] [CrossRef] [PubMed]
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32. [Google Scholar] [CrossRef]
- Davis, K.; Drey, N.; Gould, D. What are scoping studies? A review of the nursing literature. Int. J. Nurs. Stud. 2009, 46, 1386–1400. [Google Scholar] [CrossRef]
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid. Based Healthc. 2015, 13, 141–146. [Google Scholar] [CrossRef]
- Bennardo, F.; Gallelli, L.; Palleria, C.; Colosimo, M.; Fortunato, L.; De Sarro, G.; Giudice, A. Can platelet-rich fibrin act as a natural carrier for antibiotics delivery? A proof-of-concept study for oral surgical procedures. BMC Oral Health 2023, 23, 134. [Google Scholar] [CrossRef]
- Dubnika, A.; Egle, K.; Skrinda-Melne, M.; Skadins, I.; Rajadas, J.; Salma, I. Development of Vancomycin Delivery Systems Based on Autologous 3D Platelet-Rich Fibrin Matrices for Bone Tissue Engineering. Biomedicines 2021, 9, 814. [Google Scholar] [CrossRef]
- Egle, K.; Skadins, I.; Grava, A.; Micko, L.; Dubniks, V.; Salma, I.; Dubnika, A. Injectable Platelet-Rich Fibrin as a Drug Carrier Increases the Antibacterial Susceptibility of Antibiotic-Clindamycin Phosphate. Int. J. Mol. Sci. 2022, 23, 7407. [Google Scholar] [CrossRef]
- Ercan, E.; Suner, S.S.; Silan, C.; Yilmaz, S.; Siddikoglu, D.; Sahiner, N.; Tunali, M. Titanium platelet-rich fibrin (T-PRF) as high-capacity doxycycline delivery system. Clin. Oral Investig. 2022, 26, 5429–5438. [Google Scholar] [CrossRef]
- Kadam, S.; Kulloli, A.; Shetty, K.S.; Martande, S.S.; Poulose, M.; Nair, G.; Guruprasad, M.; Mehta, V. Comparative Evaluation of Efficacy of Antibiotics incorporated Platelet Rich Fibrin Versus Platelet Rich Fibrin alone in the Treatment of Intrabony Defects. J. Popul. Ther. Clin. Pharmacol. 2023, 30, 267–274. [Google Scholar]
- Knafl, D.; Thalhammer, F.; Vossen, M.G. In-vitro release pharmacokinetics of amikacin, teicoplanin and polyhexanide in a platelet rich fibrin-layer (PRF)-a laboratory evaluation of a modern, autologous wound treatment. PLoS ONE 2017, 12, e0181090. [Google Scholar] [CrossRef] [PubMed]
- Polak, D.; Clemer-Shamai, N.; Shapira, L. Incorporating antibiotics into platelet-rich fibrin: A novel antibiotics slow-release biological device. J. Clin. Periodontol. 2019, 46, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Rafiee, A.; Memarpour, M.; Najibi, Y.; Khalvati, B.; Kianpour, S.; Morowvat, M.H. Antimicrobial Efficacy of a Novel Antibiotic-Eluting Injectable Platelet-Rich Fibrin Scaffold against a Dual-Species Biofilm in an Infected Immature Root Canal Model. Biomed. Res. Int. 2020, 2020, 6623830. [Google Scholar] [CrossRef]
- Straub, A.; Vollmer, A.; Lâm, T.T.; Brands, R.C.; Stapf, M.; Scherf-Clavel, O.; Bittrich, M.; Fuchs, A.; Kübler, A.C.; Hartmann, S. Evaluation of advanced platelet-rich fibrin (PRF) as a bio-carrier for ampicillin/sulbactam. Clin. Oral Investig. 2022, 26, 7033–7044. [Google Scholar] [CrossRef]
- Straub, A.; Utz, C.; Stapf, M.; Vollmer, A.; Kasper, S.; Kübler, A.C.; Brands, R.C.; Hartmann, S.; Lâm, T.T. Investigation of three common centrifugation protocols for platelet-rich fibrin (PRF) as a bio-carrier for ampicillin/sulbactam: A prospective trial. Clin. Oral Investig. 2023, 27, 5991–5998. [Google Scholar] [CrossRef]
- Straub, A.; Utz, C.; Stapf, M.; Vollmer, A.; Breitenbuecher, N.; Kübler, A.C.; Brands, R.C.; Hartmann, S.; Lâm, T.T. Impact of aminopenicillin administration routes on antimicrobial effects of platelet-rich fibrin: An in-vitro investigation. J. Stomatol. Oral Maxillofac. Surg. 2023, 125, 101725. [Google Scholar] [CrossRef]
- Straub, A.; Stapf, M.; Utz, C.; Vollmer, A.; Flesch, J.; Kübler, A.; Scherf-Clavel, O.; Lâm, T.T.; Hartmann, S. Antimicrobial effects of clindamycin-loaded platelet-rich fibrin (PRF). Clin. Oral. Investig. 2024, 28, 144. [Google Scholar] [CrossRef]
- Wang, S.; Li, Y.; Li, S.; Yang, J.; Tang, R.; Li, X.; Li, L.; Fei, J. Platelet-rich plasma loaded with antibiotics as an affiliated treatment for infected bone defect by combining wound healing property and antibacterial activity. Platelets 2021, 32, 479–491. [Google Scholar] [CrossRef]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Khalil, H.; Larsen, P.; Marnie, C.; Pollock, D.; Tricco, A.C.; Munn, Z. Best practice guidance and reporting items for the development of scoping review protocols. JBI Evid. Synth. 2022, 20, 953–968. [Google Scholar] [CrossRef]
- Campana, M.D.; Aliberti, A.; Acerra, A.; Sammartino, P.; Dolce, P.; Sammartino, G.; Gasparro, R. The Effectiveness and Safety of Autologous Platelet Concentrates as Hemostatic Agents after Tooth Extraction in Patients on Anticoagulant Therapy: A Systematic Review of Randomized, Controlled Trials. J. Clin. Med. 2023, 12, 5342. [Google Scholar] [CrossRef] [PubMed]
- di Lauro, A.E.; Valletta, A.; Aliberti, A.; Cangiano, M.; Dolce, P.; Sammartino, G.; Gasparro, R. The Effectiveness of Autologous Platelet Concentrates in the Clinical and Radiographic Healing after Endodontic Surgery: A Systematic Review. Materials 2023, 16, 7187. [Google Scholar] [CrossRef]
- Miron, R.J.; Zhang, Y. Autologous liquid platelet rich fibrin: A novel drug delivery system. Acta Biomater. 2018, 75, 35–51. [Google Scholar] [CrossRef]
- Cl, K.; Jeyaraman, M.; Jeyaraman, N.; Ramasubramanian, S.; Khanna, M.; Yadav, S. Antimicrobial Effects of Platelet-Rich Plasma and Platelet-Rich Fibrin: A Scoping Review. Cureus 2023, 15, e51360. [Google Scholar] [CrossRef]
- Blair, P.; Flaumenhaft, R. Platelet alpha-granules: Basic biology and clinical correlates. Blood Rev. 2009, 23, 177–189. [Google Scholar] [CrossRef] [PubMed]
- Dohan Ehrenfest, D.M.; Bielecki, T.; Jimbo, R.; Barbé, G.; Del Corso, M.; Inchingolo, F.; Sammartino, G. Do the fibrin architecture and leukocyte content influence the growth factor release of platelet concentrates? An evidence-based answer comparing a pure platelet-rich plasma (P-PRP) gel and a leukocyte- and platelet-rich fibrin (L-PRF). Curr. Pharm. Biotechnol. 2012, 13, 1145–1152. [Google Scholar] [CrossRef]
- Fabbro, M.D.; Bortolin, M.; Taschieri, S.; Ceci, C.; Weinstein, R.L. Antimicrobial properties of platelet-rich preparations. A systematic review of the current pre-clinical evidence. Platelets 2016, 27, 276–285. [Google Scholar] [CrossRef]
- Radek, K.; Gallo, R. Antimicrobial peptides: Natural effectors of the innate immune system. Semin. Immunopathol. 2007, 29, 27–43. [Google Scholar] [CrossRef] [PubMed]
- Aizawa, H.; Kawabata, H.; Sato, A.; Masuki, H.; Watanabe, T.; Tsujino, T.; Isobe, K.; Nakamura, M.; Nakata, K.; Kawase, T. A Comparative Study of The Effects of Anticoagulants on Pure Platelet-Rich Plasma Quality and Potency. Biomedicines 2020, 8, 42. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Chanapiwat, P.; Paiboonvong, T.; Rattanaumpawan, P.; Montakantikul, P. Comparison of the mathematical equation and trapezoidal approach for 24 h area under the plasma concentration-time curve calculation in patients who received intravenous vancomycin in an acute care setting. Pharmacol. Res. Perspect. 2023, 11, e01046. [Google Scholar] [CrossRef]
- Pelligand, L.; Møller Sørensen, T.; Cagnardi, P.; Toutain, P.L.; Allerton, F. Population pharmacokinetic meta-analysis of five beta-lactams antibiotics to support dosing regimens in dogs for surgical antimicrobial prophylaxis. Vet. J. 2024, 305, 106136. [Google Scholar] [CrossRef]
- Mangoni, A.A.; Jackson, S.H. Age-related changes in pharmacokinetics and pharmacodynamics: Basic principles and practical applications. Br. J. Clin. Pharmacol. 2004, 57, 6–14. [Google Scholar] [CrossRef] [PubMed]
- Junkert, A.M.; Lazo, R.E.L.; Deffert, F.; Carneiro, J.; Borba, H.H.L.; de Campos, M.L.; Pontarolo, R. Pharmacokinetics of oral ciprofloxacin in adult patients: A scoping review. Br. J. Clin. Pharmacol. 2024, 90, 528–547. [Google Scholar] [CrossRef] [PubMed]
- Gao, W.; Chen, Y.; Zhang, Y.; Zhang, Q.; Zhang, L. Nanoparticle-based local antimicrobial drug delivery. Adv. Drug Deliv. Rev. 2018, 127, 46–57. [Google Scholar] [CrossRef]
- ter Boo, G.J.; Grijpma, D.W.; Moriarty, T.F.; Richards, R.G.; Eglin, D. Antimicrobial delivery systems for local infection prophylaxis in orthopedic- and trauma surgery. Biomaterials 2015, 52, 113–125. [Google Scholar] [CrossRef]
- Nazli, A.; He, D.L.; Liao, D.; Khan, M.Z.I.; Huang, C.; He, Y. Strategies and progresses for enhancing targeted antibiotic delivery. Adv. Drug Deliv. Rev. 2022, 189, 114502. [Google Scholar] [CrossRef] [PubMed]
- Ford, C.A.; Cassat, J.E. Advances in the local and targeted delivery of anti-infective agents for management of osteomyelitis. Expert. Rev. Anti Infect. Ther. 2017, 15, 851–860. [Google Scholar] [CrossRef]
- Soldevila-Boixader, L.; Fernández, A.P.; Laguna, J.M.; Uçkay, I. Local Antibiotics in the Treatment of Diabetic Foot Infections: A Narrative Review. Antibiotics 2023, 12, 124. [Google Scholar] [CrossRef]
- Grant, S.A.; Spradling, C.S.; Grant, D.N.; Fox, D.B.; Jimenez, L.; Grant, D.A.; Rone, R.J. Assessment of the biocompatibility and stability of a gold nanoparticle collagen bioscaffold. J. Biomed. Mater. Res. A 2014, 102, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Liu, D.; Wang, R.S.; Xuan, L.L.; Wang, X.H.; Li, W.Z. Two New Apotirucallane-Type Triterpenoids from the Pericarp of Toona sinensis and Their Ability to Reduce Oxidative Stress in Rat Glomerular Mesangial Cells Cultured under High-Glucose Conditions. Molecules 2020, 25, 801. [Google Scholar] [CrossRef]
- Cheng, Y.; Qin, H.; Acevedo, N.C.; Shi, X. Development of methylcellulose-based sustained-release dosage by semisolid extrusion additive manufacturing in drug delivery system. J. Biomed. Mater. Res. B Appl. Biomater. 2021, 109, 257–268. [Google Scholar] [CrossRef] [PubMed]
- Boccia, G.; Di Spirito, F.; D’Ambrosio, F.; Di Palo, M.P.; Giordano, F.; Amato, M. Local and Systemic Antibiotics in Peri-Implantitis Management: An Umbrella Review. Antibiotics 2023, 12, 114. [Google Scholar] [CrossRef] [PubMed]
- Büchter, A.; Meyer, U.; Kruse-Lösler, B.; Joos, U.; Kleinheinz, J. Sustained release of doxycycline for the treatment of peri-implantitis: Randomised controlled trial. Br. J. Oral Maxillofac. Surg. 2004, 42, 439–444. [Google Scholar] [CrossRef] [PubMed]
- Mishler, O.P.; Shiau, H.J. Management of peri-implant disease: A current appraisal. J. Evid. Based Dent. Pract. 2014, 14, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Del Amo, F.S.L.; Yu, S.H.; Sammartino, G.; Sculean, A.; Zucchelli, G.; Rasperini, G.; Felice, P.; Pagni, G.; Iorio-Siciliano, V.; Grusovin, M.G.; et al. Peri-implant Soft Tissue Management: Cairo Opinion Consensus Conference. Int. J. Environ. Res. Public Health 2020, 17, 2281. [Google Scholar] [CrossRef]
- Giudice, A.; Antonelli, A.; Muraca, D.; Fortunato, L. Usefulness of advanced-platelet rich fibrin (A-PRF) and injectable-platelet rich fibrin (i-PRF) in the management of a massive medication-related osteonecrosis of the jaw (MRONJ): A 5-years follow-up case report. Indian J. Dent. Res. 2020, 31, 813–818. [Google Scholar]
- Mozzati, M.; Gallesio, G.; Arata, V.; Pol, R.; Scoletta, M. Platelet-rich therapies in the treatment of intravenous bisphosphonate-related osteonecrosis of the jaw: A report of 32 cases. Oral Oncol. 2012, 48, 469–474. [Google Scholar] [CrossRef]
- Karasneh, J.A.; Al-Eryani, K.; Clark, G.T.; Sedghizadeh, P.P. Modified protocol including topical minocycline in orabase to manage medication-related osteonecrosis of the jaw cases. J. Oral Pathol. Med. 2016, 45, 718–720. [Google Scholar] [CrossRef]
- Deliberador, T.M.; Stutz, C.; Sartori, E.; Kluppel, L.; de Freitas, R.M. Treatment of Medication-Related Osteonecrosis of the Jaws (MRONJ) with Topical Therapy Using Active Oxygen Gel. Clin. Cosmet. Investig. Dent. 2024, 16, 249–254. [Google Scholar] [CrossRef]
- Camps-Font, O.; Sábado-Bundó, H.; Toledano-Serrabona, J.; Valmaseda-de-la-Rosa, N.; Figueiredo, R.; Valmaseda-Castellón, E. Antibiotic prophylaxis in the prevention of dry socket and surgical site infection after lower third molar extraction: A network meta-analysis. Int. J. Oral. Maxillofac. Surg. 2024, 53, 57–67. [Google Scholar] [CrossRef]
- Marenzi, G.; Gasparro, R.; Mariniello, M.; Sammartino, G.; Capone, C.; di Lauro, A.E. Advanced Platelet-Rich Fibrin as a Therapeutic Option in the Treatment of Dry Socket: Literature Review and Case Series. Appl. Sci. 2021, 11, 9474. [Google Scholar] [CrossRef]
| Domain | Inclusion Criteria | Exclusion Criteria |
|---|---|---|
| Population | Antibiotics | Drugs other than antibiotics |
| Intervention | Using autologous platelet concentrates (PRF, PRP, PRGF, CGF, i-PRF) as a sole carrier or scaffold for drug delivery | Using other carriers or scaffolds for drug delivery |
| Comparison | No antibiotic delivery | |
| Outcomes | Antibiotic loading capacity of APCs, release kinetics of antibiotic, and antibacterial effects of loaded APCs | |
| Study Design | In vitro studies, in vivo studies, animal studies, non-comparative studies, case reports, case series, and prospective/retrospective clinical trials | Narrative reviews, systematic reviews with or without meta-analysis, letters to the editors, and short communications |
| Database | Search Strategy | Hits |
|---|---|---|
| Pubmed | (“platelet-rich fibrin” [MeSH Terms] OR “platelet-rich plasma” [MeSH Terms] OR “autologous platelet concentrates” [All Fields] OR “platelet-rich in growth factors” [All Fields] OR “PRP” [All Fields] OR “PRF” [All Fields]) AND (“carrier” [Title/Abstract] OR “bio-carrier” [Title/Abstract] OR “delivery” [Title/Abstract]) OR “slow-release” [Title]) AND ((“antibiotic *”) [Title/Abstract] OR “drugs” [Title/Abstract] OR “antimicrobials”) [Title/Abstract]) | 242 |
| Scopus | TITLE-ABS-KEY (platelet-rich *) OR TITLE-ABS-KEY (autologous AND platelet AND concentrates) OR TITLE-ABS-KEY (prp) OR TITLE-ABS-KEY (prf) AND TITLE-ABS-KEY (carrier) OR TITLE-ABS-KEY (bio-carrier) OR TITLE-ABS-KEY (delivery) OR TITLE-ABS (slow-release) AND (TITLE-ABS-KEY (antibiotic *) OR TITLE-ABS-KEY (drugs) OR TITLE-ABS-KEY (antimicrobials)) | 730 |
| Web of science | (TS = (autologous platelet concentrates) OR TS = (Platelet-rich *) OR TS = (PRP) OR TS = (PRF)) AND (TS = (* carrier) OR TS = (delivery) OR TS = (slow-release)) AND (TS = (antibiotic *) OR TS = (drug *) OR TS = (antimicrobials)) | 476 |
| Author, Year of Publication | Setting | Study Design | Intervention | Control | Outcome | Results | Conclusion |
|---|---|---|---|---|---|---|---|
| Bennardo F et al., 2023 [17] | Magna Graecia University of Catanzaro, Italy | In vitro study | L-PRF loaded with gentamicin, linezolid, and vancomycin | L-PRF without antibiotics | Antibiotic release kinetics and antibacterial effects | Gentamicin and linezolid were significantly trapped or bound to the PRF membranes and released over time. Gentamicin-PRF had significant antibacterial activity against E. coli, P. aeruginosa, S. mitis, H. influenzae, S. pneumoniae, and S. aureus. Linezolid-PRF had a comparable activity against E. coli and P. aeruginosa to the control PRF. | Using PRF loaded with antibiotics after oral surgery may reduce the risk of post-operative infection and replace or enhance systemic antibiotic therapy while preserving the healing properties of PRF. |
| Dubnika A et al., 2021 [18] | Riga Stradins University | In vitro study | i-PRF loaded with Vancomycin hydrochloride (VANKA) carriers as liposomes and microcapsules | i-PRF without carriers | Antibiotic loading capacity, antibiotic release kinetics, and antibacterial effects | VANKA included in a PRF scaffold without a carrier did not ensure the controlled loading capacity and release of antibiotics. A complete antibacterial effect against S. aureus lasted for 48 h, but with a rapid drop of effectiveness after the first 24 h. | This study confirms that the use of a carrier system can ensure controlled VANKA release from PRF for 6 to 10 days. |
| Egle K et al., 2022 [19] | Riga Stradins University | In vitro study | PRF loaded with clindamycin phosphate (CLP) | PRF without CLP and pure CLP solutions | Antibiotic release kinetics and antibacterial effects | A burst release of CLP was observed for all samples at 0.25, 0.5, 1, 2, 4, 6, 17, and 24 h; at 24 h, 80% was released. A significant decrease in MIC against S. aureus and S. epidermidis was observed compared to pure CLP solutions. | This modified PRF could be used as a novel method to increase drug delivery and efficacy and to reduce the risk of postoperative infection. |
| Ercan E. et al., 2022 [20] | Canakkale OnSekiz Mart University | In vitro study | T-PRF loaded with doxyciclin | Collagen combined with doxyciclin | Antibiotic loading capacity, antibiotic release kinetics, and antibacterial effects | In comparison with collagen, approximately sevenfold more Doxy was loaded into T-PRF (281 ± 43 mg/g vs. 47 ± 4 mg/g). A total of 25% of the loaded Doxy was released from T-PRF compared to only 12% from collagen within 72 h. The largest IZD was observed for T-PRF/Dox with 32 + 6 mm and 37 ± 5 mm for P. aeruginosa and S. aureus, respectively. | T-PRF was shown to have potential autogenous long-term drug-carrying capability for doxycycline. |
| Kadam S. et al., 2023 [21] | Department of Periodontology, Dr. D. Y. Patil Dental College & Hospital, Pimpri, Pune | In vivo study: prospective randomized controlled trial (RCT) | PRF loaded with amoxicillin | PRF without antibiotic | Clinical and radiographic parameters: PPD, RAL and RGML, WHI and defect fill | Intergroup comparison of mean PPD, RAL, and RGML parameters at baseline and 6 months postoperatively showed no statistically significant difference. Comparison of WHI between groups showed significant healing at 7 days post operatively. Defect fill change showed no significant difference between groups from baseline to 6 months. | Both treatment modalities are equally effective in the treatment of intrabony defects, but the use of PRF/amoxicillin significantly benefited the initial wound healing. |
| Knafl D. et al., 2017 [22] | Medical University of Vienna | In vitro study | PRF mixed with teicoplanin, amikacin, or polyhexanide | PRF without antibiotics | Antibiotic release kinetics and antibacterial effects | More than 1000 mg/L teicoplanin were released within the first 24 h and 28.22 mg/L after 168 h. Amikacin release was above 10,000 mg/L within the first 24 h and still 120.8 mg/L after 120 h. A release of polyhexanide could be verified for the first 24 h only. Consequently, teicoplanin and amikacin released from PRF showed antimicrobial in vitro effects for almost a week, whereas the antimicrobial effect of polyhexanide could only be verified for the first 24 h. | Wound bandages in wounds treated with PRF plus amikacin or PRF plus teicoplanin can be left for at least five days, regarding antimicrobial efficacy. |
| Polak D. et al., 2019 [23] | Department of Periodontology, The Hebrew University-Hadassah Medical Center, Jerusalem, Israel | In vitro study | PRF loaded with metronidazole, clindamycin, and penicillin | Collagen sponges with and without antibiotics | Antibacterial effects | PRF with saline had minor antibacterial activity, while all PRFs with antibiotics showed significant antibacterial activity against S. aureus or Fusobacterium nucleatum. | Platelet-rich fibrin incorporated with antibiotics may be used to reduce the risk of post-operative infection in addition to the beneficial healing properties of PRF. |
| Rafiee A. et al., 2021 [24] | Shiraz University of Medical Sciences, Shiraz, Iran | In vitro study | i-PRF loaded with metronidazole, ciprofloxacin, and minocycline | i-PRF without antibiotics | Antibiotic release kinetics and antibacterial effects | The test group showed burst release within the first 24 h followed by sustained maintenance of all three antibiotics up to 14 days. The control group could not sustainably release the antibiotics. The highest antibacterial activity against A. naeslundii belonged to the group of i-PRF-loaded antibiotics. However, the test and control groups had similar antibacterial properties against E. faecalis. | Taken together, the fabricated scaffold could dramatically reduce both total bacterial gene quantification and the number of live bacteria inside the root canal. |
| Straub A. et al., 2022 [25] | University Hospital in Würzburg, Germany | In vitro study | PRF loaded with ampicillin/sulbactam | PRF without antibiotics | Antibiotic concentration and antibacterial effects | PRF is highly enriched with ampicillin/sulbactam, and the antibiotic concentration in PRF was comparable to that in the plasma concentration. The IZ of PRF was comparable to the standard ampicillin/sulbactam discs against H. influenzae, S. pneumoniae, S. aureus, and E. coli. | PRF is a reliable bio-carrier for systemic applied antibiotics and exhibits a large antimicrobial effect. |
| Straub A. et al., 2023 [26] | University Hospital in Würzburg, Germany | In vitro study | PRF prepared with three centrifugation protocols (A: 1300 rpm, 8 min; B: 2300 rpm, 12 min; C: 1500 rpm, 14 min) loaded with ampicillin/sulbactam | PRF without antibiotics | Antibiotic concentration and antibacterial effects | A single dose of ampicillin/sulbactam was sufficient to reach high concentrations in PRF in all protocols, which was comparable to the plasma concentration. Protocol B showed the largest inhibition zones against H. Influenzae, S. aureus, S. pneumoniae, E. coli, and P. gingivalis. | A single dose of ampicillin/sulbactam is sufficient to reach clinically relevant concentrations in PRF. |
| Straub A., et al., 2023 [27] | University Hospital in Würzburg, Germany | In vitro study | PRF loaded with amoxicillin/clavulanic acid or ampicillin/sulbactam | PRF without antibiotics | Antibacterial effect | A double dose of amoxicillin/clavulanic acid showed higher IZ against E. coli, S. aureus, S. pneumoniae, H. Influenzae, and P. gingivalis compared to a single dose. | The results demonstrate that oral administration is a suitable route for loading PRF with these drugs. This could expand the scope of PRF application to prevent infections at the surgical site. |
| Straub A. et al., 2024 [28] | University Hospital in Würzburg, Germany | In vitro study | PRF loaded with clindamycin | PRF without clindamycin | Antibiotic concentration and antibacterial effects | The mean concentration of clindamycin was 0.7 μg/100 mg in PRF, which was significantly lower than in plasma. IZ against S. aureus, S. pneumoniae, Streptococcus mitis, P. gingivalis, and Fusobacterium nucleatum was significant. | PRF is a suitable bio-carrier for CLI when administered systematically to patients. |
| Wang S et al., 2021 [29] | Daping Hospital Army Medical University, Chongqing, China | In vitro and in vivo study | PRP in a local antibiotic delivery system (PADS): PRP loaded with vancomycin hydrochloride, clindamycin phosphate, ceftazidime, and thrombin | PRP without vancomycin hydrochloride, clindamycin phosphate, ceftazidime, and thrombin | Antibiotic release kinetics and antibacterial effect | About 60% of the total vancomycin and ceftazidime dose was released within 10 min; then, the release rate gradually decreased. However, 90% of clindamycin was released within 10 min. There was no significant difference in IZD against S. aureus, E. coli, and P. aeruginosa between the test and control groups. | This novel PADS approach might represent a potential therapy for patients who have sustained infected bone defects. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gasparro, R.; Di Spirito, F.; Campana, M.D.; Sammartino, G.; di Lauro, A.E. The Role of Autologous Platelet Concentrates as a Local Antibiotic Delivery System: A Systematic Scoping Review. Antibiotics 2024, 13, 856. https://doi.org/10.3390/antibiotics13090856
Gasparro R, Di Spirito F, Campana MD, Sammartino G, di Lauro AE. The Role of Autologous Platelet Concentrates as a Local Antibiotic Delivery System: A Systematic Scoping Review. Antibiotics. 2024; 13(9):856. https://doi.org/10.3390/antibiotics13090856
Chicago/Turabian StyleGasparro, Roberta, Federica Di Spirito, Maria Domenica Campana, Gilberto Sammartino, and Alessandro E. di Lauro. 2024. "The Role of Autologous Platelet Concentrates as a Local Antibiotic Delivery System: A Systematic Scoping Review" Antibiotics 13, no. 9: 856. https://doi.org/10.3390/antibiotics13090856
APA StyleGasparro, R., Di Spirito, F., Campana, M. D., Sammartino, G., & di Lauro, A. E. (2024). The Role of Autologous Platelet Concentrates as a Local Antibiotic Delivery System: A Systematic Scoping Review. Antibiotics, 13(9), 856. https://doi.org/10.3390/antibiotics13090856









