Self-Medication as an Important Risk Factor for Antibiotic Resistance: A Multi-Institutional Survey among Students
Abstract
:1. Introduction
2. Results
2.1. Contributed Departments
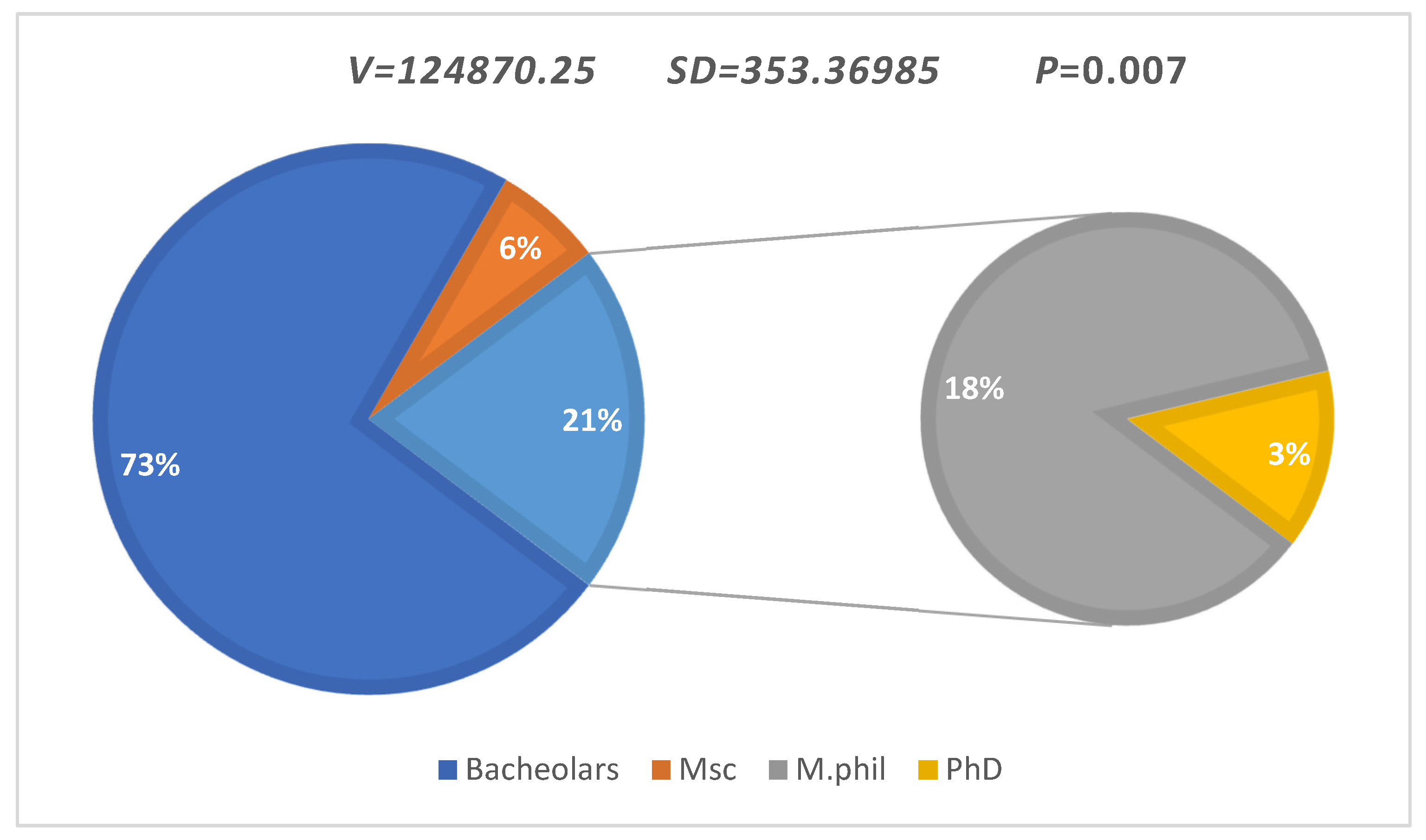
2.2. Disciplines Contributed
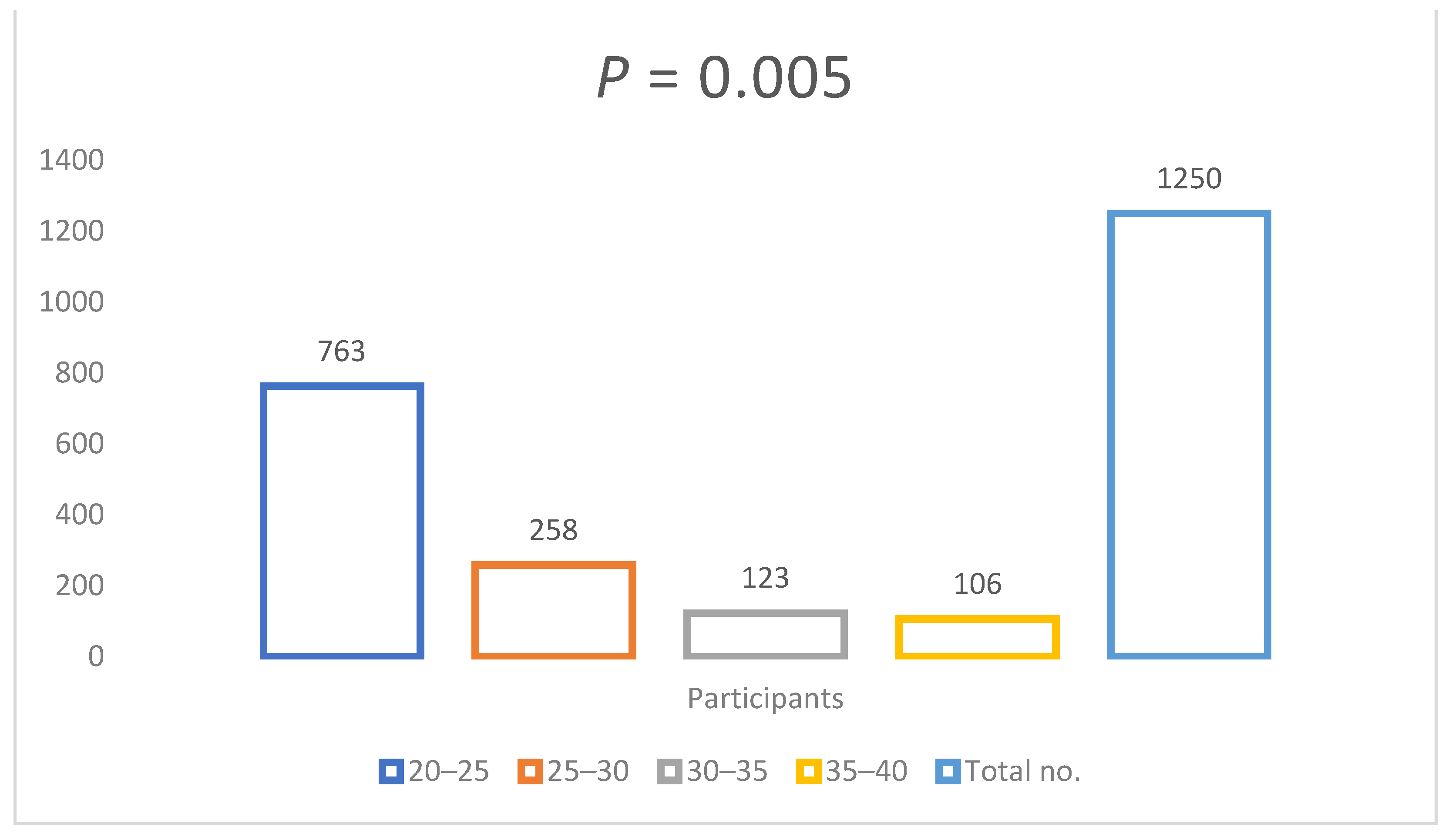
2.3. Age Interpretation
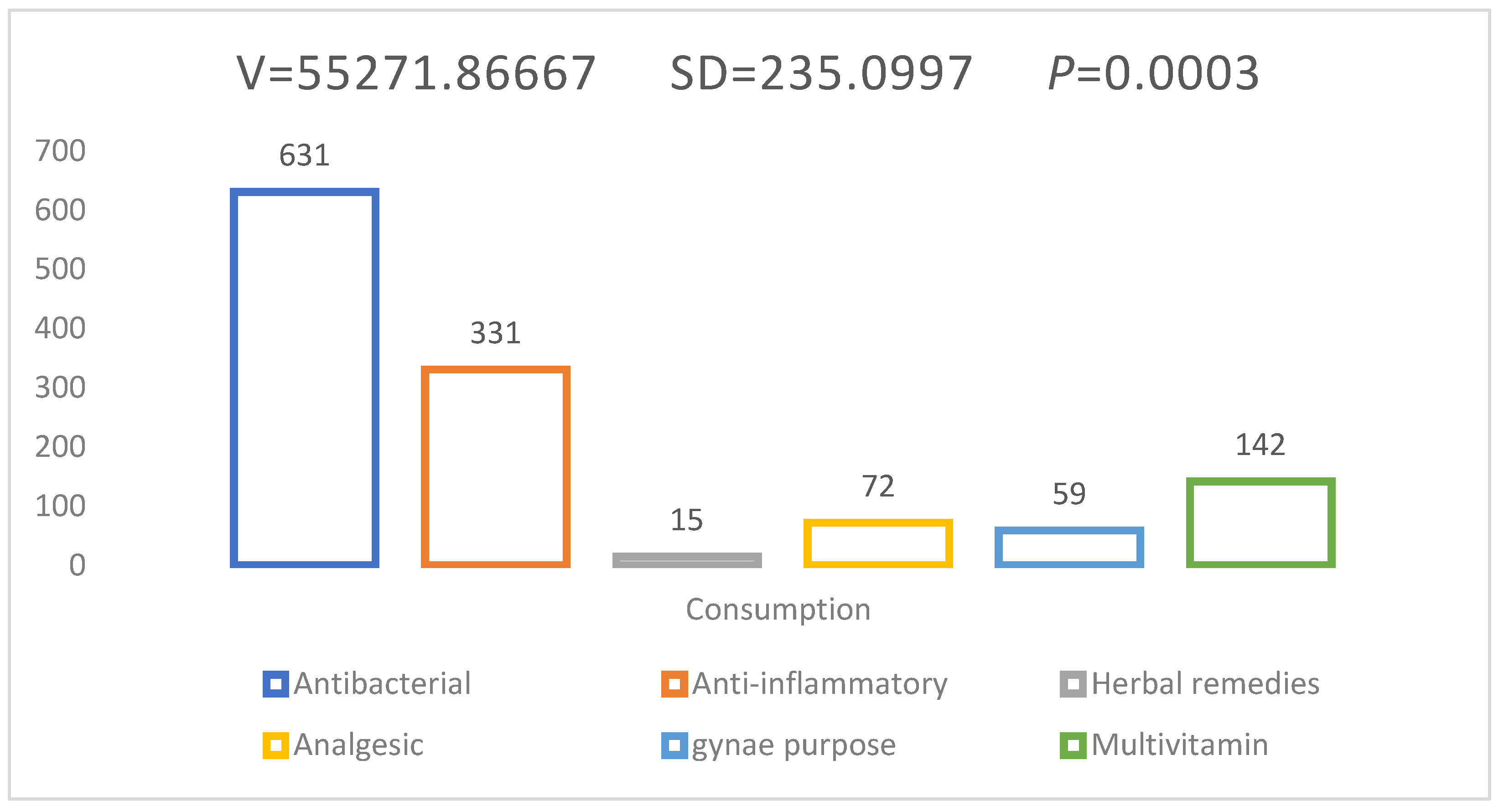
2.4. Daily Practices and Approach of Self-Medication in Students
2.5. Current Challenges and Antibiotics Mindset/Counseling in Students
2.6. Overall Relationship between Daily Practices and Knowledge of Antibiotics among Students
2.7. Self-Medication Practices in Students to Treat Disease/Illness
2.8. Relationship between Self-Practices and Treatment of Disease in Students
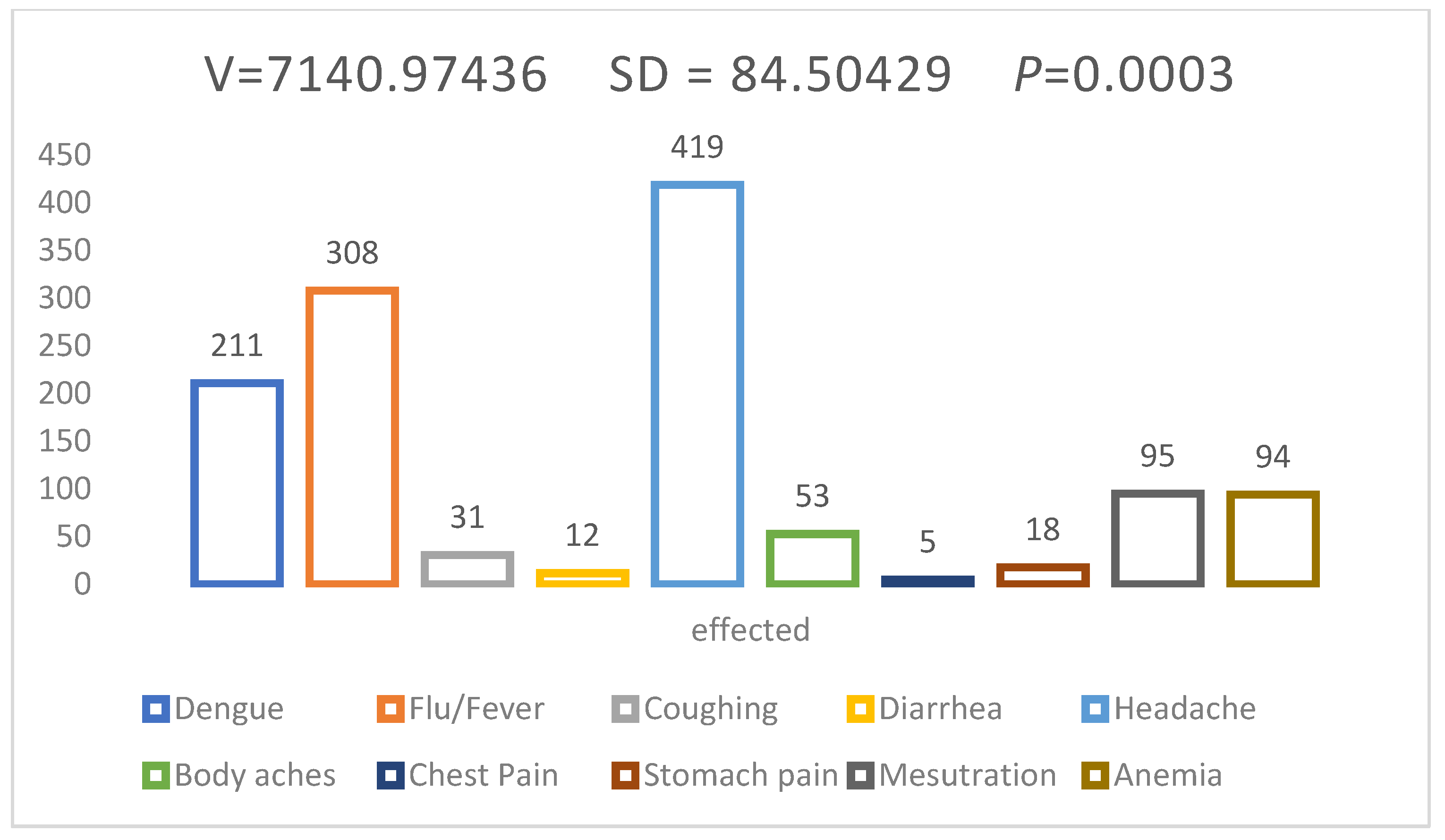
2.9. Prevalence of Infection/Disease Treated by Self-Medication in Students
3. Discussion
4. Materials and Methods
4.1. Study Area and Selection of Study Participants
4.2. Interview Calendar
4.3. Sample Processing
4.4. Statistical Analysis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zafar, S.N.; Syed, R.; Waqar, S.; Zubairi, A.J.; Vaqar, T.; Shaikh, M.; Yousaf, W.; Shahid, S.; Saleem, S. Self-medication amongst university students of Karachi: Prevalence, knowledge and attitudes. J. Pak. Med. Assoc. 2008, 58, 214. [Google Scholar]
- Mumtaz, Y.; Jahangeer, S.; Mujtaba, T.; Zafar, S.; Adnan, S. Self medication among university students of Karachi. Jlumhs 2011, 10, 102–105. [Google Scholar]
- Chuwa, B.B.; Njau, L.A.; Msigwa, K.I.; Shao, E. Prevalence and factors associated with self medication with antibiotics among University students in Moshi Kilimanjaro Tanzania. Afr. Health Sci. 2021, 21, 633–639. [Google Scholar] [CrossRef] [PubMed]
- Yin, X.; Mu, K.; Yang, H.; Wang, J.; Chen, Z.; Jiang, N.; Yang, F.; Zhang, G.; Wu, J. Prevalence of self-medication with antibiotics and its related factors among Chinese residents: A cross-sectional study. Antimicrob. Resist. Infect. Control 2021, 10, 89. [Google Scholar] [CrossRef] [PubMed]
- Zahra, N.; Zeshan, B.; Qadri, M.M.A.; Ishaq, M.; Afzal, M.; Ahmed, N. Phenotypic and Genotypic Evaluation of Antibiotic Resistance of Acinetobacter baumannii Bacteria Isolated from Surgical Intensive Care Unit Patients in Pakistan. Jundishapur J. Microbiol. 2021, 14, e113008. [Google Scholar] [CrossRef]
- Levy, M. The many faces (and potential dangers) of self-medication as an explanatory concept for substance use. Int. J. Adv. Couns. 2019, 41, 15–24. [Google Scholar] [CrossRef]
- Zawahir, S.; Lekamwasam, S.; Halvorsen, K.H.; Rose, G.; Aslani, P. Self-medication Behavior with antibiotics: A national cross-sectional survey in Sri Lanka. Expert Rev. Anti-Infect. Ther. 2021, 19, 1341–1352. [Google Scholar] [CrossRef]
- Selvaraj, K.; Kumar, S.G.; Ramalingam, A. Prevalence of self-medication practices and its associated factors in Urban Puducherry, India. Perspect. Clin. Res. 2014, 5, 32. [Google Scholar]
- Rather, I.A.; Kim, B.-C.; Bajpai, V.K.; Park, Y.-H. Self-medication and antibiotic resistance: Crisis, current challenges, and prevention. Saudi J. Biol. Sci. 2017, 24, 808–812. [Google Scholar] [CrossRef]
- Parveen, S.; Saqib, S.; Ahmed, A.; Shahzad, A.; Ahmed, N. Prevalence of MRSA colonization among healthcare-workers and effectiveness of decolonization regimen in ICU of a Tertiary care Hospital, Lahore, Pakistan. Adv. Life Sci. 2020, 8, 38–41. [Google Scholar]
- Khalid, S.; Ali, Q.; Hafeez, M.; Malik, A. Perception regarding self-medication of antibiotics in general public sector university of Southern Punjab: A comparison between medical and non-medical students. Biol. Clin. Sci. Res. J. 2021, 2021, 51. [Google Scholar] [CrossRef]
- Nusair, M.B.; Al-azzam, S.; Alhamad, H.; Momani, M.Y. The prevalence and patterns of self-medication with antibiotics in Jordan: A community-based study. Int. J. Clin. Pract. 2021, 75, e13665. [Google Scholar] [CrossRef] [PubMed]
- Owusu-Ofori, A.K.; Darko, E.; Danquah, C.A.; Agyarko-Poku, T.; Buabeng, K.O. Self-Medication and Antimicrobial Resistance: A Survey of Students Studying Healthcare Programmes at a Tertiary Institution in Ghana. Front. Public Health 2021, 9, 706290. [Google Scholar] [CrossRef] [PubMed]
- Hughes, C.M.; McElnay, J.C.; Fleming, G.F. Benefits and risks of self medication. Drug Saf. 2001, 24, 1027–1037. [Google Scholar] [CrossRef] [PubMed]
- Elmahi, O.K.O.; Musa, R.A.E.; Shareef, A.A.H.; Omer, M.E.A.; Elmahi, M.A.M.; Altamih, R.A.A.; Mohamed, R.I.H.; Alsadig, T.F.M. Perception and practice of self-medication with antibiotics among medical students in Sudanese universities: A cross-sectional study. PLoS ONE 2022, 17, e0263067. [Google Scholar] [CrossRef] [PubMed]
- Nepal, G.; Bhatta, S. Self-medication with antibiotics in WHO Southeast Asian Region: A systematic review. Cureus 2018, 10, e2428. [Google Scholar] [CrossRef] [Green Version]
- Roien, R.; Bhandari, D.; Hosseini, S.M.R.; Mosawi, S.H.; Ataie, M.A.; Ozaki, A.; Martellucci, C.A.; Kotera, Y.; Delshad, M.H.; Sawano, T. Prevalence and determinants of self-medication with antibiotics among general population in Afghanistan. Expert Rev. Anti-Infect. Ther. 2022, 20, 315–321. [Google Scholar] [CrossRef]
- Yeika, E.V.; Ingelbeen, B.; Kemah, B.L.; Wirsiy, F.S.; Fomengia, J.N.; Van der Sande, M.A. Comparative assessment of the prevalence, practices and factors associated with self-medication with antibiotics in Africa. Trop. Med. Int. Health 2021, 26, 862–881. [Google Scholar] [CrossRef]
- Bennadi, D. Self-medication: A current challenge. J. Basic Clin. Pharm. 2013, 5, 19. [Google Scholar] [CrossRef]
- Zeshan, B.; Karobari, M.I.; Afzal, N.; Siddiq, A.; Basha, S.; Basheer, S.N.; Peeran, S.W.; Mustafa, M.; Daud, N.H.A.; Ahmed, N.; et al. The Usage of Antibiotics by COVID-19 Patients with Comorbidities: The Risk of Increased Antimicrobial Resistance. Antibiotics 2021, 11, 35. [Google Scholar] [CrossRef]
- Alsous, M.; Elayeh, E.; Jalil, M.A.; Alhawmdeh, E. Evaluation of Self-Medication Practice among Pharmacy Students in Jordan. Jordan J. Pharm. Sci. 2018, 11, 15–24. [Google Scholar]
- Klemenc-Ketis, Z.; Hladnik, Z.; Kersnik, J. Self-medication among healthcare and non-healthcare students at University of Ljubljana, Slovenia. Med. Princ. Pract. 2010, 19, 395–401. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, M.E. Risks of self-medication practices. Curr. Drug Saf. 2010, 5, 315–323. [Google Scholar] [CrossRef] [PubMed]
- James, H.; Handu, S.S.; Al Khaja, K.A.; Otoom, S.; Sequeira, R.P. Evaluation of the knowledge, attitude and practice of self-medication among first-year medical students. Med. Princ. Pract. 2006, 15, 270–275. [Google Scholar] [CrossRef]
| Serial No. | Questions | Keys | Scores | p Value |
|---|---|---|---|---|
| Q1 | What is antibiotic? | Chemical used against the microbes | n = 205 | 0.002 * |
| Reduce the disease or illness | n = 45 | |||
| Inhibit or kill the micro-organism | n = 1005 | |||
| Q2 | Do you currently use any of the following antibiotics or other medications? | Broad spectrum | n = 750 | |
| Narrow spectrum | n = 355 | |||
| Others | n = 145 | |||
| Q3 | Had you got any adverse reactions? | No | n = 991 | |
| Yes | n = 259 | |||
| Q4 | Is self-medication better for human health? | Yes | n = 980 | |
| No | n = 208 | |||
| Not noted | n = 62 | |||
| Q5 | What is your concept for self-medication? Why you did choose it? | Reliable | n = 173 | |
| Exempt Physician fee | n = 241 | |||
| Unable to walk at distance | n = 199 | |||
| Self-satisfaction | n = 637 |
| Serial No. | Questions | Keys | Scores | Pearson Correlation Coefficient | (Mean) (Standard Deviation) | p Value |
|---|---|---|---|---|---|---|
| Q1 | Do you know world is facing antibiotics resistance due to self-medication or misuse of antibiotics? | Yes | n = 570 | R = 0.0311 | M = 431.5 | 0.002 * |
| No | n = 627 | |||||
| Not sure | n = 53 | |||||
| Q2 | Do you know high consumption of Antibiotics can damage your body organs? | Yes | n = 865 | |||
| No | n = 138 | |||||
| Maybe | n = 247 | |||||
| Q3 | Do you know high consumption of Antibiotics can resistance against micro-organisms? | Yes | n = 782 | SD = 1,615,917 | ||
| No | n = 152 | |||||
| Maybe | n = 316 | |||||
| Q4 | As a self-medicated person, did a doctor or dentist ever talk to you about the dangers of antibiotics? | Yes | n = 421 | |||
| No | n = 805 | |||||
| I did not see a doctor or dentist | n = 24 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zeb, S.; Mushtaq, M.; Ahmad, M.; Saleem, W.; Rabaan, A.A.; Naqvi, B.S.Z.; Garout, M.; Aljeldah, M.; Al Shammari, B.R.; Al Faraj, N.J.; et al. Self-Medication as an Important Risk Factor for Antibiotic Resistance: A Multi-Institutional Survey among Students. Antibiotics 2022, 11, 842. https://doi.org/10.3390/antibiotics11070842
Zeb S, Mushtaq M, Ahmad M, Saleem W, Rabaan AA, Naqvi BSZ, Garout M, Aljeldah M, Al Shammari BR, Al Faraj NJ, et al. Self-Medication as an Important Risk Factor for Antibiotic Resistance: A Multi-Institutional Survey among Students. Antibiotics. 2022; 11(7):842. https://doi.org/10.3390/antibiotics11070842
Chicago/Turabian StyleZeb, Shah, Mariam Mushtaq, Muneeb Ahmad, Waqas Saleem, Ali A. Rabaan, Bibi Salma Zahid Naqvi, Mohammed Garout, Mohammed Aljeldah, Basim R. Al Shammari, Nehad J. Al Faraj, and et al. 2022. "Self-Medication as an Important Risk Factor for Antibiotic Resistance: A Multi-Institutional Survey among Students" Antibiotics 11, no. 7: 842. https://doi.org/10.3390/antibiotics11070842
APA StyleZeb, S., Mushtaq, M., Ahmad, M., Saleem, W., Rabaan, A. A., Naqvi, B. S. Z., Garout, M., Aljeldah, M., Al Shammari, B. R., Al Faraj, N. J., Al-Zaki, N. A., Al Marshood, M. J., Al Saffar, T. Y., Alsultan, K. A., Al-Ahmed, S. H., Alestad, J. H., Naveed, M., & Ahmed, N. (2022). Self-Medication as an Important Risk Factor for Antibiotic Resistance: A Multi-Institutional Survey among Students. Antibiotics, 11(7), 842. https://doi.org/10.3390/antibiotics11070842







