Antimicrobial Resistance and Environmental Health: A Water Stewardship Framework for Global and National Action
Abstract
:1. Introduction
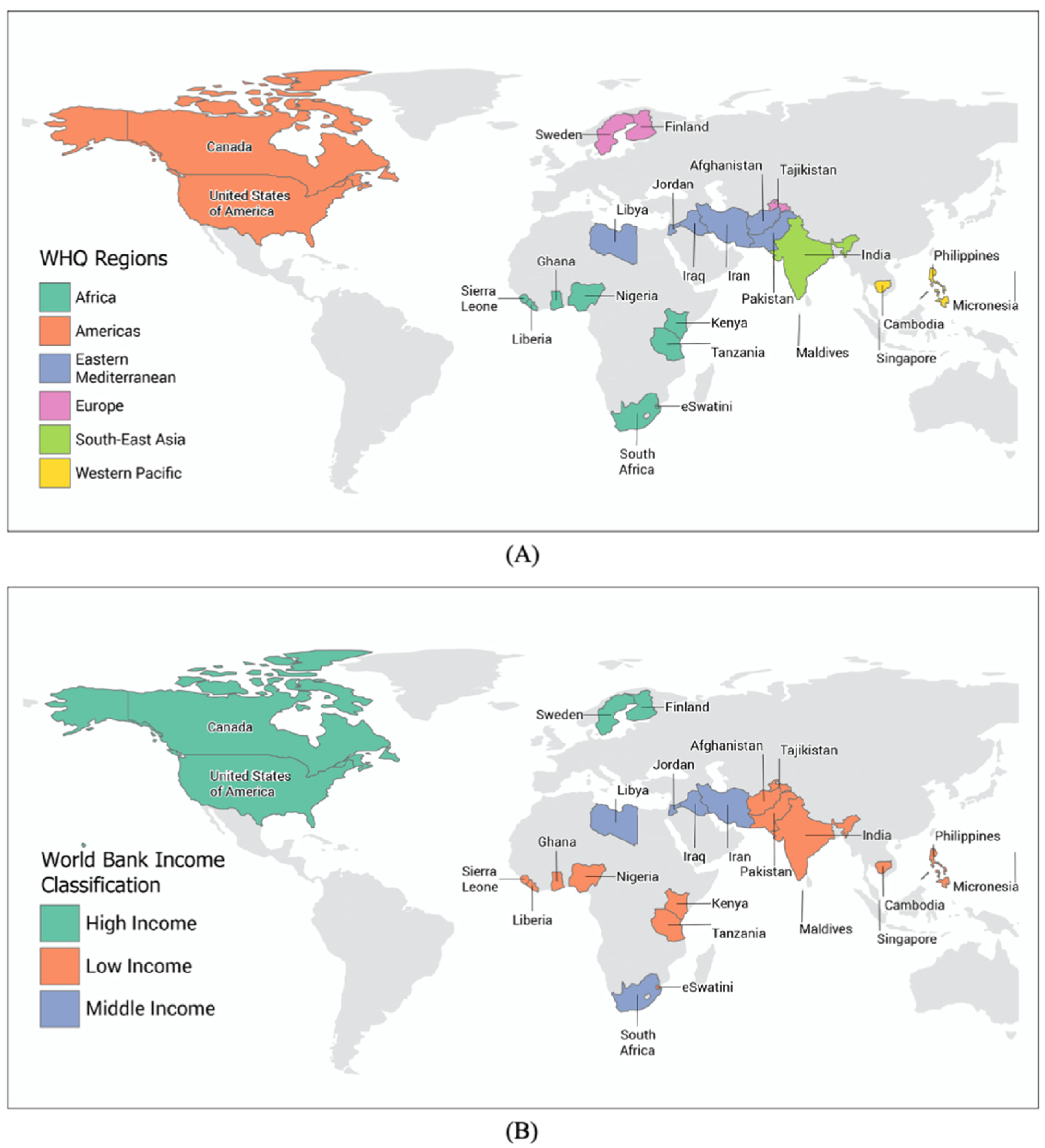
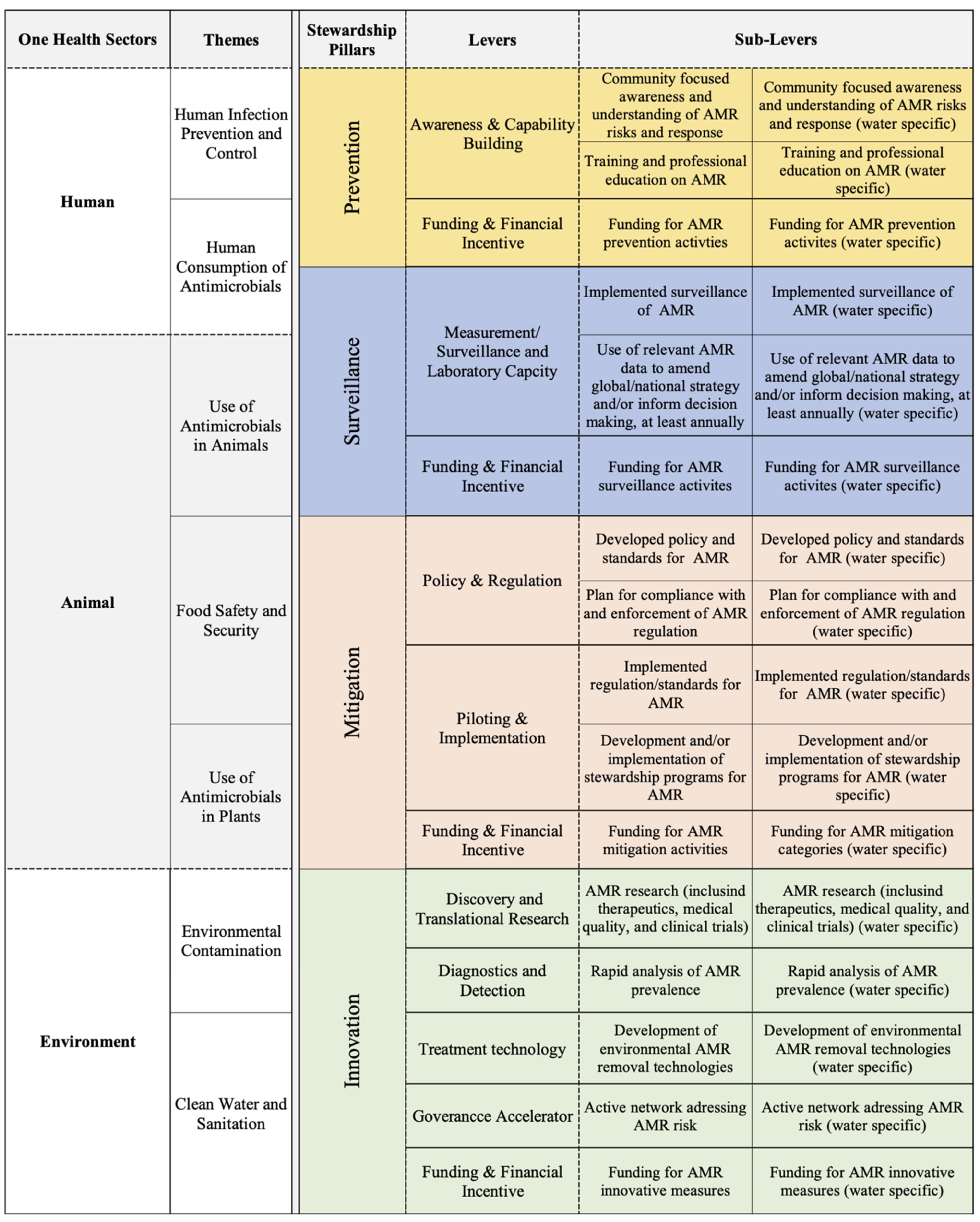
2. Results and Discussion
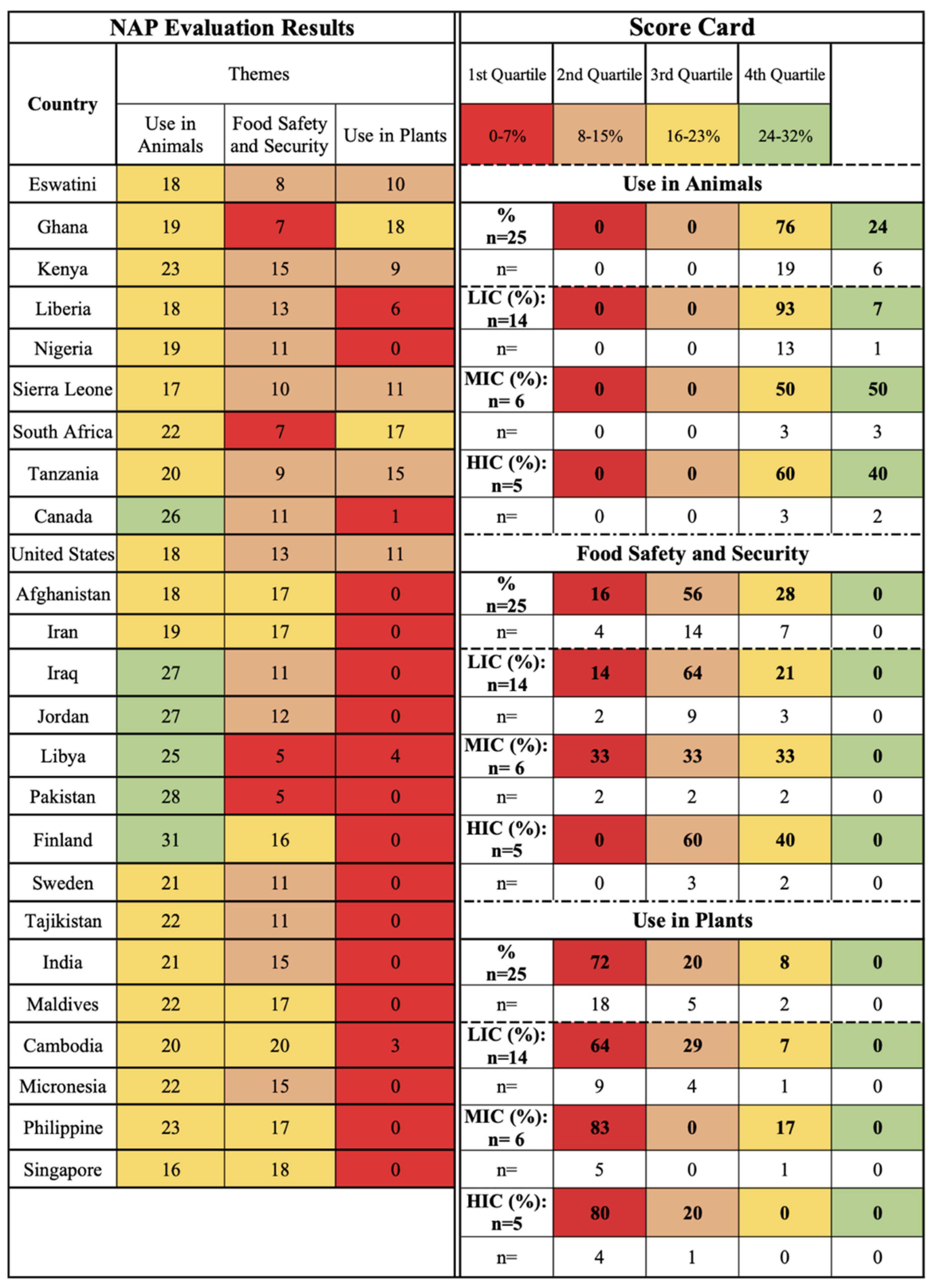
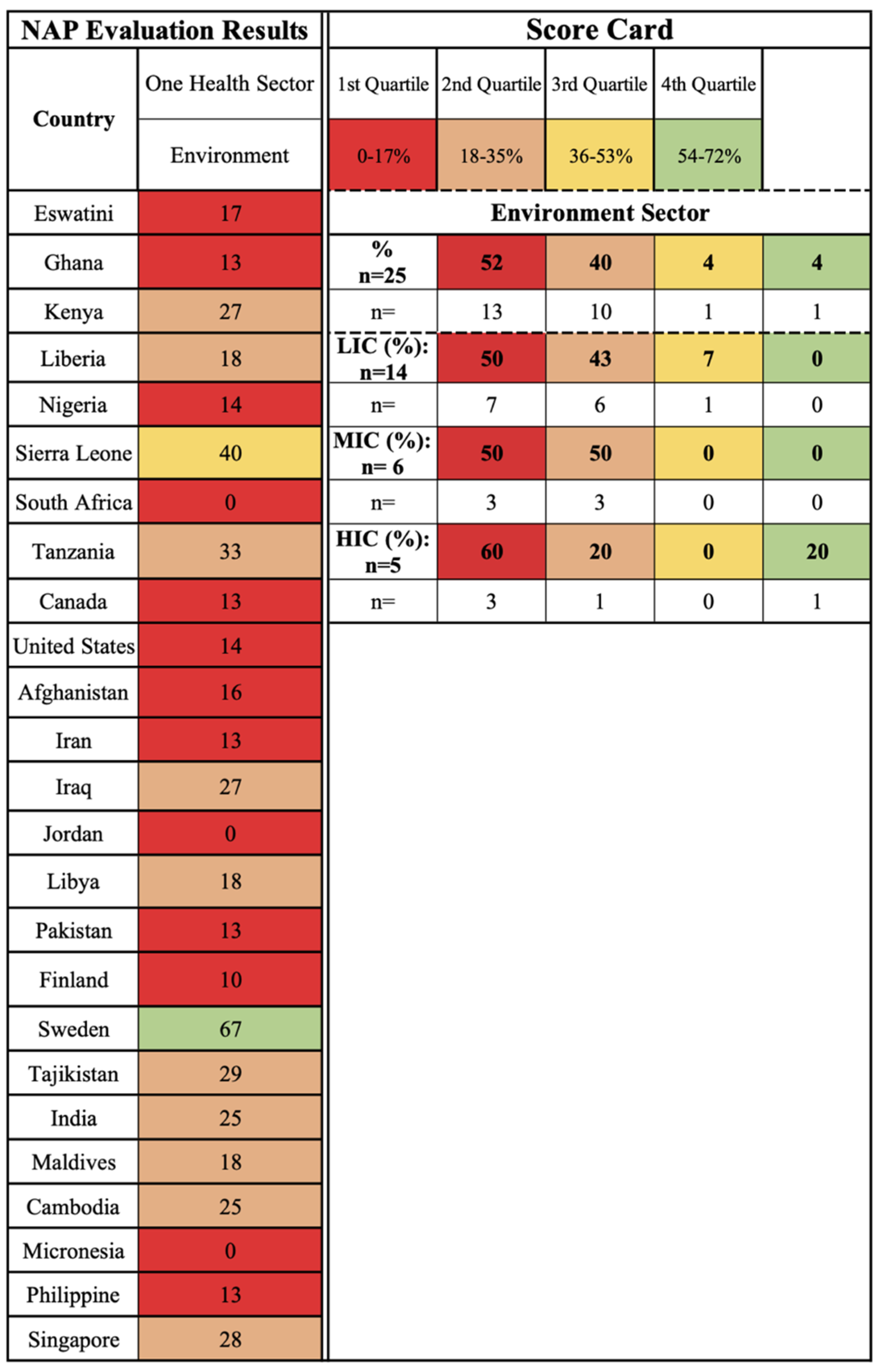
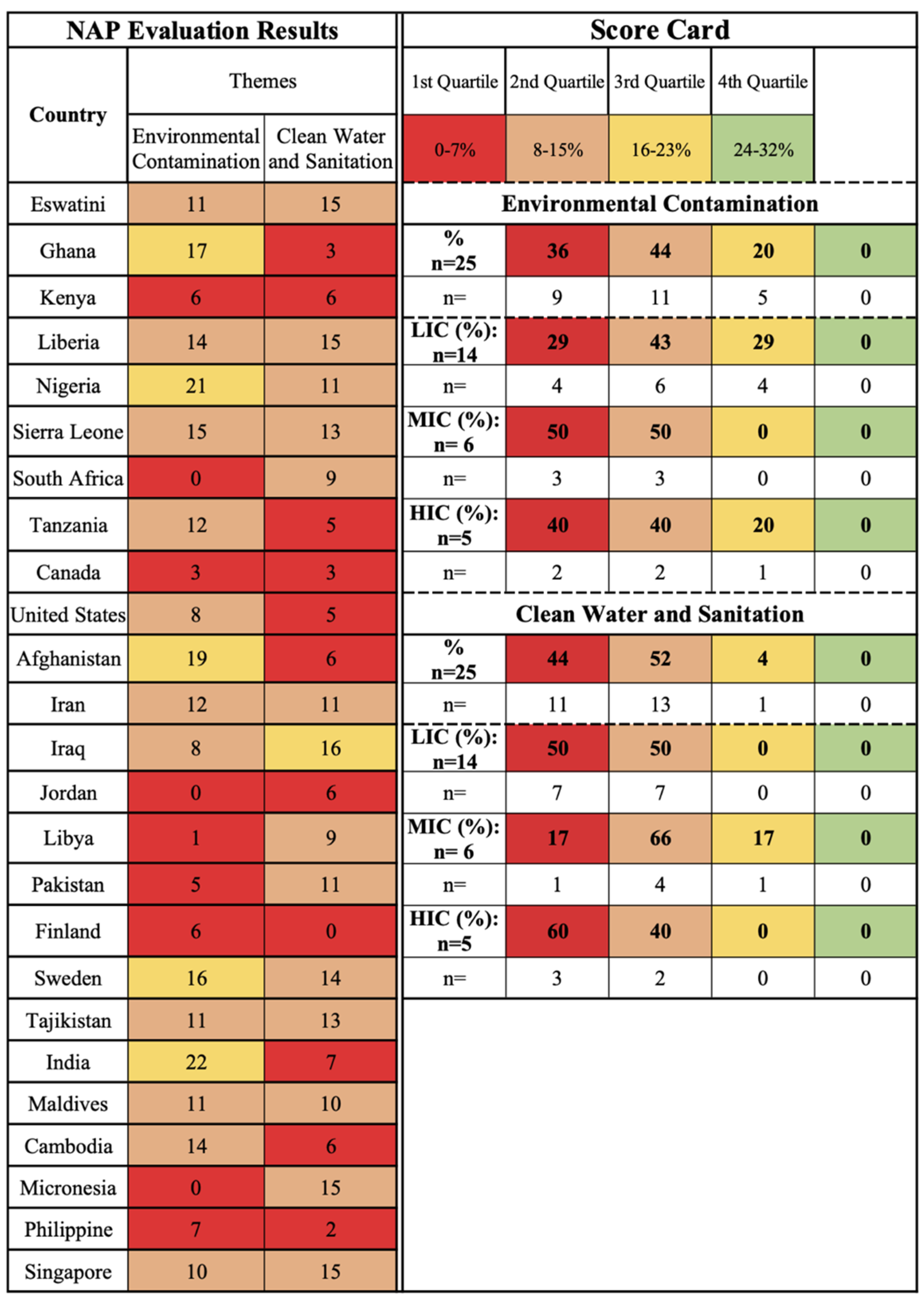
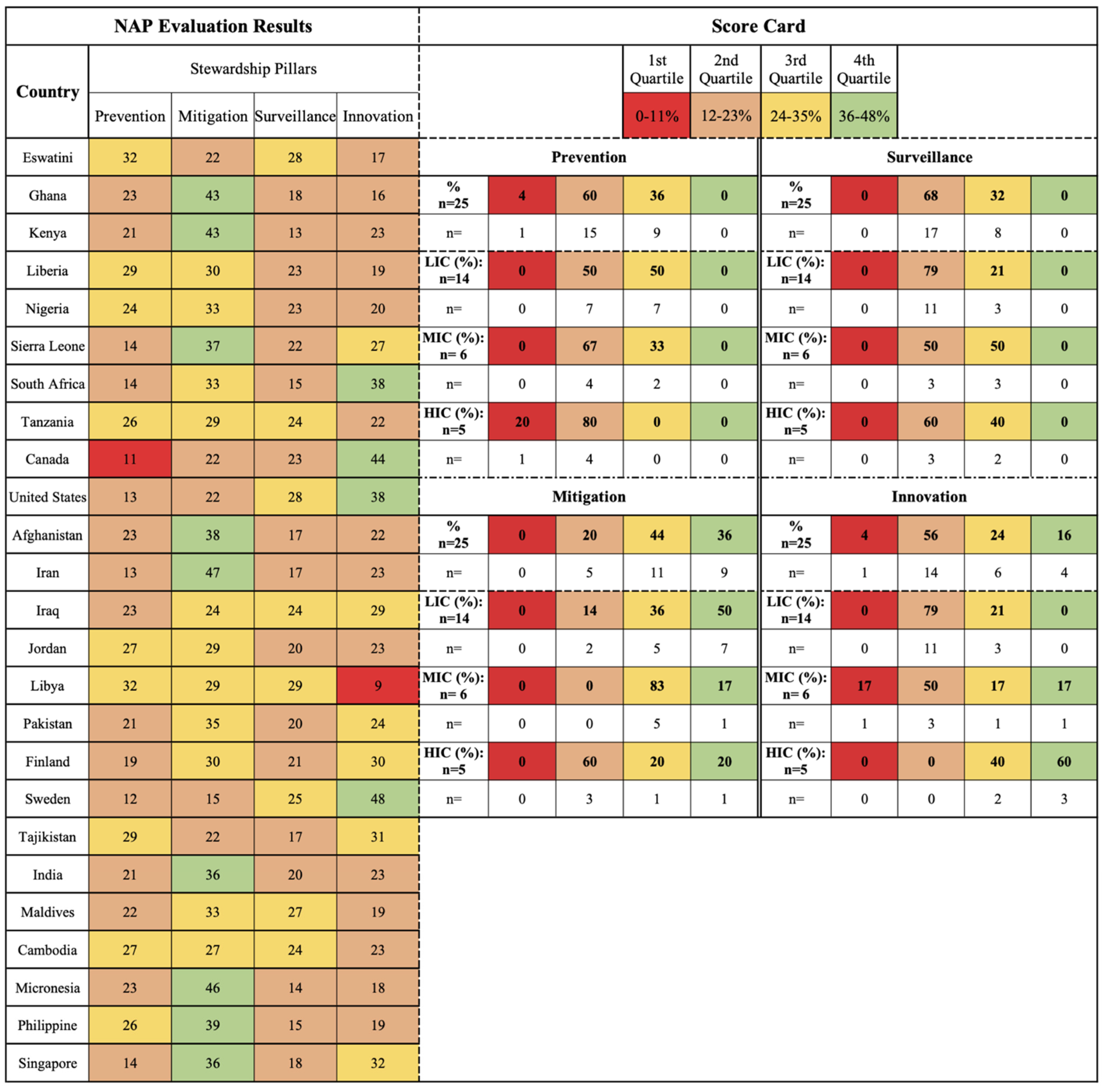
2.1. NAP Evaluation Results
- One Health sectors (human, animal, and environment) and themes (human IPC, human antimicrobial consumption, use of antimicrobials in animals, food safety and security, use of antimicrobials in plants, environmental contamination, and clean water and sanitation);
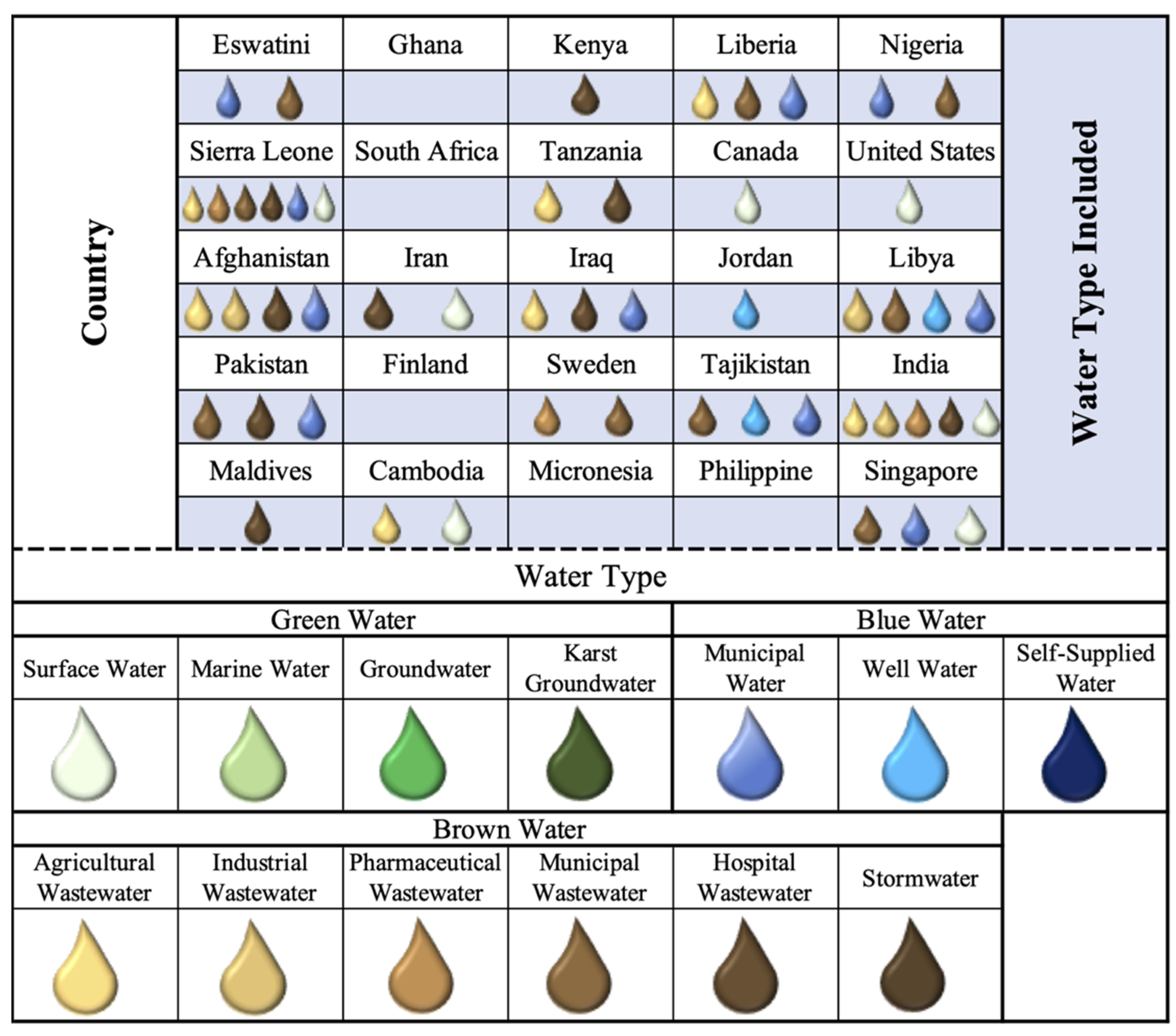
- Water types (environmental (green), supply (blue), wastewater (brown));
- Pillars (mitigation, innovation, prevention, and surveillance).
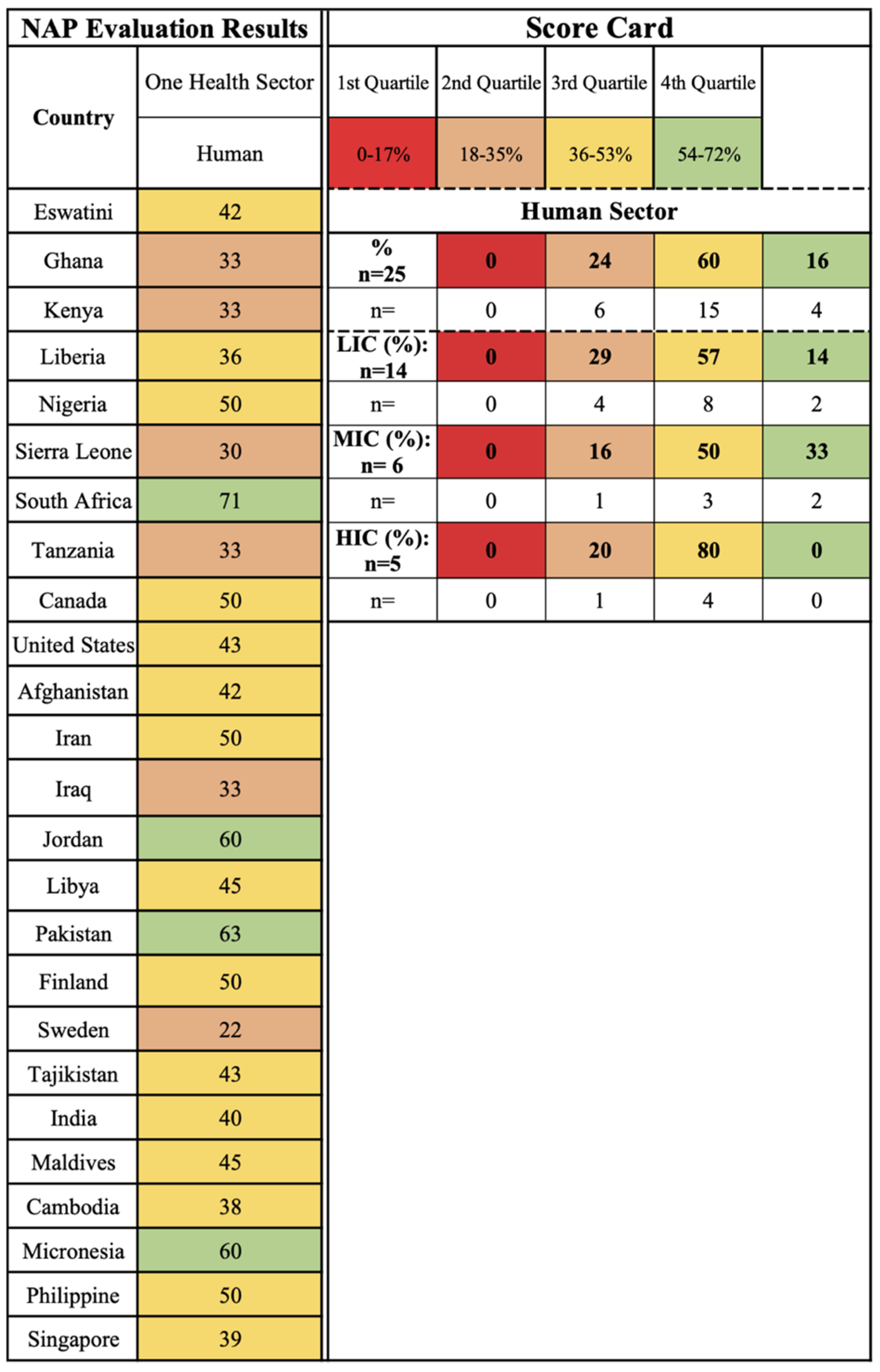
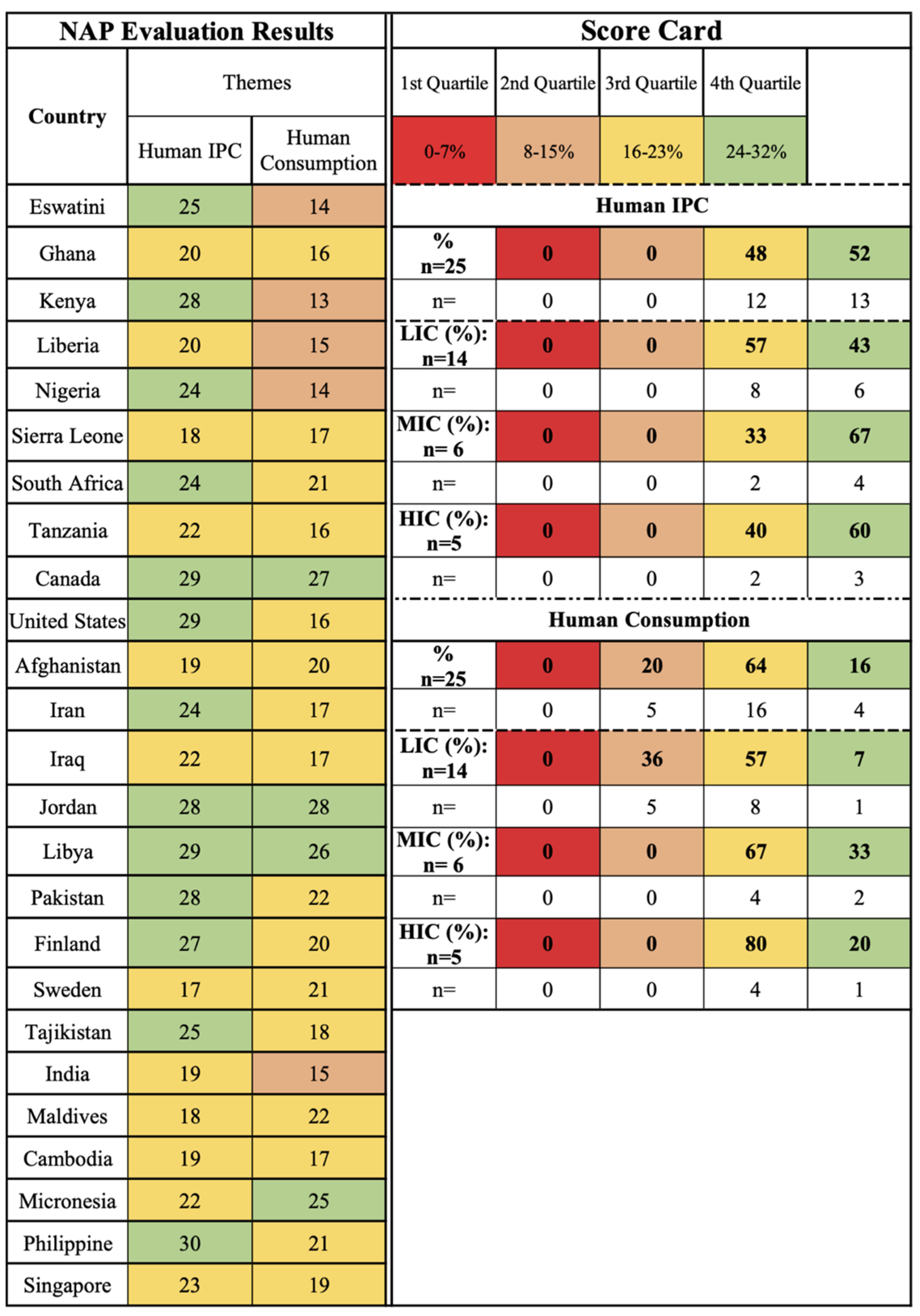
2.2. One Health Sector: Human and Related Themes Findings
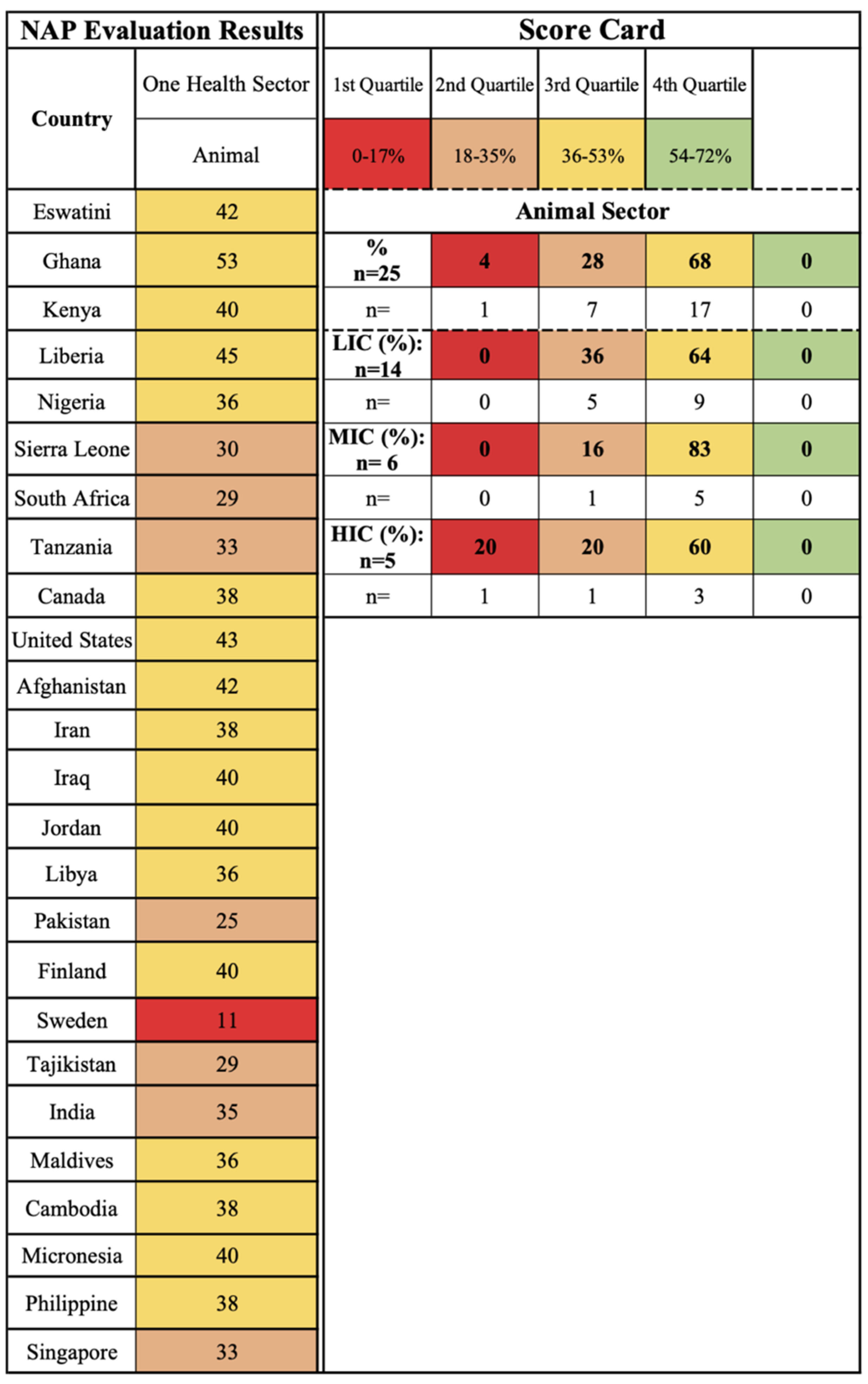
2.3. One Health Sector: Animal and Related Themes Findings
2.4. One Health Sector: Environment, Related Themes Findings, and Water Types
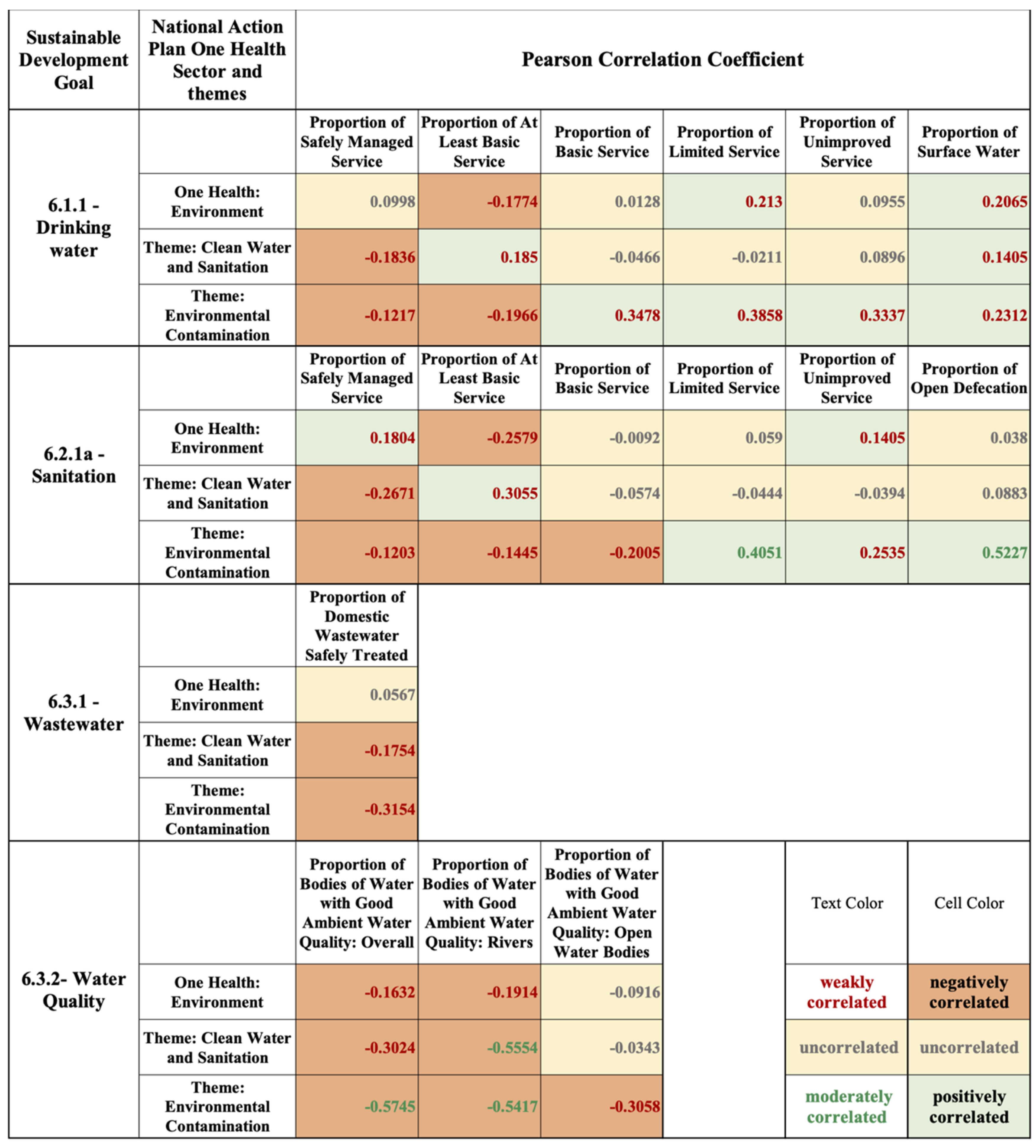
Environmental AMR Stewardship and Sustainable Development Goal 6 Relationships
2.5. Stewardship Pillar-Related Findings
2.6. Realizing an AMR One Health Approach
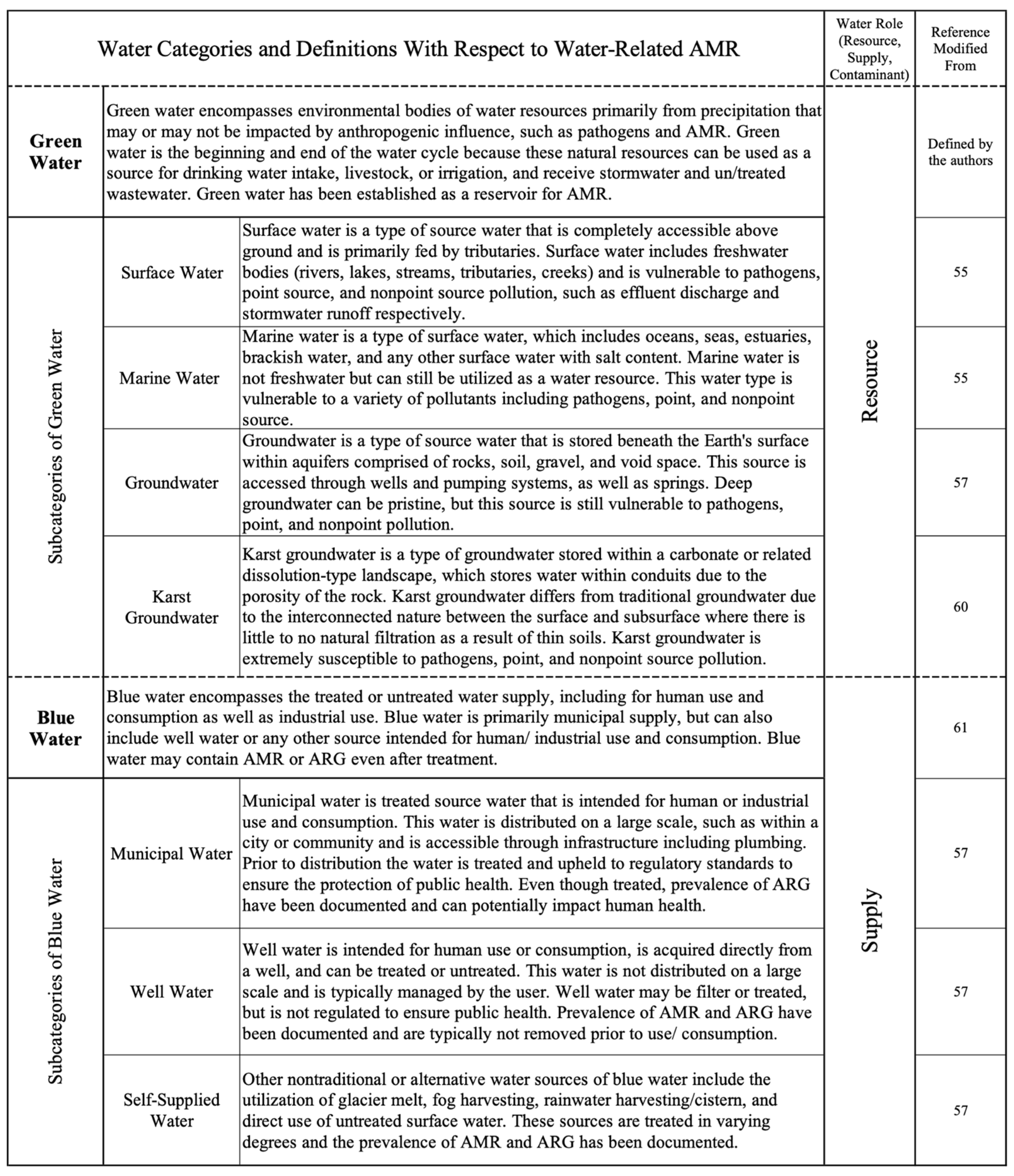
2.7. One Water AMR Stewardship
3. Methods
3.1. One Health-One Water AMR Stewardship Framework: Integrating a Water Stewardship Lens
- human infection prevention and control (IPC);
- clean water and sanitation;
- food safety and security;
- environmental contamination;
- human consumption of antimicrobials;
- use of antimicrobials in animals;
- use of antimicrobials in plants.
- surveillance;
- innovation (discovery and translation research, diagnostics, therapeutics, vaccines, medicine quality, clinical trial networks);
- national action;
- global governance.
- awareness and capability building;
- surveillance;
- funding and financial incentive;
- policy and regulation;
- championing and piloting.
- The Water Resource category indicates any of the ambient or environmental waters (surface, marine, groundwater, karst groundwater) which can be utilized for human, industrial, agricultural, or ecosystem use. Environmental waters refer to the diverse bodies of water present in human environments (natural or man-made), which can support ecosystem biodiversity and services, be utilized as a water supply, and/or receive wastewater discharge. Water resources are from open systems and are not treated but have the potential to be utilized.
- The Water Supply category indicates any water that has been collected from a water resource and is intended for human/industrial use or consumption.
- The Water Contaminant category indicates water that has been used and is not intended as a resource or supply but contributes to both types with and without treatment.
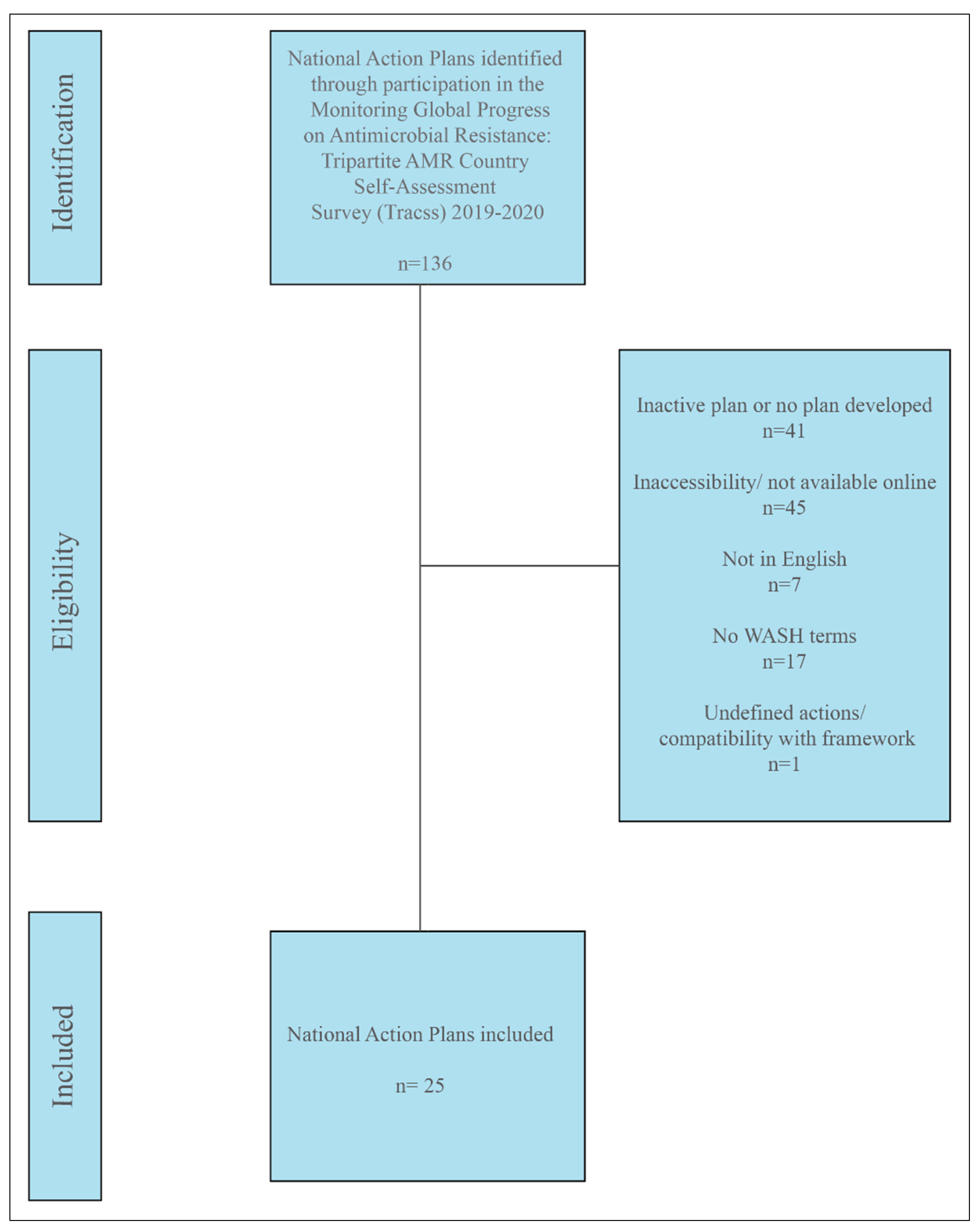
3.2. National Action Plan Case Study Selection
- The country participated in the Monitoring Global Progress on Antimicrobial resistance: 2019–2020 Tripartite AMR Country Self-Assessment Survey (TrACSS), a comprehensive list of actively involved countries;
- The NAP was fully developed and currently implemented. If multiple versions available, only the currently implemented NAP was considered;
- The NAP was published in English;
- The NAP was accessible/available online;
- The NAP included the terms “water”, “sanitation”, or “hygiene” outside of the background/introduction statement.
3.3. Data Analysis
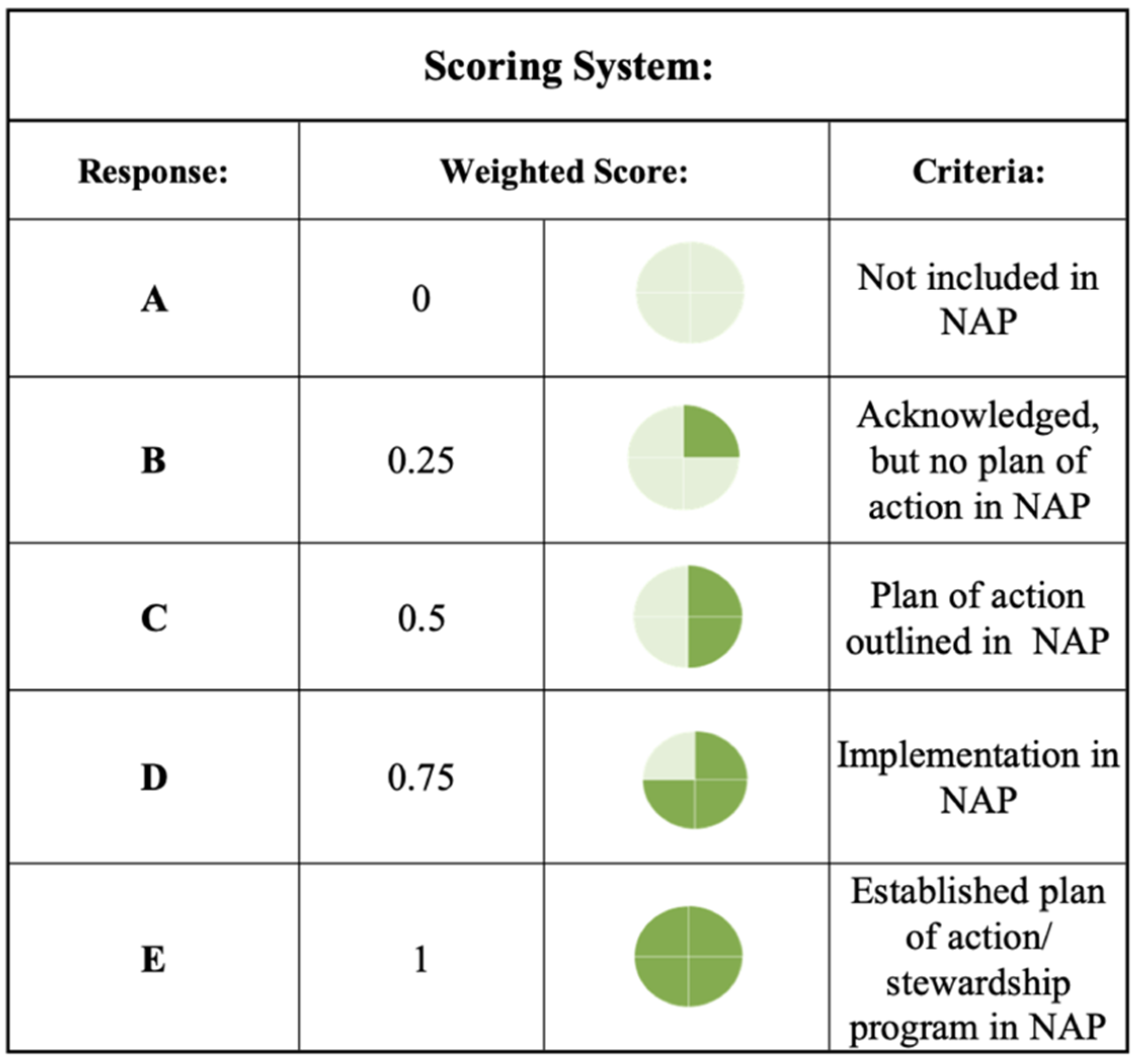
3.3.1. Framework Evaluation and National Action Plan Scorecard
3.3.2. Framework Validation with Sustainable Development Goal Correlation
3.4. Limitations
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Sriram, A.; Kalanxhi, E.; Kapoor, G.; Craig, J.; Balasubramanian, R.; Brar, S.; Criscuolo, N.; Hamilton, A.; Klein, E.; Tseng, K.; et al. The State of the World’s Antibiotics Report in 2021: A Global Analysis of Antimicrobial Resistance and Its Drivers; Center for Disease Dynamics, Economics, and Policy: Washington, DC, USA, 2021. [Google Scholar]
- Zhang, X.X.; Zhang, T.; Fang, H.H.P. Antibiotic Resistance Genes in Water Environment. Appl. Microbiol. Biotechnol. 2009, 82, 397–414. [Google Scholar] [CrossRef]
- Laroche, E.; Petit, F.; Fournier, M.; Pawlak, B. Transport of Antibiotic-Resistant Escherichia Coli in a Public Rural Karst Water Supply. J. Hydrol. 2010, 392, 12–21. [Google Scholar] [CrossRef]
- Flores Ribeiro, A.; Bodilis, J.; Alonso, L.; Buquet, S.; Feuilloley, M.; Dupont, J.-P.; Pawlak, B. Occurrence of Multi-Antibiotic Resistant Pseudomonas Spp. in Drinking Water Produced from Karstic Hydrosystems. Sci. Total Environ. 2014, 490, 370–378. [Google Scholar] [CrossRef] [PubMed]
- Bradford, S.A.; Harvey, R.W. Future Research Needs Involving Pathogens in Groundwater. Hydrogeol. J. 2017, 25, 931–938. [Google Scholar] [CrossRef]
- Szekeres, E.; Chiriac, C.M.; Baricz, A.; Szőke-Nagy, T.; Lung, I.; Soran, M.L.; Rudi, K.; Dragos, N.; Coman, C. Investigating Antibiotics, Antibiotic Resistance Genes, and Microbial Contaminants in Groundwater in Relation to the Proximity of Urban Areas. Environ. Pollut. 2018, 236, 734–744. [Google Scholar] [CrossRef] [PubMed]
- Andrade, L.; Kelly, M.; Hynds, P.; Weatherill, J.; Majury, A.; O’Dwyer, J. Groundwater Resources as a Global Reservoir for Antimicrobial-Resistant Bacteria. Water Res. 2020, 170, 115360. [Google Scholar] [CrossRef] [PubMed]
- Huang, F.; An, Z.; Moran, M.J.; Liu, F. Recognition of Typical Antibiotic Residues in Environmental Media Related to Groundwater in China (2009−2019). J. Hazard. Mater. 2020, 399, 122813. [Google Scholar] [CrossRef] [PubMed]
- Kolda, A.; Mujakić, I.; Perić, L.; Vardić Smrzlić, I.; Kapetanović, D. Microbiological Quality Assessment of Water and Fish from Karst Rivers of the Southeast Black Sea Basin (Croatia), and Antimicrobial Susceptibility of Aeromonas Isolates. Curr. Microbiol. 2020, 77, 2322–2332. [Google Scholar] [CrossRef]
- Tamtam, F.; Mercier, F.; le Bot, B.; Eurin, J.; Tuc Dinh, Q.; Clément, M.; Chevreuil, M. Occurrence and Fate of Antibiotics in the Seine River in Various Hydrological Conditions. Sci. Total Environ. 2008, 393, 84–95. [Google Scholar] [CrossRef] [PubMed]
- Stoll, C.; Sidhu, J.P.S.; Tiehm, A.; Toze, S. Prevalence of Clinically Relevant Antibiotic Resistance Genes in Surface Water Samples Collected from Germany and Australia. Environ. Sci. Technol. 2012, 46, 9716–9726. [Google Scholar] [CrossRef] [PubMed]
- Sanderson, H.; Fricker, C.; Brown, R.S.; Majury, A.; Liss, S.N. Antibiotic Resistance Genes as an Emerging Environmental Contaminant. Environ. Rev. 2016, 24, 205–218. [Google Scholar] [CrossRef]
- Jiang, Y.; Cao, M.; Yuan, D.; Zhang, Y.; He, Q. Hydrogeological Characterization and Environmental Effects of the Deteriorating Urban Karst Groundwater in a Karst Trough Valley: Nanshan, SW China. Hydrogeol. J. 2018, 26, 1487–1497. [Google Scholar] [CrossRef]
- Nadimpalli, M.L.; Marks, S.J.; Montealegre, M.C.; Gilman, R.H.; Pajuelo, M.J.; Saito, M.; Tsukayama, P.; Njenga, S.M.; Kiiru, J.; Swarthout, J.; et al. Urban Informal Settlements as Hotspots of Antimicrobial Resistance and the Need to Curb Environmental Transmission. Nat. Microbiol. 2020, 5, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Devarajan, N.; Laffite, A.; Mulaji, C.K.; Otamonga, J.P.; Mpiana, P.T.; Mubedi, J.I.; Prabakar, K.; Ibelings, B.W.; Poté, J. Occurrence of Antibiotic Resistance Genes and Bacterial Markers in a Tropical River Receiving Hospital and Urban Wastewaters. PLoS ONE 2016, 11, e0149211. [Google Scholar] [CrossRef] [PubMed]
- An, X.L.; Su, J.Q.; Li, B.; Ouyang, W.Y.; Zhao, Y.; Chen, Q.L.; Cui, L.; Chen, H.; Gillings, M.R.; Zhang, T.; et al. Tracking Antibiotic Resistome during Wastewater Treatment Using High Throughput Quantitative PCR. Environ. Int. 2018, 117, 146–153. [Google Scholar] [CrossRef]
- Karkman, A.; Do, T.T.; Walsh, F.; Virta, M.P.J. Antibiotic-Resistance Genes in Waste Water. Trends Microbiol. 2018, 26, 220–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Manaia, C.M.; Rocha, J.; Scaccia, N.; Marano, R.; Radu, E.; Biancullo, F.; Cerqueira, F.; Fortunato, G.; Iakovides, I.C.; Zammit, I.; et al. Antibiotic Resistance in Wastewater Treatment Plants: Tackling the Black Box. Environ. Int. 2018, 115, 312–324. [Google Scholar] [CrossRef]
- Sabri, N.A.; Schmitt, H.; van der Zaan, B.; Gerritsen, H.W.; Zuidema, T.; Rijnaarts, H.H.M.; Langenhoff, A.A.M. Prevalence of Antibiotics and Antibiotic Resistance Genes in a Wastewater Effluent-Receiving River in the Netherlands. J. Environ. Chem. Eng. 2020, 8, 102245. [Google Scholar] [CrossRef]
- Turolla, A.; Cattaneo, M.; Marazzi, F.; Mezzanotte, V.; Antonelli, M. Antibiotic Resistant Bacteria in Urban Sewage: Role of Full-Scale Wastewater Treatment Plants on Environmental Spreading. Chemosphere 2018, 191, 761–769. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO); Food And Agriculture Organization (FAO); World Organization For Animal Health (OIE). Technical Brief on Water, Sanitation, Hygiene and Wastewater Management to Prevent Infections and Reduce The Spread of Antimicrobial Resistance; World Health Organization: Geneva, Switzerland; Food Agriculture Organization: Rome, Italy; World Organization for Animal Health: Paris, France, 2020; ISBN 9789240006416. [Google Scholar]
- White, A.; Hughes, J.M. Critical Importance of a One Health Approach to Antimicrobial Resistance. EcoHealth 2019, 16, 404–409. [Google Scholar] [CrossRef] [Green Version]
- Wellcome Trust. The Global Response to AMR Momentum, Success, and Critical Gaps; Wellcome Trust: London, UK, 2020. [Google Scholar]
- Gaze, W.; Depledge, M. Antimicrobial Resistance: Investigating the Environmental Dimension-Frontiers 2017: Emerging Issues of Environmental Concern. Front. 2017 Emerg. Issues Environ. Concern 2017, 12–22. [Google Scholar]
- Interagency Coordination Group on Antimicrobial Resistance (IACG). No Time to Wait: Securing the Future from Drug-Resistant Infections; World Health Organization: Geneva, Switerland, 2019. [Google Scholar]
- O’Neill, J. Antimicrobial Resistance: Tackling a Crisis for the Health and Wealth of Nations, Review on Antimicrobial Resistance, Chaired by Jim O’Neill, December 2014; Wellcome Trust: London, UK, 2016. [Google Scholar]
- World Health Organization (WHO). Antibiotic Resistance. Available online: https://www.who.int/news-room/fact-sheets/detail/antibiotic-resistance (accessed on 17 September 2021).
- World Health Organization (WHO). Global Action Plan on Antimicrobial Resistance; World Health Organization: Geneva, Switzerland, 2015; ISBN 9789241509763. [Google Scholar]
- Durso, L.M.; Cook, K.L. One Health and Antibiotic Resistance in Agroecosystems. EcoHealth 2019, 16, 414–419. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- United Nations. Seventy-First United Nations General Assembly Political Declaration of the High-Level Meeting of the General Assembly on Antimicrobial Resistance; United Nations: New York, NY, USA, 2016. [Google Scholar]
- Interagency Coordination Group on Antimicrobial Resistance (IACG). AMR Indicators and Their Relevance to the Global Indicator Framework for the SDGs and Targets for the 2030 Agenda for Sustainable Development; World Health Organzation: Geneva, Switzerland, 2018. [Google Scholar]
- Centre for Science and Environment. National Action Plans Antimicrobial Resistance: Need For Greater Focus On Environmental Spread; Centre for Science and Environment: New Delhi, India, 2016. [Google Scholar]
- World Health Organization (WHO); Food And Agriculture Organization (FAO); World Organization For Animal Health (OIE). International Instruments on the Use of Antimicrobials across the Human, Animal and Plant Sectors; World Health Organization: Geneva, Switzerland; Food Agriculture Organization: Rome, Italy; World Organization for Animal Health: Paris, France, 2020. [Google Scholar]
- Singer, A.C.; Shaw, H.; Rhodes, V.; Hart, A. Review of Antimicrobial Resistance in the Environment and Its Relevance to Environmental Regulators. Front. Microbiol. 2016, 7, 1728. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Economic Forum. Antimicrobial Resistance and Water: The Risks and Costs for Economies and Societies Briefing Paper; World Economic Forum: Cologny, Switzerland, 2021. [Google Scholar]
- World Health Organization (WHO); Food And Agriculture Organization (FAO); World Organization For Animal Health (OIE). Monitoring Global Progress on Antimicrobial Resistance: Tripartite AMR Country Self-Assessment Survey (TrACSS) 2019–2020: Global Analysis Report; World Health Organization: Geneva, Switzerland; Food Agriculture Organization: Rome, Italy; World Organization for Animal Health: Paris, France, 2021. [Google Scholar]
- Food And Agriculture Organization (FAO). Thematic Evaluation Series Evaluation of FAO’s Role and Work on Antimicrobial Resistance (AMR); Food Agriculture Organization: Rome, Italy, 2021; ISBN 9789251340745. [Google Scholar]
- World Health Organization (WHO). World Health Organization Countries Classification. Available online: https://www.who.int/countries (accessed on 20 October 2021).
- World Bank. World Bank Country and Lending Groups. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups (accessed on 20 October 2021).
- World Organization for Animal Health (OIE). OIE Standards, Guidelines and Resolution on Antimicrobial Resistance and the Use of Antimicrobial Agents, 2nd ed.; World Organzation for Animal Health: Paris, France, 2020. [Google Scholar]
- Food And Agriculture Organization (FAO); World Organization For Animal Health (OIE). Joint FAO/ WHO Expert Meeting in Collaboration with OIE on Foodborne Antimicrobial Resistance: Role of the Environment, Crops and Biocides: Meeting Report; Food Agriculture Organization: Rome, Italy; World Organization for Animal Health: Paris, France, 2019. [Google Scholar]
- Kurenbach, B.; Marjoshi, D.; Amábile-Cuevas, C.F.; Ferguson, G.C.; Godsoe, W.; Gibson, P.; Heinemann, J.A. Sublethal Exposure to Commercial Formulations of the Herbicides Dicamba, 2,4-Dichlorophenoxyacetic Acid, and Glyphosate Cause Changes in Antibiotic Susceptibility in Escherichia Coli and Salmonella Enterica Serovar Typhimurium. Microbiology 2015, 6, e00009-15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kurenbach, B.; Gibson, P.S.; Hill, A.M.; Bitzer, A.S.; Silby, M.W.; Godsoe, W.; Heinemann, J.A. Herbicide Ingredients Change Salmonella Enterica Sv. Typhimurium and Escherichia Coli Antibiotic Responses. Microbiology 2017, 163, 1791. [Google Scholar] [CrossRef]
- Kurenbach, B.; Hill, A.M.; Godsoe, W.; van Hamelsveld, S.; Heinemann, J.A. Agrichemicals and Antibiotics in Combination Increase Antibiotic Resistance Evolution. PeerJ 2018, 6, e5801. [Google Scholar] [CrossRef] [Green Version]
- Interagency Coordination Group on Antimicrobial Resistance (IACG). AMR Framework for Action Supported by the IACG, Working Document; World Health Organzation: Geneva, Switzerland, 2017. [Google Scholar]
- Guerra, R. Tripartite Plus Recent Update and Memorandum of Understanding on Antimicrobial Resistance. In Proceedings of the IACG Information Session, Geneva, Switzerland, 1 October 2018. [Google Scholar]
- Wuijts, S.; van den Berg, H.H.J.L.; Miller, J.; Abebe, L.; Sobsey, M.; Andremont, A.; Medlicott, K.O.; van Passel, M.W.J.; de Roda Husman, A.M. Towards a Research Agenda for Water, Sanitation and Antimicrobial Resistance. J. Water Health 2017, 15, 175–184. [Google Scholar] [CrossRef] [Green Version]
- Sano, D.; Wester, A.L.; Schmitt, H.; Amarasiri, M.; Kirby, A.; Medlicott, K.; de Roda Husman, A.M. Updated Research Agenda for Water, Sanitation and Antimicrobial Resistance. J. Water Health 2020, 18, 858–866. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Antimicrobial Resistance: Global Report on Surveillance 2014; World Health Organzation: Geneva, Switzerland, 2016. [Google Scholar]
- World Health Organization (WHO). Global Antimicrobial Resistance and Use Surveillance System (GLASS) Report; World Health Organzation: Geneva, Switzerland, 2020. [Google Scholar]
- Food And Agriculture Organization (FAO); World Organization For Animal Health (OIE); World Health Organization (WHO). Antimicrobial Resistance Multi-Partner Trust Fund Forging Tripartite Collaboration for Urgent Global and Country Action against Antimicrobial Resistance (AMR) Annual Progress Report 2020; Food Agriculture Organization: Rome, Italy; World Organization for Animal Health: Paris, France; World Health Organization: Geneva, Switzerland, 2020. [Google Scholar]
- Xi, C.; Zhang, Y.; Marrs, C.F.; Ye, W.; Simon, C.; Foxman, B.; Nriagu, J. Prevalence of Antibiotic Resistance in Drinking Water Treatment and Distribution Systems. Appl. Environ. Microbiol. 2009, 75, 5714–5718. [Google Scholar] [CrossRef] [Green Version]
- United Nations (UN). The United Nations World Water Development Report 2021: Valuing Water; UN Water: Geneva, Switzerland, 2021. [Google Scholar]
- Bürgmann, H.; Frigon, D.; Gaze, W.H.; Manaia, C.M.; Pruden, A.; Singer, A.C.; Smets, B.F.; Zhang, T. Water and Sanitation: An Essential Battlefront in the War on Antimicrobial Resistance. FEMS Microbiol. Ecol. 2018, 94, fiy101. [Google Scholar] [CrossRef]
- National Geographic Society. Surface Water. Available online: https://www.nationalgeographic.org/encyclopedia/surface-water/ (accessed on 17 September 2021).
- USDA: Natural Resources Conservation Service Conservation Practice Standard: Waste Treatment Code 629. Available online: ttps://www.blogs.nrcs.usda.gov/Internet/FSE_DOCUMENTS/16/nrcseprd1499262.pdf (accessed on 17 September 2021).
- USGS. Dictionary of Water Terms. Available online: https://www.usgs.gov/special-topic/water-science-school/science/dictionary-water-terms?qt-science_center_objects=0#G (accessed on 17 September 2021).
- USGS. Wastewater Treatment Water Use. Available online: https://www.usgs.gov/special-topic/water-science-school/science/wastewater-treatment-water-use?qt-science_center_objects=0#qt-science_center_objects (accessed on 17 September 2021).
- USGS. Pharmaceuticals in Water. Available online: https://www.usgs.gov/special-topic/water-science-school/science/pharmaceuticals-water?qt-science_center_objects=0#qt-science_center_objects (accessed on 17 September 2021).
- Palmer, A.N. Cave Geology and Speleogenesis over the Past 65 Years: Role of The National Speleological Society in Advancing the Science. J. Cave Karst Stud. 2007, 69, 3–12. [Google Scholar]
- Falkenmark, M.; Rockström, J. The New Blue and Green Water Paradigm: Breaking New Ground for Water Resources Planning and Management. J. Water Resour. Plan. Manag. 2006, 132, 129–132. [Google Scholar] [CrossRef]
- World Health Organization (WHO). Safe Management of Wastes from Health-Care Activities, 2nd ed.; World Health Organzation: Geneva, Switzerland, 2016. [Google Scholar]
- Fonseca, L.M.; Domingues, J.P.; Dima, A.M. Mapping the Sustainable Development Goals Relationships. Sustainability 2020, 12, 3359. [Google Scholar] [CrossRef] [Green Version]
- United Nations Environment Programme. Measuring Progress: Environment and the SDGs; United Nations Enviroment Programme: Nairobi, Kenya, 2021. [Google Scholar]
- de Neve, J.E.; Sachs, J.D. The SDGs and Human Well-Being: A Global Analysis of Synergies, Trade-Offs, and Regional Differences. Sci. Rep. 2020, 10, 15113. [Google Scholar] [CrossRef] [PubMed]
- Rice, J.A. Mathematical Statistics and Data Analysis, 3rd ed.; Cenegage Learning: Boston, MA, USA, 2007; Volume 72. [Google Scholar]
- United Nations (UN). Water Indicator 6.1.1—Drinking Water. Available online: https://www.sdg6data.org/indicator/6.1.1 (accessed on 21 September 2021).
- United Nations (UN). Water Indicator 6.2.1a—Sanitation. Available online: https://www.sdg6data.org/indicator/6.2.1a (accessed on 21 September 2021).
- United Nations (UN). Water Indicator 6.3.1—Wastewater Treatment. Available online: https://www.sdg6data.org/indicator/6.3.1 (accessed on 21 September 2021).
- United Nations (UN). Water Indicator 6.3.2—Water Quality. Available online: https://www.sdg6data.org/indicator/6.3.2 (accessed on 21 September 2021).
- Weisberg, S. Applied Linear Regression, 4th ed.; Wiley: Hoboken, NJ, USA, 2005. [Google Scholar]
- Samreen; Ahmad, I.; Malak, H.A.; Abulreesh, H.H. Environmental Antimicrobial Resistance and Its Drivers: A Potential Threat to Public Health. J. Glob. Antimicrob. Resist. 2021, 27, 101–111. [Google Scholar] [CrossRef] [PubMed]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kaiser, R.A.; Taing, L.; Bhatia, H. Antimicrobial Resistance and Environmental Health: A Water Stewardship Framework for Global and National Action. Antibiotics 2022, 11, 63. https://doi.org/10.3390/antibiotics11010063
Kaiser RA, Taing L, Bhatia H. Antimicrobial Resistance and Environmental Health: A Water Stewardship Framework for Global and National Action. Antibiotics. 2022; 11(1):63. https://doi.org/10.3390/antibiotics11010063
Chicago/Turabian StyleKaiser, Rachel A., Lina Taing, and Himesh Bhatia. 2022. "Antimicrobial Resistance and Environmental Health: A Water Stewardship Framework for Global and National Action" Antibiotics 11, no. 1: 63. https://doi.org/10.3390/antibiotics11010063
APA StyleKaiser, R. A., Taing, L., & Bhatia, H. (2022). Antimicrobial Resistance and Environmental Health: A Water Stewardship Framework for Global and National Action. Antibiotics, 11(1), 63. https://doi.org/10.3390/antibiotics11010063





