Abstract
Multi-drug-resistant (MDR) organisms pose a global threat to modern medicine, which has grown as a result of irrational antibiotic use and misuse. This study aimed to assess general public knowledge in Jordan and awareness of antibiotics and antibiotic resistance during the COVID-19 pandemic. A cross-sectional study was carried out utilizing the WHO multicountry public awareness survey. The study population was composed mainly of social media users, and a total of 1213 participants completed the online survey. According to the findings, more than half of the participants were well versed in antibiotic use and resistance. Those with adequate health literacy were found to better understand antibiotics (OR = 1.37, p = 0.017) and antibiotic resistance (OR = 1.46, p = 0.003). The vast majority (88.5%) recognized at least one antibiotic resistance term; however, 53.2% believed that antibiotic resistance is a problem in other nations. The participants in this study reported using antibiotics incorrectly, believing that they were treating sore throats, colds, and flu. The participants were well aware of antibiotic resistance solutions and their consequences on health. Age, education, health literacy, and antibiotic knowledge were found to be substantially (p < 0.05) associated with greater awareness of antibiotic resistance. The findings highlight the need for antimicrobial resistance education campaigns, health literacy, and antibiotic stewardship initiatives.
1. Introduction
The emergence of multi-drug-resistant (MDR) organisms has posed a global challenge to modern medicine since the discovery of antibiotics. Antibiotic resistance occurs naturally, but unsustainable antibiotic use and misuse have expedited the process, putting humanity’s well-being in danger [1,2,3]. An estimated 700,000 people die annually as a result of antimicrobial resistance (AMR), which is defined as bacteria surviving under the influence of antimicrobial agents [4,5]. Healthcare systems and the global economy have been challenged since COVID-19 was declared a global pandemic. For the clinical management of COVID-19, increased use of empirical antibiotics in patients with respiratory symptoms has been reported [6,7,8]. These practices have the potential to amplify AMR and MDR pathogens [9,10,11,12]. Studies have associated higher education with a better understanding of antibiotic resistance [13,14]. Antibiotic resistance awareness can be considerably increased by raising people’s knowledge and health literacy, which will have a positive impact on actions such as irrational antibiotic dispensing and self-medication [15,16]. Health literacy is defined by the World Health Organization (WHO) as the ability to make effective health decisions in order to increase human health [17]. According to prior research, people who live in cities have higher levels of health literacy than those who live in rural areas [18,19]. Similarly, an Egyptian cross-sectional investigation linked antibiotic resistance awareness to health literacy. According to the study, 92% of people were unaware of antibiotic resistance, and 40% had used antibiotics without a prescription in the previous month [20]. Community pharmacies are the most common form of public primary care in Jordan, providing prescription and nonprescription medications for a wide range of conditions. Despite Jordanian regulations prohibiting the dispensing of antibiotics without a prescription, studies found that more than 40% of participants purchased antibiotics from community pharmacies without a prescription [21,22,23,24]. The majority of participants who self-medicate obtained antibiotics and sought medical advice mostly from pharmacies before contacting prescribing physicians. Previous research found that more than half of Jordanians improperly use antibiotics to treat common colds and coughs, sore throats, and influenza [21,22,24]. As a result, the lack of awareness and the broad availability of antibiotics lead to an increase in inappropriate self-medication and, as a result, antibiotic misuse among Jordanians. In a cross-sectional study conducted in an outpatient hospital environment in Jordan, Muflih et al. (2020) reported that 74.2% of patients self-medicate with antibiotics. The study found a significant association between overall health literacy and inappropriate self-medication, highlighting the importance of raising awareness and improving health literacy [25]. According to studies, the majority of interviewees reported self-medicating with antibiotics and considered it a safe and acceptable practice [26,27,28]. In addition, the increased use of antibiotics in outpatient settings could be related to lack of awareness and external patient pressure [29]. Of note, a key driver to rising antimicrobial resistance, according to Laxminarayan et al. (2013) and Pereko et al. (2015) [30,31], is the misuse of antibiotics for self-limiting diseases, such as cold and influenza, sore throat, and diarrhea. Both incorrect dosing and the use of antibiotics when they are not required significantly contribute to the rising problem of antibiotic resistance [32,33]. Despite the fact that the world’s attention is currently focused on the global COVID-19 epidemic, the AMR issue should also be prioritized [34], and research studies examining public perceptions of AMR during the present pandemic are needed. Therefore, this process was undertaken in Jordan during the COVID-19 pandemic to assess the general public’s knowledge and awareness regarding antibiotics and antibiotic resistance.
2. Results
2.1. Characteristics of Study Participants
The study included 1213 participants, the majority of whom were females (n = 856; 70.6%). Almost one-third of the participants (35.4%) were between the ages of 25 and 34, and the vast majority lived in cities (61.1%). Around half of the participants (54.9%) were educated with a bachelor’s degree, and less than one-third (28.3%) were employed in the medical field. Additional sociodemographic factors are listed in Table 1.

Table 1.
Percentage distribution of selected demographic variables of the participants in the sample (n = 1213).
2.2. Participants’ Health Literacy Levels
According to the Single Item Literacy Screener (SILS), when asked “how often do you ask someone for help reading instructions and leaflets from a doctor or pharmacy”, the participants said “1 = always” (n = 28, 2.3%), “2 = most of the time” (n = 94, 7.7%), “3 = sometimes” (n = 332, 27.4%), “4 = rarely” (n = 403, 33.2%), and “5 = never” (n = 356, 29.3%). The findings of this study indicated that nearly two-thirds (62.6%) of the participants possessed adequate health literacy, while 37.4% had inadequate health literacy. With the exception of education level, health literacy levels were comparable across groups. Consistent with previous research [15,31], this study revealed that people with a postgraduate degree were more likely than those with lower education levels to report better health literacy, which may represent the influence of education on participants’ exposure to and evaluation of health information essential to maintain their health.
2.3. Knowledge of Antibiotic Use among Participants
According to the findings, 81.5% correctly stated that patients should discontinue taking prescription antibiotics after taking them as prescribed. However, 17.1% believed that antibiotics should be discontinued after they felt better. Despite the fact that antibiotics can be used to treat similar conditions, 82.2% of the respondents felt that using antibiotics given to them by a friend or family member is unacceptable. Furthermore, 41% believed that it was appropriate to obtain or request the same medications from a doctor in order to treat the same symptoms they had previously encountered. When asked about particular infections that might be treated with antibiotics, the majority of the participants correctly identified only two conditions: bladder/urinary tract infections (75.4%) and skin/wound infections (66.4%). However, less than 14% properly classified gonorrhea and malaria as antibiotic-susceptible infections. According to 43.2% and 84.2% of the respondents, antibiotics can be used to treat colds/flu and sore throats, respectively (Table 2).

Table 2.
Knowledge of antibiotic use among participants.
2.4. Knowledge of Antibiotic Resistance among Participants
The majority of the participants (85.8%) incorrectly identified the following statement as true: “Antibiotic resistance occurs when your body becomes resistant to antibiotics and they no longer work as well,” and over half (53.2%) wrongly believed antibiotic resistance is a concern in other nations but not in Jordan. Furthermore, 57.2% incorrectly believed that antibiotic resistance is limited to people who routinely take antibiotics, whereas only 37% believed that resistant bacteria can spread from person to person. Furthermore, more than half of those surveyed correctly identified that many infections are becoming increasingly resistant to antibiotic treatment, and those antibiotic-resistant infectious agents could make medical procedures far more dangerous. The majority of the participants were familiar with the following terms: “antibiotic resistance”, “superbugs”, “drug resistance”, and “antibiotic-resistant bacteria”, while 11.5% of those surveyed had never heard of any of these terms (Table 3).

Table 3.
Knowledge of antibiotic resistance among participants.
2.5. Pattern of Antibiotic Usage in Relation to Knowledge of Antibiotics and Antibiotic Resistance
The survey results identified a correlation between individuals’ antibiotic consumption patterns and their overall knowledge of antibiotics and antibiotic resistance. Respondents who reported using antibiotics in the previous 6 months or longer had a higher likelihood of having adequate antibiotic knowledge (adjusted OR = 1.74, 95% CI: 1.294–2.35) and adequate antibiotic resistance knowledge (adjusted OR = 1.42, 95% CI: 1.06–1.91) than those who used antibiotics in the previous month; estimates for greater than 6 months are presented in Table 4. Further, respondents who reported receiving antibiotics through a healthcare provider’s prescription were more likely to have adequate knowledge of antibiotics (adjusted OR = 2.01, 95% CI: 1.57–2.58) and adequate knowledge of antibiotic resistance (adjusted OR = 1.31, 95% CI: 1.03–1.68) than those who self-medicate. Respondents who received healthcare provider counseling and instructions were more likely to have adequate antibiotic knowledge (adjusted OR = 1.98, 95% CI: 1.53–2.56) than those who did not (Table 4).

Table 4.
Logistic regression of pattern of antibiotic usage associated with adequate knowledge of antibiotics and antibiotic resistance.
2.6. Factors Associated with Participants’ Knowledge of Antibiotics and Antibiotic Resistance
After identifying factors (such as age, gender, residence, family structure, education level, employment status, family monthly income, health insurance, and infection with COVID-19) associated with adequate antibiotic knowledge and antibiotic resistance using univariate logistic regression, variables with p < 0.25 were included in the multiple logistic regression model for further analysis. The findings showed that younger and female respondents and those who resided in cities were more likely to have adequate knowledge about antibiotics than their counterparts. Respondents working in the medical field (adjusted OR = 3.08, 95% CI: 2.13–4.44, and adjusted OR = 2.78, 95% CI: 2.00–3.87) were also more likely to have adequate knowledge of antibiotics and antibiotic resistance, respectively. Furthermore, participants with health insurance (adjusted OR = 1.38, 95% CI: 1.03–1.85) were more likely to be knowledgeable about antibiotic resistance than those with no health insurance (Table 5). Participants who did not get antibiotics (adjusted OR = 0.31, 95% CI: 0.22–0.45) to treat COVID-19 and those who received COVID-19 vaccination (adjusted OR = 1.62, 95% CI: 1.02–2.18) both showed a high degree of antibiotic knowledge. Participants with appropriate health literacy were more likely to have an adequate understanding of antibiotics (adjusted OR = 1.37, 95% CI: 1.06–1.77) and antibiotic resistance (adjusted OR = 1.46, 95% CI: 1.14–1.89) than their counterparts. Family structure, education level, and family monthly income were not correlated to an adequate degree of knowledge on antibiotics and antibiotic resistance (see Table 5).

Table 5.
Multiple logistic regression of sociodemographic factors and levels of health literacy associated with participants’ knowledge of antibiotics and antibiotic resistance.
2.7. Level of Awareness of Possible Solutions to the Problem of Antibiotic Resistance
The respondents were asked to rate their awareness of approaches to addressing the problem of antibiotic resistance. The findings revealed that the participants were well aware of the resistance issue (M = 3.91 out of 5, SD = 0.97). The majority of the respondents agreed or strongly agreed that practically all antibiotic-resistance-fighting measures, such as parents ensuring that all of their children’s vaccines are up-to-date (82.9%) and doctors giving antibiotics only when required (82%), were essential. However, the least agreed-upon advice was that farmers use fewer antibiotics in food-producing animals and that people should not stockpile antibiotics to use later for other diseases (Figure 1). The findings of the t-test demonstrated that levels of health literacy, antibiotic knowledge, and antibiotic resistance knowledge all had a significant effect on overall awareness of potential antibiotic resistance solutions. The results of one-way ANOVA also demonstrated that age and education level had a significant effect on total awareness score (Table 6). The findings of post hoc Tukey tests showed that individuals from the age groups 18 to 44 were much more aware of potential antibiotic resistance solutions than those aged 45 and older. The postgraduate education group participants were more aware than the other groups.
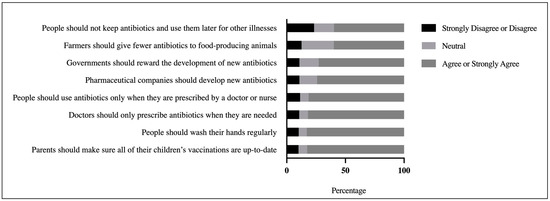
Figure 1.
Participants’ awareness of possible solutions to the problem of antibiotic resistance.

Table 6.
Participants’ awareness and perspectives concerning antibiotics in relation to variables of interest.
2.8. Participants’ Perspectives on the Scope of the Antibiotic Resistance Problem
According to the findings, the participants’ general perceptions of the magnitude of the antibiotic resistance problem were moderate (M = 3.51 out of 5, SD = 0.73). The majority (76.8%) agreed or strongly agreed that everyone must bear responsibility for safely taking antibiotics. In addition, 62.6% were concerned about the impact of antibiotic resistance on their own and their family’s health. Despite these beliefs, however, 53% of the respondents asserted that they are not in danger of acquiring an antibiotic-resistant infection if they adhere to their antibiotic regimen. There is substantial uncertainty over whether the issue of antibiotic resistance necessitates global collaboration. As illustrated in Figure 2, one-third or more of the respondents were undecided about whether antibiotic resistance is one of the world’s most serious concerns (33.2%), and 40.6% were undecided about whether medical specialists will address the problem of antibiotic resistance before it becomes too serious. The t-test results revealed that degrees of health literacy, antibiotic knowledge, and antibiotic resistance knowledge all had a significant effect on the overall perspective score (see Table 6).
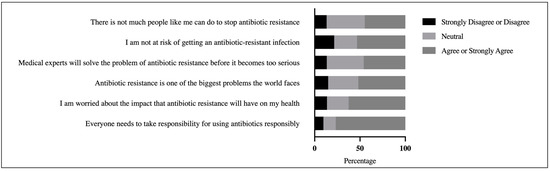
Figure 2.
Participants’ perspectives on the scope of the antibiotic resistance problem.
3. Discussion
3.1. Health Literacy
The current study investigated the levels of health literacy in Jordanian communities in relation to their knowledge and awareness of antibiotics and antibiotic resistance. Almost two-thirds (62.6%) of those surveyed had adequate health literacy, which is slightly higher than the 57.2% previously reported in a cross-sectional study on the impact of health literacy on self-medication practice [25]. In line with earlier research [16,35], the findings of this study showed that health literacy levels were comparable across groups, with the exception of the education levels, which had a substantial effect on health literacy. This finding implies that higher education levels provide more broad exposure to antibiotic and health-behavior-related information. According to the findings of this study, 721 (59.4%) and 631 (52%) of the participants had adequate knowledge of antibiotic use and antibiotic resistance, respectively. Knowledge scores were significantly higher for those with adequate health literacy than those with inadequate health literacy (OR = 1.37 (1.05–1.77), p = 0.017; OR = 1.46 (1.14–1.89), p = 0.003), suggesting that overall health literacy is a key focus that crosses all disciplines.
3.2. Knowledge of Antibiotics and Antibiotic Resistance
According to the findings of this survey, more than half of the participants have adequate understanding of antibiotics and antibiotic resistance. Levels of knowledge differ significantly based on the participants’ age, gender, employment status, insurance, health literacy, and infection with COVID-19. The term “antibiotic resistance” has been heard by almost three-quarters of the participants, suggesting that antibiotic resistance is a frequently discussed issue that the vast majority of Jordanians are aware of. Similar findings were reported for all the participating countries in the WHO multicountry public awareness survey [2]. The participants in this study, however, frequently mischaracterized antibiotic resistance, such as “antibiotic resistance occurs when your body becomes resistant to antibiotics and they no longer work as well”, “antibiotic resistance is an issue in other countries but not in my country”, and “antibiotic resistance is only a problem for people who take antibiotics on a regular basis”. Acquainting patients with the fact that antibiotic resistance is attributed to bacteria’s capacity to overcome the action of therapeutic agents and that it is a global issue making everyone susceptible to antibiotic-resistant, difficult-to-treat infections may enhance social contributions to the implementation of antibiotic resistance prevention strategies. Previous studies reported similar results [2,20,36]. The findings of this study revealed that more than four-fifths (83%) of the participants made wrong assumptions regarding whether antibiotics heal sore throats, whereas less than half (43%) were incorrect in their assertion that antibiotics can be used to treat colds and the flu. This might be attributed to their lack of knowledge about the appropriate use of antibiotics as well as their lack of awareness regarding available alternatives that might help alleviate the symptoms of viral infections. Pereko et al. (2015) reported similar findings [31]. In contrast to the findings of Mostafa et al. (2021) [20], smaller percentages wrongly believed that antibiotics treat fever (24.6%) and diarrhea (16.7%).
The findings also revealed that more than two-thirds of the patients correctly believed that antibiotics are effective in treating urinary tract infections and skin infections; similar findings were observed by the WHO multicountry survey [2]. However, most participants were unaware that antibiotics can be used to treat gonorrhea and measles. These data suggest that the general population has conflicting understandings of antibiotic use. Solving these knowledge conflicts by promoting patient-centered interaction and developing antibiotic resistance education may help to combat antibiotic resistance and enhance public health by driving individuals to seek more accurate health-related information.
3.2.1. Factors Associated with Participants’ Knowledge of Antibiotics and Antibiotic Resistance
According to the findings of this study, lack of knowledge of antibiotic use was more prevalent among older and male participants, as well as those who resided in rural areas and those who were unemployed or worked in nonmedical occupations. The findings suggest that older persons have poor comprehension of antibiotics. Similar findings were reported by other countries [37,38,39]. In contrast to the findings of Kong et al. (2019) [37], this study implies that men and women are disproportionately concerned about antibiotics. This could be because women are more likely to use primary healthcare services, are more experienced with antibiotic treatment, and take greater responsibility for their family’s health [40,41]. The findings mirror those of a recent study that found that rural residents possessed less knowledge about antibiotics than those who resided in cities [19]. This could be due to lack of access to healthcare and health insurance coverage. This study’s findings are in line with those of Haque et al. (2019), supporting the fact that working in medical disciplines is strongly associated with increased knowledge and learning capacities regarding antibiotic effectiveness and proper antibiotic use [26]. This study’s findings indicate that medical field participants have access to antibiotic courses at their institutions. While physicians should graduate from medical schools with the knowledge necessary to make sound decisions about antibiotic use, this issue should be given equal weight in nonmedical field studies all across Jordan. Comparisons among healthcare workers warrant further evaluations in future studies.
Further, the participants in this study who did not have health insurance had lack of knowledge about antibiotic resistance, which could imply that they are less likely to learn more about antibiotics and antibiotic resistance and are more likely to engage in less responsible self-medication as a result of economic restrictions. The incorrect and excessive use of broad-spectrum antibiotics in COVID-19 patients has been documented to outnumber the prevalence of bacterial coinfections and secondary illnesses [6,7,8]. However, this study’s findings indicate that individuals who did not get antibiotics to avoid the COVID-19 infection and those who received COVID-19 vaccine have a greater level of knowledge about antibiotics. This suggests that the respondents are aware of COVID-19-related information that was widely disseminated to the general population and have a higher degree of health literacy. Further, the participants with low health literacy were also shown to have lack of knowledge about antibiotics and antibiotic resistance, which may be a result of their inability to evaluate information received from healthcare practitioners. Similar findings were observed in Egypt, where low levels of antibiotic knowledge and awareness of antibiotic resistance were connected to low levels of health literacy [20].
3.2.2. The Use of Antibiotics
The percentage of the respondents in this study who reported using antibiotics in the previous month, in the previous 6 months, and a year ago (28.4%, 30.1%, and 9.8%, respectively) was lower than that of the general public in low-income countries (e.g., Egypt, Sudan, and Indonesia), as reported by a WHO multicountry survey [2]. In comparison with prior studies conducted in Jordan [25,42], the current study’s finding of a general decrease in antibiotic use can be attributed to the increased level of knowledge of antibiotics and antibiotic resistance, stringent public health measures (e.g., promoting social distancing measures), and increasing antibiotic use and resistance awareness programs. Additionally, as a result of public health prevention initiatives and the availability of telemedicine, people are attending outpatient clinics less frequently [43]. Additional research is needed to determine the importance of antibiotic stewardship interventions, particularly those that involve remote monitoring, in order to optimize antibiotic use and infection treatment appropriateness.
Although a lower percentage of participants (30%) in this study reported inappropriate self-medication practices compared with a previous household study in Jordan (39.5%) [23], they demonstrated lack of understanding about antibiotic use and resistance compared with those who obtained antibiotics via a doctor’s or nurse’s prescription. These findings underscore the importance of conducting additional studies into the reasons for self-medication in order to increase public awareness and guide practice among the general public and healthcare professionals. Consistent with previous research, approximately half of those surveyed in this study indicated that pharmacies are their primary source of self-medicated antibiotics [13,26,44]. While pharmacists are responsible for promoting safe and cost-effective drug use, the study findings support previous research emphasizing the pharmacist’s role in referring patients with infectious diseases to physicians, advocating for prudent antibiotic use, and preventing antimicrobial resistance [13,35,45].
3.2.3. Implications for Education Campaigns
In light of the current study’s findings and those of previous studies [4,30,46,47], ongoing educational activities should emphasize the importance of improving health literacy and information-seeking behavior to enhance health outcomes and to educate participants about the proper use of antibiotics, which may help curb the spread of antibiotic resistance. To increase public awareness of antibiotic resistance, efforts and educational initiatives should be directed toward the elderly, uninsured, those who self-medicate with antibiotics, and those with low health literacy. Additionally, a community-based health education program targeting various sections of the community would be the most effective strategy to educate people about judicious antibiotic usage.
3.3. Participants’ Awareness of Possible Solutions to the Problem of Antibiotic Resistance
Previous research revealed that the Jordanian community has a general lack of information and awareness about antibiotic use and antibiotic resistance [42]. The current study, on the other hand, found that the participants were well aware of potential solutions to the problem of antibiotic resistance. These disparities may be explained by a high level of health literacy, as well as the effectiveness of regular media messaging against antibiotic use during COVID-19, which may have served to expand knowledge. The participants in this study agreed or strongly agreed that physicians should prescribe antibiotics only when they are deemed necessary, and people should use antibiotics only when they are prescribed by a doctor or nurse, which was also reported in previous studies from other countries regarding overuse, underuse, and inappropriate use of antibiotics [2,48]. The positive attitude among the participants suggests better knowledge of antibiotic use and resistance. However, there was some confusion regarding some items, such as “Farmers should give fewer antibiotics to food-producing animals” and “People should not keep antibiotics and use them later for other illnesses”, which were the least agreed upon by the participants to address the problem of antibiotic resistance. Previous research yielded similar results [2,20]. The findings of this study propose instant solutions and various techniques to improve antibiotic stewardship in various livestock sectors. While boosting understanding regarding antibiotic use and resistance may be beneficial in raising awareness, methods such as employing nonantibiotic treatments, such as herbs and probiotics, or vaccinating herds may have a positive impact on limiting antibiotic resistance [49,50]. In line with earlier findings [2,20], about two-thirds of the participants in this study believed that the problem of antibiotic resistance is more likely to be avoided if many investments were dedicated to antibiotic research and development by the government and pharmaceutical companies (see Figure 1). While governments and pharmaceutical companies should develop novel approaches and interventions to address antimicrobial resistance, increasing public engagement and awareness to promote rational drug use could be critical in combating antimicrobial resistance in humans and animals. Although incorrect dosing and the use of antibiotics when they are not needed both contribute to the rising problem of antibiotic resistance [32,33], nearly half of the participants expressed misconceptions, believing that antibiotic-resistant infections could be avoided by taking antibiotics as prescribed, which may reflect lack of understanding of antibiotic resistance.
The participants’ awareness of potential solutions to the problem of antibiotic resistance differed significantly across age groups, education levels, health literacy levels, levels of knowledge of antibiotics, and levels of knowledge of antibiotic resistance. The findings could be due to the fact that younger participants and those with greater levels of education had more information about antibiotic resistance than their counterparts [13,14]. In line with previous studies [15,16], this study concludes that raising people’s knowledge and health literacy can significantly improve their awareness of antibiotic resistance, which can have an impact on practices such as irrational dispensing and self-medication. The lack of connections between gender and levels of awareness could indicate that individuals of both genders have similar views about the problem of antibiotic resistance. Similarly, the lack of any connections between the region of residence, work status, and awareness levels may signal that people have received sufficient messages aimed at increasing awareness and are paying close attention to the problem of antibiotic resistance.
3.4. Participants’ Perspectives on the Scope of the Antibiotic Resistance Problem
When asked about their opinions on antibiotic resistance and how it might affect their health, almost 63% were worried about the impact of antibiotic resistance on their health and their family’s health; similar results were reported in previous studies [2,20]. These findings may reflect a higher level of antibiotic awareness among the general public, as well as individual responsibility in the fight against antibiotic resistance. However, a study conducted in Malaysia reported a much lower percentage (48.5%) for perceived impact of antibiotic resistance on the participants and their family. Contrary to findings reported by previous studies [2,20,51,52], an intriguing research finding in this study was that only 52% of the participants recognized antibiotic resistance as one of the greatest challenges the world faces today. The main reason could be attributed to lack of knowledge as only 46.8% of the participants believed that antibiotic resistance is an issue that is not limited to Jordan but also concerns other countries. Thus, raising public knowledge and awareness through social and mass media could help in recognizing antibiotic resistance and the perceived threat it poses [53]. In this study, the participants with higher levels of knowledge and health literacy had better perspectives on the breadth of the antibiotic resistance problem than those with lower levels of knowledge and health literacy. This finding could be attributable to the effect of health information on favorable health-related behaviors, which could have a positive impact on responsible antibiotic use. Furthermore, participants with higher health literacy may be more aware of the potential negative repercussions associated with incorrect antibiotic usage and inaccurate diagnosis as reported recently elsewhere [16,54].
3.5. Limitations and Strengths
A convenience sampling method was applied to select participants based on their availability and willingness to participate in the online survey. However, this study’s findings have a number of limitations. Recruiting participants through social media is susceptible to a nonresponse bias due to the digital divide-unequal access to the Internet and disparities in usage style and frequency of social media; thus, the characteristics of nonresponders might differ from those of responders [55,56]; however, the survey link has been repeatedly posted and tagged to friends on Facebook to maximize the response rate, thus minimizing the possibility of nonresponse bias. There was an over-representation of younger respondents with more females and more unemployment that did not perfectly represent the target population according to Jordan’s census administrative records [57]. Therefore, the findings of this study could fall short in representativeness. Moreover, participants who might be concerned with the antibiotic topic could be more likely to take the survey, which might lead to self-selection [58]. This study defined health literacy as the perceived ability to read health-related information, as measured by the Single Item Literacy Screener (SILS), which could not detect literacy difficulties in those with modest reading abilities, and it is subject to false negative replies [59]. Moreover, the impact of chronic diseases on escalating antibiotic consumption was not a focus of this study. The study’s strength is that it involved a large number of participants, which enables the assessment of the relationship between knowledge, awareness, and antibiotic use in relation to a variety of sociodemographic factors. Given the scarcity of studies in Jordan on this topic, these findings are particularly useful and fill a gap in the literature by establishing a baseline of Jordanians’ knowledge, perspective, and behavior toward antibiotics.
In conclusion, while this study provides preliminary evidence of public awareness of antibiotic resistance and common antibiotic-resistance-related behaviors in Jordan, planning a future study with a more representative sample would help in generalizing the collected data to the larger population and confirming the validity of the study findings. To counteract and alleviate the severity of antibiotic resistance, public knowledge and awareness about antibiotic use should be increased. The vast majority of people were aware of antibiotics and antibiotic resistance, as well as their potential consequences on health. In the Jordanian community, there were widespread misconceptions about appropriate antibiotic use and behavioral components of antibiotic resistance. Antibiotic awareness was found to be associated with a high level of education, adequate health literacy, and adequate knowledge of antibiotics and antibiotic resistance. Future multicenter, well-designed prospective research studies should investigate the impact of chronic illnesses and patient–physician interactions on knowledge and its implications for responsible antibiotic use. Other programs should address the issue of self-medication and antibiotic resistance by addressing the entire spectrum of health literacy.
4. Materials and Methods
4.1. Study Design and Setting
A cross-sectional study design was carried out among Jordanians utilizing a convenience sample approach. The general public was invited to participate in an online self-administered questionnaire via an electronic invitation disseminated on social media (e.g., mainly Facebook). The survey link was frequently shared on Facebook in order to enhance response rates. The following criteria were used to identify eligible participants: (a) is a Jordanian citizen, (b) possesses adequate Arabic language abilities, (c) is 18 years of age or older, and (d) is willing to participate voluntarily in this study. A sample size of 1100 individuals was estimated using Raosoft software to attain the needed precision at a 95% confidence level, a 50% response distribution, and a 3% margin of error [60]. Responses to the study survey were automatically collected in Google Forms. The survey links redirected Facebook users to the survey’s first page, which contained thorough instructions regarding the study’s goal and expected outcomes, prior to participants consenting to participate and gaining access to the survey items. It was mentioned unequivocally that participation was completely voluntary and that confidentiality and anonymity would be maintained throughout the study. For data organization and analysis, Google Forms was linked to a Google spreadsheet.
4.2. Survey Instrument
A 47-item online survey questionnaire was employed in this study. At the beginning of the questionnaire, nine sociodemographic characteristics (i.e., age, gender, residence, family structure, education level, employment status, family monthly income, health insurance, and infection with COVID-19) were included. Participants of both genders were recruited on the basis of their age (>18 years) and geographic location (urban, suburban, and rural). The participants were asked about their family structure, which was classified as a nuclear family composed of parents and their children; a joint family composed of sets of siblings, their wives, and their dependent children; or an extended family composed of at least three generations. Employment status was also classified into three categories to ascertain whether the participants were unemployed, defined as unable to secure a paid job or out of paid work; employed in a nonmedical field, defined as any occupation that does not require a degree in a health-related field; or employed in a medical field, defined as any occupation that requires a degree in a health-related field (e.g., medicine, pharmacy, public health, clinical laboratory sciences, or nursing). The respondents’ educational attainment was operationalized as having completed high school, a bachelor’s degree, or a postgraduate degree (e.g., MSc or Ph.D.). The family monthly income of the participants was defined as the sum of the monthly household incomes of all family members who live together, which was classified as follows: less than JOD 500 (USD 700), between JOD 501 (USD 700) and JOD 1000 (USD 1400), between JOD 1001 (USD 1400) and JOD 1500 (USD 2100), and greater than JOD 1500 (USD 2100). Additionally, the respondents were asked whether they had health insurance at the time of the survey. Finally, the participants were asked whether they had previously been infected with COVID-19. The Single Item Literacy Screener (SILS) (2006) developed by Morris et al. (2006) [61] was adapted to serve as a predictor of the participants’ overall health literacy. The participants were asked, “How frequently do you seek assistance in reading the instructions and leaflets from your doctor or pharmacy?” The replies to the preceding question were scored using a 5-point Likert scale (5 = never, 4 = rarely, 3 = sometimes, 2 = often, 1 = always).
The World Health Organization’s (WHO) validated antibiotic resistance: multicountry public awareness survey was adapted in this study [2]. The WHO multicountry public awareness survey has a total of 37 items that assess people’s knowledge about antibiotics and antibiotic resistance, as well as their awareness of alternative solutions to antibiotic resistance and its health impacts. Antibiotic knowledge scores assess the levels of understanding around the appropriate use of antibiotics, including how and when to use antibiotics and what indications they should be used for. Antibiotic knowledge scores are computed as the number of correct responses to 13 items, ranging between 0 and 13 as 1 was assigned to correct answers and zero for all other cases. Knowledge of antibiotic resistance assesses the level of understanding around the issue of antibiotic resistance, which was measured by computing the number of correct responses to 8 statements. The scores ranged between 0 and 8 as 1 was assigned to correct answers and zero for all other cases. The participants’ level of awareness of possible solutions to the problem of antibiotic resistance measures the level of the participants’ awareness of possible solutions to address the problem of antibiotic resistance. A 5-point Likert scale of 8 items was used to assess the participants’ agreement with a series of solutions to antibiotic resistance. Additionally, the participants’ perspectives on the scope of the antibiotic resistance problem measure the level of the participants’ awareness and understanding of how respondents believe the issue of antibiotic resistance is serious and whether it will have an impact on their health. A 5-point Likert scale of 6 items was used to assess the participants’ agreement with a series of statements connected to antibiotic resistance.
To verify face and content validity, the final survey was assessed by five professionals in clinical pharmacy and pharmacy practice. Because the survey was available in English, two native Arabic speakers translated it into Arabic to verify that an English equivalent version was obtained. Following back translation, two independent fluent English speakers, and native Arabic speakers, assessed the Arabic version’s optimal wording and structure. Twenty pilot study participants were recruited primarily to assess survey readability and comprehension, with the goal of standardizing the items provided to the participants. Following that, Cronbach’s alpha was calculated for the scales utilized in this study (see Table 7).

Table 7.
Internal consistency of main concepts.
4.3. Statistical Analysis
The data collected in this study were analyzed using the IBM SPSS (Statistical Package for the Social Sciences) version 24.0 computer software. Descriptive analysis was used to report percentages, frequencies, means, and standard deviations of antibiotic knowledge and awareness scores obtained from the participants. In this study, a health literacy score of 1, 2, or 3 was classified as inadequate health literacy, whereas a score of 4 or 5 was classified as adequate health literacy. For subsequent analysis, knowledge of antibiotics was considered “inadequate” if the percentage scores were ≤50% (respondents’ score of 7 or less out of 13) and was considered “adequate” if the percentage scores >50%. Similarly, knowledge of antibiotic resistance was considered “inadequate” if the percentage scores were ≤50% (respondents’ score of 4 or less out of 8) and was considered “adequate” if the percentage scores >50%. The scores of both the participants’ perspectives on the scope of the antibiotic resistance problem and the level of awareness of possible solutions to the problem of antibiotic resistance were calculated by taking the average of the individuals’ responses to the multiple items on the scale as described by Kerlinger (1986) [62]; the scores ranged from 1 to 5. Since knowledge of antibiotic and antibiotic resistance was not following a normal distribution, a logistic regression model was then used to identify many factors (i.e., age, gender, residence, family structure, education level, employment status, family monthly income, health insurance, and infection with COVID-19) associated with adequate knowledge of antibiotics and antibiotic resistance. After completing univariate logistic regression, variables with p < 0.25 were included in the multiple logistic regression model (Supplementary Material Table S1) [63]. The adjusted odds ratios and 95% confidence intervals (CIs) were reported. The use of standard statistics (e.g., t-test and ANOVA) allowed this study to assess disparities across groups based on sociodemographic variables and to identify factors associated with the participants’ understanding of possible antibiotic resistance solutions and their perspectives on the scope of the antibiotic resistance problem. Following ANOVA testing, post hoc Tukey tests were performed to determine whether any of the groups varied substantially from the others. Data transformation was conducted using an inverse distribution function to ensure that data conformed to normality [64]. Levene’s statistics were used to test the assumption of variance homogeneity. The p-value was used to determine the statistical significance of all of the analyses, and significant findings were defined as a p-value of less than 0.05.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/antibiotics10091107/s1: Table S1: Simple logistic regression of sociodemographic factors and levels of health literacy associated with participants’ knowledge of antibiotics and antibiotic resistance.
Author Contributions
Conceptualization, all authors; methodology, all authors; software, S.M.M.; validation, S.M.M., S.A.-A. and R.A.K.; formal analysis, S.M.M. and R.A.K.; resources, S.A.-A., B.R.C. and M.A.A.; writing—original draft preparation, S.M.M., S.A.-A. and R.A.K.; writing—review and editing, all authors; supervision, S.A.-A. and M.A.A.; project administration, S.M.M., S.A.-A. and R.A.K. All authors have read and agreed to the published version of the manuscript.
Funding
This research received financial support from the Deanship of Scientific Research at the Jordan University of Science and Technology (Research Grant No: 20210357).
Institutional Review Board Statement
The study was carried out in accordance with the Declaration of Helsinki criteria and was approved by the Jordan University of Science and Technology’s Institutional Review Board (IRB, Reference: 56/140/2021).
Informed Consent Statement
The participants received an invitation leading them to a Google Forms-based online survey.
Data Availability Statement
Data are available on reasonable request and in line with permission approval processes from the Jordan University of Science and Technology.
Acknowledgments
We would like to thank the Deanship of Scientific Research at the Jordan University of Science and Technology for supporting this scientific production.
Conflicts of Interest
The authors declare no conflict of interest.
References
- D’Costa, V.M.; King, C.E.; Kalan, L.; Morar, M.; Sung, W.W.L.; Schwarz, C.; Froese, D.; Zazula, G.; Calmels, F.; Debruyne, R. Antibiotic resistance is ancient. Nature 2011, 477, 457–461. [Google Scholar] [CrossRef]
- World Health Organization. Antibiotic Resistance: Multi-Country Public Awareness Survey; World Health Organization: Geneva, Switzerland, 2015. [Google Scholar]
- Rodrigues, O.P.; Costa, T.; Branco, M.C.; Dinis, P. What’s the importance of portable tele-monitoring devices in patient therapeutic adherence? J. Int. Soc. Telemed. eHealth 2017, 5, e45. [Google Scholar]
- McNulty, C.A.M.; Boyle, P.; Nichols, T.; Clappison, P.; Davey, P. Don’t wear me out—the public’s knowledge of and attitudes to antibiotic use. J. Antimicrob. Chemother. 2007, 59, 727–738. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. New Report Calls for Urgent Action to Avert Antimicrobial Resistance Crisis. Volume 4. Available online: https://www.who.int/news/item/29-04-2019-new-report-calls-for-urgent-action-to-avert-antimicrobial-resistance-crisis (accessed on 25 April 2020).
- Beović, B.; Doušak, M.; Ferreira-Coimbra, J.; Nadrah, K.; Rubulotta, F.; Belliato, M.; Berger-Estilita, J.; Ayoade, F.; Rello, J.; Erdem, H. Antibiotic use in patients with COVID-19: A ‘snapshot’Infectious Diseases International Research Initiative (ID-IRI) survey. J. Antimicrob. Chemother. 2020, 75, 3386–3390. [Google Scholar] [CrossRef] [PubMed]
- Rawson, T.M.; Moore, L.S.P.; Zhu, N.; Ranganathan, N.; Skolimowska, K.; Gilchrist, M.; Satta, G.; Cooke, G.; Holmes, A. Bacterial and fungal coinfection in individuals with coronavirus: A rapid review to support COVID-19 antimicrobial prescribing. Clin. Infect. Dis. 2020, 71, 2459–2468. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Yu, Y.; Xu, J.; Shu, H.; Liu, H.; Wu, Y.; Zhang, L.; Yu, Z.; Fang, M.; Yu, T. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: A single-centered, retrospective, observational study. Lancet Respir. Med. 2020, 8, 475–481. [Google Scholar] [CrossRef]
- Getahun, H.; Smith, I.; Trivedi, K.; Paulin, S.; Balkhy, H.H. Tackling antimicrobial resistance in the COVID-19 pandemic. Bull. World Health Organ. 2020, 98, 442. [Google Scholar] [CrossRef] [PubMed]
- Hayajneh, W.A.; Al-Azzam, S.; Yusef, D.; Lattyak, W.J.; Lattyak, E.A.; Gould, I.; López-Lozano, J.M.; Conway, B.R.; Conlon-Bingham, G.; Aldeyab, M.A. Identification of thresholds in relationships between specific antibiotic use and carbapenem-resistant Acinetobacter baumannii (CRAb) incidence rates in hospitalized patients in Jordan. J. Antimicrob. Chemother. 2021, 76, 524–530. [Google Scholar] [CrossRef] [PubMed]
- Jirjees, F.J.; Al-Obaidi, H.J.; Sartaj, M.; Conlon-Bingham, G.; Farren, D.; Scott, M.G.; Gould, I.M.; López-Lozano, J.M.; Aldeyab, M.A.; Jirjees, F.J.; et al. Antibiotic Use and Resistance in Hospitals: Time-Series Analysis Strategy for Determining and Prioritising Interventions. Hosp. Pharm. Eur. 2020. Available online: https://hospitalpharmacyeurope.com/news/reviews-research/antibiotic-use-and-resistance-in-hospitals-time-series-analysis-strategy-for-determining-and-prioritising-interventions/ (accessed on 27 May 2021).
- Patel, A.; Emerick, M.; Cabunoc, M.K.; Williams, M.H.; Preas, M.A.; Schrank, G.; Rabinowitz, R.; Luethy, P.; Johnson, J.K.; Leekha, S. Rapid Spread and Control of Multidrug-Resistant Gram-Negative Bacteria in COVID-19 Patient Care Units. Emerg. Infect. Dis. 2021, 27, 1234. [Google Scholar] [CrossRef]
- Pavydė, E.; Veikutis, V.; Mačiulienė, A.; Mačiulis, V.; Petrikonis, K.; Stankevičius, E. Public knowledge, beliefs and behavior on antibiotic use and self-medication in Lithuania. Int. J. Environ. Res. Public Health 2015, 12, 7002–7016. [Google Scholar] [CrossRef] [PubMed]
- Vallin, M.; Polyzoi, M.; Marrone, G.; Rosales-Klintz, S.; Tegmark Wisell, K.; Stålsby Lundborg, C. Knowledge and attitudes towards antibiotic use and resistance-a latent class analysis of a Swedish population-based sample. PLoS ONE 2016, 11, e0152160. [Google Scholar] [CrossRef]
- Anderson, A. Online health information and public knowledge, attitudes, and behaviours regarding antibiotics in the UK: Multiple regression analysis of Wellcome Monitor and Eurobarometer Data. PLoS ONE 2018, 13, e0204878. [Google Scholar] [CrossRef] [PubMed]
- Salm, F.; Ernsting, C.; Kuhlmey, A.; Kanzler, M.; Gastmeier, P.; Gellert, P. Antibiotic use, knowledge and health literacy among the general population in Berlin, Germany and its surrounding rural areas. PLoS ONE 2018, 13, e0193336. [Google Scholar] [CrossRef]
- Kickbusch, I.; Pelikan, J.M.; Apfel, F.; Tsouros, A. Health Literacy; WHO Regional Office for Europe: Copenhagen, Denmark, 2013; ISBN 9289000155. [Google Scholar]
- Wang, M.P.; Viswanath, K.; Lam, T.H.; Wang, X.; Chan, S.S. Social determinants of health information seeking among Chinese adults in Hong Kong. PLoS ONE 2013, 8, e73049. [Google Scholar] [CrossRef]
- El Sherbiny, N.A.; Ibrahim, E.H.; Masoud, M. Assessment of knowledge, attitude and behavior towards antibiotic use in primary health care patients in Fayoum Governorate, Egypt. Alex. J. Med. 2018, 54, 535–540. [Google Scholar] [CrossRef]
- Mostafa, A.; Abdelzaher, A.; Rashed, S.; AlKhawaga, S.I.; Afifi, S.K.; AbdelAlim, S.; Mostafa, S.A.; Zidan, T.A. Is health literacy associated with antibiotic use, knowledge and awareness of antimicrobial resistance among non-medical university students in Egypt? A cross-sectional study. BMJ Open 2021, 11, e046453. [Google Scholar] [CrossRef]
- Sawair, F.A.; Baqain, Z.H.; Abu Karaky, A.; Abu Eid, R. Assessment of self-medication of antibiotics in a Jordanian population. Med. Princ. Pract. 2008, 18, 21–25. [Google Scholar] [CrossRef] [PubMed]
- Nusair, M.B.; Al-azzam, S.; Alhamad, H.; Momani, M.Y. The prevalence and patterns of self-medication with antibiotics in Jordan: A community-based study. Int. J. Clin. Pract. 2021, 75, e13665. [Google Scholar] [CrossRef]
- Al-Azzam, S.I.; Al-Husein, B.A.; Alzoubi, F.; Masadeh, M.M.; Al-Horani, M.A.S. Self-medication with antibiotics in Jordanian population. Int. J. Occup. Med. Environ. Health 2007, 20, 373–380. [Google Scholar] [CrossRef] [PubMed]
- Alshogran, O.Y.; Alzoubi, K.H.; Khabour, O.F.; Farah, S. Patterns of self-medication among medical and nonmedical university students in Jordan. Risk Manag. Healthc. Policy 2018, 11, 169. [Google Scholar] [CrossRef]
- Muflih, S.M.; Bashir, H.N.; Khader, Y.S.; Karasneh, R.A. The impact of health literacy on self-medication: A cross-sectional outpatient study. J. Public Health 2020. [Google Scholar] [CrossRef] [PubMed]
- Haque, M.; Rahman, N.A.A.; McKimm, J.; Kibria, G.M.; Majumder, M.A.A.; Haque, S.Z.; Islam, M.Z.; Abdullah, S.L.B.; Daher, A.M.; Zulkifli, Z. Self-medication of antibiotics: Investigating practice among university students at the Malaysian National Defence University. Infect. Drug Resist. 2019, 12, 1333. [Google Scholar] [CrossRef] [PubMed]
- Ruiz, M.E. Risks of self-medication practices. Curr. Drug Saf. 2010, 5, 315–323. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Guidelines for the Regulatory Assessment of Medicinal Products for Use in Self-Medication; World Health Organization: Geneva, Switzerland, 2000. [Google Scholar]
- Schroeck, J.L.; Ruh, C.A.; Sellick, J.A.; Ott, M.C.; Mattappallil, A.; Mergenhagen, K.A. Factors associated with antibiotic misuse in outpatient treatment for upper respiratory tract infections. Antimicrob. Agents Chemother. 2015, 59, 3848–3852. [Google Scholar] [CrossRef] [PubMed]
- Laxminarayan, R.; Duse, A.; Wattal, C.; Zaidi, A.K.M.; Wertheim, H.F.L.; Sumpradit, N.; Vlieghe, E.; Hara, G.L.; Gould, I.M.; Goossens, H. Antibiotic resistance—the need for global solutions. Lancet Infect. Dis. 2013, 13, 1057–1098. [Google Scholar] [CrossRef]
- Pereko, D.D.; Lubbe, M.S.; Essack, S.Y. Public knowledge, attitudes and behaviour towards antibiotic usage in Windhoek, Namibia. S. Afr. J. Infect. Dis. 2015, 30, 27–29. [Google Scholar] [CrossRef]
- Gowri, S.; Mehta, D.; Kannan, S. Antibiotic use in dentistry: A cross-sectional survey from a developing country. J. Orofac. Sci. 2015, 7, 90. [Google Scholar]
- Nathan, C.; Cars, O. Antibiotic resistance—problems, progress, and prospects. N. Engl. J. Med. 2014, 371, 1761–1763. [Google Scholar] [CrossRef]
- Knight, G.M.; Glover, R.E.; McQuaid, C.F.; Olaru, I.D.; Gallandat, K.; Leclerc, Q.J.; Fuller, N.M.; Willcocks, S.J.; Hasan, R.; van Kleef, E. Antimicrobial resistance and COVID-19: Intersections and implications. eLife 2021, 10, e64139. [Google Scholar] [CrossRef]
- Effah, C.Y.; Amoah, A.N.; Liu, H.; Agboyibor, C.; Miao, L.; Wang, J.; Wu, Y. A population-base survey on knowledge, attitude and awareness of the general public on antibiotic use and resistance. Antimicrob. Resist. Infect. Control 2020, 9, 105. [Google Scholar] [CrossRef]
- Brookes-Howell, L.; Elwyn, G.; Hood, K.; Wood, F.; Cooper, L.; Goossens, H.; Ieven, M.; Butler, C.C. “The body gets used to them”: Patients’ interpretations of antibiotic resistance and the implications for containment strategies. J. Gen. Intern. Med. 2012, 27, 766–772. [Google Scholar] [CrossRef]
- Kong, L.S.; Islahudin, F.; Muthupalaniappen, L.; Chong, W.W. Knowledge and expectations on antibiotic use among older adults in Malaysia: A cross-sectional survey. Geriatrics 2019, 4, 61. [Google Scholar] [CrossRef]
- Lim, K.K.; Teh, C.C. A cross sectional study of public knowledge and attitude towards antibiotics in Putrajaya, Malaysia. South. Med. Rev. 2012, 5, 26. [Google Scholar]
- Kim, S.S.; Moon, S.; Kim, E.J. Public knowledge and attitudes regarding antibiotic use in South Korea. J. Korean Acad. Nurs. 2011, 41, 742–749. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.R.M.; Dolk, F.C.K.; Smieszek, T.; Robotham, J.V.; Pouwels, K.B. Understanding the gender gap in antibiotic prescribing: A cross-sectional analysis of English primary care. BMJ Open 2018, 8, e020203. [Google Scholar] [CrossRef]
- Waaseth, M.; Adan, A.; Røen, I.L.; Eriksen, K.; Stanojevic, T.; Halvorsen, K.H.; Garcia, B.H.; Holst, L.; Ulshagen, K.M.; Blix, H.S.; et al. Knowledge of antibiotics and antibiotic resistance among Norwegian pharmacy customers—A cross-sectional study. BMC Public Health 2019, 19, 66. [Google Scholar] [CrossRef]
- Abdel-Qader, D.H.; Albassam, A.; Ismael, N.S.; El-Shara’, A.; Shehri, A.; Almutairi, F.S.; Al-Harbi, D.M.; Al Zahrani, M.M.; Chen, L.-C.; Al Mazrouei, N. Awareness of antibiotic use and resistance in Jordanian Community. J. Prim. Care Community Health 2020, 11, 2150132720961255. [Google Scholar] [CrossRef] [PubMed]
- Baum, A.; Kaboli, P.J.; Schwartz, M.D. Reduced in-person and increased telehealth outpatient visits during the COVID-19 pandemic. Ann. Intern. Med. 2021, 174, 129–131. [Google Scholar] [CrossRef] [PubMed]
- Araia, Z.Z.; Gebregziabher, N.K.; Mesfun, A.B. Self medication practice and associated factors among students of Asmara College of Health Sciences, Eritrea: A cross sectional study. J. Pharm. Policy Pract. 2019, 12, 3. [Google Scholar] [CrossRef]
- Hoxha, I.; Malaj, A.; Kraja, B.; Bino, S.; Oluka, M.; Marković-Peković, V.; Godman, B. Are pharmacists’ good knowledge and awareness on antibiotics taken for granted? The situation in Albania and future implications across countries. J. Glob. Antimicrob. Resist. 2018, 13, 240–245. [Google Scholar] [CrossRef]
- Jafari, F.; Khatony, A.; Rahmani, E. Prevalence of self-medication among the elderly in Kermanshah-Iran. Glob. J. Health Sci. 2015, 7, 360. [Google Scholar] [CrossRef] [PubMed]
- Mahmood, A.; Naqvi, R.; Grewal, A.; Diachun, L.; Gutmanis, I. Antibiotic resistance knowledge in the elderly. UWO Med. J. 2009, 78, 69–72. [Google Scholar]
- Davis, M.E.; Liu, T.-L.; Taylor, Y.J.; Davidson, L.; Schmid, M.; Yates, T.; Scotton, J.; Spencer, M.D. Exploring patient awareness and perceptions of the appropriate use of antibiotics: A mixed-methods study. Antibiotics 2017, 6, 23. [Google Scholar] [CrossRef] [PubMed]
- Hoelzer, K.; Bielke, L.; Blake, D.P.; Cox, E.; Cutting, S.M.; Devriendt, B.; Erlacher-Vindel, E.; Goossens, E.; Karaca, K.; Lemiere, S. Vaccines as alternatives to antibiotics for food producing animals. Part 1: Challenges and needs. Vet. Res. 2018, 49, 64. [Google Scholar] [CrossRef] [PubMed]
- Smulski, S.; Turlewicz-Podbielska, H.; Wylandowska, A.; Włodarek, J. Non-antibiotic possibilities in prevention and treatment of calf diarrhoea. J. Vet. Res. 2020, 64, 119. [Google Scholar] [CrossRef] [PubMed]
- Higuita-Gutiérrez, L.F.; Villamil, G.E.R.; Quiceno, J.N.J. Knowledge, attitude, and practice regarding antibiotic use and resistance among medical students in Colombia: A cross-sectional descriptive study. BMC Public Health 2020, 20, 1861. [Google Scholar] [CrossRef]
- Dixit, A.; Kumar, N.; Kumar, S.; Trigun, V. Antimicrobial resistance: Progress in the decade since emergence of New Delhi metallo-β-lactamase in India. Indian J. Community Med. 2019, 44, 4. [Google Scholar]
- Aldeyab, M.; López-Lozano, J.M.; Gould, I.M. Global antibiotics use and resistance. In Global Pharmaceutical Policy; Palgrave Macmillan: London, UK, 2020; pp. 331–344. ISBN 9789811527241. [Google Scholar]
- Shebehe, J.; Ottertun, E.; Carlén, K.; Gustafson, D. Knowledge about infections is associated with antibiotic use: Cross-sectional evidence from the health survey Northern Ireland. BMC Public Health 2021, 21, 1041. [Google Scholar] [CrossRef]
- van Dijk, J.A.G.M. The Deepening Divide: Inequality in the Information Society; Sage Publications: London, UK, 2005. [Google Scholar]
- Hargittai, E. Second-Level Digital Divide: Mapping Differences in People’s Online Skills. arXiv 2001, arXiv:cs/0109068. [Google Scholar] [CrossRef]
- Department of Statistics. Available online: http://dosweb.dos.gov.jo/ (accessed on 22 August 2021).
- Lehdonvirta, V.; Oksanen, A.; Räsänen, P.; Blank, G. Social Media, Web, and Panel Surveys: Using Non-Probability Samples in Social and Policy Research. Policy Internet 2021, 13, 134–155. [Google Scholar] [CrossRef]
- Evangelista, L.S.; Rasmusson, K.D.; Laramee, A.S.; Barr, J.; Ammon, S.E.; Dunbar, S.; Ziesche, S.; Patterson, J.H.; Yancy, C.W. Health literacy and the patient with heart failure—implications for patient care and research: A consensus statement of the Heart Failure Society of America. J. Card. Fail. 2010, 16, 9–16. [Google Scholar] [CrossRef]
- Sample Size Calculator by Raosoft, Inc. Available online: http://www.raosoft.com/samplesize.html (accessed on 22 April 2021).
- Morris, N.S.; MacLean, C.D.; Chew, L.D.; Littenberg, B. The Single Item Literacy Screener: Evaluation of a brief instrument to identify limited reading ability. BMC Fam. Pract. 2006, 7, 21. [Google Scholar] [CrossRef] [PubMed]
- Kerlinger, F. Foundations of Behavioral Research, 3rd ed.; Holt, Rinehart and Winston: New York, NY, USA, 1986. [Google Scholar]
- Sperandei, S. Understanding logistic regression analysis. Biochem. Med. 2014, 24, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Templeton, G.F. A two-step approach for transforming continuous variables to normal: Implications and recommendations for IS research. Commun. Assoc. Inf. Syst. 2011, 28, 4. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).