Oral Antibiotic for Empirical Management of Acute Dentoalveolar Infections—A Systematic Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Protocol and Research Question
2.2. Search Strategies and Study Selection
2.3. Quality Assessment
2.4. Extraction of Antibiotics and Outcomes
3. Results
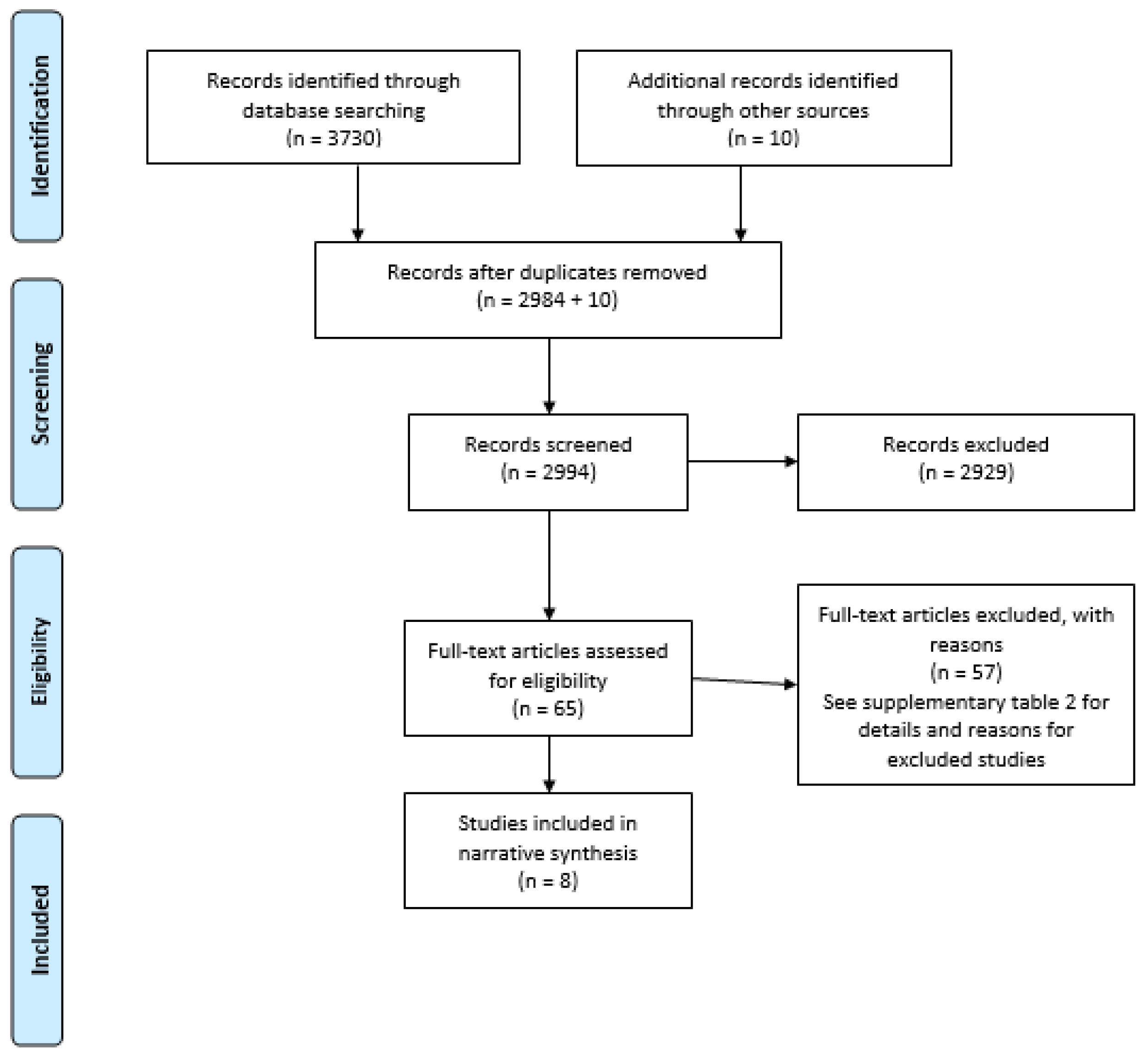
3.1. Study Selection
3.2. Study Characteristics
3.3. Antibiotic Regimens Used
3.4. Outcomes of Oral Antibiotics for Dentoalveolar Infections
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Matthews, D.C.; Sutherland, S.; Basrani, B. Emergency management of acute apical abscesses in the permanent dentition: A systematic review of the literature. J. Can. Dent. Assoc. 2003, 69, 660. [Google Scholar]
- Oral and Dental Expert Group. Therapeutic Guidelines: Oral and Dental Version 3; Therapeutic Guidelines Ltd.: Melbourne, Australia, 2019. [Google Scholar]
- Marton, I.J.; Kiss, C. Protective and destructive immune reactions in apical periodontitis. Oral Microbiol Immunol 2000, 15, 139–150. [Google Scholar] [CrossRef]
- Kuriyama, T.; Absi, E.G.; Williams, D.W.; Lewis, M.A. An outcome audit of the treatment of acute dentoalveolar infection: Impact of penicillin resistance. Br. Dent. J. 2005, 198, 759–763. [Google Scholar] [CrossRef]
- Lockhart, P.B.; Tampi, M.P.; Abt, E.; Aminoshariae, A.; Durkin, M.J.; Fouad, A.F.; Gopal, P.; Hatten, B.W.; Kennedy, E.; Lang, M.S.; et al. Evidence-based clinical practice guideline on antibiotic use for the urgent management of pulpal- and periapical-related dental pain and intraoral swelling: A report from the American Dental Association. J. Am. Dent. Assoc. 2019, 150, 906–921. [Google Scholar] [CrossRef]
- FGDP (UK). Antimicrobial Prescribing for GDPs. Available online: https://www.fgdp.org.uk/guidance-standards/antimicrobial-prescribing-gdps (accessed on 10 January 2019).
- Guidance Dental Group. Drug Prescribing for Dentistry; Scottish Dental Clinical Effectiveness Programe: Dundee, UK, 2016. [Google Scholar]
- Teoh, L.S.K.; Marino, R.; McCullough, M. Part 1. Current prescribing trends of antibiotics by dentists in Australia from 2012 to 2016. Aust. Dent. J. 2018, 63, 329–337. [Google Scholar] [CrossRef]
- Marra, F.; George, D.; Chong, M.; Sutherland, S.; Patrick, D.M. Antibiotic prescribing by dentists has increased: Why? J. Am. Dent. Assoc. 2016, 147, 320–327. [Google Scholar] [CrossRef]
- Thornhill, M.H.; Dayer, M.J.; Durkin, M.J.; Lockhart, P.B.; Baddour, L.M. Oral antibiotic prescribing by NHS dentists in England 2010-2017. Br. Dent. J. 2019, 227, 1044–1050. [Google Scholar] [CrossRef]
- Suda, K.J.; Roberts, R.M.; Hunkler, R.J.; Taylor, T.H. Antibiotic prescriptions in the community by type of provider in the United States, 2005-2010. J. Am. Pharm. Assoc. 2016, 56, 621–626. [Google Scholar] [CrossRef] [PubMed]
- Gross, A.E.; Hanna, D.; Rowan, S.A.; Bleasdale, S.C.; Suda, K.J. Successful Implementation of an Antibiotic Stewardship Program in an Academic Dental Practice. Open Forum Infect. Dis 2019, 6, ofz067. [Google Scholar] [CrossRef] [PubMed]
- Teoh, L.; Stewart, K.; Marino, R.J.; McCullough, M.J. Improvement of dental prescribing practices using education and a prescribing tool: A pilot intervention study. Br. J. Clin Pharmacol 2020, 87, 152–162. [Google Scholar] [CrossRef] [PubMed]
- World Dental Federation FDI. Antibiotic Stewardship in Dentistry; FDI: San Francisco, CA, USA, 2019. [Google Scholar]
- Teoh, L.; Marino, R.J.; Stewart, K.; McCullough, M.J. A survey of prescribing practices by general dentists in Australia. BMC Oral Health 2019, 19, 193. [Google Scholar] [CrossRef] [PubMed]
- Cope, A.L.; Francis, N.A.; Wood, F.; Chestnutt, I.G. Antibiotic prescribing in UK general dental practice: A cross-sectional study. Community Dent. Oral Epidemiol. 2016, 44, 145–153. [Google Scholar] [CrossRef]
- Suda, K.J.; Calip, G.S.; Zhou, J.; Rowan, S.; Gross, A.E.; Hershow, R.C.; Perez, R.I.; McGregor, J.C.; Evans, C.T. Assessment of the Appropriateness of Antibiotic Prescriptions for Infection Prophylaxis Before Dental Procedures, 2011 to 2015. JAMA Netw. Open 2019, 2, e193909. [Google Scholar] [CrossRef] [PubMed]
- Kudiyirickal, M.G.; Hollinshead, F. Antimicrobial prescribing practice by dentists: A study from two primary care centres in UK. Minerva Stomatol. 2011, 60, 495–500. [Google Scholar] [PubMed]
- Banawas, S.S. Clostridium difficile Infections: A Global Overview of Drug Sensitivity and Resistance Mechanisms. Biomed. Res. Int. 2018, 2018, 8414257. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Jin, D.; Kim, H.B.; Stratton, C.W.; Wu, B.; Tang, Y.W.; Sun, X. Update on Antimicrobial Resistance in Clostridium difficile: Resistance Mechanisms and Antimicrobial Susceptibility Testing. J. Clin. Microbiol. 2017, 55, 1998–2008. [Google Scholar] [CrossRef]
- Bye, M.W.T.; Holzbauer, S. Antibiotic prescribing for dental procedures in community-associated Clostridium difficile cases, Minnesota, 2009–2015. Open Forum. Infect. Dis. 2017, 4 (Suppl. 1). [Google Scholar] [CrossRef]
- Liau, I.; Han, J.; Bayetto, K.; May, B.; Goss, A.; Sambrook, P.; Cheng, A. Antibiotic resistance in severe odontogenic infections of the South Australian population: A 9-year retrospective audit. Aust. Dent. J. 2018, 63, 187–192. [Google Scholar] [CrossRef]
- Sundararajan, K.; Gopaldas, J.A.; Somehsa, H.; Edwards, S.; Shaw, D.; Sambrook, P. Morbidity and mortality in patients admitted with submandibular space infections to the intensive care unit. Anaesth. Intensive Care 2015, 43, 420–422. [Google Scholar]
- Cachovan, G.; Boger, R.H.; Giersdorf, I.; Hallier, O.; Streichert, T.; Haddad, M.; Platzer, U.; Schon, G.; Wegscheider, K.; Sobottka, I. Comparative efficacy and safety of moxifloxacin and clindamycin in the treatment of odontogenic abscesses and inflammatory infiltrates: A phase II, double-blind, randomized trial. Antimicrob. Agents Chemother. 2011, 55, 1142–1147. [Google Scholar] [CrossRef]
- Baum, S.H.; Ha-Phuoc, A.K.; Mohr, C. Treatment of odontogenic abscesses: Comparison of primary and secondary removal of the odontogenic focus and antibiotic therapy. Oral Maxillofac. Surg. 2020, 24, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.K.; Chuang, S.K.; August, M. Antibiotic Resistance in Severe Orofacial Infections. J. Oral Maxillofac. Surg. 2017, 75, 962–968. [Google Scholar] [CrossRef] [PubMed]
- Sirriyeh, R.L.R.; Gardner, P.; Armitage, G. Reviewing studies with diverse designs: The development and evaluation of a new tool. J. Eval. Clin. Pract. 2012, 18, 746–752. [Google Scholar] [CrossRef]
- Gilmore, W.C.; Jacobus, N.V.; Gorbach, S.L.; Doku, H.C.; Tally, F.P. A prospective double-blind evaluation of penicillin versus clindamycin in the treatment of odontogenic infections. J. Oral Maxillofac. Surg. 1988, 46, 1065–1070. [Google Scholar] [CrossRef]
- von Konow, L.; Kondell, P.A.; Nord, C.E.; Heimdahl, A. Clindamycin versus phenoxymethylpenicillin in the treatment of acute orofacial infections. Eur. J. Clin. Microbiol. Infect. Dis. 1992, 11, 1129–1135. [Google Scholar] [CrossRef]
- Martin, M.V.; Longman, L.P.; Hill, J.B.; Hardy, P. Acute dentoalveolar infections: An investigation of the duration of antibiotic therapy. Br. Dent. J. 1997, 183, 135–137. [Google Scholar] [CrossRef] [PubMed]
- Matijevic, S.; Lazic, Z.; Kuljic-Kapulica, N.; Nonkovic, Z. Empirical antimicrobial therapy of acute dentoalveolar abscess. Vojnosanit. Pregl. 2009, 66, 544–550. [Google Scholar] [CrossRef]
- Kumari, S.; Mohanty, S.; Sharma, P.; Dabas, J.; Kohli, S.; Diana, C. Is the routine practice of antibiotic prescription and microbial culture and antibiotic sensitivity testing justified in primary maxillofacial space infection patients? A prospective, randomized clinical study. J. Craniomaxillofac. Surg. 2018, 46, 446–452. [Google Scholar] [CrossRef]
- von Konow, L.; Nord, C.E. Ornidazole compared to phenoxymethylpenicillin in the treatment of orofacial infections. J. Antimicrob. Chemother. 1983, 11, 207–215. [Google Scholar] [CrossRef]
- Ellison, S.J. An outcome audit of three day antimicrobial prescribing for the acute dentoalveolar abscess. Br. Dent. J. 2011, 211, 591–594. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.C.G.W. The diagnosis and treatment of Ludwig’s angina: A report of twenty cases. N. Engl. J. Med. 1943, 228. [Google Scholar] [CrossRef]
- Smith, A.; Al-Mahdi, R.; Malcolm, W.; Palmer, N.; Dahlen, G.; Al-Haroni, M. Comparison of antimicrobial prescribing for dental and oral infections in England and Scotland with Norway and Sweden and their relative contribution to national consumption 2010-2016. BMC Oral Health 2020, 20, 172. [Google Scholar] [CrossRef]
- Igoumenakis, D.; Giannakopoulos, N.N.; Parara, E.; Mourouzis, C.; Rallis, G. Effect of Causative Tooth Extraction on Clinical and Biological Parameters of Odontogenic Infection: A Prospective Clinical Trial. J. Oral Maxillofac. Surg. 2015, 73, 1254–1258. [Google Scholar] [CrossRef] [PubMed]
- Flynn, T.R. What are the antibiotics of choice for odontogenic infections, and how long should the treatment course last? Oral Maxillofac. Surg. Clin. N. Am. 2011, 23, 519–536. [Google Scholar] [CrossRef]
- Johri, A.; Piecuch, J.F. Should teeth be extracted immediately in the presence of acute infection? Oral Maxillofac. Surg. Clin. N. Am. 2011, 23, 507–511. [Google Scholar] [CrossRef]
- Lang, P.M.; Jacinto, R.C.; Dal Pizzol, T.S.; Ferreira, M.B.; Montagner, F. Resistance profiles to antimicrobial agents in bacteria isolated from acute endodontic infections: Systematic review and meta-analysis. Int. J. Antimicrob. Agents 2016, 48, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Teoh, L.; Thompson, W.; McCullough, M.J. Questioning dual antimicrobial therapy as first line in recent Australian Therapeutic Guidelines. Aust. Dent. J. 2020, 65, 302–304. [Google Scholar] [CrossRef]
- Shilnikova, I.I.; Dmitrieva, N.V. Evaluation of antibiotic susceptibility of Bacteroides, Prevotella and Fusobacterium species isolated from patients of the N. N. Blokhin Cancer Research Center, Moscow, Russia. Anaerobe 2015, 31, 15–18. [Google Scholar] [CrossRef]
- Bancescu, G.; Didilescu, A.; Bancescu, A.; Bari, M. Antibiotic susceptibility of 33 Prevotella strains isolated from Romanian patients with abscesses in head and neck spaces. Anaerobe 2015, 35 Pt A, 41–44. [Google Scholar] [CrossRef]
- Veloo, A.C.M.; Tokman, H.B.; Jean-Pierre, H.; Dumont, Y.; Jeverica, S.; Lienhard, R.; Novak, A.; Rodloff, A.; Rotimi, V.; Wybo, I.; et al. Antimicrobial susceptibility profiles of anaerobic bacteria, isolated from human clinical specimens, within different European and surrounding countries. A joint ESGAI study. Anaerobe 2020, 61, 102111. [Google Scholar] [CrossRef] [PubMed]
- Sweeney, L.C.; Dave, J.; Chambers, P.A.; Heritage, J. Antibiotic resistance in general dental practice—A cause for concern? J. Antimicrob. Chemother. 2004, 53, 567–576. [Google Scholar] [CrossRef] [PubMed]
- José, F.; Siqueira, I.N.R., Jr. Present status and future directions in endodontic microbiology. Endodontic Top. 2014, 30, 3–22. [Google Scholar]
- Costelloe, C.; Metcalfe, C.; Lovering, A.; Mant, D.; Hay, A.D. Effect of antibiotic prescribing in primary care on antimicrobial resistance in individual patients: Systematic review and meta-analysis. BMJ 2010, 340, c2096. [Google Scholar] [CrossRef] [PubMed]
| Study | Study Design | Objectives | Participants | Clinical Intervention | Definition of Clinical Outcomes | Outcomes |
|---|---|---|---|---|---|---|
| Von Konow and Nord, 1983 [33] | Prospective, randomised, double-blind study | To compare the efficacy of ornidazole to that of PMV in the treatment of orofacial infections | 60 adult patients with acute orofacial infections. Ornidazole group: 14 males, 16 females, age range: 22–77 years Phenoxymethylpenicillin group: 17 males, 13 females, age range: 22–77 years | Surgical drainage was provided to all patients, except for two in each group, who received antimicrobial therapy only | Response to treatment was considered moderate or poor when the signs and symptoms of fever, swelling, pain and disturbance of sleep had not resolved or markedly subsided within 5 days | Ornidazole group: all patients cured in 7 days PMV group: 25 patients were cured in 7 days; 5 patients did not respond. Adverse effects: Ornidazole group: 1 patient reported metallic taste, 1 had feebleness, 1 had headache, and others had headache, weakness, nausea. Phenoxymethylpenicillin group: 3 patients had nausea |
| Gilmore et al., 1988 [28] | Prospective, randomised, double-blind clinical study | To compare the efficacy of PMV versus clindamycin in the treatment of moderate–severe orofacial infections of odontogenic origin | 55 adult patients (41 males and 14 females) with moderate–severe orofacial infection of odontogenic origin | Incision and drainage procedure via an intraoral approach | Patients were seen at baseline and days 3 and 7. Success was defined as elimination of the infection in 7 days Improvement: decrease in signs/symptoms by day 7 but requiring an additional course of antibiotic Failure: increasing signs/symptoms of infection by day 7 | PMV group: 22 patients (81%) had a successful outcome; 5 (19%) showed improvement Clindamycin group: 23 (82%) had a successful outcome; 5 (18%) showed improvement Adverse effects: PMV group: 1 patient had diarrhoea Clindamycin: 2 patients had diarrhoea (in 1 case, it was C. difficile-associated diarrhoea) |
| Von Konow et al., 1992 [29] | Prospective, randomised study | To compare penicillin and clindamycin with respect to microbiological and clinical efficacy and adverse effects in the treatment of orofacial infections | 60 patients (36 males and 24 females, mean age 46 years, range 20–70 years), with acute dentoalveolar infections | Incision and drainage (where indicated) | Patients were examined on days 1, 3, 7 and 14. Treatment was regarded as poor when clinical symptoms had not disappeared or markedly subsided within 5 days, or when symptoms recurred during the observation period | Clinical outcomes: All patients except for one in each group responded to treatment Adverse effects: PMV group: 1 patient had severe diarrhoea Clindamycin group: 6 patients with moderate–severe gastrointestinal discomfort and 1 case of C. difficile-associated diarrhoea |
| Martin et al., 1997 [30] | Prospective clinical study over 3 years | To evaluate shortened courses of antibiotics in the management of dentoalveolar abscesses | 759 patients (483 males and 276 females, age range: 16–81 years) with acute dentoalveolar abscesses associated with systemic signs (swelling, temperature elevation) | Drainage of the abscess by incision (124 patients) or extraction (635 patients) | Primary outcome: resolution of the swelling and a normal temperature | At 2–3 days, the primary outcome was achieved in: Amoxicillin group: 537/546 patients Clindamycin group: 140/141 patients Erythromycin group: 71/72 patients At 2–3 days, 748 patients had achieved the primary outcome and discontinued antibiotic therapy; 11 patients required re-incision of the abscess after 2–3 days |
| Kuriyama et al., 2005 [4] | Retrospective study | To determine if the outcome of treatment of dentoalveolar infection was influenced by the choice of antibiotic and the presence of penicillin-resistant bacteria. | 112 patients (88 males and 24 females, age range: 17–81 years) with acute dentoalveolar infection | Surgical drainage through incision of the soft tissue swelling or through the pulp chamber | Clinical signs and symptoms were reassessed at 48 or 72 h. A four-point scale was used to measure success as follows: 3, Completely improved (complete resolution) 2, Much improved (almost complete resolution) 1, Slightly improved (the intensity of signs/symptoms slightly reduced)0, No improvement (same signs/symptoms as at baseline) | All antibiotic regimens produced a satisfactory outcome at 48 or 72 h, (mean score 2.3–2.6), with no significant differences in the regimens. Of the patients who underwent incisional drainage, the mean improvement score was 2.5 |
| Matijevic et al., 2009 [31] | Prospective comparative study | To investigate the clinical efficiency of amoxicillin and cefalexin in the empirical treatment of acute odontogenic abscesses and assess the antimicrobial susceptibility of the isolated bacteria in early phases of its development | 90 patients with acute odontogenic abscesses who received surgical treatment | Extraction of the tooth and/or abscess incision | Inflammatory swelling, regional lymphadenopathy, trismus, temperature were considered clinical symptoms of infection. Antibiotic therapy was stopped after full regression of all clinical symptoms | Amoxicillin group: 93.3% of patients had full recovery on the 5th day; signs and symptoms lasted for 4.47 days on average, but significant regression of swelling was recorded on the 2nd day for 22/30 patients. Cefalexin group: 90.0% of patients had full recovery on the 5th day; signs and symptoms lasted for 4.67 days on average; significant regression of swelling was recorded on the 2nd day for 23/30 patients. Surgical group: 93.3% of patients had full recovery on the 7th day; signs and symptoms lasted on average for 6.17 days, with significant regression of swelling on the 3rd day for 25/30 patients |
| Cachovan et al., 2011 [24] | Phase II, prospective, double-blind, randomised trial | To compare the efficacies and safeties of moxifloxacin and clindamycin for the treatment of patients with gingival inflammatory infiltrates and as adjuvant therapy for patients with odontogenic abscesses requiring surgical treatment. | 31 patients (minimum age 18 years) with a diagnosis of odontogenic abscess (dentoalveolar, periodontal, pericoronitis) requiring surgical intervention and adjunctive antibiotic treatment | Surgical interventions in accordance with the guidelines of the German Society for Oral and Maxillofacial surgery, including surgical incisions, drainages, tooth extraction, debridement and puncture. | Pain reduction using a visual analogue scale at days 2–3 from baseline. Rating of cure: resolution of all signs of inflammation including fever, negative palpation for lymphadenopathy, subjectively unobstructed opening of the mouth and incisal edge distance of at least 35 mm, no need for further therapy. Improvement: signs of inflammation were decreased by at least 50%, body temperature ≤ 38.0 °C, reduced excretion of pus, soft/palpable lymph nodes, opening of the mouth was slightly obstructed, incisal edge distance was 35 mm or lower Failure: initial fever did not decrease, excretion of pus was unchanged, palpation for lymphadenopathy was positive | Pain reduction: Mean pain reduction on days 2–3 was higher for moxifloxacin compared to clindamycin, but the difference did not reach statistical significance. All patients had clinical outcomes rated as improved or cure in both the moxifloxacin group and the clindamycin group by days 5–7. The differences between the treatment groups did not reach statistical significance. Adverse effects: The rate was higher for clindamycin compared to moxifloxacin, especially nausea and diarrhoea |
| Kumari et al., 2018 [32] | Prospective, randomised clinical study | To compare treatment outcome of removal of foci and incision and drainage, with or without antibiotic therapy, in the management of single primary maxillofacial space infection with a known focus | 40 patients (age range 10–50 years, mean: 27.3 years) with a single primary odontogenic maxillofacial space infection | Extraction or endodontics; surgical drainage (either extraoral or intraoral) | Patients were evaluated on days 1, 2, 3, 5 and 7. Pain, mouth opening, swelling, purulent discharge, return to normal life | Pain: The majority of patients in both groups were pain-free by day 7. The difference in the mean pain scores between groups A and B were clinically significant at any visit. Mouth opening: the percentage increase in mouth opening was 25% for the antibiotic group and 21% for the group without antibiotics between days 1 and days 7. Purulent discharge stopped within 3 days for 75% of the patients. Return to normal life: 47.5% of the patients reported a return to normal life on day 7. No significant differences between both groups for any category of clinical outcome |
| Study | Number of Patients | Drug | Dose | Frequency | Duration | |
|---|---|---|---|---|---|---|
| Von Konow and Nord, 1983 [33] | 30 | Ornidazole | 500 mg | 12-hourly | 7 days | |
| 30 | Phenoxymethylpenicillin | 800 mg | 12-hourly | 7 days | ||
| Gilmore et al., 1988 [28] | 28 | Clindamycin | 150 mg | 4/day | 7 days | |
| 27 | Phenoxymethylpenicillin | 250 mg | 4/day | 7 days | ||
| Von Konow et al., 1992 [29] | 30 | Clindamycin | 150 mg | 6-hourly | 7 days | |
| 30 | Phenoxymethylpenicillin | 1 g | 12-hourly | 7 days | ||
| Martin et al., 1997 [30] | 546 | Amoxicillin | 250 mg | 8-hourly | 537/546 patients: 2–3 days; 9/546 patients: 10 days | |
| 141 | Clindamycin | 150 mg | 6-hourly | 140/141 patients: 2–3 days; 1/141 patients: 10 days | ||
| 72 | Erythromycin | 250 mg | 6-hourly | 71/72 patients: 2–3 days; 1/72 patients: 10 days | ||
| Kuriyama et al., 2005 [4] | 65 | Amoxicillin | 500 mg | 8-hourly | 2–3 days | |
| Phenoxymethylpenicillin | 500 mg | 6-hourly | ||||
| 24 | Phenoxymethylpenicillin/Metronidazole | 500 mg/400 mg | 8-hourly/8-hourly | |||
| 9 | Metronidazole 400 mg | 400 mg | 8-hourly | |||
| 6 | Amoxicillin/Clavulanic Acid | 375 mg (CA) | 8-hourly | |||
| 6 | Erythromycin/Metronidazole | 250 mg/400 mg | 8-hourly/8-hourly | |||
| 2 | Erythromycin | 250 mg | 6-hourly | |||
| Matijevic et al., 2009 [31] | 30 | Amoxicillin | 500 mg | 6-hourly | Until symptoms had resolved; 5 days | |
| 30 | Cefalexin | 500 mg | 6-hourly | |||
| Cachovan et al., 2011 [24] | 16 | Clindamycin | 300 mg | 4/day | 5 days | |
| 15 | Moxifloxacin | 400 mg | 1/day | 5 days | ||
| Kumari et al., 2018 [32] | 20 | Amoxicillin/Clavulanic Acid and Metronidazole | 625 mg and 400 mg | 3/day | Unreported | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Teoh, L.; Cheung, M.C.; Dashper, S.; James, R.; McCullough, M.J. Oral Antibiotic for Empirical Management of Acute Dentoalveolar Infections—A Systematic Review. Antibiotics 2021, 10, 240. https://doi.org/10.3390/antibiotics10030240
Teoh L, Cheung MC, Dashper S, James R, McCullough MJ. Oral Antibiotic for Empirical Management of Acute Dentoalveolar Infections—A Systematic Review. Antibiotics. 2021; 10(3):240. https://doi.org/10.3390/antibiotics10030240
Chicago/Turabian StyleTeoh, Leanne, Monique C Cheung, Stuart Dashper, Rodney James, and Michael J McCullough. 2021. "Oral Antibiotic for Empirical Management of Acute Dentoalveolar Infections—A Systematic Review" Antibiotics 10, no. 3: 240. https://doi.org/10.3390/antibiotics10030240
APA StyleTeoh, L., Cheung, M. C., Dashper, S., James, R., & McCullough, M. J. (2021). Oral Antibiotic for Empirical Management of Acute Dentoalveolar Infections—A Systematic Review. Antibiotics, 10(3), 240. https://doi.org/10.3390/antibiotics10030240






