The Effects of Antibiotics for Helicobacter pylori Eradication or Dapsone on Chronic Spontaneous Urticaria: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Literature Search and Study Selection
2.2. Data Extraction and Quality Assessments
2.3. Data Synthesis and Analyses
3. Results
3.1. Study Selection
3.2. Outcomes
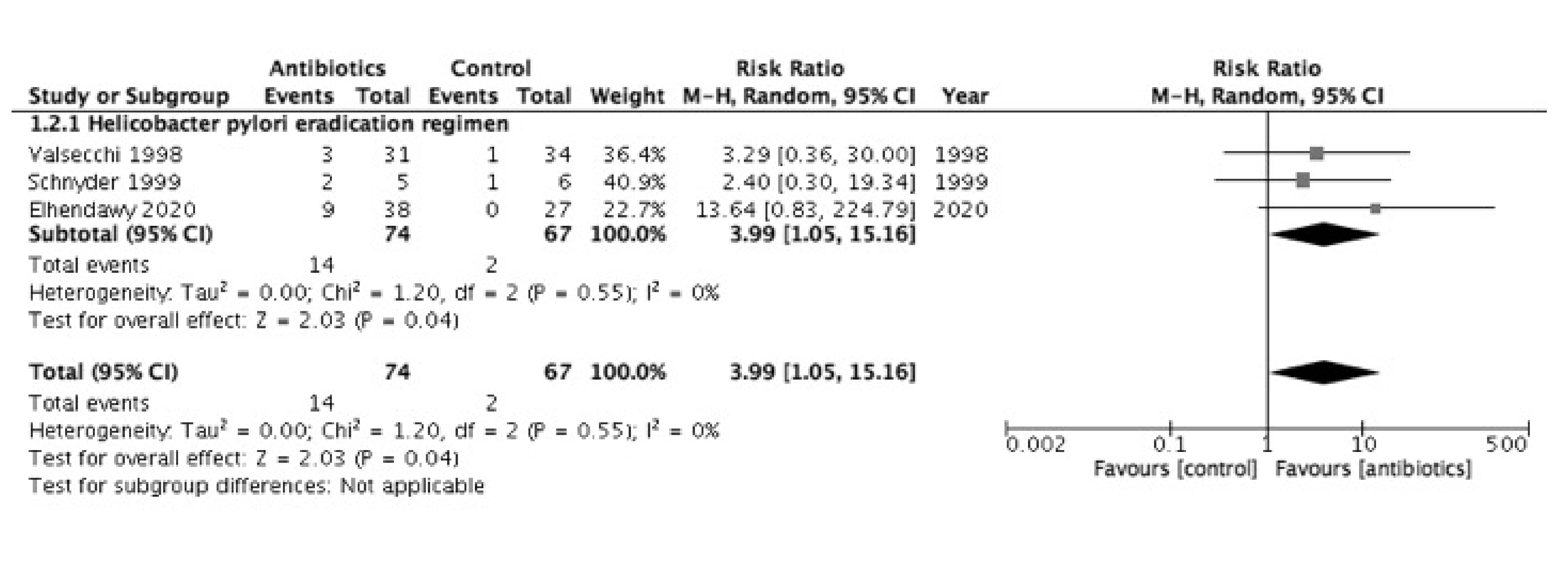
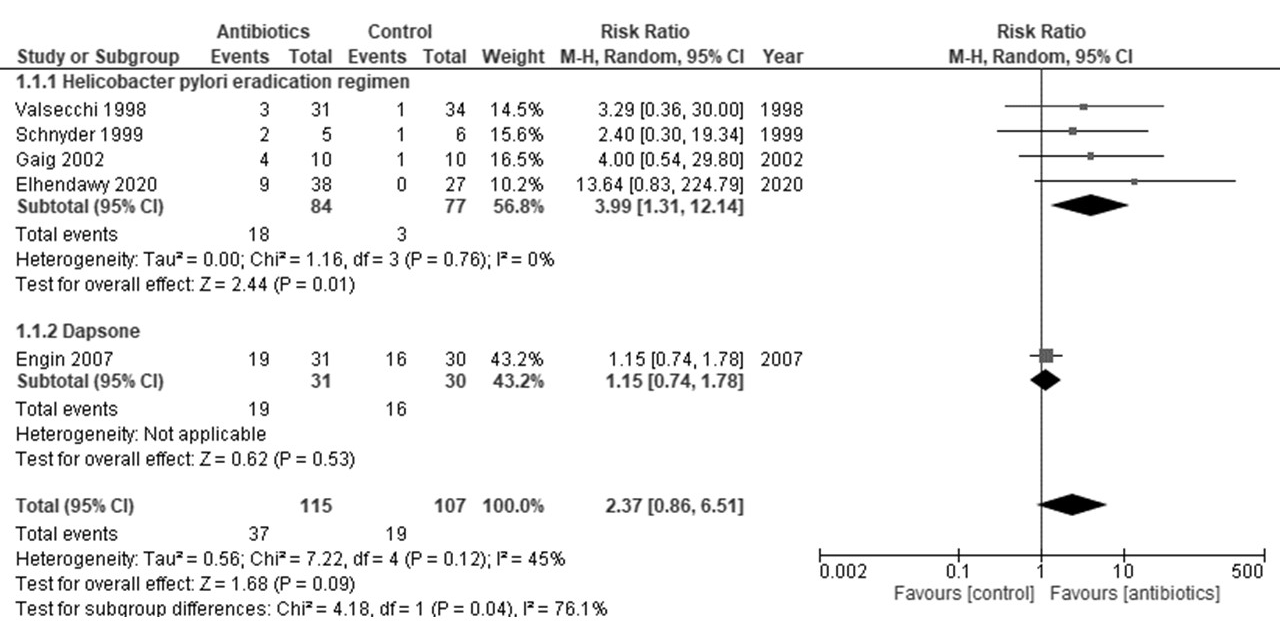
3.2.1. Remission Rate
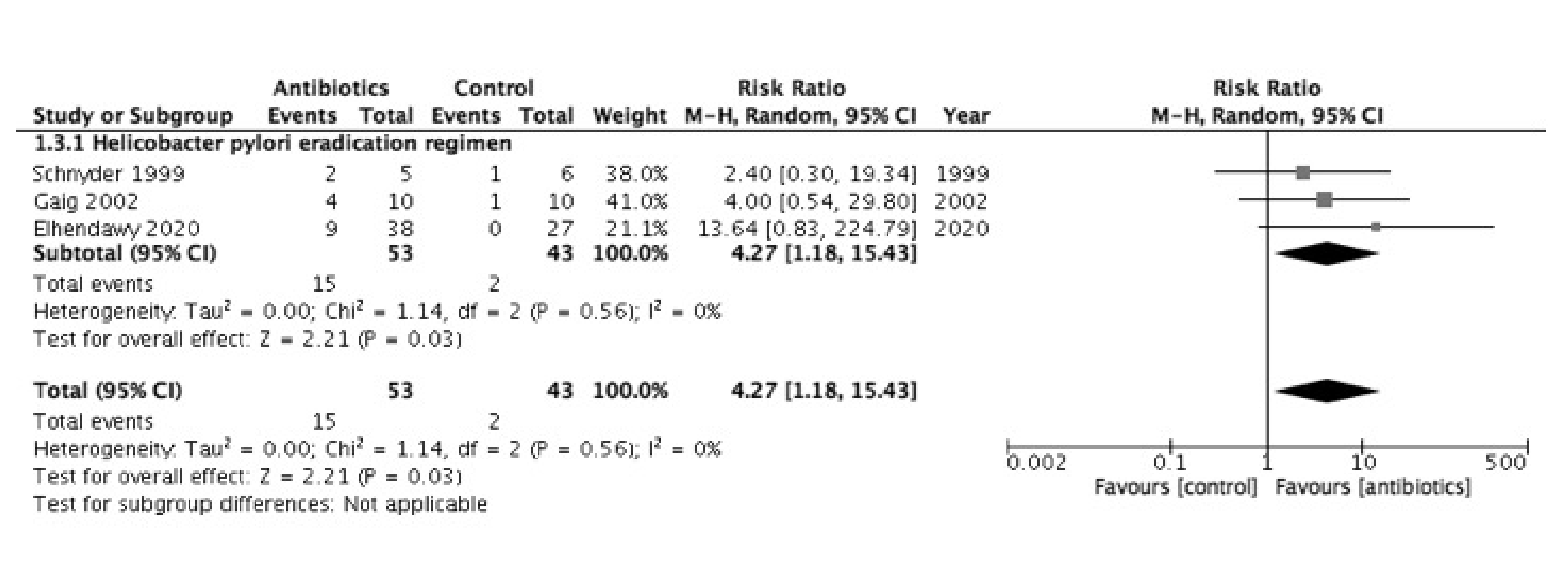
3.2.2. Clinical Improvement
3.2.3. Adverse Events
3.3. Additional Analyses
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
Appendix A

| Authors. (Ref No.) | Risk of Bias 2 Tool Assessment | |||||
|---|---|---|---|---|---|---|
| Bias Arising from the Randomization Process | Bias due to Deviations from Intended Interventions | Bias due to Missing Outcome Data | Bias in Measurement of the Outcome | Bias in Selection of the Reported Results | Overall Risk of Bias | |
| Magen [25] | Some concerns | Low | Low | Some concerns | Some concerns | Some concerns |
| Pawłowicz [26] | Some concerns | Low | Low | Low | Some concerns | Some concerns |
| Engin [10] | Some concerns | Low | Low | Some concerns | Some concerns | Some concerns |
| Morgan [29] | Low | Low | Low | Low | Some concerns | Some concerns |
| Authors (Ref No.) | Risk of Bias 2 Tool Assessment | |||||
|---|---|---|---|---|---|---|
| Bias Arising from the Randomization Process | Bias due to Deviations from Intended Interventions | Bias due to Missing Outcome Data | Bias in Measurement of the Outcome | Bias in Selection of the Reported Results | Overall Risk of Bias | |
| Gaig [24] | Some concerns | Low | Low | Low | Some concerns | Some concerns |
| Engin [10] | Some concerns | Low | Low | High | Some concerns | High |
| Rajan [28] | Some concerns | Low | High | High | Some concerns | High |
| Morgan [29] | Low | Low | Low | Low | Some concerns | Some concerns |
Appendix B
- MeSH descriptor: [Urticaria] explode all trees
- urticaria:ti,ab,kw (Word variations have been searched)
- hives:ti,ab,kw (Word variations have been searched)
- 1. OR 2. OR 3.
- MeSH descriptor:[Anti-Bacterial Agents]explode all tree
- 6 (antibiotic* or antibacteri* or anti* bacter* or bacteriocid* or bactericid* or anti*microbial or ciprofloxacin or metronidazole or levamisole or ornidazole or fusidin or rifaximin or vancomycin or fusidic acid or nitazoxanide or teicoplanin or rifampicin or bacitracin or fidaxomicin or amoxicillin or azithromycin or cephalosporin* or cephalexin or clarithromycin or clindamycin or doxycycline or erythromycin or fluoroquinolone* or levofloxacin or macrolide* or nitrofurantoin or penicillin or tetracycline or trimethoprim or dapsone):ti,ab,kw (Word variations have been searched)
- 5. OR 6
- MeSH descriptor: [Helicobacter] explode all trees
- MeSH descriptor: [Helicobacter Infections] explode all trees
- MeSH descriptor: [Helicobacter pylori] explode all trees
- 11 (helicobacter or pylori or pyloridis or Campylobacter):ti,ab,kw (Word variations have been searched)
- 8. OR 9. OR 10. OR 11.
- 13 7. OR 12.
- 4. AND 13.
- exp Urticaria/
- urticaria.tw.
- hives.tw.
- or/1–3
- exp Anti-bacterial Agents/
- (antibiotic$ or antibacteri$ or anti$bacter$ or bacteriocid$ or bactericid$ or anti$microbial or ciprofloxacin or metronidazole or levamisole or ornidazole or fusidin or rifaximin or vancomycin or fusidic acid or nitazoxanide or teicoplanin or rifampicin or bacitracin or fidaxomicin or amoxicillin or azithromycin or cephalosporin$ or cephalexin or clarithromycin or clindamycin or doxycycline or erythromycin or fluoroquinolone$ or levofloxacin or macrolide$ or nitrofurantoin or penicillin or tetracycline or trimethoprim or dapsone).tw.
- or/5–6
- exp Helicobacter pylori/ or exp Helicobacter/ or exp Helicobacter infection/
- (pylori or pyloridis or HP).tw.
- (helicobacter or Campylobacter).tw.
- or/8–10
- 7 or 11
- 4 and 12
- ((randomized controlled trial or controlled clinical trial).pt. or randomized.ab. or randomised.ab. or placebo.ab. or drug therapy.fs. or randomly.ab. or trial.ab. or groups.ab.) not (exp animals/ not humans.sh.)
- 13 and 14
- S1. EMB.EXACT.EXPLODE(“chronic urticaria”)
- S2. (ab(urticaria) OR ti(urticaria))
- S3. (ab(hives) OR ti(hives))
- S4. S1 OR S2 OR S3
- S5. EMB.EXACT.EXPLODE(“antibiotic agent”)
- S6. (ab(antibiotic) OR ti(antibiotic) OR ab(antibiotics) OR ti(antibiotics))
- S7. (ab(antibacterial) OR ti(antibacterial) OR ab(anti bacteral) OR ti(anti bacteral))
- S8. (ab(bacteriocidal) OR ti(bacteriocidal) OR ab(bactericidal) OR ti(bactericidal) OR ab(anti microbial) OR ti(anti microbial))
- S9. (ab(ciprofloxacin) OR ti(ciprofloxacin) OR ab(metronidazole) OR ti(metronidazole) OR ab(levamisole) OR ti(levamisole) OR ab(ornidazole) OR ti(ornidazole) OR ab(fusidin) OR ti(fusidin) OR ab(rifaximin) OR ti(rifaximin) OR ab(vancomycin) OR ti(vancomycin) OR ab(fusidic acid) OR ti(fusidic acid) OR ab(nitazoxanide) OR ti(nitazoxanide) OR ab(teicoplanin) OR ti(teicoplanin) OR ab(rifampicin) OR ti(rifampicin) OR ab(bacitracin) OR ti(bacitracin) OR ab(fidaxomicin) OR ti(fidaxomicin) OR ab(amoxicillin) OR ti(amoxicillin) OR ab(azithromycin) OR ti(azithromycin) OR ab(cephalosporin) OR ti(cephalosporin) OR ab(cephalosporinic) OR ti(cephalosporinic) OR ab(cephalexin) OR ti(cephalexin) OR ab(clarithromycin) OR ti(clarithromycin) OR ab(clindamycin) OR ti(clindamycin) OR ab(doxycycline) OR ti(doxycycline) OR ab(erythromycin) OR ti(erythromycin) OR ab(flouroquinolone) OR ti(flouroquinolone) OR ab(levofloxacin) OR ti(levofloxacin) OR ab(macrolide) OR ti(macrolide) OR ab(nitrofurantoin) OR ti(nitrofurantoin) OR ab(penicillin) OR ti(penicillin) OR ab(tetracycline) OR ti(tetracycline) OR ab(trimethoprim) OR ti(trimethoprim) OR ab(dapsone) OR ti(dapsone))
- S10. S5 OR S6 OR S7 OR S8 OR S9
- S11. EMB.EXACT.EXPLODE(“Helicobacter pylori”)
- S12. EMB.EXACT.EXPLODE(“Helicobacter”)
- S13. EMB.EXACT.EXPLODE(“Helicobacter infection”)
- S14. (ab(pylori or pyloridis or HP) OR ti(pylori or pyloridis or HP))
- S15. (ab(helicobacter or Campylobacter) OR ti(helicobacter or Campylobacter))
- S16. S11 OR S12 OR S13 OR S14 OR S15
- S17. S10 OR S16
- S18. S4 AND S17
- S19. (ab(random*) OR ti(random*)) OR (ab(placebo*) OR ti(placebo*)) OR (ab(double NEAR/1 blind*) OR ti(double NEAR/1 blind*))
- S20. S18 AND S19
References
- Leech, S.; Grattan, C.; Lloyd, K.; Deacock, S.; Williams, L.; Langford, A.; Warner, J. The RCPCH care pathway for children with Urticaria, Angio-oedema or Mastocytosis: An evidence and consensus based national approach. Arch. Dis. Child. 2011, 96, i34–i37. [Google Scholar] [CrossRef]
- Powell, R.J.; Leech, S.C.; Till, S.; Huber, P.A.J.; Nasser, S.M.; Clark, A. BSACI guideline for the management of chronic urticaria and angioedema. Clin. Exp. Allergy 2015, 45, 547–565. [Google Scholar] [CrossRef] [PubMed]
- Zuberbier, T.; Aberer, W.; Asero, R.; Abdul Latiff, A.H.; Baker, D.; Ballmer-Weber, B.; Bernstein, J.A.; Bindslev-Jensen, C.; Brzoza, Z.; Buense Bedrikow, R.; et al. The EAACI/GA2LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy 2018, 73, 1393–1414. [Google Scholar] [CrossRef] [PubMed]
- Poddighe, D. The prevalence of chronic spontaneous urticaria (CSU) in the pediatric population. J. Am. Acad. Dermatol. 2019, 81, e149. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, S.S.; Sánchez-Borges, M. Chronic Urticaria: Comparisons of US, European, and Asian Guidelines. Curr. Allergy Asthma Rep. 2018, 18, 36. [Google Scholar] [CrossRef] [PubMed]
- Shakouri, A.; Compalati, E.; Lang, D.M.; A Khan, D. Effectiveness of Helicobacter pylori eradication in chronic urticaria: Evidence-based analysis using the Grading of Recommendations Assessment, Development, and Evaluation system. Curr. Opin. Allergy Clin. Immunol. 2010, 10, 362–369. [Google Scholar] [CrossRef]
- Cornillier, H.; Giraudeau, B.; Munck, S.; Hacard, F.; Jonville-Bera, A.-P.; D’Acremont, G.; Pham, B.-N.; Maruani, A. Chronic spontaneous urticaria in children—A systematic review on interventions and comorbidities. Pediatr. Allergy Immunol. 2018, 29, 303–310. [Google Scholar] [CrossRef]
- Kim, H.J.; Kim, Y.-J.; Lee, H.J.; Hong, J.Y.; Park, A.Y.; Chung, E.H.; Lee, S.Y.; Lee, J.S.; Park, Y.L.; Lee, S.H.; et al. Systematic review and meta-analysis: Effect of Helicobacter pylori eradication on chronic spontaneous urticaria. Helicobacter 2019, 24, e12661. [Google Scholar] [CrossRef]
- Akashi, R.; Ishiguro, N.; Shimizu, S.; Kawashima, M. Clinical study of the relationship between Helicobacter pylori and chronic urticaria and prurigo chronica multiformis: Effectiveness of eradication therapy for Helicobacter pylori. J. Dermatol. 2010, 38, 761–766. [Google Scholar] [CrossRef]
- Engin, B.; Özdemir, M. Prospective randomized non-blinded clinical trial on the use of dapsone plus antihistamine vs. antihistamine in patients with chronic idiopathic urticaria. J. Eur. Acad. Dermatol. Venereol. 2008, 22, 481–486. [Google Scholar] [CrossRef]
- González, P.; Soriano, V.; Caballero, T.; Niveiro, E. Idiopatic angioedema treated with dapsone. Allergol. Immunopathol. 2005, 33, 54–56. [Google Scholar] [CrossRef] [PubMed]
- Eiser, A.R.; Singh, P.; Shanies, H.M. Sustained dapsone-induced remission of hypocomplementemic urticarial vasculitis—A case report. Angiology 1997, 48, 1019–1022. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.D.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Health Care Interventions: Explanation and Elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Kimko, H.H.C.; Thyssen, A.; Mould, D.R.; Mannaert, E.; Treem, W.R. Helicobacter pyloritreatment in children: Defining a dose for rabeprazole as a part of a triple therapy regimen. J. Clin. Pharmacol. 2015, 55, 592–600. [Google Scholar] [CrossRef]
- Cumpston, M.; Li, T.; Page, M.J.; Chandler, J.; A Welch, V.; Higgins, J.P.; Thomas, J. Updated guidance for trusted systematic reviews: A new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst. Rev. 2019, 10, ED000142. [Google Scholar] [CrossRef]
- Guyatt, G.; Oxman, A.D.; Akl, E.A.; Kunz, R.; Vist, G.; Brozek, J.; Norris, S.; Falck-Ytter, Y.; Glasziou, P.; Debeer, H. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J. Clin. Epidemiol. 2011, 64, 383–394. [Google Scholar] [CrossRef]
- Pasricha, J.S. Therapeutic Effect of Anti- Bacterial Agents in Urticaria. Indian J. Dermatol. Venereol. Leprol. 1979, 45, 344–347. [Google Scholar]
- Gorczyza, M.; Schoepke, N.; Krause, K.; Hawro, T.; Maurer, M. Patients with chronic cold urticaria may benefit from doxycycline therapy. Br. J. Dermatol. 2016, 176, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.-L.; Jia, Q.-L.; Liu, P.-H.; Jin, W.-J.; Zhou, Y.; Wang, L.-X.; Gao, X.-G. Efficacy observation on acupoint catgut embedding therapy combined medication for treatment of chronic urticaria induced by Helicobacter pylori infection. Zhongguo Zhen Jiu Chin. Acupunct. Moxibustion 2010, 30, 993–996. [Google Scholar]
- Feizollah, F. Study of the effect of medications used to treat Helicobacter pylori infection on quality of life in chronic idiopathic urticaria. 2016. Available online: https://en.irct.ir/trial/13988 (accessed on 23 December 2020).
- Akelma, A.; Cizmeci, M.; Mete, E.; Tufan, N.; Bozkurt, B. A neglected cause for chronic spontaneous urticaria in children: Helicobacter pylori. Allergol. Immunopathol. 2015, 43, 259–263. [Google Scholar] [CrossRef] [PubMed]
- Valsecchi, R.; Pigatto, P. Chronic urticaria and Helicobacter pylori. Acta Derm. Venereol. 1998, 78, 440–442. [Google Scholar]
- Schnyder, B.; Helbling, A.; Pichler, W.J. Chronic Idiopathic Urticaria: Natural Course and Association with Helicobacter pylori Infection. Int. Arch. Allergy Immunol. 1999, 119, 60–63. [Google Scholar] [CrossRef]
- Gaig, P.; García-Ortega, P.; Enrique, E.; Papo, M.; Quer, J.; Richard, C. Efficacy of the eradication of Helicobacter pylori infection in patients with chronic urticaria. A placebo-controlled double blind study. Allergol. Immunopathol. 2002, 30, 255–258. [Google Scholar] [CrossRef]
- Magen, E.; Mishal, J.; Schlesinger, M.; Scharf, S. Eradication of Helicobacter pylori Infection Equally Improves Chronic Urticaria With Positive and Negative Autologous Serum Skin Test. Helicobacter 2007, 12, 567–571. [Google Scholar] [CrossRef] [PubMed]
- Pawłowicz, R.; Wytrychowski, K.; Panaszek, B. Eradication of Helicobacter pylori, as add-on therapy, has a significant, but temporary influence on recovery in chronic idiopathic urticaria: A placebo-controlled, double blind trial in the Polish population. Adv. Dermatol. Allergol. 2018, 35, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Elhendawy, M.; Hagras, M.M.; Soliman, S.S.; E Shaker, E.S. Positive Effect of Helicobacter pylori Treatment on Outcome of Patients With Chronic Spontaneous Urticaria. Am. J. Clin. Pathol. 2020, 134. [Google Scholar] [CrossRef]
- Rajan, N.; Darne, S.; Ah-Weng, A.; Carmichael, A. Dapsone as adjuvant treatment in chronic ordinary urticaria: Positive implications for quality of life. Br. J. Dermatol. 2010, 163, 49. [Google Scholar]
- Morgan, M.; Cooke, A.; Rogers, L.; Adams-Huet, B.; Khan, D.A. Double-Blind Placebo-Controlled Trial of Dapsone in Antihistamine Refractory Chronic Idiopathic Urticaria. J. Allergy Clin. Immunol. Pr. 2014, 2, 601–606. [Google Scholar] [CrossRef]
- De Amici, M.; Marseglia, G.L. Spontaneous (Autoimmune) Chronic Urticaria in Children: Current Evidences, Diagnostic Pitfalls and Therapeutic Management. Recent Patents Inflamm. Allergy Drug Discov. 2016, 10, 34–39. [Google Scholar] [CrossRef]
- Kohli, S.; Mahajan, V.K.; Rana, B.S.; Mehta, K.S.; Raina, R.K.; Chauhan, P.S.; Sharma, V.; Rawat, R. Clinicoepidemiologic Features of Chronic Urticaria in Patients with versus without Subclinical Helicobacter pylori Infection: A Cross-Sectional Study of 150 Patients. Int. Arch. Allergy Immunol. 2018, 175, 114–120. [Google Scholar] [CrossRef]
- Bansal, C.J.; Bansal, A.S. Stress, pseudoallergens, autoimmunity, infection and inflammation in chronic spontaneous urticaria. Allergy Asthma Clin. Immunol. 2019, 15, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Desai, A.; Jung, M.-Y.; Olivera, A.; Gilfillan, A.M.; Prussin, C.; Kirshenbaum, A.S.; Beaven, M.A.; Metcalfe, D.D. IL-6 promotes an increase in human mast cell numbers and reactivity through suppression of suppressor of cytokine signaling 3. J. Allergy Clin. Immunol. 2016, 137, 1863–1871.e6. [Google Scholar] [CrossRef] [PubMed]
- Varghese, R.; Rajappa, M.; Chandrashekar, L.; Kattimani, S.; Archana, M.; Munisamy, M.; Revathy, G.; Thappa, D.M. Association among stress, hypocortisolism, systemic inflammation, and disease severity in chronic urticaria. Ann. Allergy Asthma Immunol. 2016, 116, 344–348.e1. [Google Scholar] [CrossRef] [PubMed]
- Ivetić Tkalčević, V.; Čužić, S.; Kramarić, M.D.; Parnham, M.J.; Haber, V.E. Topical Azithromycin and Clarithromycin Inhibit Acute and Chronic Skin Inflammation in Sensitized Mice, with Apparent Selectivity for Th2-Mediated Processes in Delayed-Type Hypersensitivity. Inflammation 2011, 35, 192–205. [Google Scholar] [CrossRef] [PubMed]
- Salem, I.; Ramser, A.; Isham, N.; Ghannoum, M.A. The Gut Microbiome as a Major Regulator of the Gut-Skin Axis. Front. Microbiol. 2018, 9, 1459. [Google Scholar] [CrossRef]
- Zhao, Y.; Gao, X.; Guo, J.; Yu, D.; Xiao, Y.; Wang, H.; Li, Y. Helicobacter pyloriinfection alters gastric and tongue coating microbial communities. Helicobacter 2019, 24, e12567. [Google Scholar] [CrossRef]
- Lu, T.; Chen, Y.; Guo, Y.; Sun, J.; Shen, W.; Yuan, M.; Zhang, S.; He, P.; Jiao, X. Altered Gut Microbiota Diversity and Composition in Chronic Urticaria. Dis. Markers 2019, 2019, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Nabizadeh, E.; Jazani, N.H.; Bagheri, M.; Shahabi, S. Association of altered gut microbiota composition with chronic urticaria. Ann. Allergy Asthma Immunol. 2017, 119, 48–53. [Google Scholar] [CrossRef]
- Rolig, A.S.; Cech, C.; Ahler, E.; Carter, J.E.; Ottemann, K.M. The Degree of Helicobacter pylori-Triggered Inflammation Is Manipulated by Preinfection Host Microbiota. Infect. Immun. 2013, 81, 1382–1389. [Google Scholar] [CrossRef]
- Tan, R.; Sun, H.; Zhang, W.; Yuan, H.; Li, B.; Yan, H.; Lan, C.; Yang, J.; Zhao, Z.; Wu, J. A 21-35 kDa Mixed Protein Component from Helicobacter pylori Activates Mast Cells Effectively in Chronic Spontaneous Urticaria. Helicobacter 2016, 21, 565–574. [Google Scholar] [CrossRef]
- Hong, G.U.; Ro, J.Y.; Bae, Y.; Kwon, I.-H.; Park, G.-H.; Choi, Y.H.; Choi, J.-H. Association of TG2 from mast cells and chronic spontaneous urticaria pathogenesis. Ann. Allergy Asthma Immunol. 2016, 117, 290–297. [Google Scholar] [CrossRef]
- O’Donnell, B.F.; Lawlor, F.; Simpson, J.; Morgan, M.; Greaves, M.W. The impact of chronic urticaria on the quality of life. Br. J. Dermatol. 1997, 136, 197–201. [Google Scholar] [CrossRef]
- Wozel, G.; Blasum, C. Dapsone in dermatology and beyond. Arch. Dermatol. Res. 2014, 306, 103–124. [Google Scholar] [CrossRef]
- Wozel, G.; Blasum, C.; Winter, C.; Gerlach, B. Dapsone hydroxylamine inhibits the LTB4-induced chemotaxis of polymorphonuclear leukocytes into human skin: Results of a pilot study. Inflamm. Res. 1997, 46, 420–422. [Google Scholar] [CrossRef]
- Wozel, G.; Lehmann, B. Dapsone Inhibits the Generation of 5-Lipoxygenase Products in Human Polymorphonuclear Leukocytes. Ski. Pharmacol. Physiol. 1995, 8, 196–202. [Google Scholar] [CrossRef] [PubMed]
- A Booth, S.; E Moody, C.; Dahl, M.V.; Herron, M.J.; Nelson, R.D. Dapsone Suppresses Integrin-Mediated Neutrophil Adherence Function. J. Investig. Dermatol. 1992, 98, 135–140. [Google Scholar] [CrossRef] [PubMed]
- Bonney, R.J.; Wightman, P.D.; Dahlgren, M.E.; Sadowski, S.J.; Davies, P.; Jensen, N.; Lanza, T.; Humes, J.L. Inhibition of the release of prostaglandins, leukotrienes and lysosomal acid hydrolases from macrophages by selective inhibitors of lecithin biosynthesis. Biochem. Pharmacol. 1983, 32, 361–366. [Google Scholar] [CrossRef]
- Du, L.J.; Chen, B.R.; Kim, J.J.; Kim, S.; Shen, J.H.; Dai, N. Helicobacter pylori eradication therapy for functional dyspepsia: Systematic review and meta-analysis. World J. Gastroenterol. 2016, 22, 3486–3495. [Google Scholar] [CrossRef] [PubMed]
- Chen, M.-J.; Chen, C.-C.; Chen, Y.-N.; Chen, C.-C.; Fang, Y.-J.; Lin, J.-T.; Wu, M.-S.; Liou, J.-M.; For the Taiwan Gastrointestinal Disease and Helicobacter Consortium. Systematic Review with Meta-Analysis: Concomitant Therapy vs. Triple Therapy for the First-Line Treatment of Helicobacter pylori Infection. Am. J. Gastroenterol. 2018, 113, 1444–1457. [Google Scholar] [CrossRef]
- Liou, J.-M.; Chen, C.-C.; Chang, C.-M.; Fang, Y.-J.; Bair, M.-J.; Chen, P.-Y.; Chang, C.-Y.; Hsu, Y.-C.; Chen, M.-J.; Chen, C.-C.; et al. Long-term changes of gut microbiota, antibiotic resistance, and metabolic parameters after Helicobacter pylori eradication: A multicentre, open-label, randomised trial. Lancet Infect. Dis. 2019, 19, 1109–1120. [Google Scholar] [CrossRef]



| Authors (Ref No.) | Year | Country | Subject No. | Age (Years) | Antibiotics (Months) | Control | Follow-Up (Months) | Eradication Rate (%) |
|---|---|---|---|---|---|---|---|---|
| Valsecchi [22] | 1998 | Italy | 65 | 24–61 | CMO (7) | No placebo | 12 | 93.5 |
| Schnyder [23] | 1999 | Switzerland | 11 | 34–73 | AL (14) | Placebo | 2 | 20.0 |
| Gaig [24] | 2002 | Spain | 16 | 27–55 | ACO (7) | Placebo | 1.5 | 100 |
| Magen [25] | 2007 | Israel | 78 | 42.5 (6.8) * | ACO (14) | No placebo | 4 | 86.7 |
| Pawłowicz [26] | 2018 | Poland | 64 | 42.8 (13.3) ** | ACO (7) | Placebo/no placebo | 6 | 91.7 |
| El-hendawy [27] | 2020 | Egypt | 27 | 30.9 (7.9) | ACO (14) | Placebo | 2 | 85.7 |
| Engin [10] | 2007 | Turkey | 65 | 16–60 | Dapsone | No Placebo | 6 | - |
| Rajan [28] | 2010 | United Kingdom | 13 | - | Dapsone | Placebo | 4 | - |
| Morgan [29] | 2014 | USA | 22 | 25–64 | Dapsone | Placebo | 1.5 | - |
| Authors (Ref No.) | Risk of Bias 2 Tool Assessment | |||||
|---|---|---|---|---|---|---|
| Bias Arising from the Randomization Process | Bias due to Deviations from Intended Interventions | Bias due to Missing Outcome Data | Bias in Measurement of the Outcome | Bias in Selection of the Reported Results | Overall Risk of Bias | |
| Valsecchi [22] | Some concerns | High | High | High | Some concerns | High |
| Schnyder [23] | Some concerns | Low | Low | Low | Some concerns | Some concerns |
| Gaig [24] | Some concerns | Low | Low | Low | Some concerns | Some concerns |
| Elhendawy [27] | Low | Low | Low | Low | Some concerns | Some concerns |
| Engin [10] | Low | Some concerns | Low | Some concerns | Some concerns | Some concerns |
| The Efficacy and Safety of Antibiotics for Chronic Spontaneous Urticaria | ||||||
|---|---|---|---|---|---|---|
| Patient or Population: Adults Setting: Chronic Spontaneous Urticaria Intervention: Antibiotics Comparison: Control | ||||||
| Outcomes | Anticipated Absolute Effects * (95% CI) | Relative Effect(95% CI) | Patient Number(Studies) | Certainty of the Evidence (GRADE) | Comments | |
| Risk with Control | Risk with Antibiotics | |||||
| Remission rate | 178 per 1000 | 421 per 1000 (153 to 1000) | RR = 2.37 (0.86 to 6.51) | 222 (5 RCTs) | Moderate a | The H. pylori eradication regimen likely increased the remission rate of chronic urticaria, but not dapsone. |
| Clinical improvement | - | SMD 3.59 SD higher (0.16 to 7.03) | - | 229 (4 RCTs) | Moderate a | Antibiotics (H. pylori eradication regimen and dapsone) likely increased the improvement of chronic urticaria. |
| Adverse events | 0% in a study of H. pylori eradication, 11.5% in 3 studies of dapsone. | 117 (5 RCTs) | Low a,b | Dapsone had mild adverse events, such as nausea, fatigue, and headache. | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Watanabe, J.; Shimamoto, J.; Kotani, K. The Effects of Antibiotics for Helicobacter pylori Eradication or Dapsone on Chronic Spontaneous Urticaria: A Systematic Review and Meta-Analysis. Antibiotics 2021, 10, 156. https://doi.org/10.3390/antibiotics10020156
Watanabe J, Shimamoto J, Kotani K. The Effects of Antibiotics for Helicobacter pylori Eradication or Dapsone on Chronic Spontaneous Urticaria: A Systematic Review and Meta-Analysis. Antibiotics. 2021; 10(2):156. https://doi.org/10.3390/antibiotics10020156
Chicago/Turabian StyleWatanabe, Jun, Junya Shimamoto, and Kazuhiko Kotani. 2021. "The Effects of Antibiotics for Helicobacter pylori Eradication or Dapsone on Chronic Spontaneous Urticaria: A Systematic Review and Meta-Analysis" Antibiotics 10, no. 2: 156. https://doi.org/10.3390/antibiotics10020156
APA StyleWatanabe, J., Shimamoto, J., & Kotani, K. (2021). The Effects of Antibiotics for Helicobacter pylori Eradication or Dapsone on Chronic Spontaneous Urticaria: A Systematic Review and Meta-Analysis. Antibiotics, 10(2), 156. https://doi.org/10.3390/antibiotics10020156







