Carbon Dot Nanoparticles Exert Inhibitory Effects on Human Platelets and Reduce Mortality in Mice with Acute Pulmonary Thromboembolism
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents
2.2. Preparation of CDOTs
2.3. Characterization of the Synthesized CDOTs
2.4. Preparation of Washed Human Platelets and Lactate Dehydrogenase (LDH) Release Assay
2.5. Platelet Aggregation
2.6. Western Blotting
2.7. Tail Bleeding Time in Mice
2.8. ADP-Induced Acute Pulmonary Thromboembolism in Mice
2.9. Statistical Analysis
3. Results
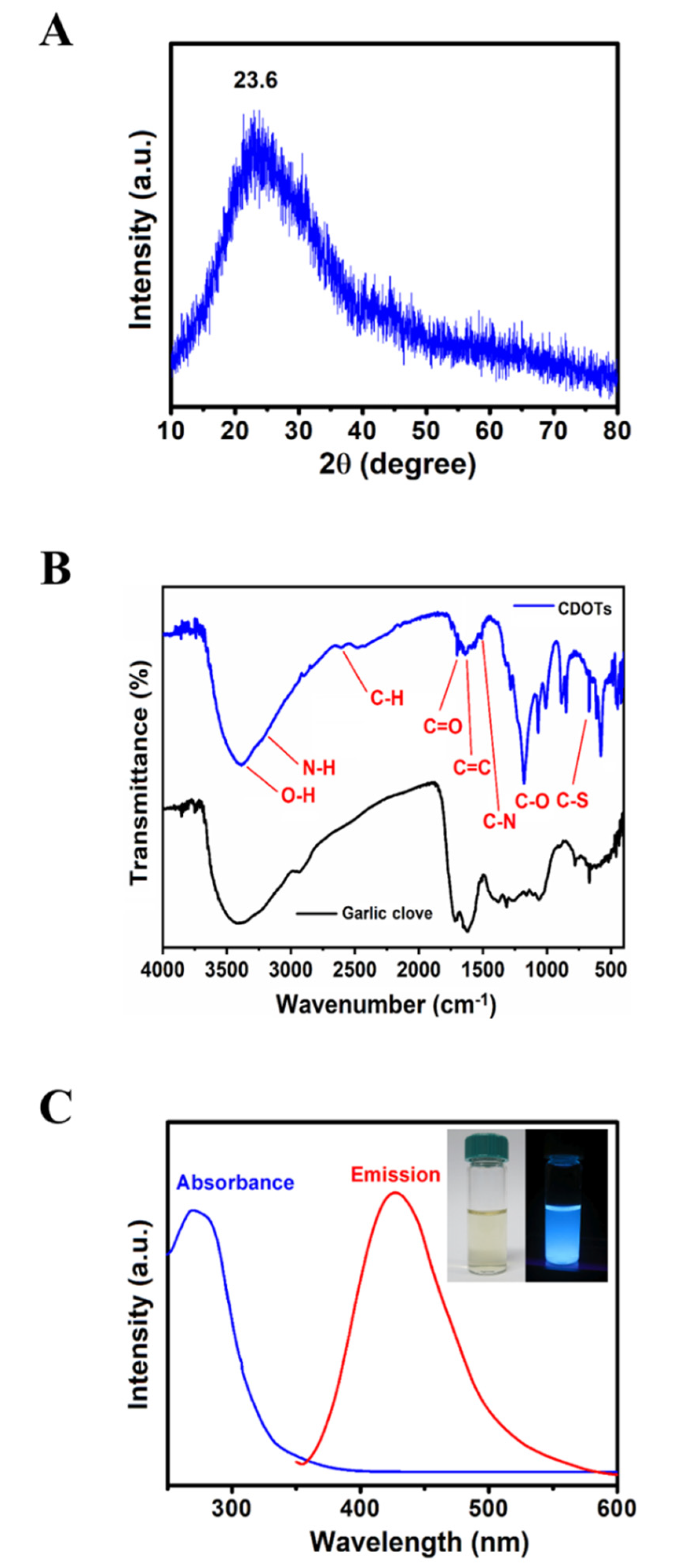
3.1. Characterization of the CDOTs
3.1.1. X-ray Diffraction Analysis
3.1.2. FT–IR
3.1.3. UV–vis Spectroscopy
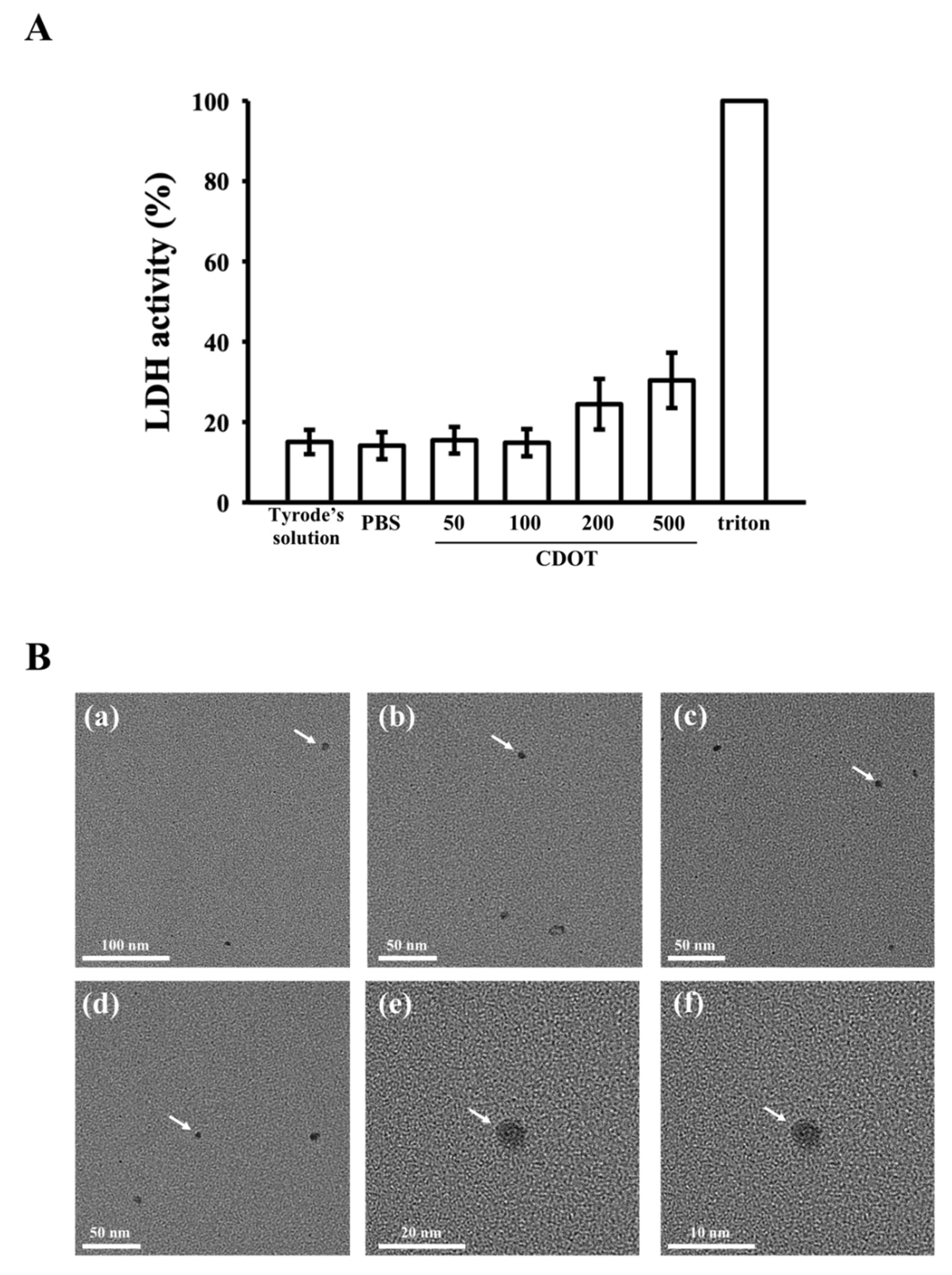
3.2. LDH Assay and FE-TEM
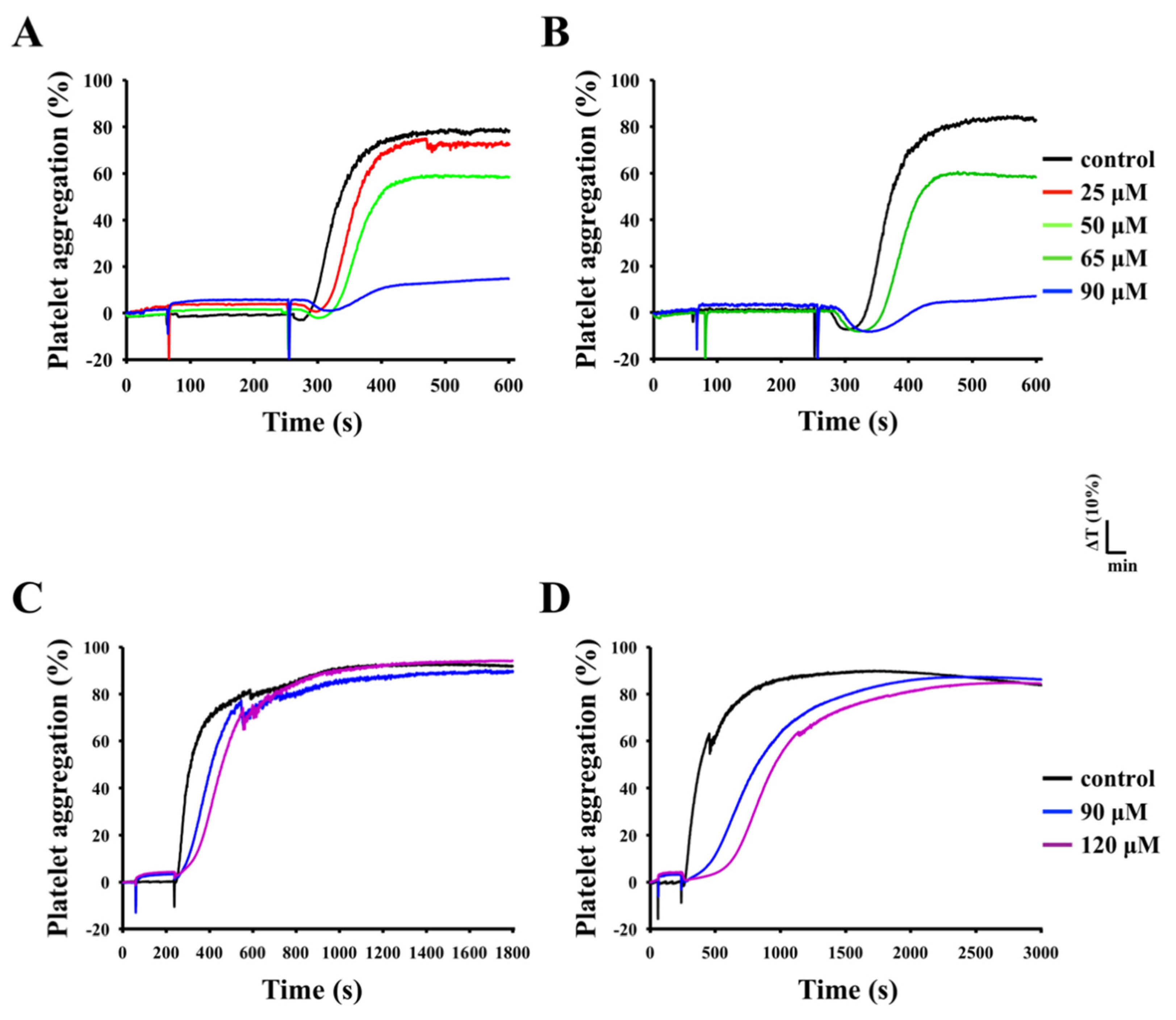
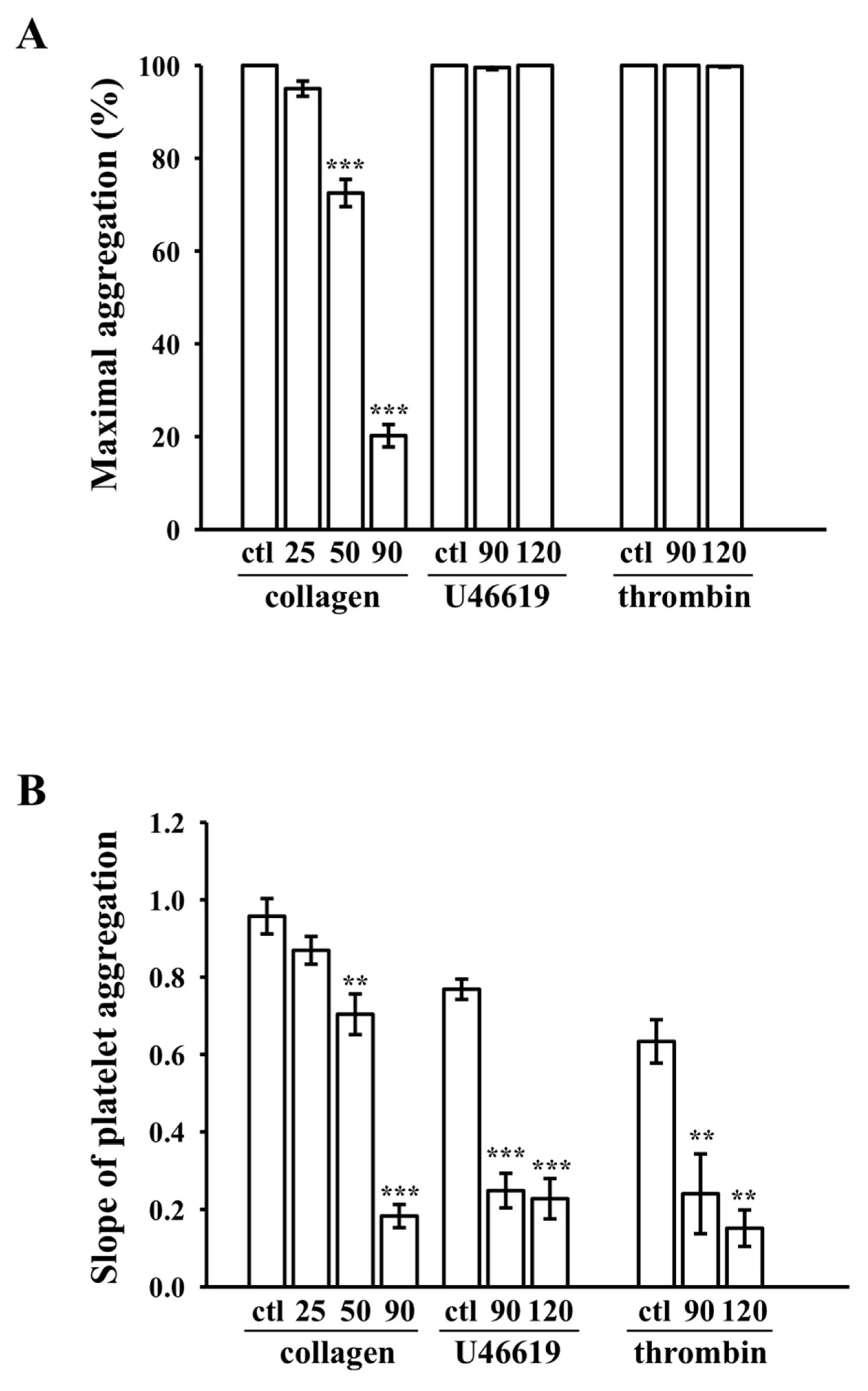
3.3. Inhibition of Platelet Aggregation Stimulated by Collagen
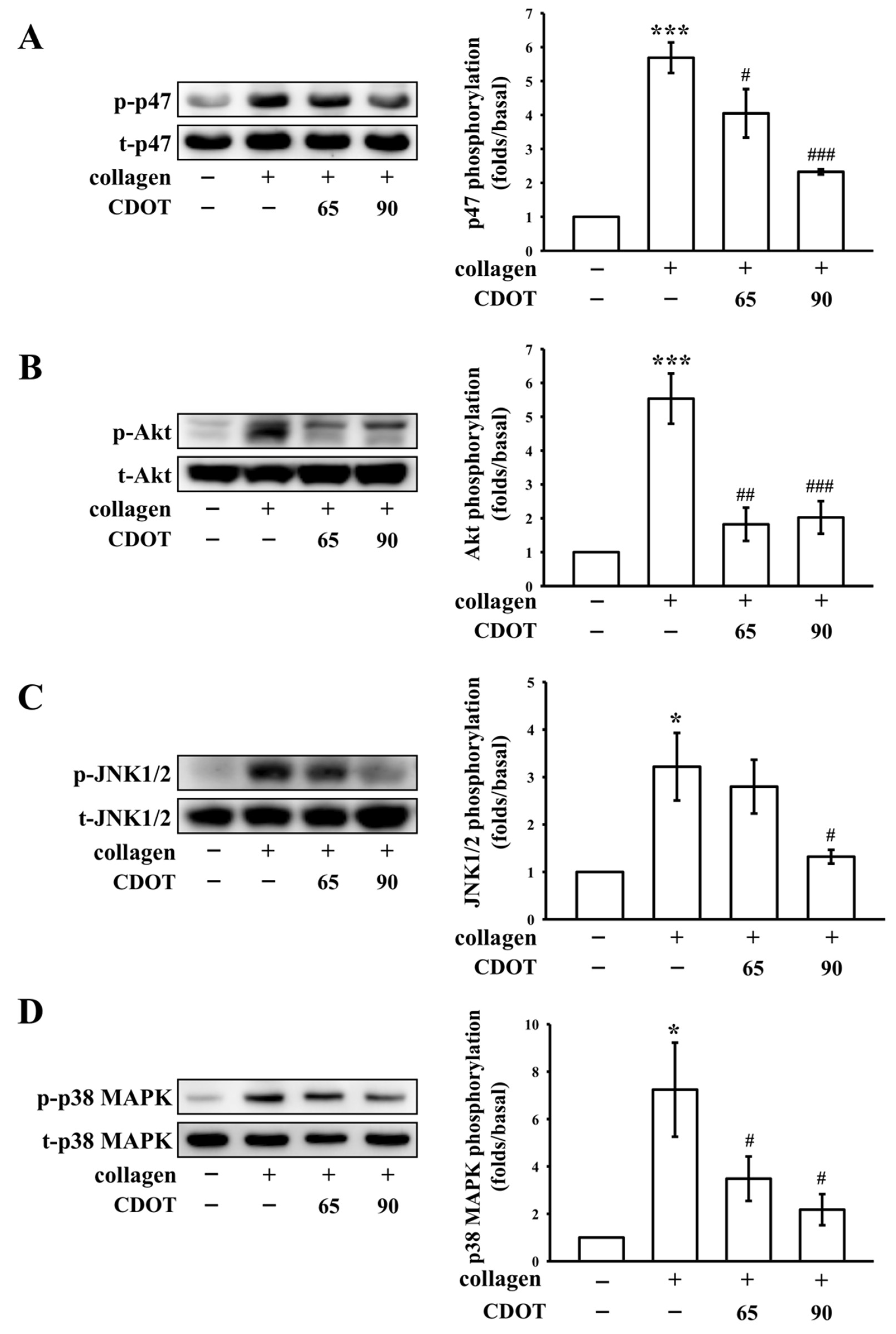
3.4. Inhibition of PKC Activation (p47; Pleckstrin) and Akt, JNK1/2, and p38 MAPK Phosphorylation
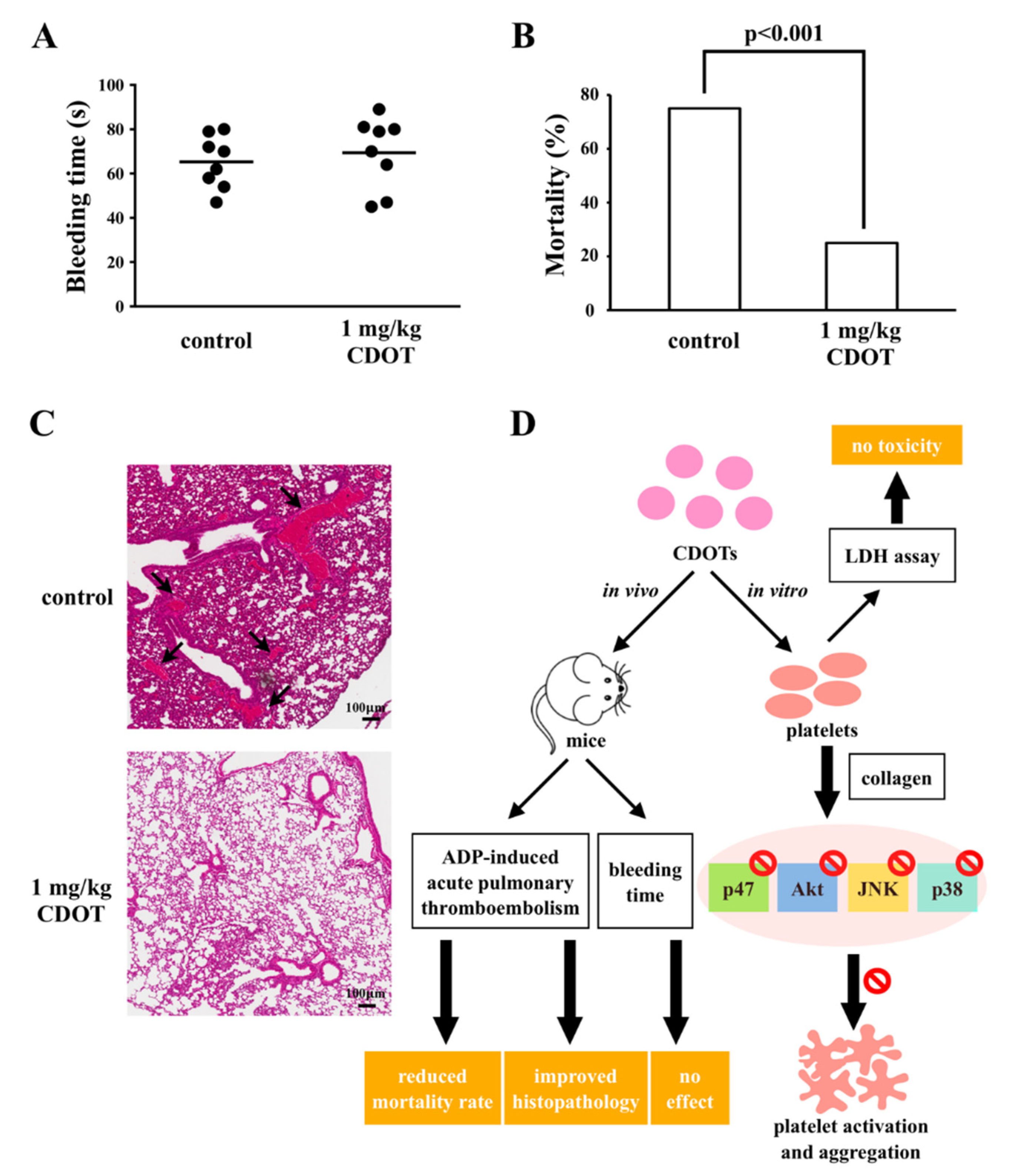
3.5. Effects of the CDOTs on Tail Bleeding and Mortality in Mice with ADP-Induced Pulmonary Thromboembolism
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Watson, R.D.; Chin, B.S.; Lip, G.Y. Antithrombotic therapy in acute coronary syndromes. Br. Med. J. 2002, 325, 1348–1351. [Google Scholar] [CrossRef] [PubMed]
- Baruah, D.B.; Dash, R.N.; Chaudhari, M.R.; Kadam, S.S. Plasminogen activators: A comparison. Vasc. Pharmacol. 2006, 44, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Almoosa, K. Is Thrombolytic therapy effective for pulmonary embolism. Am. Fam. Physician 2002, 65, 1097–1102. [Google Scholar] [PubMed]
- Maxwell, M.J.; Yuan, Y.; Anderson, K.E.; Hibbs, M.L.; Salem, H.H.; Jackson, S.P. SHIP1 and Lyn Kinase negatively regulate integrin αIIbβ3 signaling in platelets. J. Biol. Chem. 2004, 279, 32196–32204. [Google Scholar] [CrossRef] [PubMed]
- Scuri, M.; Chen, B.T.; Castranova, V.; Reynolds, J.S.; Johnson, V.J.; Samsell, L.; Walton, C.; Piedmonte, G. Effects of titanium dioxide nanoparticle exposure on neuroimmuneresponses in rat airways. J. Toxicol. Environ. Health A 2010, 73, 1353–1369. [Google Scholar] [CrossRef] [PubMed]
- Buffle, J. The key role of environmental colloids/nanoparticles for the sustainability of life. Environ. Chem. 2006, 3, 155–158. [Google Scholar] [CrossRef]
- Hasan, A.; Morshed, M.; Memic, A.; Hassan, S.; Webster, T.J.; Marei, H.E. Nanoparticles in tissue engineering: Applications, challenges and prospects. Int. J. Nanomed. 2018, 13, 5637–5655. [Google Scholar] [CrossRef]
- Berry, J.P.; Arnoux, B.; Stanislas, G.; Galle, P.; Chretien, J. A microanalytic study of particles transport across the alveoli: Role of blood platelets. Biomedicine 1977, 27, 354–357. [Google Scholar]
- Gaffney, A.M.; Santos-Martinez, M.J.; Satti, A.; Major, T.C.; Wynne, K.J.; Gun’ko, Y.K.; Annich, G.M.; Elia, G.; Radomski, M.W. Blood biocompatibility of surface-bound multi-walled carbon nanotubes. Nanomedicine 2015, 11, 39–46. [Google Scholar] [CrossRef]
- Anselmo, A.C.; Modery-Pawlowski, C.L.; Menegatti, S.; Kumar, S.; Vogus, D.R.; Tian, L.L.; Chen, M.; Squires, T.M.; Sen Gupta, A.; Mitragotri, S. Platelet-like nanoparticles: Mimicking shape, flexibility, and surface biology of platelets to target vascular injuries. ACS Nano 2014, 8, 11243–11253. [Google Scholar] [CrossRef]
- Roy, S.C.; Paulose, M.; Grimes, C.A. The effect of TiO2 nanotubes in the enhancement of blood clotting for the control of hemorrhage. Biomaterials 2007, 28, 4667–4672. [Google Scholar] [CrossRef]
- Gayen, B.; Palchoudhury, S.; Chowdhury, J. Carbon dots: A mystic star in the world of nanoscience. J. Nanomater. 2019, 2019, 19. [Google Scholar] [CrossRef]
- Lim, S.Y.; Shen, W.; Gao, Z. Carbon quantum dots and their applications. Chem. Soc. Rev. 2015, 44, 362–381. [Google Scholar] [CrossRef] [PubMed]
- Zuo, J.; Jiang, T.; Zhao, X.; Xiong, X.; Xiao, S.; Zhu, Z. Preparation and application of fluorescent carbon dots. J. Nanomater. 2015, 2015, 1–13. [Google Scholar] [CrossRef]
- Wang, R.; Lu, K.-Q.; Tang, Z.-R.; Xu, Y.-J. Recent progress in carbon quantum dots: Synthesis, properties and applications in photocatalysis. J. Mater. Chem. A 2017, 5, 3717–3734. [Google Scholar] [CrossRef]
- Yan, X.; Zhao, Y.; Luo, J.; Xiong, W.; Liu, X.; Cheng, J.; Wang, Y.; Zhang, M.; Qu, H. Hemostatic bioactivity of novel Pollen Typhae Carbonisata-derived carbon quantum dots. J. Nanobiotechnol. 2017, 15, 60. [Google Scholar] [CrossRef] [PubMed]
- Zhao, Y.; Zhang, Y.; Liu, X.; Kong, H.; Wang, Y.; Qin, G.; Cao, P.; Song, X.; Yan, X.; Wang, Q.; et al. Novel carbon quantum dots from egg yolk oil and their haemostatic effects. Sci. Rep. 2017, 7, 4452. [Google Scholar] [CrossRef]
- Liu, X.; Wang, Y.; Yan, X.; Zhang, M.; Zhang, Y.; Cheng, J.; Lu, F.; Qu, H.; Wang, Q.; Zhao, Y. Novel phellodendri cortex (huang bo)-derived carbon dots and their hemostatic effect. Nanomedicine 2018, 13, 391–405. [Google Scholar] [CrossRef]
- Fedel, M. Hemocompatibility of carbon nanostructures. C J. Carbon Res. 2020, 6, 12. [Google Scholar] [CrossRef]
- Sheu, J.R.; Lee, C.R.; Lin, C.H.; Hsiao, G.; Ko, W.C.; Chen, Y.C.; Yen, M.H. Mechanisms involved in the antiplatelet activity of Staphylococcus aureus lipoteichoic acid in human platelets. Thromb. Haemost. 2000, 83, 777–784. [Google Scholar]
- Lu, W.J.; Lee, J.J.; Chou, D.S.; Jayakumar, T.; Fong, T.H.; Hsiao, G.; Sheu, J.R. A novel role of andrographolide, an NF-κB inhibitor, on inhibition of platelet activation: The pivotal mechanisms of endothelial nitric oxide synthase/cyclic GMP. J. Mol. Med. 2011, 89, 1261–1273. [Google Scholar] [CrossRef] [PubMed]
- Zhu, C.; Zhai, J.; Dong, S. Bifunctional fluorescent carbon nanodots: Green synthesis via soy milk and application as metal-free electrocatalysts for oxygen reduction. Chem. Commun. (Camb.) 2012, 48, 9367–9369. [Google Scholar] [CrossRef]
- Alkian, I.; Prasetio, A.; Anggara, L.; Karnaji; Fonisyah, M.H.; Rizka, Z.M.; Widiyandari, H. A facile microwave-assisted synthesis of carbon dots and their application as sensitizers in nanocrystalline TiO2 solar cells. J. Phys. Conf. Ser. 2019, 1204, 012093. [Google Scholar] [CrossRef]
- Wu, Z.L.; Zhang, P.; Gao, M.X.; Liu, C.F.; Wang, W.; Leng, F.; Huang, C.Z. One-pot hydrothermal synthesis of highly luminescent nitrogen-doped amphoteric carbon dots for bioimaging from bombyx mori silk—Natural proteins. J. Mater. Chem. B 2013, 1, 2868–2873. [Google Scholar] [CrossRef] [PubMed]
- Zhao, S.; Lan, M.; Zhu, X.; Xue, H.; Ng, T.W.; Meng, X.; Lee, C.S.; Wang, P.; Zhang, W. Green synthesis of bifunctional fluorescent carbon dots from garlic for cellular imaging and free radical scavenging. ACS Appl. Mater. Interfaces 2015, 7, 17054–17060. [Google Scholar] [CrossRef]
- Woulfe, D.S. Akt signaling in platelet and thrombosis. Expert Rev. Hematol. 2010, 3, 81–91. [Google Scholar] [CrossRef]
- Bugaud, F.; Nadal-Wollbold, F.; Levy-Toledano, S.; Rosa, J.P.; Bryckaert, M. Regulation of c-jun-NH2 terminal kinase and extracellular-signal regulated kinase in human platelets. Blood 1999, 94, 3800–3805. [Google Scholar] [CrossRef] [PubMed]
- Shrivastava, S.; Bera, T.; Singh, S.K.; Singh, G.; Ramachandrarao, P.; Dash, D. Characterization of antiplatelet properties of silver nanoparticles. ACS Nano 2009, 3, 1357–1364. [Google Scholar] [CrossRef]
- Krishnaraj, R.N.; Berchmans, S. In vitro antiplatelet activity of silver nanoparticles synthesized using the microorganism Gluconobacter roseus: An AFM-based study. RSC Adv. 2013, 3, 8953–8959. [Google Scholar] [CrossRef]
- Hajtuch, J.; Hante, N.; Tomczyk, E.; Wojcik, M.; Radomski, M.W.; Santos-Martinez, M.J.; Inkielewicz-Stepniak, I. Effects of functionalized silver nanoparticles on aggregation of human blood platelets. Int. J. Nanomed. 2019, 14, 7399–7417. [Google Scholar] [CrossRef]
- Love, S.A.; Thompson, J.W.; Haynes, C.L. Development of screening assays for nanoparticle toxicity assessment in human blood: Preliminary studies with charged Au nanoparticles. Nanomedicine 2012, 7, 1355–1364. [Google Scholar] [CrossRef] [PubMed]
- Deb, S.; Patra, H.K.; Lahiri, P.; Dasgupta, A.K.; Chakrabarti, K.; Chaudhuri, U. Multistability in platelets and their response to gold nanoparticles. Nanomedicine 2011, 7, 376–384. [Google Scholar] [CrossRef] [PubMed]
- Jun, E.A.; Lim, K.M.; Kim, K.; Bae, O.N.; Noh, J.Y.; Chung, K.H.; Chung, J.H. Silver nanoparticles enhance thrombus formation through increased platelet aggregation and procoagulant activity. Nanotoxicology 2011, 5, 157–167. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.; Lai, W.; Cui, M.; Liang, L.; Lin, Y.; Fang, Q.; Liu, Y.; Xie, L. An evaluation of blood compatibility of silver nanoparticles. Sci. Rep. 2016, 6, 255180. [Google Scholar] [CrossRef] [PubMed]
- Ragaseema, V.M.; Unnikrishnan, S.; Kalliyana Krishnan, V.; Krishnan, L.K. The antithrombotic and antimicrobial properties of PEG-protected silver nanoparticle coated surfaces. Biomaterials 2012, 33, 3083–3092. [Google Scholar] [CrossRef] [PubMed]
- Singer, W.D.; Brown, H.A.; Sternweis, P.C. Regulation of eukaryotic phosphatidylinositol-specific phospholipase C and phospholipase D. Ann. Rev. Biochem. 1997, 66, 475–509. [Google Scholar] [CrossRef]
- Fan, X.; Wang, C.; Shi, P.; Gao, W.; Gu, J.; Geng, Y.; Yang, W.; Wu, N.; Wang, Y.; Xu, Y.; et al. Platelet MEKK3 regulates arterial thrombosis and myocardial infarct expansion in mice. Blood Adv. 2018, 2, 1439–1448. [Google Scholar] [CrossRef]
- Mazharian, A.; Roger, S.; Berrou, E.; Adam, F.; Kauskot, A.; Nurden, P.; Jandrot-Perrus, M.; Bryckaert, M. Protease-activating receptor-4 induces full platelet spreading on a fibrinogen matrix: Involvement of ERK2 and p38 and Ca2+ mobilization. J. Biol. Chem. 2007, 282, 5478–5487. [Google Scholar] [CrossRef]
- Adam, F.; Kauskot, A.; Nurden, P.; Sulpice, E.; Hoylaerts, M.F.; Davis, R.J.; Rosa, J.P.; Bryckaert, M. Platelet JNK1 is involved in secretion and thrombus formation. Blood 2010, 115, 4083–4092. [Google Scholar] [CrossRef]
- Adam, F.; Kauskot, A.; Rosa, J.P.; Bryckaert, M. Mitogen-activated protein kinases in hemostasis and thrombosis. J. Thromb. Haemost. 2008, 6, 2007–2016. [Google Scholar] [CrossRef]
- Guo, C.; Xia, Y.; Niu, P.; Jiang, L.; Duan, J.; Yu, Y.; Zhou, X.; Li, Y.; Sun, Z. Silica nanoparticles induce oxidative stress, inflammation, and endothelial dysfunction in vitro via activation of the mapk/nrf2 pathway and nuclear factor-kappab signaling. Int. J. Nanomed. 2015, 10, 1463–1477. [Google Scholar] [CrossRef] [PubMed]
- Miller, V.M.; Hunter, L.W.; Chu, K.; Kaul, V.; Squillace, P.D.; Lieske, J.C.; Jayachandran, M. Biologic nanoparticles and platelet reactivity. Nanomedicine 2009, 4, 725–733. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.S.; Kim, J.S.; Cho, H.S.; Rha, D.S.; Kim, J.M.; Park, J.D.; Choi, B.S.; Lim, R.; Chang, H.K.; Chung, Y.H.; et al. Twenty-eight-day oral toxicity, genotoxicity, and gender-related tissue distribution of silver nanoparticles in Sprague-Dawley rats. Inhal. Toxicol. 2008, 20, 575–583. [Google Scholar] [CrossRef] [PubMed]
- Tian, Y.; Zhao, Y.; Zheng, W.; Zhang, W.; Jiang, X. Antithrombotic functions of small molecule-capped gold nanoparticles. Nanoscale 2014, 6, 8543–8550. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, T.-Y.; Jayakumar, T.; Thanasekaran, P.; Lin, K.-C.; Chen, H.-M.; Veerakumar, P.; Sheu, J.-R. Carbon Dot Nanoparticles Exert Inhibitory Effects on Human Platelets and Reduce Mortality in Mice with Acute Pulmonary Thromboembolism. Nanomaterials 2020, 10, 1254. https://doi.org/10.3390/nano10071254
Lee T-Y, Jayakumar T, Thanasekaran P, Lin K-C, Chen H-M, Veerakumar P, Sheu J-R. Carbon Dot Nanoparticles Exert Inhibitory Effects on Human Platelets and Reduce Mortality in Mice with Acute Pulmonary Thromboembolism. Nanomaterials. 2020; 10(7):1254. https://doi.org/10.3390/nano10071254
Chicago/Turabian StyleLee, Tzu-Yin, Thanasekaran Jayakumar, Pounraj Thanasekaran, King-Chuen Lin, Hui-Min Chen, Pitchaimani Veerakumar, and Joen-Rong Sheu. 2020. "Carbon Dot Nanoparticles Exert Inhibitory Effects on Human Platelets and Reduce Mortality in Mice with Acute Pulmonary Thromboembolism" Nanomaterials 10, no. 7: 1254. https://doi.org/10.3390/nano10071254
APA StyleLee, T.-Y., Jayakumar, T., Thanasekaran, P., Lin, K.-C., Chen, H.-M., Veerakumar, P., & Sheu, J.-R. (2020). Carbon Dot Nanoparticles Exert Inhibitory Effects on Human Platelets and Reduce Mortality in Mice with Acute Pulmonary Thromboembolism. Nanomaterials, 10(7), 1254. https://doi.org/10.3390/nano10071254









