Abstract
The assessment of mobility and functional impairments in the elderly is important for early detection and prevention of fall conditions. Falls create serious threats to health by causing disabling fractures that reduce independence in the elderly. Moreover, they exert heavy economic burdens on society due to high treatment costs. Modern smartphones enable the development of innovative mobile health (mHealth) applications by integrating a growing number of inertial and environmental sensors along with the ever-increasing data processing and communication capabilities. Mobility assessment is one of the promising mHealth application domains. In this paper, we introduce a suite of smartphone applications for assessing mobility in the elderly population. The suite currently includes smartphone applications that automate and quantify the following standardized medical tests for assessing mobility: Timed Up and Go (TUG), 30-Second Chair Stand Test (30SCS), and 4-Stage Balance Test (4SBT). For each application, we describe its functionality and a list of parameters extracted by processing signals from smartphone’s inertial sensors. The paper shows the results from studies conducted on geriatric patients for TUG tests and from experiments conducted in the laboratory on healthy subjects for 30SCS and 4SBT tests.
1. Introduction
The quality of life of the elderly is highly correlated with their mobility. Reduced mobility creates serious risk of fall. Falls in the elderly are defined as “unintentionally coming to the ground, or some lower level because of sudden loss of balance, loss of consciousness, sudden onset of paralysis as in stroke or an epileptic seizure” [1]. Falls are a major concern among the elderly because of their negative impact on a person’s physical and physiological state. Falls are the third leading cause of worldwide chronic disability [2], and a study found that approximately 81%–98% of hip fractures are caused by falls in the elderly [3]. Falls not only create serious threats to health among the elderly, but the treatment costs and resources required to address them also exert a heavy economic burden on the society. The total costs resulting from falls were in the range of 0.85 to 1.5 percent of the total healthcare costs in the United States, Australia, the United Kingdom and the European Union (EU) in 2009 [3]. These costs are expected to further increase, as there will be an estimated 88.5 million individuals aged 65 and older in the United States alone in 2050, a 120% increase over the elderly population in 2010 [4]. The risks of falling and of fall related injury increase with the person’s age because of loss of agility, vision loss, and medication side-effects [5]. In addition to physical damage and their high costs, falls create fear of falling again by reducing self confidence among the elderly, particularly while walking on uneven pathways or a wet floor. The consequences of falls also include increased risks of pneumonia, pressure ulcers, and even death [6]. Therefore, the assessment of mobility and early recognition of individuals prone to falls are the key strategies to reduce fall related injuries and prevent their consequences.
The Centers for Disease Control and Prevention (CDC) created the STEADI (Stopping Elderly Accidents, Deaths & Injuries) tool kit for health care providers [7]. The CDC recommends the evaluation of gait, strength, and balance using three tests: the Timed Up and Go (TUG) test [8], the 30-Second Chair Stand Test (30SCS) [9], and the 4-Stage Balance Test (4SBT) [10]. These tests are generally performed in a clinical setting, thus limiting the frequency of testing and increasing the total test costs. Because of the demographic changes, there will be an increasing number of geriatric patients in the near future and probably fewer professionals would be available to assess the risk of fall in clinical settings. Therefore researchers have attempted to bring these assessment tests to patients’ homes [11]. In the new era of health monitoring, wireless sensing, mobile and cloud computing technologies support the development of mobile health applications. These technologies have been proven to effectively monitor the activities of daily living [12,13,14]. Automatic activity recognition and quantification systems that utilize inertial sensors are proposed for long-term health and fitness monitoring [15,16,17], assessment of mobility in the elderly and people with Parkinson’s disease [18,19], automatic fall detection [20,21], and rehabilitation [22,23]. An instrumented Timed Up and Go (iTUG) test has been recently introduced and proven to be sensitive to pathologies [24,25] and useful in fall risk prediction [26]. Approaches for automatic activity recognition used by researchers vary in number, type, and placement of utilized sensors, as well as in processing of recorded signals. While some researchers used multiple sensors for automatic activity recognition [27,28,29], an increasing number of projects use a single inertial sensor [30,31,32,33] usually placed on the subject’s chest. The rapid proliferation of smartphones and continual growth in smartphone capabilities have opened up new opportunities for health monitoring applications. Modern smartphones include a number of built-in inertial and environmental sensors that can be utilized in health and fitness monitoring applications. Modern smartphones typically include accelerometers, gyroscopes, magnetometers, barometers, and humidity sensors. With growing data processing and communication capabilities, smartphones enable the development of innovative mobile health (mHealth) applications.
In this paper, we introduce a suite of smartphone applications for mobility assessment. The suite includes applications for automating and quantifying standard mobility tests recommended by the Centers for Disease Control and Prevention (CDC): Timed Up and Go (TUG), 30-Second Chair Stand Test (30SCS), and the 4-Stage Balance Test (4SBT). The names of the applications are sTUG (Smart TUG) Doctor, 30SCS and 4SBT, respectively. The applications record and process the signals from the smartphone’s accelerometer, gyroscope, and magnetometer sensors to extract the parameters that quantify individual phases of the tests. The applications offer an affordable solution for quantifying mobility of the elderly with an immediate feedback and automated logging. The test procedures require minimum setup that includes a chair, a floor marker at the distance of three meters from the chair, and an inexpensive instrumentation with a smartphone placed on the chest or belt running the mobility assessment applications. The applications are quite easy to use and can be used in both ambulatory and clinical settings. For example, in ambulatory settings elderly subjects can periodically use applications to quantify their mobility and possibly detect early signs of mobility deterioration. The tests can be self-guided or conducted with a help of caregiver. In clinical settings, healthcare professionals can use applications to assess mobility of multiple patients. With automatic updates to an mHealth server over the Internet and services provided by the mHealth web portal, healthcare professionals can gain insights into mobility of tested subjects over time. For example, they can assess the impact of therapeutic interventions, e.g., impact of drugs, by analyzing the parameters from multiple tests performed in a single day. Next, healthcare professionals and researchers can monitor and evaluate evolution of disease by analyzing the trends in the parameters collected over longer periods of time.
The rest of the paper is organized as follows. Section 2 describes system architecture of the mobility assessment framework. Section 3 describes TUG test procedure and application including signal processing and parameter extraction. Section 4 and Section 5 describe the 30SCS and 4SBT applications, respectively, including parameters and signal processing. Section 6 describes the results from preliminary tests performed on the geriatric as well as healthy individuals. Section 7 concludes the paper.
2. Mobility Assessment System
2.1. System Architecture
Figure 1 illustrates system architecture of the application suite. The system requires an Android smartphone with built-in accelerometer, gyroscope and orientation sensors running Android 2.3 or above. During tests, the smartphone is mounted on the subject’s chest or back using an elastic band to keep it stationary and close to the body. The z-axis corresponds to the sagittal axis, the y-axis corresponds to the longitudinal axis, and the x-axis corresponds to the frontal axis of the human body. Smartphone applications record and process signals from the sensors, extract parameters, and display results on the smartphone’s screen. The applications stop monitoring automatically after the completion of the test is detected. They create test descriptors that include date and time when the tests are taken and all parameters that quantify the tests. A test descriptor is stored in a .csv file on the smartphone.
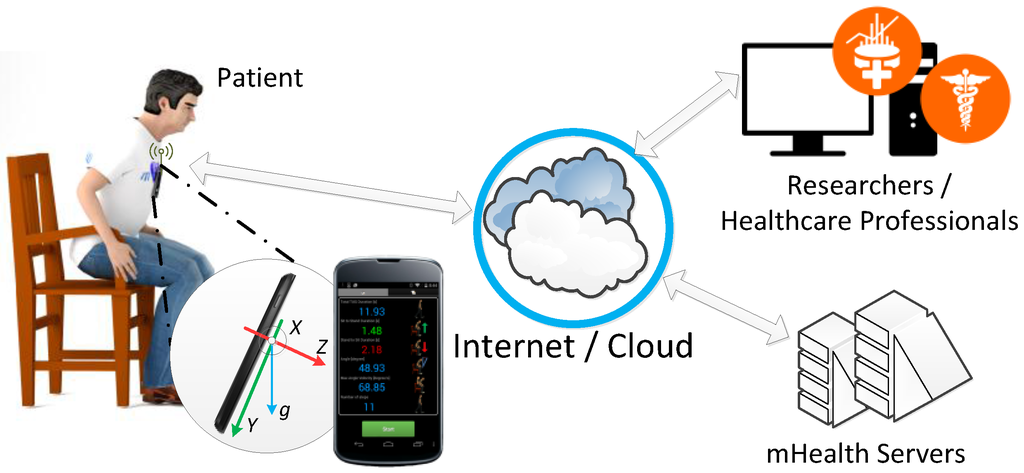
Figure 1.
System architecture for mobility assessment.
The smartphone applications can be configured for use in clinical settings. In this mode of operation, the applications require healthcare professionals to be registered users in the mHealth server databases with privileges to administer mobility tests. A test administrator can enter a new patient or select a patient already registered in the system. Upon completion of a test, the application automatically uploads the test descriptor to the mHealth server. The mHealth server consists of multiple virtual machines providing storage, database management, access control, and data visualization services. It includes three main components: mHealth database, mHealth Web API, and mHealth Web Portal [34]. The mHealth database is built to support a variety of physiological records with annotations. Each record has information about the subject, equipment used to collect records, and conditions under which the data are recorded, including application type, timestamp of the recording, and location. The Web API is designed to be intermediary between personal devices and the mHealth database. Any interaction with the mHealth API requires user authentication. Authorized healthcare professionals and researchers can use the mHealth Web portal services for remote access to physiological records and for rudimentary visualization of data. Through these services, longitudinal studies aimed at quantifying improvements or deterioration in mobility can be performed.
With the proposed mounting of the smartphone on the chest or back, the applications record the x, y, and z components of the acceleration of the subject’s upper trunk and use these signals to determine the upper body movement. The smartphone’s gyroscope measures angular movements, specifically the rotation around the x-axis (roll), y-axis (yaw), and z-axis (pitch). In our setup, we record the angular velocity from the gyroscope and use the signals to detect and locate important transitions during the TUG and 30SCS tests. Smartphone’s magnetic sensor is sensing the Earth’s magnetic field and is normally used to aid navigation by determining the Earth’s magnetic poles and the smartphone’s orientation. In our setup, we use these signals to detect the subject’s orientation in the TUG test.
The tests can be administered by the subject himself/herself or a healthcare practitioner in a clinical setting. The tests can be taken many times in a day. Analysis of the parameters collected over longer periods of time may help in tracking long-term changes in mobility and diagnosis of balance impairments. All the applications have been tested on Nexus 4 smartphone, HTC M7 and M8 (HTC Corporation, Taoyuan, Taiwan), Motorola RAZR M, and RAZR HD (Motorola, Inc., Schaumburg, IL, USA).
2.2. Settings and Configurations
Figure 2 shows the smartphone screens demonstrating the settings and configurations of the applications when used in clinical settings. The applications need to be set up before conducting the tests and this is typically done by healthcare professionals in charge of administering the tests. First, four settings screens (a), (b), (c) and (d) are common to all the applications, whereas the last two settings screens (e) and (f) are used for the 30SCS and sTUG Doctor applications, respectively.

Figure 2.
Settings and configuration of the applications suite: (a) Login screen; (b) Configuration screen; (c) Adding a new subject screen; (d) Subjects screen; (e) 30SCS configuration screen; (f) sTUG Doctor configuration screen.
Figure 2a shows a login interface. The applications use the Internet to communicate with the mHealth server. The applications require application users, typically healthcare professionals, to enter their credentials for login to the mHealth server. A “setting” button on the login screen takes the user to the configuration screen shown in Figure 2b. The checkbox “Remember Me” enables the user to save and cache the login credentials. The “Save to External SD card” option enables saving raw data and tests descriptors to the external SD card memory. The “Offline Session” allows the user to perform tests without uploading data on the server. The “Save Configurations” option saves the modified configuration. After logging into the application, it shows up a screen shown in Figure 2d with the list of subjects (with subject ids and dates of birth) who already participated in the tests. The “add new subject” icon on the screen opens up a screen shown in Figure 2c and asks for the new subject information such as unique id, gender and date of birth. The subject is added to the list of users when the “save” button on the screen is pressed. Screens shown in Figure 2e,f show the configurations available for the sTUG Doctor and 30SCS applications, respectively. “Upload TUG Parameters to Server” enables the data upload to the mHealth server. “Save to Files” check boxes enable the user to selectively save the raw data as well as parameters of the tests in the files. “Advance Configuration” allows a user to specify the smartphone location, which can be on the subject’s back or chest (default). For research and development purposes, we allowed options in the advanced settings to set up sampling frequency and thresholds used in the applications. The sTUG Doctor and 30SCS applications use default thresholds as shown in Figure 2f.
3. Smart Timed Up and Go (sTUG Doctor) Application
The Timed Up and Go (TUG) is a frequently used clinical test for the assessment of mobility, and fall risk prediction in the elderly population and people with Parkinson’s disease [35]. This is a simple test and easy to administer anywhere, anytime. In this test, a subject sits in a standard arm chair. The subject uses regular footwear and he/she can use a walking aid if needed. On the command “Go”, the subject stands up from the chair and walks to a three-meter marker on the floor at a normal pace, turns around, walks back to the chair, and sits down again. Figure 3 demonstrates the typical phases of TUG test. The test outcome is the TUG time from the command “Go” to the time when the subject sits on the chair again. An adult with mobility impairments may take more than 30 s to complete the test, whereas a healthy adult can perform this test in less than 10 s. This test has been proven valuable in early assessment of balance and mobility, although it is limited as its only outcome is the time to complete the test. An older adult who takes more than 12 s to complete the TUG test is at high risk for falling [36]. In addition, the health care professionals also observe and report the subject’s postural stability, gait, stride length, and sway to fill in a form identifying slow, tentative pace; loss of balance; short strides; little or no arm swing; shuffling; or improper use of walking aids.
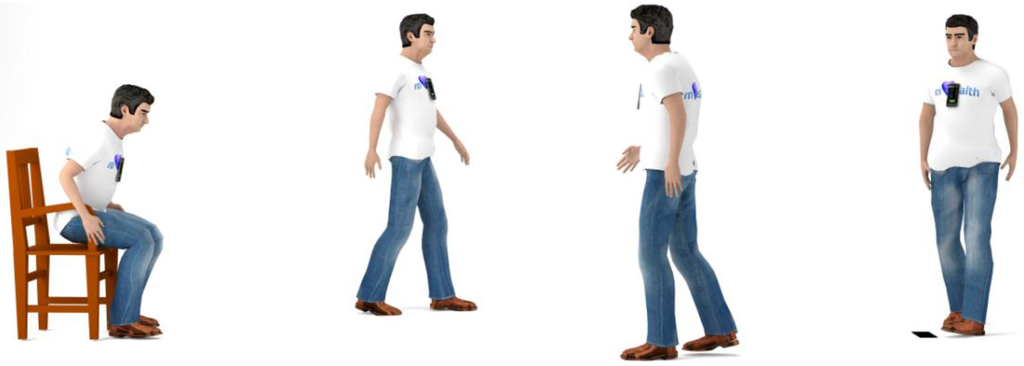
Figure 3.
Timed Up and Go (TUG) test phases.
The sTUG Doctor application automates and quantifies the standard Timed Up and Go (TUG) test [37]. On application start, it provides options to set up configuration and subject information as shown in Figure 2. Then it opens the main display screen shown in Figure 4a. When the subject or the test administrator presses the green “Start” button on the screen, the application starts recording and processing data from in-built inertial sensors and calculates TUG test parameters in real time. The application starts measuring time from the point it finds a sit-to-stand transition during the test. The application stops automatically after it detects a stand-to-sit transition and important parameters are calculated and displayed instantly on the screen as shown in Figure 4b. The application quantifies all the phases of the TUG test and calculates parameters listed in the Table 1. These parameters include the total TUG duration, sit-to-stand duration, stand-to-sit duration, maximum lean forward angle, maximum angular velocity, and the total number of steps taken during walking. The detailed set of test parameters with subject’s unique id and timestamp are saved on the smartphone and sent to the mHealth server. This application also has an alternative display tab which keeps all the recordings for each subject with exact date and time of the test with summary parameters as shown in Figure 4c. It should be noted that in standalone application mode, subjects are expected to be able to start the application and press the Start button. The screens described in Figure 4a,b are designed to accommodate older adults by featuring big buttons and large fonts with posture icons.

Figure 4.
sTUG Doctor smartphone application screens: (a) application screen before the test is started; (b) application screen with a selected set of parameters upon completion of a test; and (c) application screen showing a log with multiple measurements for a single subject.

Table 1.
Parameters for TUG characterization.
Figure 5 shows raw acceleration and gyroscope signals collected by the sTUG Doctor application during a TUG test. When the “Start” button on the screen is pressed, the beginning timestamp is captured. The program then waits for the beginning of the sit-to-stand transition by searching for a change in the angular velocity around the frontal axis (the x component of the gyroscope). This change is caused by leaning forward as the subject prepares to stand up. Additionally, acceleration thresholds are checked to ensure that the leaning forward signature is caused by an actual motion rather than by swinging forward while still in the sitting position. The angular velocity during the sit-to-stand transition has a distinct profile as it starts from zero, increases to reach the maximum, and drops to a zero at the end of the lean forward phase (LF). To determine the beginning of the transition, the application finds the maximum angular velocity (v.LF) that is above a certain threshold, and then searches backward to find the beginning of the slope. The maximum upper trunk angle (a.S2ST) is reached at the end of the lean forward phase. The time duration between the beginning of the transition and the end of the lean forward phase represents the duration of the lean forward phase (d.LF). The second phase of the sit-to-stand transition is characterized by a negative angular velocity as the subject moves into an upright position. The angular velocity reaches the minimum (i.e., v.LT), and then increases back to zero. The moment when it becomes positive is considered to be the end of the lift up phase and the end of the sit-to-stand transition. By time stamping this moment, we calculate the duration of the lift up phase (d.LT), and the total duration of sit-to-stand transition, d.S2ST = d.LF + d.LT. A stand-to-sit transition can also be divided into two separate phases, a prepare-to-sit (PS) and a sit-down (SD) phase. The angular velocity increases to the maximum and then drops back to zero as the subject leans forward in preparation to sit down. The moment when the angular velocity drops to zero marks the end of the prepare-to-sit phase and the beginning of the sit-down phase. By timestamping these characteristic points, the application determines the duration of the preparation to sit phase (d.PS). In the sit-down phase, the angular velocity is negative as the subject’s upper trunk moves back into the upright position. The moment it becomes positive marks the end of the sit-down phase and the entire stand-to-sit transition. By capturing the time stamp of this moment the application calculates the duration of the sit-down phase (d.SD), and the entire stand-to-sit transition (d.ST2S = d.PS + d.SD). The total walk time (d.WALK) is calculated using captured timestamps and the number of steps (n.STEP) using the acceleration and gyroscope thresholds. The application uses the smartphone’s magnetic sensor data to detect turning and the number of steps before turn (n.SBT).
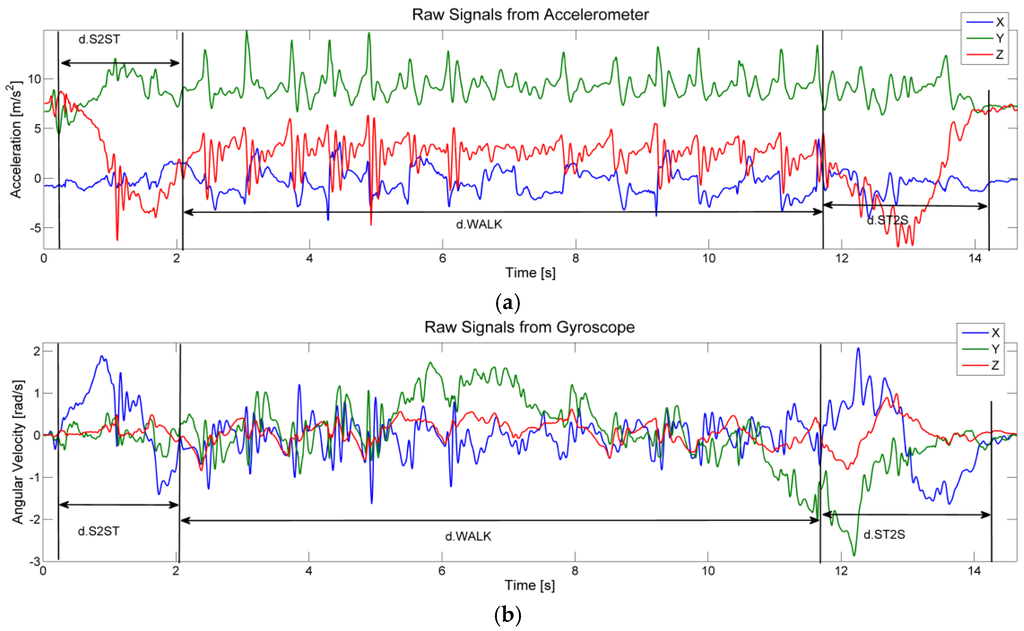
Figure 5.
Inertial signals recorded during a TUG test: (a) raw signals from accelerometer; (b) raw signals from gyroscope.
4. The 30-Second Chair Stand (30SCS) Application
The 30-Second Chair Stand Test measures the number of stand ups a person can perform during a 30 s interval which is based on the five-times-sit-to-stand test [38]. The primary goal of this test is to measure the lower extremity strength and endurance, but it can also indicate speed, balance, and mobility [39,40,41]. The standard test is limited as its only quantitative outcome is the number of stands completed within 30 s. The test is conducted using a straight back chair without arm rests, and a stopwatch. The patient is sitting in the middle of the chair with feet flat on the floor, hands placed on opposite shoulders and crossed at the wrists. The typical phases of 30SCS test are shown in the Figure 6. On the command “Start” the patient rises to a full standing position and then sits back down holding arms against his/her chest. The patient keeps repeating these steps for 30 s. Table 2 gives 30SCS test scores as a function of gender and age used to determine whether the patient is at high risk for falls [42]. A below average scores indicates a high risk of falls.
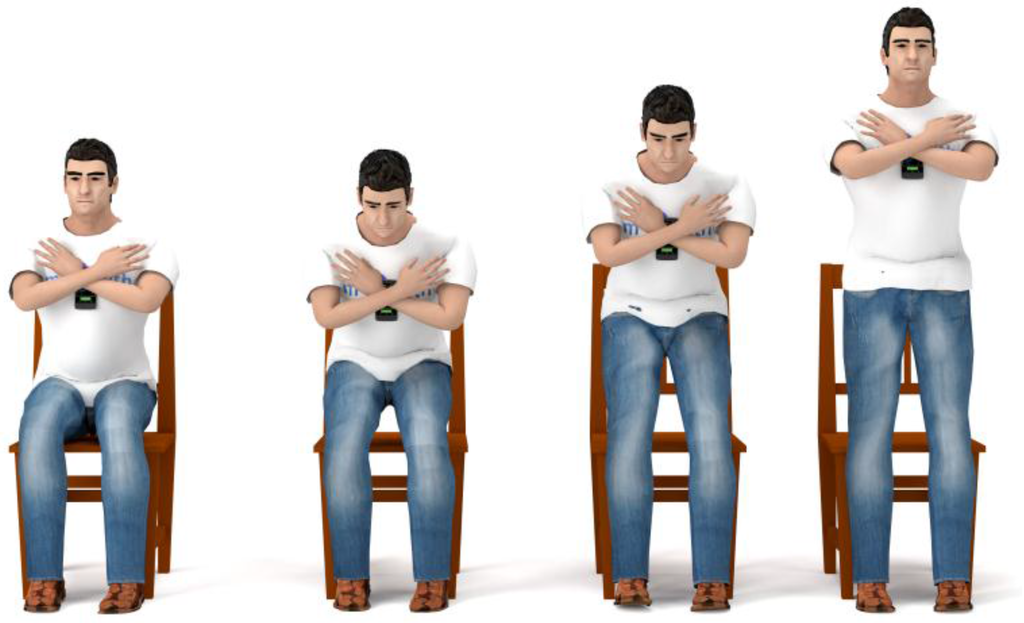
Figure 6.
The 30-Second Chair Stand (30SCS) test phases.

Table 2.
The 30-Second Chair Stand Test scores with ages and genders.
The 30SCS smartphone application automates and quantifies the standard 30-Second Chair Stand Test. Application begins the test when a subject presses the green “Start” button on the screen shown in Figure 7a. The subject then makes as many stand-ups as he/she can during 30 s. The application makes an acoustic cue (beep sound) after 30 s to indicate the test completion. Our application counts the total number of stand-ups as well as total number of complete cycles (stand-up to sit-down). The complete set of derived parameters for each cycle of 30SCS test is presented in Table 3. The application displays important parameters immediately on the screen after the completion of the test as shown in Figure 7b. The application also has an alternative tab to display the test summary with important test parameters for a single subject with data and time as shown in Figure 7c. The values of parameters listed along with the raw signals of the test are saved in the .csv file on the smartphone as well as uploaded on the mHealth server.

Figure 7.
30SCS smartphone application screens: (a) application screen before the test is started; (b) application screen with a selected set of parameters upon completion of a test; and (c) application screen showing a log with multiple measurements for a single subject.

Table 3.
Parameters for 30SCS characterization.
Raw acceleration and gyroscope data for three chair stands during a 30SCS test is presented in Figure 8. The plots are annotated with markers indicating relevant events for each cycle of a chair stand. The test starts when the command “Start” button is pressed. Similar to the sTUG application, the 30SCS application detects a stand-up phase with its sub-phases (leaning forward and lifting up). A subject can spend some time in the standing position, described by a parameter d.STi. The standing is followed by a stand-to-sit transition. In the sitting position, a subject may also stay for some time before a new cycle is started. The sitting is characterized for each cycle by a parameter d.SITi. Please note that in healthy subjects the parameters d.STi and d.SITi may be equal to zero, i.e., the subjects may move from one transition to the other without any delays. However, elderly people and people with balance and mobility impairments may require some time to prepare for the next cycle. To detect characteristic events, the starting and ending points of transitions, algorithms used in the sTUG application are slightly modified to work for the 30SCS test. The signals from the gyroscope sensors are processed to timestamp all the phases of each cycle for 30SCS. The application counts the number of stand-ups, and the number of complete stand-up/sit-down cycles during the test.
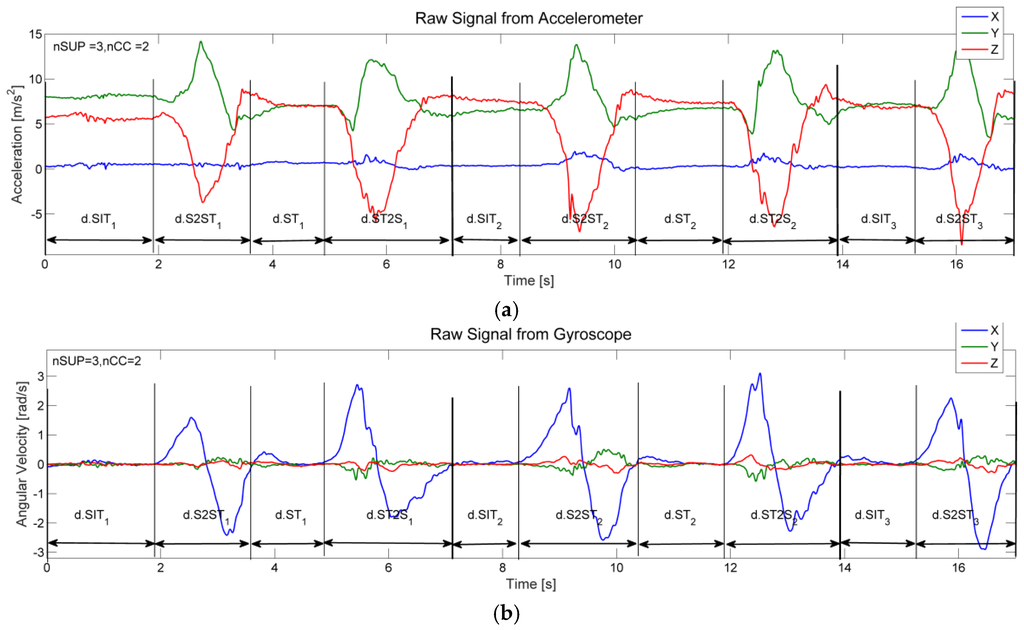
Figure 8.
Inertial signals recorded during three cycles of a 30SCS test: (a) raw signals from accelerometer; (b) raw signals from gyroscope.
5. The 4-Stage Balance Test (4SBT) Application
The 4-stage balance test is used to assess static balance of the elderly during four progressively more challenging balancing positions. In this test, the subject should not use any assistive devices and should keep their eyes open during the test. The four respective positions of the 4SBT are shown in Figure 9. The positions are described as follows: (a) Feet together stand assumes feet are placed side by side; (b) Semi-tandem stand assumes that the instep of one foot is touching the big toe of the other foot; (c) Tandem stand assumes that one foot is placed in front of the other-heel of one foot touches the toe of other foot; and (d) One leg stand assumes standing on one leg. A nurse supervising the test clearly describes and demonstrates each position and always stands next to the subject to hold his/her arm and help them assume the correct foot position. When the subject is steady, the nurse starts measuring time using a stopwatch, but remains ready to catch the subject in case of a balance loss. If the subject can hold a position for 10 s without moving his/her feet or needing support, the test advances to the next position. The standard test outcomes are times in seconds the subject is able to hold each of four positions. It has been shown that an older adult who cannot hold the tandem stance for at least 10 s is at increased risk of falling [10].

Figure 9.
The 4-Stage Balance Test (4SBT) feet positions.
The 4SBT smartphone application consists of four tests that can be selected using the test selector screen shown in Figure 10a. The application starts the test after the green “Start” button on the display screen is pressed as shown in Figure 10b. The standard outcome of this test is the number of seconds a subject can hold the position. We have quantified the subject’s ability to hold the balance by calculating the displacement of the chest and timestamping excessive movements. Table 4 describes the derived 4SBT test parameters. The 4SBT application provides the average chest movements during each of the four phases/positions of the balance test. The application uses accelerometer signals to quantify relative displacement of the chest. The chest displacement values indicate the balance control of the subject; the lower displacement values demonstrate better stability during the tests. When the subject stumbles during any of the four tests and comes back in the stable position (e.g., put the foot down during one leg stand), the 4SBT application reports the time of stumbling and loss of balance. Figure 10c presents the display of parameters as well as the stumble status.
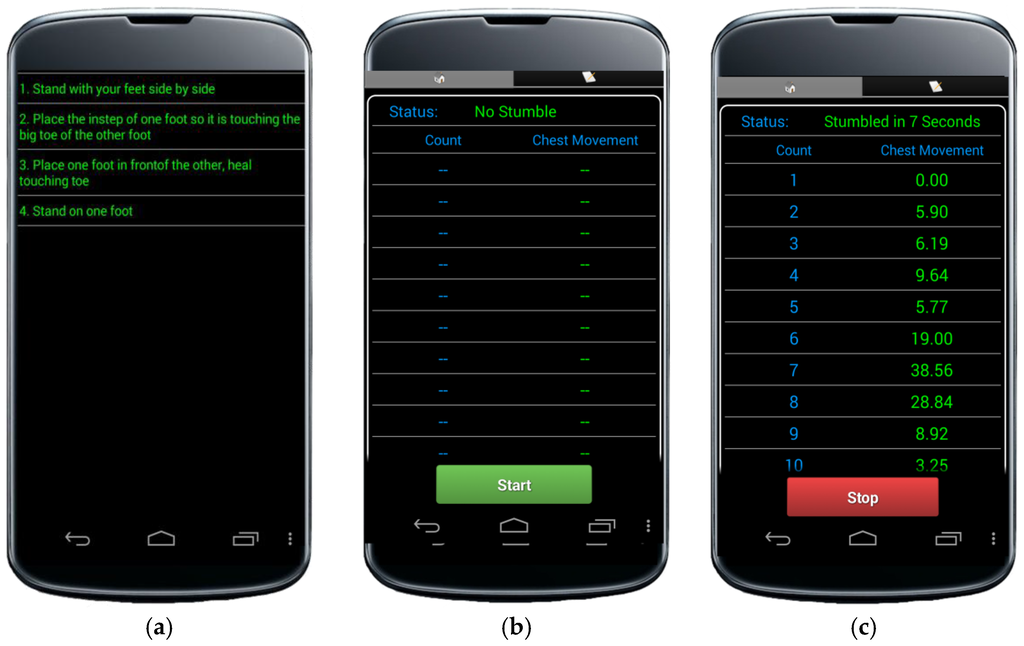
Figure 10.
4SBT smartphone application screens: (a) application screen for test position selection; (b) application screen before the test is started; and (c) application screen with a selected set of parameters upon completion of a test.

Table 4.
Parameters for 4-Stage Balance Test characterization.
Figure 11 shows the chest acceleration magnitude during a semi-tandem stand when a healthy subject maintains stable position (top graph), maintains stable position with an effort (middle graph), and when the balance is lost approximately after two seconds from the beginning of the test (bottom graph). The graphs show that acceleration magnitude can indeed be used as a metric for quantifying stability; significant changes in the acceleration magnitude in the bottom graph are due to a loss of balance. The 4SBT application calculates the displacement for each second of the test using Equations (1)–(4). Acc is the raw 3D acceleration magnitude (Equation (1)), Acc’ represent Acc without the DC offset, eliminated by subtracting the value of Acc at rest, as shown in Equation (2). The velocity vel is calculated at every sample using Equation (3), where ∆t is the sampling interval (10 ms in our case). Next, the displacement Disp is calculated as shown in Equation (4). After analyzing the displacement data from a several tests performed in the laboratory with and without stumbling, we have found a displacement threshold of 30 cm that reliably detects the stumbling for the existing data sets However, more tests collected in clinical settings are necessary to find a threshold that would work reasonably well in majority of test cases. It should be noted that the current algorithm for detecting a stumbling could fail if a subject drops a foot gently while maintaining a perfect stability. An alternative to relying on algorithms to detect stumbling is to allow test administrator to automatically annotate a stumbling event when it occurs (e.g., by pressing a button or issuing a voice command).
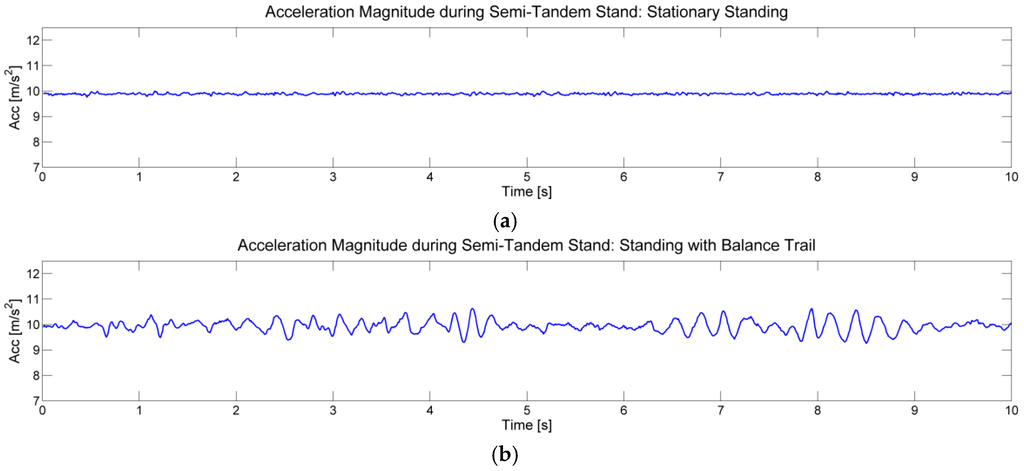
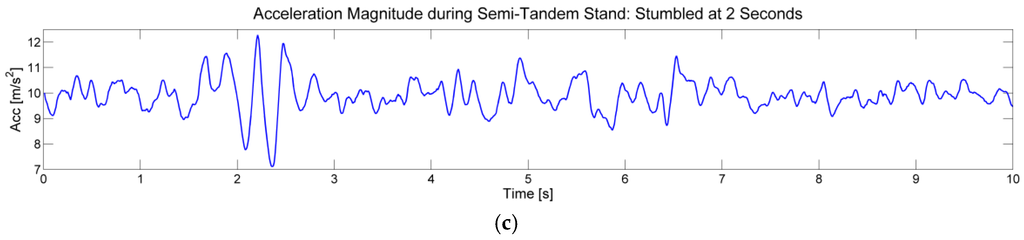
Figure 11.
Comparison of accelerometer vector magnitudes during semi-tandem stands for: (a) stationary standing; (b) standing with balance trail; and (c) standing with stumble.
6. Application Suite Verification and Validation
In this section we briefly discuss our experiments aimed at verification of the applications in the mobility assessment suite. During the development of the algorithms for posture transitions from the smartphone’s inertial sensors in the TUG and 30SCS tests we used the following approach. A number of volunteers participated in data collection, ranging from healthy subjects that performed the tests as quickly as possible to people with mobility impairments affiliated with a local Parkinson’s support group. The inertial sensor data collected by the smartphone are used in the initial development of offline signal processing algorithms in Matlab (R1024a, The MathWorks, Inc., Natick, MA, USA). To guide and inform algorithm development, each session is videotaped using a regular camera and videos are manually annotated by timestamping posture transitions. For a selected group of participants we also performed the test in a laboratory equipped with the Vicon motion capture system. This laboratory allows for accurate tracking of reflective markers using 33 Vicon T40 series IR cameras (Vicon Industries, Inc., Ipswich, UK). Test users carry the smartphone and strategically placed reflective markers as shown in Figure 12. The motion capture system records the absolute position of each marker with a millimeter precision every 20 ms. Using these data, we extract the acceleration vectors from two reflective markers attached to smartphone and compare them to the acceleration vector recorded synchronously by the smartphone during typical posture transitions. Whereas the algorithms for detection and characterization of posture transitions used in the smartphone applications rely exclusively on the sensor data from the smartphone, the Vicon system provides absolute location that is used for verification of algorithms. We find that accelerometer data captured by the smartphone match the accelerometer data derived from the reflective markers attached to the smartphone. In addition, we verify that angles and angular velocity signals calculated by the smartphone application match those derived from the Vicon system—the difference between the two is less than 1%. Once the algorithms were tested and perfected in Matlab, they were ported to Java and the Android OS.

Figure 12.
A subject instrumented by reflective markers and the smartphone during posture detection algorithms verification.
The second phase of the testing is carried out in both laboratory conditions and in clinical settings under supervision of healthcare professionals. In the laboratory conditions, a variety of subjects perform the mobility assessment tests. We capture videos of these sessions. These videos are manually annotated to identify timestamps of posture transitions. Time parameters describing duration of posture transitions are extracted from videos and compared to the time parameters reported by the sTUG and 30SCS applications. Below we show the results of verification for a selected set of parameters.
Table 5 shows the results of a laboratory testing of the sTUG Doctor application, specifically the verification of the dTUG parameter, which is the main quantitative outcome of the TUG test. We consider three subjects, each performing three TUG tests (Test#1, Test#2, and Test#3). For each test we show the time reported by the sTUG application (sTUG) and the time extracted from the video, as well as the absolute error. The rows marked as Error indicate the absolute difference in measurements, if we assume the times extracted from the video are taken as reference times. The results show that the maximum error falls below 4%. In a clinical setting, the sTUG application is tested as follows. A nurse in charge of mobility assessment carries out the standard TUG test with a stopwatch to measure the time a subject needs to complete a TUG test. In addition, the subject has a smartphone on his or her chest or back and the start button is pressed when the command GO is issued by the nurse. The time recorded by the nurse using the stopwatch is compared to the time reported by the sTUG Doctor application. In an experiment with 20 older adults we find that the test times recorded by the stopwatch with the resolution of 0.1 s match the times reported by the sTUG in all conducted tests within 400 ms.

Table 5.
Testing the sTUG Doctor application: duration of the TUG test (d.TUG).
Table 6 shows the results of a laboratory testing of the 30SCS application. We consider three subjects S#1, S#2, and S#3, each performing the test two times (Test#1 and Test#2). For each test, we show the times to perform the sit-to-stand transitions. The rows marked with 30SCS include the sit-to-stand times in seconds reported for individual stand-ups during the test reported by the application, and rows marked with Video include the sit-to-stand times extracted from manually annotated videos. If we assume that times extracted from the videos are reference times, the absolute errors by the 30SCS application range from 0% to 14.4%, but are typically less than 5%. We find these errors quite satisfactory. For the medical outcome of the 30SCS test, the number of stand-ups, the 30SCS application is 100% accurate. Similar observations can be found for the stand-to-sit times—the absolute errors for the times reported by the 30SCS range between 0% and 3.7%.

Table 6.
Testing the 30SCS application: sit-to-stand transition times (d.S2STi).
7. Results
The sTUG Doctor application has been used in the Center for Aging, Huntsville, AL. The Center led by a gerontologist provides an innovative and comprehensive model of care for adults over the age of 65. Its primary goal is to empower the general population with the latest knowledge about issues of aging, particularly about the use of medications and unique problems of the elderly, such as memory disturbances, polypharmacy, falls, incontinence, dementia, depression, and mobility problems. Specifically, sTUG Doctor is used in a pilot study aimed at fall prevention and improved mobility. It is used to quantify the impact of medical interventions that typically include changes in medications and community-based exercise sessions designed to improve mobility. Initial pilot study included 30 patients. Table 7 shows the results for three patients (P#1, P#2, and P#3) who participated in the study. For each patient, we show the TUG test results taken: (a) when the patient is admitted into the study; (b) once midway through the study; and (c) once approximately three months through the study. The TUG results showed that all three patients significantly improved their performance in the TUG test (e.g., almost 34% improvement of the total time d.TUG for P#1, more than 31% improvement for P#2, and 28% improvement for P#3). Sit-to-stand (d.S2ST), stand-to–sit (d.ST2S) and total walk time (d.WALK) durations have also been improved significantly. Moreover, total number of steps (n.STP) taken to cover the three-meter distance has been reduced indicating the improved stability of walking. These certainly indicate improved mobility over time.

Table 7.
The TUG test results recorded during stability improvement program.
The 30SCS application has been tested in our mHealth laboratory. Five healthy subjects participated in this test. Table 8 presents the average/standard deviation of the 30SCS test cycle parameters for those subjects. P#5 completed 16 stand ups and 15 complete cycles (i.e., from the moment of sitting to the completion of stand-to-sit transition). The average trunk angle (a.S2ST) is also smaller when compared to other cases. This indicates that the subject P#5 avoids leaning forward in order to increase the number of stand ups. We observed that most subjects require more time per cycle as the test progresses, which may be an indication of the fitness level. Figure 13 illustrates the change of the cycle time during the 30SCS tests, as well as the fitted regression line. We estimated the slope of the regression line by calculating ratio of the height of the line at the end to the height of the line at the beginning. Slope values greater than one indicate that a subject needs more time to complete a test cycle as the test progresses. In addition, an increase in the duration of individual phases (such as d.SIT, d.S2ST, d.ST, d.ST2S, etc.) have also been noticed towards the end of the test.

Table 8.
The 30SCS test results.
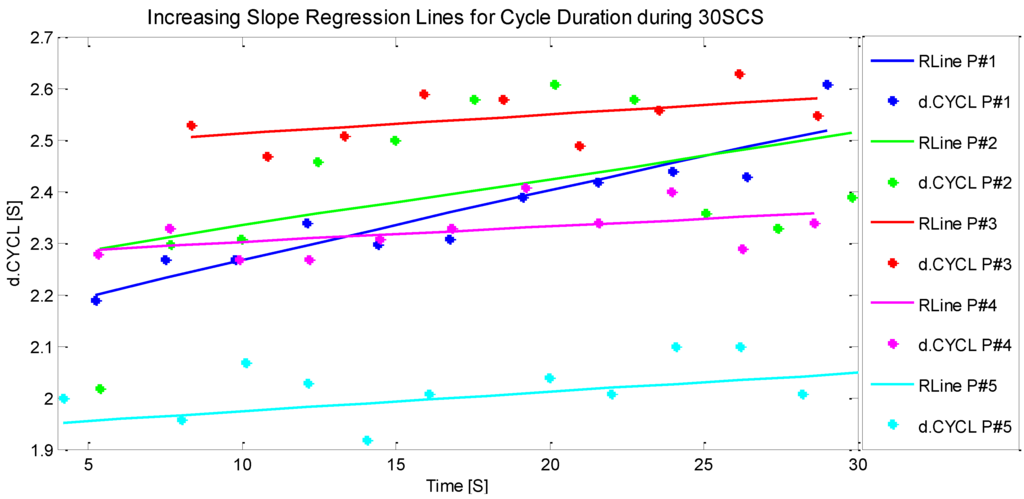
Figure 13.
Regression lines fitted in all cycle times (d.CYCL) with 95% Confidence interval.
Table 9 presents the 4SBT application results performed on a healthy female 28-year-old subject recorded for three different cases (stationary, balancing and stumbling) explained in the 4SBT application section. The mean and standard deviation (M and SD rows in the table) are shown to illustrate variability of the displacement during 10 s of each test. We notice that the displacement values in full tandem stand (s.FTS) are lower than the values in a one leg stand (s.OL). There is more variation in the values for standing when a subject stumbles. The stumbling occurs at T = 3 in the one-leg stand test. Therefore, we can say that the higher values of chest displacements are associated with the decreased stability during the positions of the 4SBT test.

Table 9.
The 4-stage balance test results.
8. Conclusions
Proliferation of smartphones that integrate increasingly sophisticated sensors creates new opportunities for instrumentation and quantification of standard monitoring and diagnostic procedures. This is particularly important for the monitoring of elderly and chronic patients. In this paper, we describe a suite of smartphone applications we developed to automate standard recommended mobility assessment tests: TUG, 30SCS, and 4SBT. The applications provide instantaneous feedback to the user and automatically upload the test results to the mHealth server. The application has been tested on a group of healthy volunteers and elderly patients with recent falls and showed promising results. By utilizing commodity smartphones, the application suite offers an affordable tool for instantaneous quantification of the mobility assessment. Analysis of the parameters collected over longer periods of time may help in longitudinal monitoring of mobility of subjects and quantify the effectiveness of exercise programs and therapies.
Acknowledgments
This work was supported in part by National Science Foundation grants CNS-1205439 and CNS-1217470. Authors would like to thank Mladen Milosevic for developing a computing infrastructure which included an mHealth server and a number of mHealth applications for mobile health and wellness monitoring, including the original sTUG smartphone application. We thank Zaheer Khan from Center for Elder Care, Huntsville, AL and Karen Frith and Amy Hunter for providing TUG records from longitudinal study of assessment of mobility used as test cases in this paper.
Author Contributions
Priyanka Madhushri developed the 30SCS and 4SBT smartphone applications and worked on paper preparation. Armen Dzhagaryan proposed the test parameters for 30SCS application, developed signal processing algorithms for 30SCS, and helped in preparing figures. Emil Jovanov and Aleksandar Milenkovic proposed the idea, established the mHealth framework, and provided guidance and management throughout the completion of the project. All authors have read and approved the final manuscript.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Gibson, M.J.; Andres, R.O.; Isaacs, B.; Radebaugh, T.; Wormpetersen, J. The prevention of falls in later life. A report of the Kellogg International Work Group on the Prevention of Falls by the Elderly. Dan. Med. Bull. 1987, 34 (Suppl. 4), 1–24. [Google Scholar]
- Hsu, C.L.; Nagamatsu, L.S.; Davis, J.C.; Liu-Ambrose, T. Examining the relationship between specific cognitive processes and falls risk in older adults: A systematic review. Osteoporos. Int. J. Establ. Result Coop. Eur. Found. Osteoporos. Natl. Osteoporos. Found. USA 2012, 23, 2409–2424. [Google Scholar] [CrossRef] [PubMed]
- Hamacher, D.; Singh, N.B.; Van Dieën, J.H.; Heller, M.O.; Taylor, W.R. Kinematic measures for assessing gait stability in elderly individuals: A systematic review. J. R. Soc. Interface R. Soc. 2011, 8, 1682–1698. [Google Scholar] [CrossRef] [PubMed]
- Vincent, G.K.; Velkoff, V.A. The Next Four Decades: The Older Population in the United States: 2010 to 2050; U.S. Department of Commerce; Economics and Statistics Administration, U.S. Census Bureau: Suitland, MD, USA, 2010.
- Alexander, B.H.; Rivara, F.P.; Wolf, M.E. The cost and frequency of hospitalization for fall-related injuries in older adults. Am. J. Public Health 1992, 82, 1020–1023. [Google Scholar] [CrossRef] [PubMed]
- Habib, M.A.; Mohktar, M.S.; Kamaruzzaman, S.B.; Lim, K.S.; Pin, T.M.; Ibrahim, F. Smartphone-Based Solutions for Fall Detection and Prevention: Challenges and Open Issues. Sensors 2014, 14, 7181–7208. [Google Scholar] [CrossRef] [PubMed]
- Schneider, D.L. Preventing Falls: Time for Action. Available online: http://www.todaysgeriatricmedicine.com/archive/110113p34.shtml (accessed on 31 January 2016).
- Thrane, G.; Joakimsen, R.M.; Thornquist, E. The association between timed up and go test and history of falls: The Tromsø study. BMC Geriatr. 2007, 7, 1. [Google Scholar] [CrossRef] [PubMed]
- Millor, N.; Lecumberri, P.; Gómez, M.; Martínez-Ramírez, A.; Izquierdo, M. An evaluation of the 30-s chair stand test in older adults: Frailty detection based on kinematic parameters from a single inertial unit. J. NeuroEng. Rehabil. 2013, 10, 86. [Google Scholar] [CrossRef] [PubMed]
- CDC The 4-Stage Balance Test. Available online: http://www.cdc.gov/steadi/pdf/4-stage_balance_test-a.pdf (accessed on 31 January 2016).
- Zampieri, C.; Salarian, A.; Carlson-Kuhta, P.; Nutt, J.G.; Horak, F.B. Assessing mobility at home in people with early Parkinson’s disease using an instrumented Timed Up and Go test. Parkinsonism Relat. Disord. 2011, 17, 277–280. [Google Scholar] [CrossRef] [PubMed]
- Milenković, A.; Otto, C.; Jovanov, E. Wireless sensor networks for personal health monitoring: Issues and an implementation. Comput. Commun. 2006, 29, 2521–2533. [Google Scholar] [CrossRef]
- Jovanov, E.; Poon, C.; Yang, G.-Z.; Zhang, Y.T. Guest Editorial Body Sensor Networks: From Theory to Emerging Applications. IEEE Trans. Inf. Technol. Biomed. 2009, 13, 859–863. [Google Scholar] [CrossRef] [PubMed]
- Jovanov, E.; Milenkovic, A. Body area networks for ubiquitous healthcare applications: Opportunities and Challenges. J. Med. Syst. 2011, 35, 1245–1254. [Google Scholar] [CrossRef] [PubMed]
- Bosch, S.; Marin-Perianu, M.; Marin-Perianu, R.; Havinga, P.; Hermens, H. Keep on moving! Activity monitoring and Stimulation using wireless sensor networks. In Smart Sensing and Context, Proceedings of the 4th European Conference on Smart Sensing and Context (EuroSSC’09), Guildford, UK, 16–18 September 2009; Lecture Notes in Computer Science. Springer-Verlag: Berlin, Germany; Heidelberg, Germany, 2009; Volume 5741, pp. 11–23. [Google Scholar]
- Pitta, F.; Troosters, T.; Probst, V.S.; Spruit, M.A.; Decramer, M.; Gosselink, R. Quantifying physical activity in daily life with questionnaires and motion sensors in COPD. Eur. Respir. J. 2006, 27, 1040–1055. [Google Scholar] [CrossRef] [PubMed]
- Madhushri, P.; Ahmed, B.; Penzel, T.; Jovanov, E. Periodic leg movement (PLM) monitoring using a distributed body sensor network. Conf. Proc. IEEE Eng. Med. Biol. Soc. (EMBC) 2015, 2015, 1837–1840. [Google Scholar]
- Al-Jawad, A.; Adame, M.R.; Romanovas, M.; Hobert, M.; Maetzler, W.; Traechtler, M.; Moeller, K.; Manoli, Y. Using multi-dimensional dynamic time warping for TUG test instrumentation with inertial sensors. In Proceedings of the 2012 IEEE Conference on Multisensor Fusion and Integration for Intelligent Systems (MFI), Hamburg, Germany, 13–15 September 2012; pp. 212–218.
- Zijlstra, A.; Mancini, M.; Lindemann, U.; Chiari, L.; Zijlstra, W. Sit-stand and stand-sit transitions in older adults and patients with Parkinson’s disease: Event detection based on motion sensors versus force plates. J. NeuroEng. Rehabil. 2012, 9, 75. [Google Scholar] [CrossRef] [PubMed]
- Tacconi, C.; Mellone, S.; Chiari, L. Smartphone-Based Applications for Investigating Falls and Mobility. In Proceedings of the 2011 5th International Conference on Pervasive Computing Technologies for Healthcare (PervasiveHealth) and Workshops, Dublin, Ireland, 23–26 May 2011.
- Wongpatikaseree, K.; Lim, A.O.; Tan, Y.; Kanai, H. Range-based algorithm for posture classification and fall-down detection in smart homecare system. In Proceedings of the 1st IEEE Global Conference on Consumer Electronics, Tokyo, Japan, 2–5 October 2012; pp. 243–247.
- Jovanov, E.; Milenkovic, A.; Otto, C.; de Groen, P.C. A wireless body area network of intelligent motion sensors for computer assisted physical rehabilitation. J. NeuroEng. Rehabil. 2005, 2, 6. [Google Scholar] [CrossRef] [PubMed]
- Santhiranayagam, B.K.; Lai, D.T.H.; Jiang, C.; Shilton, A.; Begg, R. Automatic detection of different walking conditions using inertial sensor data. In Proceedings of the 2012 International Joint Conference on Neural Networks (IJCNN), Brisbane, Australia, 10–15 June 2012; pp. 1–6.
- Weiss, A.; Herman, T.; Plotnik, M.; Brozgol, M.; Maidan, I.; Giladi, N.; Gurevich, T.; Hausdorff, J.M. Can an accelerometer enhance the utility of the Timed up & Go Test when evaluating patients with Parkinson’s disease? Med. Eng. Phys. 2010, 32, 119–125. [Google Scholar] [PubMed]
- Zampieri, C.; Salarian, A.; Carlson-Kuhta, P.; Aminian, K.; Nutt, J.G.; Horak, F.B. The instrumented timed up and go test: Potential outcome measure for disease modifying therapies in Parkinson’s disease. J. Neurol. Neurosurg. Psychiatry 2010, 81, 171–176. [Google Scholar] [CrossRef] [PubMed]
- Marschollek, M.; Nemitz, G.; Gietzelt, M.; Wolf, K.H.; Meyer Zu Schwabedissen, H.; Haux, R. Predicting in-patient falls in a geriatric clinic: A clinical study combining assessment data and simple sensory gait measurements. Z. Gerontol. Geriatr. 2009, 42, 317–321. [Google Scholar] [CrossRef] [PubMed]
- Bao, L.; Intille, S.S. Activity Recognition from User-Annotated Acceleration Data. In Pervasive Computing; Ferscha, A., Mattern, F., Eds.; Lecture Notes in Computer Science; Springer: Berlin, Germany; Heidelberg, Germany, 2004. [Google Scholar]
- Ghasemzadeh, H.; Loseu, V.; Jafari, R. Structural action recognition in body sensor networks: Distributed classification based on string matching. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Lester, J.; Choudhury, T.; Borriello, G. A practical approach to recognizing physical activities. In Pervasive Computing, Proceedings of the 4th International Conference on Pervasive Computing (PERVASIVE’06), Dublin, Ireland, 7–10 May 2006; Lecture Notes in Computer Science. Springer: Berlin, Germany; Heidelberg, Germany, 2006; Volume 3968, pp. 1–16. [Google Scholar]
- Aminian, K.; Najafi, B. Body Movement Monitoring System and Method. U.S. Patent 7141026 B2, 1 October 2001. [Google Scholar]
- Florentino-Liano, B.; O’Mahony, N.; Artes-Rodriguez, A. Human activity recognition using inertial sensors with invariance to sensor orientation. In Proceedings of the 2012 3rd International Workshop on Cognitive Information Processing (CIP), Baiona, Spain, 28–30 May 2012.
- Fuentes, D.; Gonzalez-Abril, L.; Angulo, C.; Ortega, J.A. Online motion recognition using an accelerometer in a mobile device. Expert Syst. Appl. 2012, 39, 2461–2465. [Google Scholar] [CrossRef]
- Godfrey, A.; Bourke, A.K.; Ólaighin, G.M.; van de Ven, P.; Nelson, J. Activity classification using a single chest mounted tri-axial accelerometer. Med. Eng. Phys. 2011, 33, 1127–1135. [Google Scholar] [CrossRef] [PubMed]
- Milosevic, M.; Milenkovic, A.; Jovanov, E. mHealth @ UAH: Computing Infrastructure for Mobile Health and Wellness Monitoring. XRDS 2013, 20, 43–49. [Google Scholar] [CrossRef]
- Podsiadlo, D.; Richardson, S. The timed “Up & Go”: A test of basic functional mobility for frail elderly persons. J. Am. Geriatr. Soc. 1991, 39, 142–148. [Google Scholar] [PubMed]
- CDC The Timed Up and Go (TUG) Test. Available online: http://www.cdc.gov/steadi/pdf/tug_test-a.pdf (accessed on 31 January 2016).
- Milosevic, M.; Jovanov, E.; Milenkovic, A. Quantifying Timed-Up-and-Go test: A smartphone implementation. In Proceedings of the 2013 IEEE International Conference on Body Sensor Networks (BSN), Cambridge, MA, USA, 6–9 May 2013.
- Csuka, M.; McCarty, D.J. Simple method for measurement of lower extremity muscle strength. Am. J. Med. 1985, 78, 77–81. [Google Scholar] [CrossRef]
- Lord, S.R.; Murray, S.M.; Chapman, K.; Munro, B.; Tiedemann, A. Sit-to-Stand Performance Depends on Sensation, Speed, Balance, and Psychological Status in Addition to Strength in Older People. J. Gerontol. A Biol. Sci. Med. Sci. 2002, 57, M539–M543. [Google Scholar] [CrossRef] [PubMed]
- Whitney, S.L.; Wrisley, D.M.; Marchetti, G.F.; Gee, M.A.; Redfern, M.S.; Furman, J.M. Clinical measurement of sit-to-stand performance in people with balance disorders: Validity of data for the Five-Times-Sit-to-Stand Test. Phys. Ther. 2005, 85, 1034–1045. [Google Scholar] [PubMed]
- Buatois, S.; Miljkovic, D.; Manckoundia, P.; Gueguen, R.; Miget, P.; Vançon, G.; Perrin, P.; Benetos, A. Five times sit to stand test is a predictor of recurrent falls in healthy community-living subjects aged 65 and older. J. Am. Geriatr. Soc. 2008, 56, 1575–1577. [Google Scholar] [CrossRef] [PubMed]
- CDC 30-Second Chair Stand Test. Available online: http://www.cdc.gov/steadi/pdf/30_second_chair_stand_test-a.pdf (accessed on 31 January 2016).
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).