Development of a Virtual Reality-Based Game Approach for Supporting Sensory Processing Disorders Treatment †
Abstract
1. Introduction
2. Related Works
2.1. Sensory Processing Disorder (SPD)
2.2. Vestibular Disorders
2.3. Autism Spectrum Disorder (ASD)
2.4. Attention Deficit Hyperactivity Disorder (ADHD)
2.5. Speech Disorder
2.6. Summary
3. Developing an SPD Treatment Support System
3.1. Requirements
3.2. Development Tools
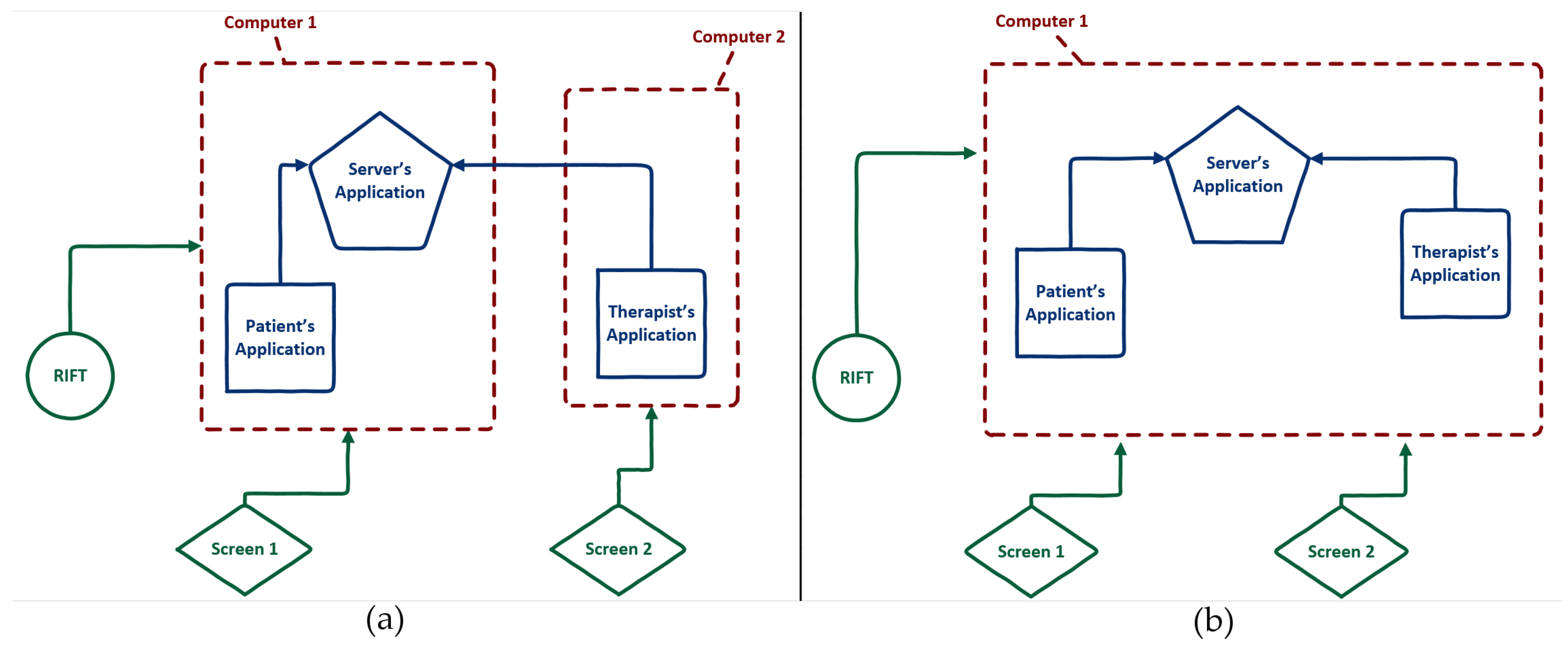
3.3. System’s Architecture
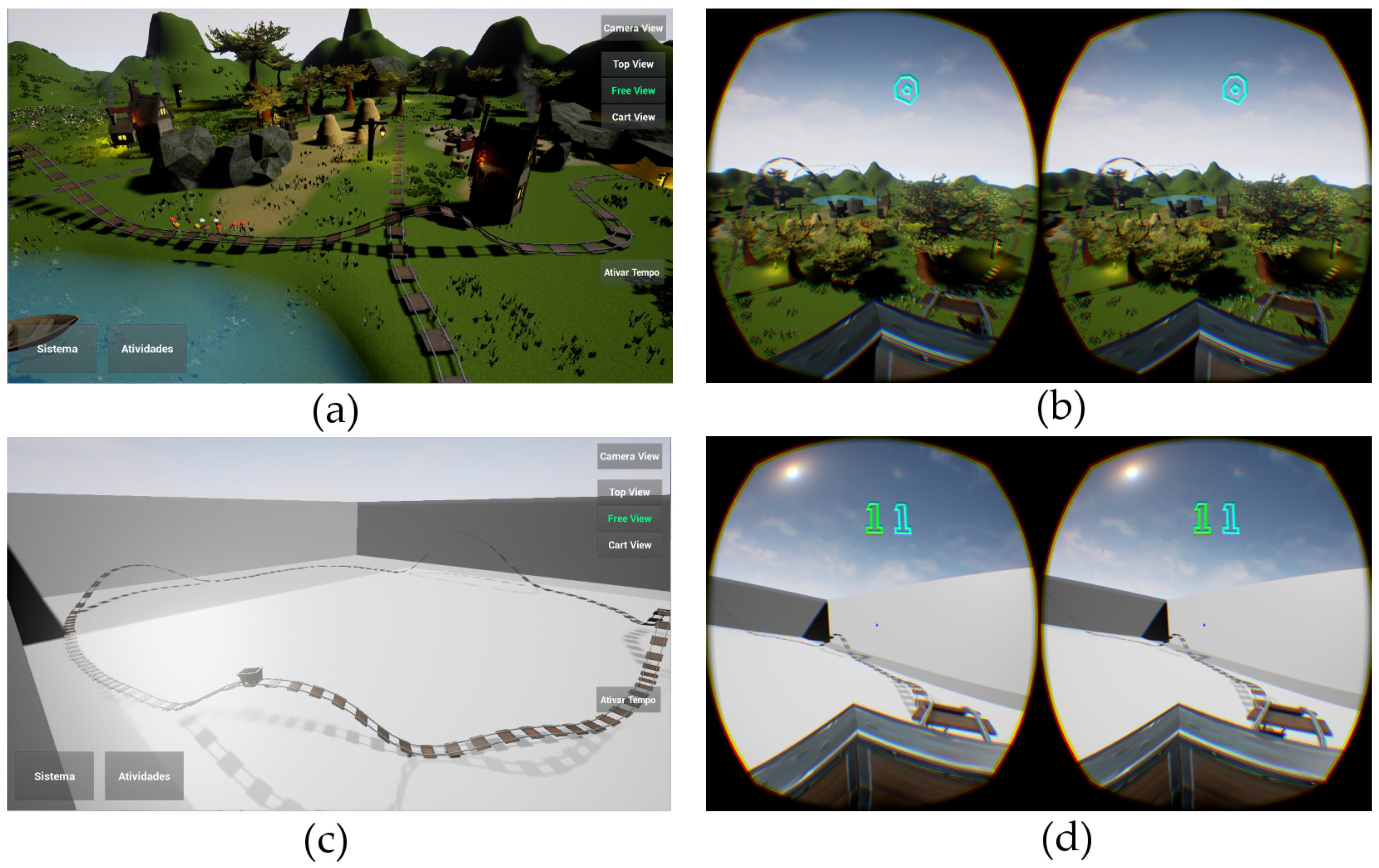
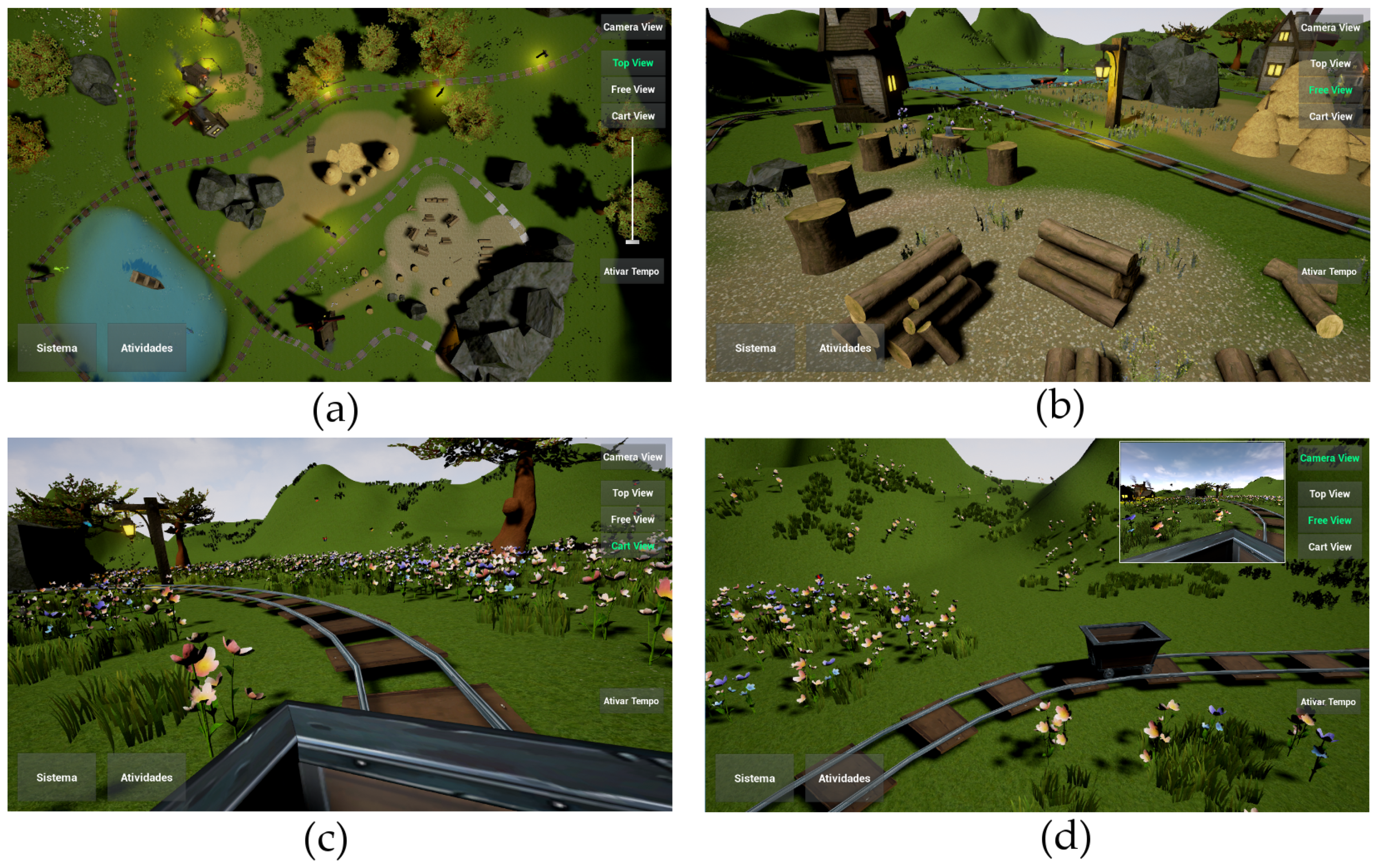
3.4. Imaginator
- Top View: The therapist views the world from above. It is possible to move the view window using the directional arrow keys that move left/right/front/back. In addition, it is also possible to zoom in or out of the scene by changing a slide control.
- Free View: It positions the therapist’s perspective in the center of the map. From this position, therapists can rotate their view using the mouse, turning left/right or up/down. Using the directional arrows on the keyboard, it is possible to move around following the orientation set by the mouse. For example, if the therapists position their visual field upwards (looking at the sky) and press the Up/Down directional arrow it will move towards the sky/ground.
- Kart View: It positions the therapists view within the cart, as a first person perspective. It is the same perspective that is being seen by patients. Notice that in this view, the therapist does not have any control of how the view changes, it moves along with the cart.
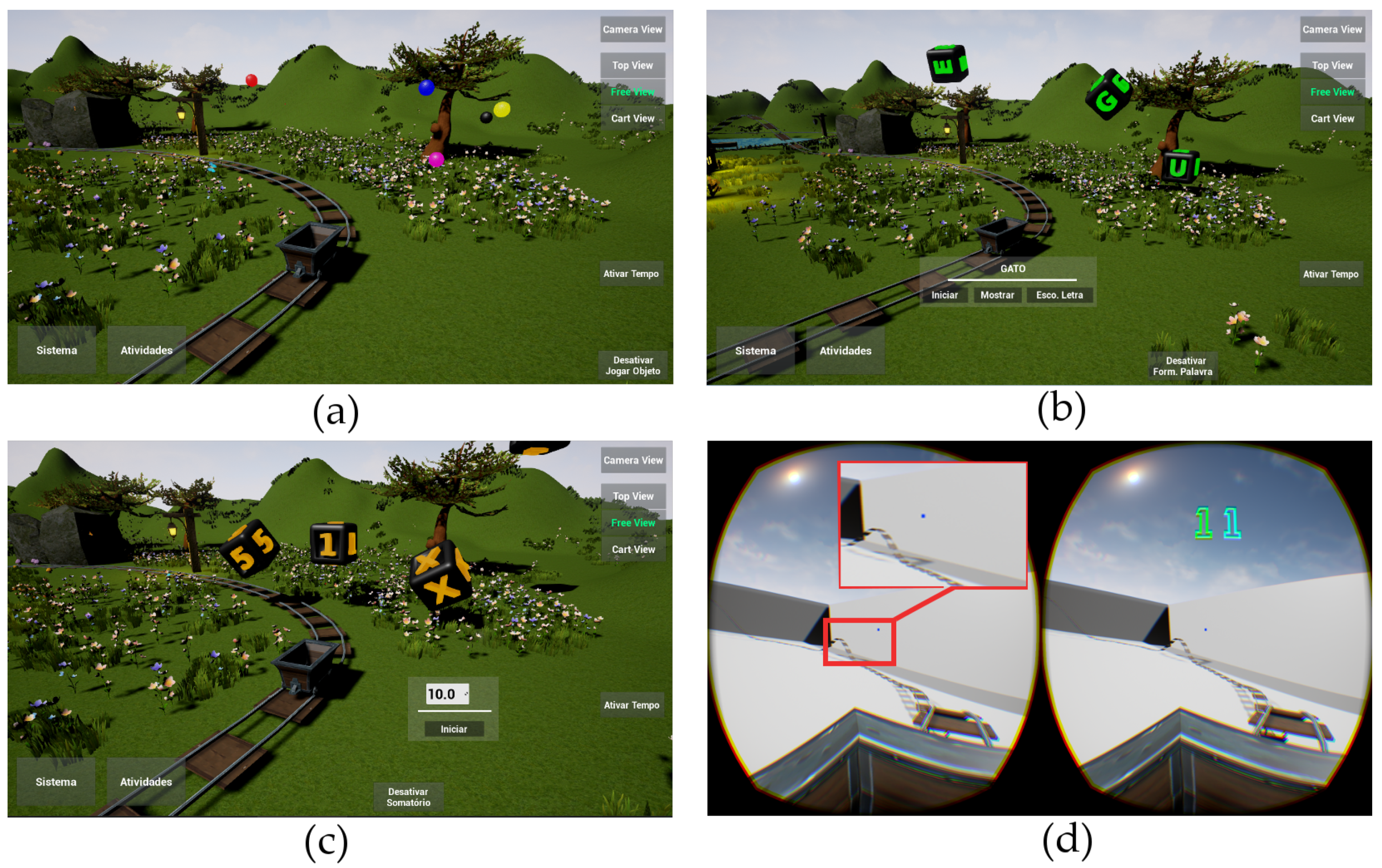
- Playing Ball: In this game, the goal is to hit a moving ball of a specific color defined by the OT (see Figure 5a). At each hit the player’s score increases and another ball automatically appears next to the player’s cart. The therapist may define if all balls should be the same color, or if the balls should be of different colors (increasing the difficulty for the patient to hit balls). If the patient looks long enough for a ball of a different color the system will count it as an error.
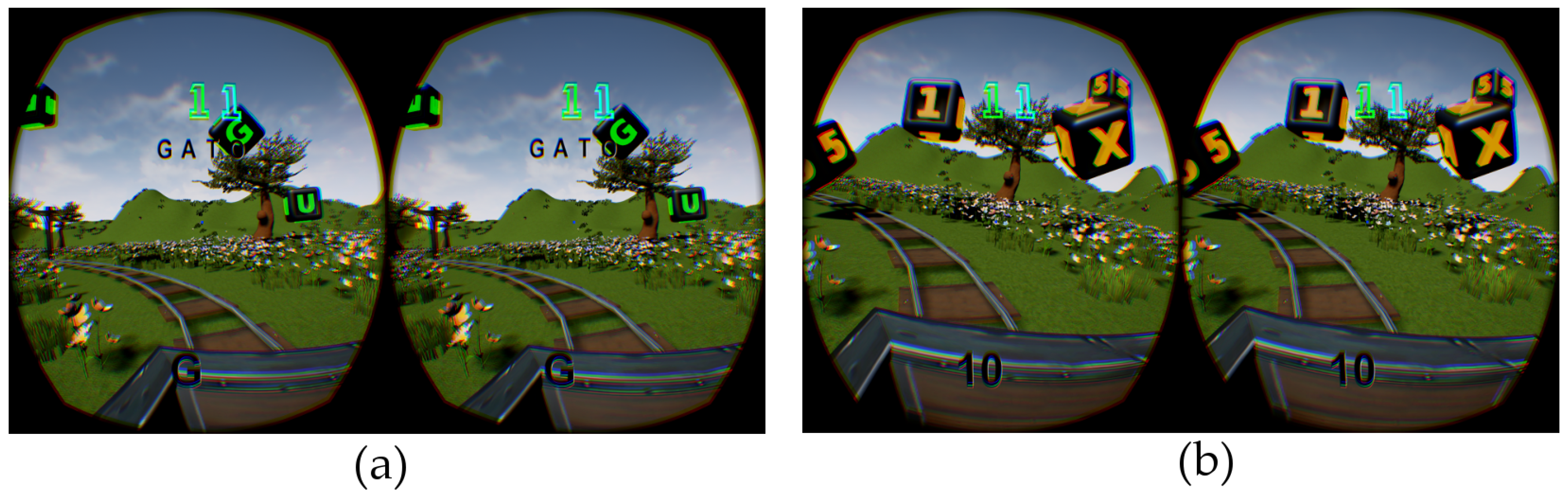
- Forming Words: In this activity, the goal is to hit moving letters in the correct order to form the word shown (see Figure 5b). The OT is responsible for choosing the word in each turn of the game. Each letter is represented in the game by a virtual cube which depicts the letter in its six sides. The word inserted into the system is displayed on the patient’s interface (see Figure 6a) and remains available until it is completed. Whenever the player hits a cube with the correct letter, it is instantly colored at the interface, and the next letter is highlighted. During the activity the system also generates and drops random letters that are not part of the word being formed. Imaginator also allows the OT to increase the level of difficulty of the game, by choosing the option to present the letters of the word out of order. In this case, whenever a letter present in the word is shown, the player will need to hit it. If the player hits a letter which in not present in the word it will be considered an error.
- Summation: In this activity the goal is to choose numbers that will add up to a predefined value (see Figure 5c). As in the Forming Words game, the numbers will be represented in moving cubes which the player will select by looking at them. The patients’ interface shows the final value to be achieved, but not the resulting partial sum (see Figure 6b). Whenever players believe they have reached the intended sum, they should look at a cube that has the letter “X” stamped which is always available in the scenario so players can indicate the end of the game. If the player achieved the intended sum he/she scores, otherwise Imaginator counts it as an error. The OTs are responsible for choosing the final sum intended. They also have the choice to define a range of numbers and let Imaginator randomly choose a number within this range. The final intended sum can be changed by the OT at any moment. Furthermore, the system allows OTs to control which numbers will be used in the activity. The numbers range from (1–9), but a summation activity can be set up to spawn only the number 5, or only even numbers, or any other combinations.
- Select one of the two available scenarios (The Box or Medieval).
- Add or remove predefined groups of virtual objects available in the medieval scenario (houses, ornaments, trees and stones).
- Turn on or off audio effects from the virtual environment (e.g., water noise, tree leafs noise, insects’ noise, wind noise, etc.) or from the system (e.g., cart movement noise, the background music, ball/cube bouncing noise, hit ball/cube noise, etc.)
- Choose among the different roller-coaster tracks, which have different amounts of ascents and descents.
- Modify the speed of the patient’s cart (i.e., the minimum or maximum velocity) or change it to an idle state.
- Change the color (Imaginator offers 10 different color options) of the goal object (e.g., ball, letter/number, edges or background of the cubes).
- Modify the size of the goal object (e.g., ball, cube).
- Change the period of time the user is required to focus on the goal object for it be considered a hit by the system (in seconds).
- Change the period of time (in seconds) that the goal object stays in the virtual environment.
- Change activity specific option settings (e.g., generating or not additional balls in the Playing Ball game that could confuse the patient, or shuffling the letters in Forming Word game).
4. Evaluation
4.1. Methodology
- Presentation and initial interview: First, Imaginator was installed at the OTs workplace. The equipment was comprised of one computer (with processing level suitable to run the simulator at 75+ frames per second), two monitors and the Oculus Rift. Then we presented the system to the therapists, including its settings and features. We also, handed and explained to them a short step-by-step manual on how to initialize Imaginator. The OTs could interrupt and ask any questions or clear doubts they had. This presentation took about 1 h.Next, we conducted a short interview containing 8 open questions that aimed at collecting data about their profile and experience in SPD, as well as their previous experience in using technologies in treatments. Then we asked questions about their first impressions regarding Imaginator (the design and graphics of the simulator, the realism of the movements, about their feeling of being inside the virtual environment, and the sound effects). These first interviews took from 10 to 15 min.
- Usage period: Imaginator stayed at the therapists workplace for a period of 2 to 3 weeks. During this time, OTs should decide whether they would the system with any patient, and in case they did, with which patients, how often and how it would fit into their therapy plan.
- Final interview: After the 2 to 3 weeks usage period, we scheduled a time to collect the system and conduct a second interview with the OTs. The goal of this second interview was to collect data on the OTs’ experience in using Imaginator in their treatments, their insights and attitudes towards the system.This interview’s script contained 12 open questions, divided into 2 main thematic blocks: the first one was about their use of the system in therapy, and the second their views about the system itself. For the first block, we addressed questions regarding what stimuli they believe were affected by the simulator, their thoughts about applying the VR solution to SPD treatments, how they selected patients to use the system and if they perceived any benefits or costs associated to the use of the system in their treatments. For the second block, we addressed questions related to the system, such as its interface, configuration of activities and possible improvements. In average the interviews had a duration of 25 to 35 min.
4.2. Execution
4.3. Results
4.3.1. Category 1: The Simulator Generates the Sense of Presence in the Virtual Space
4.3.2. Category 2: The System Generated Stimuli in More than One Sense
4.3.3. Category 3: Patients Felt Motivated to Use the System
4.3.4. Category 4: The System Caused Positive Changes in Patients’ Behavior or Attitude
4.3.5. Category 5: The System Caused Adverse Reactions in Some Patients
4.3.6. Category 6: Importance of Customization in the System
4.3.7. Category 7: Content Diversity Is Necessary in order to Maintain Patients’ Interest in the System
4.3.8. Category 8: Suggestions for Improving the System
4.3.9. Category 9: Therapists Would Consider Using the System as a Resource for Treatments
5. Discussion
5.1. Use of Imaginator in SPD Treatment
5.2. Comments on the Imaginator, Criticism and Suggestions
- Turn on the computer (using the two monitors setup), and wait for it to initialize the operating system.
- Log into the computer through one of the monitors (one of them had password) and wait for the interface of the Oculus Rift to be initialized.
- Initialize the OT’s interface by clicking on the specific icon, and then dragging its window to the second computer monitor.
- Initialize the patients’ interface, by clicking on the specific icon, and once it was running, disable the security message that appears within the HMD.
6. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| ADHD | Attention Deficit Hyperactivity Disorder |
| ASD | Autism Spectrum Disorder |
| HMD | Head Mount Display |
| OT | Occupational Therapist |
| SPD | Sensory Processing Disorders |
| SSD | Speech Sound Disorders |
| VR | Virtual Reality |
References
- Kranowitz, C.S. The Out-Of-Sync Child: Recognizing and Coping with Sensory Processing Disorder; Penguin: London, UK, 2005. [Google Scholar]
- Ayres, A.J.; Robbins, J. Sensory Integration and the Child: Understanding Hidden Sensory Challenges; Western Psychological Services: Torrance, CA, USA, 2005. [Google Scholar]
- Fisher, A.; Murray, E.; Bundy, A. Sensory Integration: Theory and Practice; Davis, F.A., Ed.; Contemporary Perspectives in Rehabilitation; FA Davis: Philadelphia, PA, USA, 1991. [Google Scholar]
- Ben-Sasson, A.; Carter, A.; Briggs-Gowan, M. Sensory over-responsivity in elementary school: Prevalence and social-emotional correlates. J. Abnorm. Child Psychol. 2009, 37, 705–716. [Google Scholar] [CrossRef] [PubMed]
- Miller, L.J.; Schoen, S.A.; Mulligan, S.; Sullivan, J. Identification of Sensory Processing and Integration Symptom Clusters: A Preliminary Study. Occup. Ther. Int. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Ahn, R.R.; Miller, L.J.; Milberger, S.; McIntosh, D.N. Prevalence of parents’ perceptions of sensory processing disorders among kindergarten children. Am. J. Occup. Ther. 2004, 58, 287–293. [Google Scholar] [CrossRef] [PubMed]
- Abraham, D.; Braley, C.; Drobnjak, L. Sensory Processing 101; Ellechor Media, LLC: Portland, OR, USA, 2015. [Google Scholar]
- Oculus, V.R.L. Oculus Rift DK2. 2016. Available online: https://developer.oculus.com/blog/open-source-release-of-rift-dk2/ (accessed on 13 May 2019).
- Lubetzky, A.V.; Harel, D.; Lubetzky, E. On the effects of signal processing on sample entropy for postural control. PLoS ONE 2018, 13, e0193460. [Google Scholar] [CrossRef] [PubMed]
- Rausch, M.; Simon, J.E.; Starkey, C.; Grooms, D.R. Smartphone virtual reality to increase clinical balance assessment responsiveness. Phys. Ther. Sport 2018, 32, 207–211. [Google Scholar] [CrossRef] [PubMed]
- Lubetzky, A.V.; Kary, E.E.; Darmanin, H.; Hujsak, B.; Perlin, K. An Oculus platform to measure sensory integration for postural control in patients with vestibular dysfunction. In Proceedings of the 2017 International Conference on Virtual Rehabilitation (ICVR), Montreal, QC, Canada, 19–22 June 2017; pp. 1–7. [Google Scholar]
- Rodrigues, M.A.F.; Macedo, D.V.; Pontes, H.P.; Serpa, Y.R.; Serpa, Y.R. A serious game to improve posture and spinal health while having fun. In Proceedings of the 2016 IEEE International Conference on Serious Games and Applications for Health (SeGAH), Orlando, FL, USA, 11–13 May 2016; pp. 1–8. [Google Scholar]
- Bergeron, M.; Lortie, C.L.; Guitton, M.J. Use of virtual reality tools for vestibular disorders rehabilitation: A comprehensive analysis. Adv. Med. 2015, 2015, 916735. [Google Scholar] [CrossRef] [PubMed]
- McConville, K.M.V.; Milosevic, M. Active video game head movement inputs. Pers. Ubiquitous Comput. 2014, 18, 253–257. [Google Scholar] [CrossRef]
- Silva-Calpa, G.F.M.; Raposo, A.B.; Suplino, M. CoASD: A tabletop game to support the collaborative work of users with autism spectrum disorder. In Proceedings of the 2018 IEEE 6th International Conference on Serious Games and Applications for Health (SeGAH), Vienna, Austria, 16–18 May 2018; pp. 1–8. [Google Scholar]
- Barajas, A.O.; Al Osman, H.; Shirmohammadi, S. A Serious Game for children with Autism Spectrum Disorder as a tool for play therapy. In Proceedings of the 2017 IEEE 5th International Conference on Serious Games and Applications for Health (SeGAH), Perth, Australia, 2–4 April 2017; pp. 1–7. [Google Scholar]
- Sturm, D.; Peppe, E.; Ploog, B. eMot-iCan: Design of an assessment game for emotion recognition in players with Autism. In Proceedings of the 2016 IEEE International Conference on Serious Games and Applications for Health (SeGAH), Orlando, FL, USA, 11–13 May 2016; pp. 1–7. [Google Scholar]
- Hughes, D.E.; Vasquez, E.; Nicsinger, E. Improving perspective taking and empathy in children with autism spectrum disorder. In Proceedings of the 2016 IEEE International Conference on Serious Games and Applications for Health (SeGAH), Orlando, FL, USA, 11–13 May 2016; pp. 1–5. [Google Scholar]
- Silva, G.; Raposo, A.; Suplino, M. Exploring collaboration patterns in a multitouch game to encourage social interaction and collaboration among users with autism spectrum disorder. Comput. Support. Coop. Work. 2015, 24, 149–175. [Google Scholar] [CrossRef]
- Ribeiro, P.C.; Raposo, A.B. ComFiM: A game for multitouch devices to encourage communication between people with autism. In Proceedings of the 2014 IEEE 3rd International Conference on Serious Games and Applications for Health (SeGAH), Rio de Janeiro, Brazil, 14–16 May 2014; pp. 1–8. [Google Scholar]
- Avila-Pesantez, D.; Rivera, L.A.; Vaca-Cardenas, L.; Aguayo, S.; Zuñiga, L. Towards the improvement of ADHD children through augmented reality serious games: Preliminary results. In Proceedings of the 2018 IEEE Global Engineering Education Conference (EDUCON), Tenerife, Spain, 17–20 April 2018; pp. 843–848. [Google Scholar]
- Alchalcabi, A.E.; Eddin, A.N.; Shirmohammadi, S. More attention, less deficit: Wearable EEG-based serious game for focus improvement. In Proceedings of the 2017 IEEE 5th International Conference on Serious Games and Applications for Health (SeGAH), Perth, Australia, 2–4 April 2017; pp. 1–8. [Google Scholar]
- Rohani, D.A.; Sorensen, H.B.; Puthusserypady, S. Brain-computer interface using P300 and virtual reality: a gaming approach for treating ADHD. In Proceedings of the 36th International Conference of the IEEE Engineering in Medicine and Biology Society, Chicago, IL, USA, 26–30 August 2014; pp. 3606–3609. [Google Scholar]
- Mandryk, R.L.; Dielschneider, S.; Kalyn, M.R.; Bertram, C.P.; Gaetz, M.; Doucette, A.; Taylor, B.A.; Orr, A.P.; Keiver, K. Games as neurofeedback training for children with FASD. In Proceedings of the 12th International Conference on Interaction Design and Children, New York, NY, USA, 24–27 June 2013; pp. 165–172. [Google Scholar]
- Santos, F.E.; Bastos, A.P.; Andrade, L.C.; Revoredo, K.; Mattos, P. Assessment of ADHD through a computer game: An experiment with a sample of students. In Proceedings of the 2011 Third International Conference on Games and Virtual Worlds for Serious Applications (VS-GAMES), Athens, Greece, 4–6 May 2011; pp. 104–111. [Google Scholar]
- Nasiri, N.; Shirmohammadi, S.; Rashed, A. A serious game for children with speech disorders and hearing problems. In Proceedings of the 2017 IEEE 5th International Conference on Serious Games and Applications for Health (SeGAH), Perth, Australia, 2–4 April 2017; pp. 1–7. [Google Scholar]
- Grossinho, A.; Guimaraes, I.; Magalhaes, J.; Cavaco, S. Robust phoneme recognition for a speech therapy environment. In Proceedings of the 2016 IEEE International Conference on Serious Games and Applications for Health (SeGAH), Orlando, FL, USA, 11–13 May 2016; pp. 1–7. [Google Scholar]
- Chuang, T.Y.; Kuo, M.S.; Fan, P.L.; Hsu, Y.W. A kinect-based motion-sensing game therapy to foster the learning of children with sensory integration dysfunction. Educ. Technol. Res. Dev. 2017, 65, 699–717. [Google Scholar] [CrossRef]
- Chuang, T.Y.; Kuo, M.S. A Motion-sensing game-based therapy to foster the learning of children with sensory integration dysfunction. J. Educ. Technol. Soc. 2016, 19, 4. [Google Scholar] [CrossRef]
- Kandalaft, M.R.; Didehbani, N.; Krawczyk, D.C.; Allen, T.T.; Chapman, S.B. Virtual reality social cognition training for young adults with high-functioning autism. J. Autism Dev. Disord. 2013, 43, 34–44. [Google Scholar] [CrossRef] [PubMed]
- Herrera, G.; Alcantud, F.; Jordan, R.; Blanquer, A.; Labajo, G.; De Pablo, C. Development of symbolic play through the use of virtual reality tools in children with autistic spectrum disorders Two case studies. wAutism 2008, 12, 143–157. [Google Scholar]
- Miller, L.J.; Fuller, D.A.; Roetenberg, J. Sensational Kids Revised Edition: Hope and Help for Children with Sensory Processing Disorder (SPD); Penguin: London, UK, 2014. [Google Scholar]
- Jerald, J. The VR Book: Human-Centered Design for Virtual Reality; Morgan & Claypool: San Rafael, CA, USA, 2015. [Google Scholar]
- Kim, J.; Chung, C.Y.; Nakamura, S.; Palmisano, S.; Khuu, S.K. The Oculus Rift: A cost-effective tool for studying visual-vestibular interactions in self-motion perception. Front. Psychol. 2015, 6. [Google Scholar] [CrossRef] [PubMed]
- Riccelli, R.; Indovina, I.; Staab, J.P.; Nigro, S.; Augimeri, A.; Lacquaniti, F.; Passamonti, L. Neuroticism modulates brain visuo-vestibular and anxiety systems during a virtual rollercoaster task. Hum. Brain Mapp. 2017, 38, 715–726. [Google Scholar] [CrossRef] [PubMed]
- Epic Games, I. Unreal Engine 4. 2017. Available online: https://www.unrealengine.com/en-US/what-is-unreal-engine-4 (accessed on 13 May 2019).
- Lazar, J.; Feng, J.H.; Hochheiser, H. Research Methods in Human-Computer Interaction; Morgan Kaufmann: Burlington, MA, USA, 2017. [Google Scholar]
- Blandford, A. Semi-structured qualitative studies. In The Encyclopedia of Human-Computer Interaction; Soegaard, M., Dam, R.F., Eds.; The Interaction Design Foundation: Aarhus, Denmark, 2012; Chapter 52. [Google Scholar]
- Nicolaci-da Costa, A.M.; Leitão, C.F.; Romão-Dias, D. How to Know Users through the Underlying Discourse Unveiling Method (UDUM). In Proceedings of the VI Brazilian Symposium of Human Factors in Computing Systems (IHC), Porto Alegre, Brazil, 10–12 December 2004; pp. 47–56. [Google Scholar]
- Slater, M.; Wilbur, S. A framework for immersive virtual environments (FIVE): Speculations on the role of presence in virtual environments. Presence Teleoperators Virtual Environ. 1997, 6, 603–616. [Google Scholar] [CrossRef]
- LaViola, J.J., Jr. A discussion of cybersickness in virtual environments. ACM SIGCHI Bull. 2000, 32, 47–56. [Google Scholar] [CrossRef]
- Anthes, C.; García-Hernández, R.J.; Wiedemann, M.; Kranzlmüller, D. State of the art of virtual reality technology. In Proceedings of the 2016 IEEE Aerospace Conference, Big Sky, MT, USA, 5–12 March 2016; pp. 1–19. [Google Scholar]
- Kiryu, T.; So, R.H. Sensation of presence and cybersickness in applications of virtual reality for advanced rehabilitation. J. NeuroEng. Rehabil. 2007, 4, 34. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, A.S.; Kim, G.J. A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence Teleoperators Virtual Environ. 2005, 14, 119–146. [Google Scholar] [CrossRef]
- Davis, S.; Nesbitt, K.; Nalivaiko, E. Comparing the onset of cybersickness using the Oculus Rift and two virtual roller coasters. In Proceedings of the 11th Australasian Conference on Interactive Entertainment (IE 2015), Sydney, Australia, 27–30 January 2015; Volume 27, p. 30. [Google Scholar]
- Nie, G.Y.; Duh, H.B.L.; Liu, Y.; Wang, Y. Analysis on Mitigation of Visually Induced Motion Sickness by Applying Dynamical Blurring on a User’s Retina. IEEE Trans. Vis. Comput. Graph. 2019. [Google Scholar] [CrossRef] [PubMed]
- Zaidi, S.F.M.; Male, T. Experimenting Novel Virtual-reality Immersion Strategy to Alleviate Cybersickness. In Proceedings of the 24th ACM Symposium on Virtual Reality Software and Technology, Tokyo, Japan, 28 November–1 December 2018; ACM: New York, NY, USA, 2018; pp. 89:1–89:2. [Google Scholar] [CrossRef]
- Kilteni, K.; Groten, R.; Slater, M. The sense of embodiment in virtual reality. Presence Teleoperators Virtual Environ. 2012, 21, 373–387. [Google Scholar] [CrossRef]
- Jüris, L. Hyperacusis: Clinical Studies and Effect of Cognitive Behaviour Therapy. Ph.D. Thesis, Acta Universitatis Upsaliensis, Uppsala University, Uppsala, Sweden, 2013. [Google Scholar]

© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rossi, H.; Prates, R.; Santos, S.; Ferreira, R. Development of a Virtual Reality-Based Game Approach for Supporting Sensory Processing Disorders Treatment. Information 2019, 10, 177. https://doi.org/10.3390/info10050177
Rossi H, Prates R, Santos S, Ferreira R. Development of a Virtual Reality-Based Game Approach for Supporting Sensory Processing Disorders Treatment. Information. 2019; 10(5):177. https://doi.org/10.3390/info10050177
Chicago/Turabian StyleRossi, Henrique, Raquel Prates, Sibele Santos, and Renato Ferreira. 2019. "Development of a Virtual Reality-Based Game Approach for Supporting Sensory Processing Disorders Treatment" Information 10, no. 5: 177. https://doi.org/10.3390/info10050177
APA StyleRossi, H., Prates, R., Santos, S., & Ferreira, R. (2019). Development of a Virtual Reality-Based Game Approach for Supporting Sensory Processing Disorders Treatment. Information, 10(5), 177. https://doi.org/10.3390/info10050177




