The Effect of Spiritual Care on Depression in Patients Following Coronary Artery Bypass Surgery: A Randomized Controlled Trial
Abstract
1. Introduction
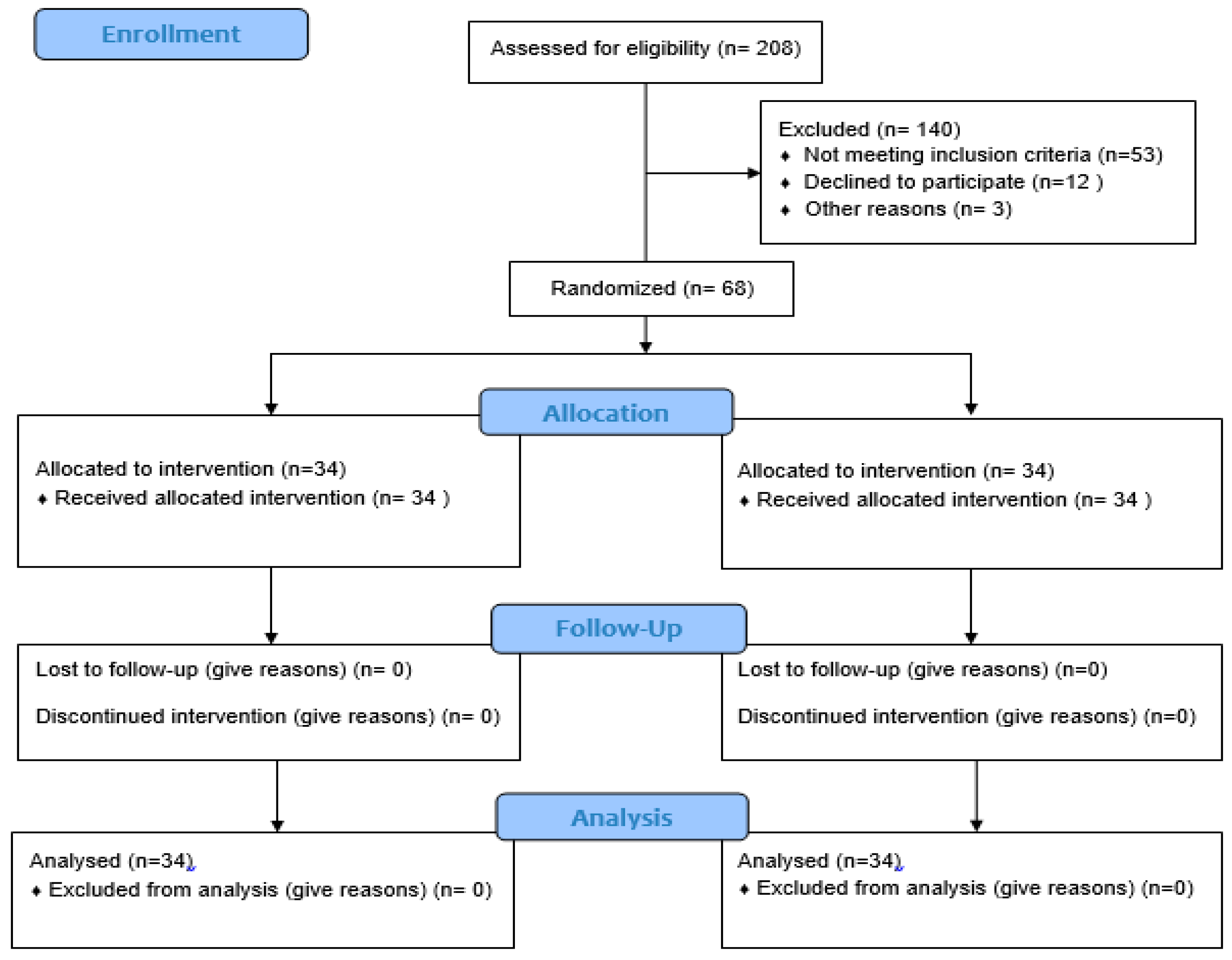
2. Methods
2.1. Design
2.2. Instrument and Data Analysis
3. Results
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Adib-Hajbaghery, Mohsen, and Zahra Saeadnejad. 2016. Barriers to Provide Patients Admitted to Hospitals in Kashan with Spiritual Care: Nurses’ Viewpoints. Medical Ethics Journal 10: 49–59. [Google Scholar] [CrossRef]
- Bekelman, Davia B., Sydney M. Dy, Diane M. Becker, Ilan S. Wittstein, Danetta E. Hendricks, Traci E. Yamashita, and Sheldon H. Gottlieb. 2007. Spiritual well-being and depression in patients with heart failure. Journal of General Internal Medicine 22: 470–77. [Google Scholar] [CrossRef] [PubMed]
- Braxton, Nikia D., Delia L. Lang, Jessica M. Sales, Gina M. Wingood, and Ralph J. DiClemente. 2007. The role of spirituality in sustaining the psychological well-being of HIV-positive black women. Women & Health 46: 113–29. [Google Scholar]
- Büssing, Arndt, Thomas Ostermann, and Peter F. Matthiessen. 2005. Role of religion and spirituality in medical patients: Confirmatory results with the SpREUK questionnaire. Health and Quality of Life Outcomes 3: 10. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Carney, Robert M., and Kenneth E. Freedland. 2008. Depression in patients with coronary heart disease. The American Journal of Medicine 121: S20–27. [Google Scholar] [CrossRef] [PubMed]
- Doering, Lynn V., Debra K. Moser, Walter Lemankiewicz, Cristina Luper, and Steven Khan. 2005. Depression, healing, and recovery from coronary artery bypass surgery. American Journal of Critical Care 14: 316–24. [Google Scholar] [PubMed]
- Duits, Annelien, Hugo Duivenvoorden, Saskia Boeke, Bas Mochtar, Jan Passchier, and Ruud Erdman. 2002. Psychological and somatic factors in patients undergoing coronary artery bypass graft surgery: Towards building a psychological framework. Psychology and Health 17: 159–71. [Google Scholar] [CrossRef]
- Eisenberg, Mark J., Kristian B. Filion, Arik Azoulay, Anya C. Brox, Seema Haider, and Louise Pilote. 2005. Outcomes and cost of coronary artery bypass graft surgery in the United States and Canada. Archives of Internal Medicine 165: 1506–13. [Google Scholar] [CrossRef] [PubMed]
- Falahi-Khoshknab, Masoud, and Nahid Ghazanfari. 2007. The Effect of Group Recreational Activities on the Self Care Skills of Schizophrenic Patients. IJNR 2: 25–30. [Google Scholar]
- Fatemi, Mir Massoud, Robab Nazari, Mahboubeh Safavi, Mohammad Kazem Naini, and Mohammad Taghi Savadpour. 2016. The Relationships between nurses’ spirituality and PATIENTS’SATISFACTION in the Hospitals of Ardabil University of Medical Science. Medical Ethics Journal 5: 141–59. [Google Scholar]
- Freedland, Kenneth E., Judith A. Skala, Robert M. Carney, Eugene H. Rubin, Patrick Lustman, Victor G. Dávila-Román, Brain C. Steinmeyer, and Charles W Hogue. 2009. Treatment of depression after coronary artery bypass surgery: A randomized controlled trial. Archives of General Psychiatry 66: 387–96. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, Robyn, and Sharon McKinley. 2009. Anxiety, depression and perceived control in patients having coronary artery bypass grafts. Journal of Advanced Nursing 65: 2386–96. [Google Scholar] [CrossRef] [PubMed]
- Hanifi, Nasrin, Nasrin Bahraminejad, Tayebeh Mirzaee, Fazilillah Ahmadi, Mohammad Khani, and Leila Taran. 2012. The effect of orientation program on stress, anxiety and depression of patients undergoing coronary angiography. IJNR 7: 1–8. [Google Scholar]
- Holzapfel, Nicole, Bernd Löwe, Beate Wild, Dieter Schellberg, Christian Zugck, Andrew Remppis, Hugo A. Katus, Markus Haass, Bernhard Rauch, Jana Jünger, and et al. 2009. Self-care and depression in patients with chronic heart failure. Heart & Lung: The Journal of Acute and Critical Care 38: 392–97. [Google Scholar] [PubMed]
- Hosseini, Mohammadali, Patricia M. Davidson, Masoud Fallahi Khoshknab, and Anna Green. 2013. Spiritual and religious interventions in health care: An integrative review. Iranian Rehabilitation Journal 11: 87–93. [Google Scholar]
- Jamshidi, Nhid, Abas Abaszade, and Majid Najafi-Kaliani. 2012. Stress, anxiety and depression of patients before coronary angiography. Zahedan Journal of Research in Medical Sciences 13: 29. [Google Scholar]
- Karimollahi, Mansoureh, Heidar ali Abedi, and Alireza Yousefi. 2008. Antecedents of spiritual distress experienced by Iranian Muslim patients. Research Journal of Biological Science 3: 1815–46. [Google Scholar]
- Koenig, Harold G. 2007. Religion and remission of depression in medical inpatients with heart failure/pulmonary disease. The Journal of Nervous and Mental Disease 195: 389–95. [Google Scholar] [PubMed]
- McCoubrie, Rachel C., and Andrew N. Davies. 2006. Is there a correlation between spirituality and anxiety and depression in patients with advanced cancer? Supportive Care in Cancer 14: 379. [Google Scholar] [CrossRef] [PubMed]
- Melhem, Ghaith Ahmad Bani, Ruqayya S. Zeilani, Ossama Abed Zaqqout, Ashraf Ismail Aljwad, Mohammed Qasim Shawagfeh, and Maysoon Abd Al-Rahim. 2016. Nurses’ perceptions of spirituality and spiritual care giving: A comparison study among all health care sectors in Jordan. Indian Journal of Palliative Care 22: 42–49. [Google Scholar] [CrossRef] [PubMed]
- Nabolsi, Manar M., and Alexander M. Carson. 2011. Spirituality, illness and personal responsibility: The experience of Jordanian Muslim men with coronary artery disease. Scandinavian Journal of Caring Sciences 25: 716–24. [Google Scholar] [CrossRef] [PubMed]
- Oxman, Thomas E., Daniel H. Freeman, and Eric D. Manheimer. 1995. Lack of social participation or religious strength and comfort as risk factors for death after cardiac surgery in the elderly. Psychosomatic Medicine 57: 5–15. [Google Scholar] [CrossRef] [PubMed]
- Rafanelli, Chiara, Renzo Roncuzzi, and Yuri Milaneschi. 2006. Minor depression as a cardiac risk factor after coronary artery bypass surgery. Psychosomatics 47: 289–95. [Google Scholar] [CrossRef] [PubMed]
- Ravven, Simha, Caroline Bader, Armin Azar, and James L. Rudolph. 2013. Depressive symptoms after CABG surgery: A meta-analysis. Harvard Review of Psychiatry 21: 59–69. [Google Scholar] [CrossRef] [PubMed]
- Rippentrop, A. Elizabeth, Elizabeth M. Altmaier, Joseph J. Chen, Ernest M. Found, and Valerie J. Keffala. 2005. The relationship between religion/spirituality and physical health, mental health, and pain in a chronic pain population. Pain 116: 311–21. [Google Scholar] [CrossRef] [PubMed]
- Ross, Linda. 2006. Spiritual care in nursing: An overview of the research to date. Journal of Clinical Nursing 15: 852–62. [Google Scholar] [CrossRef] [PubMed]
- Rutledge, Thomas, Viola Vaccarino, B. Delia Johnson, Vera Bittner, Marian B. Olson, Sarah Elizabeth Linke, Carol E. Cornell, Wafia Eteiba, David Sheps, Jennifer Francis, and et al. 2009. Depression and cardiovascular health care costs among women with suspected myocardial ischemia: Prospective results from the WISE (Women’s Ischemia Syndrome Evaluation) Study. Journal of the American College of Cardiology 53: 176–83. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sahebi, Ali, Mohammad Javad Asghari, and Razie Sadat Salari. 2005. Validation of depression anxiety and stress scale (DASS-21) for an Iranian population. Iranian Psychologists. Available online: https://www.scienceopen.com/document?vid=7528f000-2e97-4811-8ff0-028faa5b3d8c (accessed on 14 May 2018).
- Smith, Timothy B., Jeremy Bartz, and P. Scott Richards. 2007. Outcomes of religious and spiritual adaptations to psychotherapy: A meta-analytic review. Psychotherapy Research 17: 643–55. [Google Scholar] [CrossRef]
- Stafford, Lesley, Michael Berk, Prasuna Reddy, and Henry J. Jackson. 2007. Comorbid depression and health-related quality of life in patients with coronary artery disease. Journal of Psychosomatic Research 62: 401–10. [Google Scholar] [CrossRef] [PubMed]
- Vural, Mutlu, Mehmet Acer, and Berfu Akbaš. 2008. The scores of Hamilton depression, anxiety, and panic agoraphobia rating scales in patients with acute coronary syndrome. Anatolian Journal of Cardiology/Anadolu Kardiyoloji Dergisi 8: 43–47. [Google Scholar] [PubMed]
- Whelan-Gales, Mary Ann, Mary T. Quinn Griffin, Judith Maloni, and Joyce J. Fitzpatrick. 2009. Spiritual well-being, spiritual practices, and depressive symptoms among elderly patients hospitalized with acute heart failure. Geriatric Nursing 30: 312–17. [Google Scholar] [CrossRef] [PubMed]
| p-Value | Intervention | Control | Groups | Variables | ||
|---|---|---|---|---|---|---|
| % | Count | % | Count | |||
| 0/307 | 48/4 | 15 | 61/3 | 19 | Male | Gender |
| 51/6 | 16 | 38/7 | 12 | Female | ||
| 6/5 | 2 | 12/9 | 4 | Illiterate | Education | |
| 0/233 | 35/5 | 11 | 32/3 | 10 | Elementary | |
| 22/6 | 7 | 38/7 | 12 | Junior high school | ||
| 35/5 | 11 | 16/1 | 5 | High school | ||
| 93/5 | 29 | 80/6 | 25 | Parents | Tutelage | |
| 0/130 | 6/5 | 2 | 19/4 | 6 | Care center | |
| 41/9 | 13 | 45/2 | 14 | ALL * | Cancer type | |
| 0/851 | 16/1 | 5 | 19/4 | 6 | CLL * | |
| 29 | 9 | 29 | 9 | AML * | ||
| 12/9 | 4 | 6/5 | 2 | CML * | ||
| 9/7 | 3 | 12/9 | 4 | Yes | History of psychological disorders | |
| 1/000 | 90/3 | 28 | 87/1 | 27 | No | |
| 0/508 | 14/5/(2/02) | 15 (2/86) | Age | |||
| 0/871 | 28 (12) | 30 (16) | Hospitalization period (days) | |||
| 0/622 | 5/9(3/65) | 6/38(4/03) | Number of chemotherapies | |||
| p-Value | t | SD | Mean | Group | |
|---|---|---|---|---|---|
| 0/606 | -0/519 | 13/99 | 58/93 | Intervention | Pain |
| 7/59 | 57/45 | Control | |||
| 0/331 | -0/980 | 6/89 | 36/16 | Intervention | Depression |
| 10/16 | 34/00 | control | |||
| P ** | P * | Mean ± SD | Group | ||
|---|---|---|---|---|---|
| 0/001 | <0/001 | 58/9±13/99 | Before | Intervention | Pain |
| 32/7±6/58 | After | ||||
| 0/126 | 57/4±4/59 | Before | Control | ||
| 53/29±13/25 | After | ||||
| <0/001 | <0/001 | 34/10±0/16 | Before | Intervention | Depression |
| 30/09±10/46 | After | ||||
| 0/221 | 36/16±6/89 | Before | Control | ||
| 18/19±9/31 | After | ||||
| Effect size | Mean ± SD | Group | ||
|---|---|---|---|---|
| −3.12 | 32/7± 6/58 | Intervention | Pain | |
| 53/29± 13/25 | Control | |||
| −1.13 | 30/09 ± 10/46 | Intervention | Depression | |
| 18/19 ±9/31 | Control | |||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tajbakhsh, F.; Hosseini, M.; Fallahi-Khoshknab, M.; Rokofian, A.; Rahgozar, M.; Mary Davidson, P. The Effect of Spiritual Care on Depression in Patients Following Coronary Artery Bypass Surgery: A Randomized Controlled Trial. Religions 2018, 9, 159. https://doi.org/10.3390/rel9050159
Tajbakhsh F, Hosseini M, Fallahi-Khoshknab M, Rokofian A, Rahgozar M, Mary Davidson P. The Effect of Spiritual Care on Depression in Patients Following Coronary Artery Bypass Surgery: A Randomized Controlled Trial. Religions. 2018; 9(5):159. https://doi.org/10.3390/rel9050159
Chicago/Turabian StyleTajbakhsh, Fereshteh, MohammadAli Hosseini, Masoud Fallahi-Khoshknab, Asghar Rokofian, Mehdi Rahgozar, and Patricia Mary Davidson. 2018. "The Effect of Spiritual Care on Depression in Patients Following Coronary Artery Bypass Surgery: A Randomized Controlled Trial" Religions 9, no. 5: 159. https://doi.org/10.3390/rel9050159
APA StyleTajbakhsh, F., Hosseini, M., Fallahi-Khoshknab, M., Rokofian, A., Rahgozar, M., & Mary Davidson, P. (2018). The Effect of Spiritual Care on Depression in Patients Following Coronary Artery Bypass Surgery: A Randomized Controlled Trial. Religions, 9(5), 159. https://doi.org/10.3390/rel9050159





