The Effectiveness of Spirituality-Centered Cognitive Therapy on Body Image, Sexual Function, Illness Perception and Intrusive Thoughts in Iranian Women after Mastectomy
Abstract
1. Introduction
2. Methodology
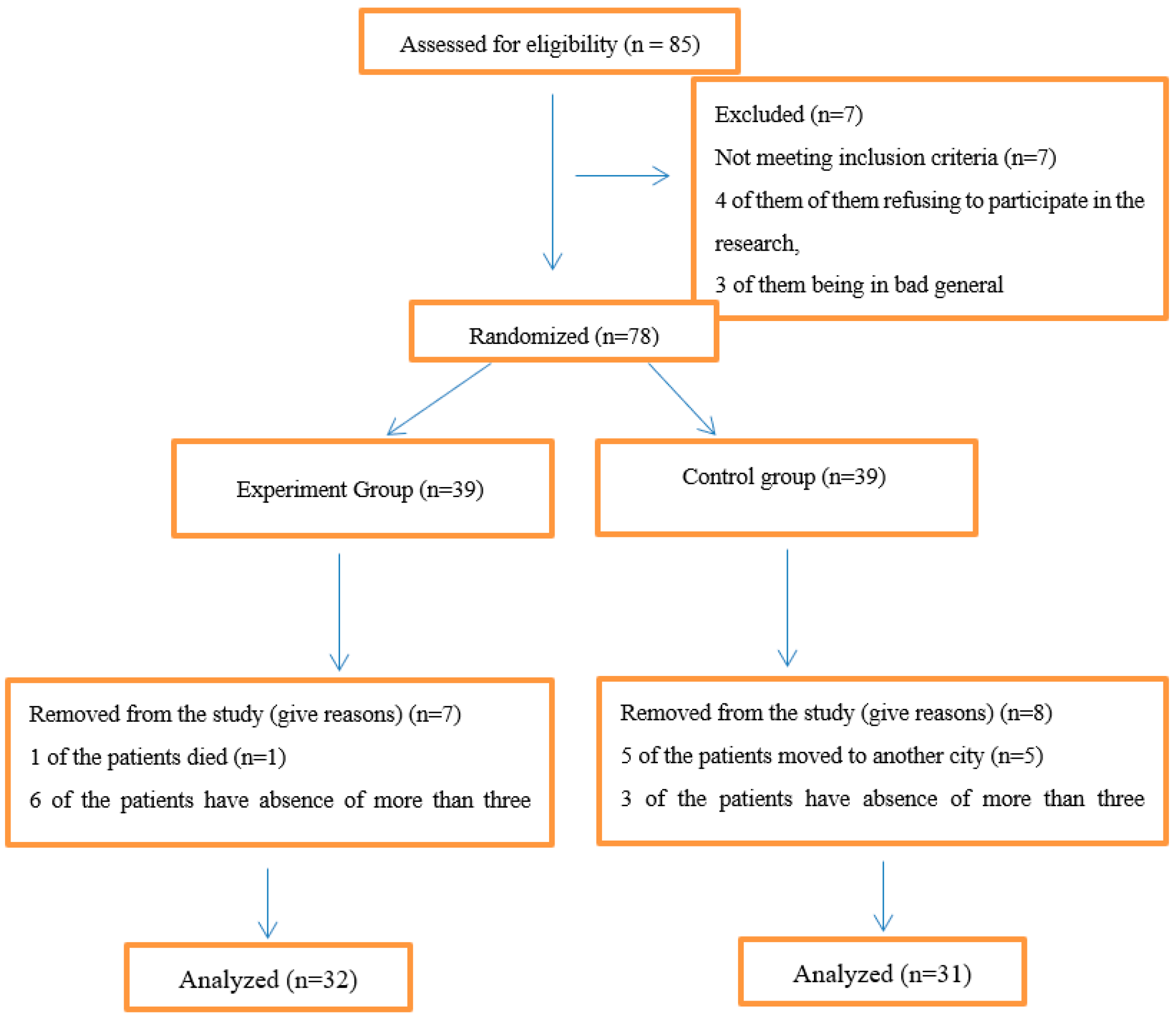
2.1. Participants
2.2. Measures
2.2.1. The Revised Illness Perception Questionnaire (IPQ-R)
2.2.2. Rumination Scale
2.2.3. Body Image and Relationship Scale
2.2.4. Female Sexual Function Index (FSFI-6)
2.2.5. Procedure
3. Analysis
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abdulkadiroğlu, Abdülkerim. 1996. Maneviyat Dünyamiz Üzerine Düşünceler [Thoughts on our world of spirituality]. Erdem İnsan ve Toplum Bilimleri Dergisi [Journal of Erdem Humanities and Social Sciences] 24: 707–16. [Google Scholar] [CrossRef]
- Abdul-Rahman, Zohair. 2017. İslam Maneviyatı ve Ruhani Refah [Islamic Spirituality and Spiritual Wellbeing]. Available online: https://yaqeeninstitute.org/read/paper/islam-maneviyati-ve-ruhani-refah (accessed on 25 April 2024).
- Akbari, Mahboobeh, Kashani F. Lotfi, and Sh Vaziri. 2017. The efficacy of four-factor psychotherapy on increasing sexual self-esteem in breast cancer survivors. Iranian Quarterly Journal of Breast Disease 10: 48–60. [Google Scholar]
- Albayrak, İsmail. 2015. İslam Dini Açısından ‘Din-Maneviyat’ İlişkisi [The relationship between ‘religion and spirituality’ in terms of Islam]. In Değerler Eğitimi-II [Values Education-II]. Edited by Recep Kaymakcan, Nuri Tınaz Zarife, Şeyma Altın, Mahmut Zengin, Ahmet Yasin Okudan and Hulusi Yiğit. pp. 107–16. Available online: https://www.academia.edu/44153950/%C4%B0SLAM_D%C4%B0N%C4%B0_A%C3%87ISINDAN_D%C4%B0N (accessed on 25 April 2024).
- Alinejad Mofrad, Samaneh, Ritin Fernandez, Heidi Lord, and Ibrahim Alananzeh. 2021. The impact of mastectomy on Iranian women sexuality and body image: A systematic review of qualitative studies. Supportive Care in Cancer 29: 5571–80. [Google Scholar] [CrossRef] [PubMed]
- Anagnostopoulos, Fotios, Julie Slater, and Deborah Fitzsimmons. 2010. Intrusive thoughts and psychological adjustment to breast cancer: Exploring the moderating and mediating role of global meaning and emotional expressivity. Journal of Clinical Psychology in Medical Settings 17: 137–49. [Google Scholar] [CrossRef] [PubMed]
- Aydın Sayılan, Aylin, and Melike Demir Doğan. 2020. Illness perception, perceived social support and quality of life in patients with diagnosis of cancer. European Journal of Cancer Care 29: e13252. [Google Scholar] [CrossRef]
- Basharpoor, Sajjad, Behnam NasriNasrabadi, Fazeleh Heidari, and Parviz Molavi. 2018. The role of health beliefs and illness perceptions in predicting health-promoting behaviors in cancer patients. Iranian Journal of Health Education and Health Promotion 6: 102–13. [Google Scholar] [CrossRef]
- Beatty, Lisa, and Bogda Koczwara. 2010. An effective study of a CBT group program for women with breast cancer. Clinical Psychologist 14: 45–53. [Google Scholar] [CrossRef]
- Brandberg, Yvonne, Kerstin Sandelin, Staffan Erikson, Göran Jurell, Annelie Liljegren, Annika Lindblom, Ann Lindén, Anna Von Wachenfeldt, Marie Wickman, and Brita Arver. 2008. Psychological reactions, quality of life, and body image after bilateral prophylactic mastectomy in women at high risk for breast cancer: A prospective 1-year follow-up study. Journal of Clinical Oncology 26: 3943–49. [Google Scholar] [CrossRef]
- Carnelli, Letizia, V. Di Mattei, Martina Mazzetti, Martina Bernardi, Rossella Di Pierro, Alice Bergamini, Francesca Pella, Giorgia Mangili, Lucio Sarno, and Massimo Candiani. 2017. Illness perception in gestational trophoblastic disease patients: How mental representations affect anxiety, depression, and infertility-related stress. Open Journal of Medical Psychology 6: 1–15. [Google Scholar] [CrossRef]
- Cohen, Adam B., and Harold G. Koenig. 2004. Religion and mental health. In Encyclopedia of Applied Psychology. Edited by Charles Spielberger. Cambridge: Elsevier Academic Press, vol. 3, pp. 255–58. [Google Scholar]
- Cook, Sharon A., Peter Salmon, Graham Dunn, Chris Holcombe, Philip Cornford, and Peter Fisher. 2015. The association of metacognitive beliefs with emotional distress after diagnosis of cancer. Health Psychology 34: 207–15. [Google Scholar] [CrossRef]
- Costanzo, Erin S., Susan K. Lutgendorf, and Susan L. Roeder. 2011. Common-sense beliefs about cancer and health practices among women completing treatment for breast cancer. Psychooncology 20: 53–61. [Google Scholar] [CrossRef]
- Coughlin, Steven S. 2008. Surviving cancer or other serious illness: A review of individual and community resources. CA Cancer Journal for Clinicians 58: 60–64. [Google Scholar] [CrossRef] [PubMed]
- Dadfar, Mahboubeh, David Lester, Yahya Turan, James A. Beshai, and Human-Friedrich Unterrainer. 2019. Validation of the Multidimensional Inventory for Religious Spiritual Well-being with Iranian samples. Mental Health, Religion & Culture 22: 591–601. [Google Scholar] [CrossRef]
- Dadfar, Mahboubeh, Merhardad Kazemzadeh Atoofi, and Atiye Rezaei. 2023. Effectiveness of religious spiritual integrated therapy (RSIT) for reduction of death distress in the Iranian outpatients with generalized anxiety disorder (GAD). Mankind Quarterly 63: 427–42. [Google Scholar] [CrossRef]
- Dehkhoda, Aida. 2013. The Effectiveness of Spirituality-Centered Cognitive Therapy on Reduction Depressive Symptoms in Mothers of Children with Cancer. Master’s thesis, University of Social Welfare and Rehabilitation Sciences, Tehran, Iran. [Google Scholar]
- Dempster, Martin, and Noleen K. McCorry. 2012. The factor structure of the Revised Illness Perception Questionnaire in a population of oesophageal cancer survivors. Psychooncology 21: 524–30. [Google Scholar] [CrossRef] [PubMed]
- Fazeli, Zahra, Fs Fazeli Bavandpour, Ar Abdi, Ma Pour Hosaingholi, Ali Akbari, and Jafar Salimian. 2013. Trend analysis of breast cancer mortality in Iranian women. Journal of Ilam University of Medical Sciences 20: 246–51. [Google Scholar]
- Fischer, Maarten J, Marion E Wiesenhaan, Aukje Does-den Heijer, Wim C Kleijn, Johan W R Nortier, and Adrian A Kaptein. 2013. From despair to hope: A longitudinal study of illness perceptions and coping in a psycho-educational group intervention for women with breast cancer. British Journal of Health Psychology 18: 526–45. [Google Scholar] [CrossRef]
- Ghahari, Shahrbanoo, Rahele Fallah, Mohammad Mazloumi Rad, Nazanin Farrokhi, Jafar Bolhari, Mehdi Mousavi, Zahra Razzaghi, and Mohammad Esmaeel Akbari. 2017. Effect of cognitive-behavioral therapy and spiritual-religious intervention on improving coping responses and quality of life among women with breast cancer in Tehran. Bali Medical Journal 6: 409–14. [Google Scholar] [CrossRef]
- Groarke, AnnMarie, Ruth Curtis, and Michael Kerin. 2013. Cognitive-behavioural stress management enhances adjustment in women with breast cancer. British Journal of Health Psychology 18: 623–41. [Google Scholar] [CrossRef]
- Haaga, David A. F., Windy Dryden, and Christine P. Dancey. 1991. Measurement of rational-emotive therapy in outcome studies. Journal of Rational-Motive and CognitiveBehavior Therapy 9: 73–93. [Google Scholar] [CrossRef]
- Haddadi Kuhsar, Ali Akbar, Alireza Moradi, Bagher Ghobari Bonab, and Farnad Imani. 2017. Comparing the effectiveness of spiritual therapy based on Iranian culture with a cognitive-behavioral approach with a mindfulness approach based on reducing stress in reducing depression, anxiety, and stress in patients with chronic pain. Clinical Psychology Studies 8: 1–30. [Google Scholar]
- Hajabadi, Negar Ranjbar, Roya Ebrahimi, Sakine Farhadi, Hojjati Hamid, and Mahboubeh Tabrsa. 2020. The relationship between frequency of prayer and death anxiety in cancer patients. Indian Journal of Forensic Medicine & Toxicology 14: 2163–67. [Google Scholar]
- Hakami Shalamzai, Kowsar, Negar Asghari Pour, Jamshid Jamali, Ali Taghizadeh Kermani, and Raheleh Babazadeh. 2022. The effect of sexual counseling based on BETTER and PLISSIT model on quality of sexual life in women with breast cancer after mastectomy. Journal of Midwifery and Reproductive Health 10: 3490–98. [Google Scholar]
- Hannoun-Levi, Jean Michel. 2005. Traitement du cancer du sein et de l’utérus: Impact physiologique et psychologique sur la fonction sexuelle [Treatment of breast and uterus cancer: Physiological and psychological impact on sexual function]. Cancer Radiotherapie: Journal de la Societe Francaise de Radiotherapie Oncologique 9: 175–82. [Google Scholar] [CrossRef] [PubMed]
- Henderson, Phyllis D., Shirley V. Gore, Bertha Lane Davis, and Esther H. Condon. 2003. African American women coping with breast cancer: A qualitative analysis. Oncology Nursing Forum 30: 641–47. [Google Scholar] [CrossRef] [PubMed]
- Hill, Peter C., Kenneth II Pargament, Ralph W. Hood, Jr., Michael E. McCullough, James P. Swyers, David B. Larson, and Brian J. Zinnbauer. 2000. Conceptualizing religion and spirituality: Points of commonality, points of departure. Journal for the Theory of Social Behaviour 30: 51. [Google Scholar] [CrossRef]
- Holzner, Bernhard, Georg Kemmler, Martin Kopp, Roland Moschen, Hansjo Rd Schweigkofler, Martina Du Nser, Raimund Margreiter, Wolfgang W. Fleischhacker, and Barbara Sperner-Unterweger. 2001. Quality of life in breast cancer patients-not enough attention for long-term survivors? Psychosomatics 42: 117–23. [Google Scholar] [CrossRef] [PubMed]
- Hormes, Julia M., Leslie A. Lytle, Cynthia R. Gross, Rehana L. Ahmed, Andrea B. Troxel, and Kathryn H. Schmitz. 2008. The Body Image and Relationships Scale: Development and validation of a measure of body image in female breast cancer survivors. Journal of Clinical Oncology 26: 1269–74. [Google Scholar] [CrossRef] [PubMed]
- Horne, David, and Maggie Watson. 2011. Cognitive-behavioural therapies in cancer care. In Handbook of Psychotherapy in Cancer Care. Edited by Maggie Watson and David W. Kissane. Hoboken: John Wiley & Sons, Inc., pp. 15–26. [Google Scholar]
- Jafari, Najmeh, Ahmadreza Zamani, Ziba Farajzadegan, Fatemeh Bahrami, Hamid Emami, and Amir Loghmani. 2013. The effect of spiritual therapy for improving the quality of life of women with breast cancer: A randomized controlled trial. Psychology, Health & Medicine 18: 56–69. [Google Scholar]
- Karataş, Tuğba, Şükrü Özen, and Sevinç Kutlutürkan. 2017. Factor structure and psychometric properties of the Brief Illness Perception Questionnaire in Turkish cancer patients. Asia-Pacific Journal of Oncology Nursing 4: 77. [Google Scholar] [CrossRef]
- Karekla, Maria, and Marios Constantinou. 2010. Religious coping and cancer: Proposing an acceptance and commitment therapy approach. Cognitive and Behavioral Practice 17: 371–81. [Google Scholar] [CrossRef]
- Koenig, Harold G. 2008. Medicine, Religion, and Health: Where Science and Spirituality Meet. West Conshohocken: Templeton Foundation Press. [Google Scholar]
- Koenig, Harold G., and Arndt Büssing. 2010. The Duke University Religion Index (DUREL): A five-item measure for use in epidemiological studies. Religions 1: 78–85. [Google Scholar] [CrossRef]
- Koenig, Harold G., and David B. Larson. 2001. Religion and mental health: Evidence for an association. International Review of Psychiatry 13: 67–78. [Google Scholar] [CrossRef]
- Krok, Dariusz, Ewa Telka, and Beata Zarzycka. 2019. Illness perception and affective symptoms in gastrointestinal cancer patients: A moderated mediation analysis of meaning in life and coping. Psychooncology 28: 1728–34. [Google Scholar] [CrossRef] [PubMed]
- Larson, David B., and Susan S. Larson. 2003. Spirituality’s potential relevance to physical and emotional health: A brief review of quantitative research. Journal of Psychology and Theology 31: 37–51. [Google Scholar] [CrossRef]
- Memaryan, Nadereh, Zeinab Ghaempanah, Mir Majid Saeedi, Aidin Aryankhesal, Nafiseh Ansarinejad, and Ruohollah Seddigh. 2017. Content of spiritual counseling for cancer patients undergoing chemotherapy in Iran: A qualitative content analysis. Asian Pacific Journal of Cancer Prevention 18: 1791. [Google Scholar]
- Mete, Birgül, and Kerime Derya Beydağ. 2021. Mastektomi sonrası meme rekonstrüksiyonu yapılan kadınlarda benlik saygısı ve sosyal görünüş kaygısı ilişkisi [Relationship between self-esteem and social appearance anxiety in women who had breast reconstruction after mastectomy]. Sağlık ve Toplum 31: 159–71. [Google Scholar]
- Molavi, Amene, Khadije Hekmat, Poorandokht Afshari, and Mohammad Hoseini. 2015. Evaluation of couples’ sexual function and satisfaction after mastectomy. The Iranian Journal of Obstetrics, Gynecology and Infertility 17: 17–24. [Google Scholar] [CrossRef]
- Moss-Morris, Rona, John Weinman, Keith Petrie, Robert Horne, Linda Cameron, and Deanna Buick. 2002. The Revised Illness Perception Questionnaire (IPQ-R). Psychology & Health 17: 1–16. [Google Scholar]
- Nasution, Lina Anisa, and Yati Afiyanti. 2021. Spiritual based intervention effect on the psychological aspect of patients with gynecologic and breast cancer: A systematic review. Enfermería Clínica 31: S90–S95. [Google Scholar] [CrossRef]
- Nehir, Sevgi, Nurgül Güngör Tavşanli, Çiğdem Özdemir, and Tuğba Akyol. 2019. A determination of hopelessness and the perception of illness in cancer. Omega (Westport) 79: 115–31. [Google Scholar] [CrossRef] [PubMed]
- Nolen-Hoeksema, Susan, and Jannay Morrow. 1991. A prospective study of depression and posttraumatic stresssymptoms after a natural disaster: The 1989 Loma Prieta earthquake. Journal of Personality and Social Psychology 61: 115–21. [Google Scholar] [CrossRef]
- Onen Sertoz, Ozen, Hayriye Elbi Mete, Ayşin Noyan, Mehmet Alper, and Murat Kapkaç. 2004. Effects of surgery type on body image, sexuality, self-esteem, and marital adjustment in breast cancer: A controlled study. Turk Psikiyatri Dergisi 15: 264–75. [Google Scholar]
- Park, Jay J H, Grace Hsu, Ellie G Siden, Kristian Thorlund, and Edward J Mills. 2020. An overview of precision oncology basket and umbrella trials for clinicians. CA: A Cancer Journal for Clinicians 70: 125–37. [Google Scholar] [CrossRef]
- Pearce, Michelle J., Harold G. Koenig, Clive J. Robins, Bruce Nelson, Sally F. Shaw, Harvey J. Cohen, and Michael B. King. 2015. Religiously integrated cognitive behavioral therapy: A new method of treatment for major depression in patients with chronic medical illness. Psychotherapy 52: 56–66. [Google Scholar] [CrossRef]
- Pecor, Melissa J. 2004. The Impact of Breast Cancer and Body Image in Ethnically Diverse Women. Unpublished. Doctoral dissertation, Auburn University, Auburn, AL, USA. [Google Scholar]
- Pirnia, Bijan, Nasrin Homayounfar, Nasim Hosseini, Farshid Ebrahimi, Zahra Haj Sadeghi, and Parastoo Malekanmehr. 2020. The predictive role of body image and sexual function in the quality of life after modified radical mastectomy regarding the mediating role of emotion: A cross-sectional study. International Journal of Cancer Management 13: e101371. [Google Scholar] [CrossRef]
- Renna, Megan E., M. Rosie Shrout, Annelise A. Madison, Maryam Lustberg, Stephen P. Povoski, Doreen M. Agnese, Raquel E. Reinbolt, Robert Wesolowski, Nicole O. Williams, Bhuvaneswari Ramaswamy, and et al. 2021. Worry and rumination in breast cancer patients: Perseveration worsens self-rated health. Journal of Behavioral Medicine 44: 253–59. [Google Scholar] [CrossRef]
- Renshaw, Domeena C. 1994. Beacons, breasts, symbols, sex, and cancer. Theoretical Medicine 15: 349–60. [Google Scholar] [CrossRef] [PubMed]
- Sajadi, Mahbobeh, Naimeh Niazi, Sharareh Khosravi, Abolghasem Yaghobi, Mahboubeh Rezaei, and Harold G. Koenig. 2018. Effect of spiritual counseling on spiritual well-being in Iranian women with cancer: A randomized clinical trial. Complementary Therapies in Clinical Practice 30: 79–84. [Google Scholar] [CrossRef]
- Saritas, Seyhan Citlik, and Aysel Özdemir. 2018. Identification of the correlation between illness perception and anxiety level in cancer patients. Perspectives in Psychiatric Care 54: 380–85. [Google Scholar] [CrossRef]
- Schoenberg, Bruce. 1979. Sex after mastectomy: Counseling husband and wife. Medical Aspects of Human Sexuality 13: 88–103. [Google Scholar]
- Sharifi, Mehdi, Sakineh Saeidi, Harold G. Koenig, Mahboubeh Dadfar, and Yahya Turan. 2023. The effect of integrated religious cognitive behavioral therapy (ICBT) on psychological symptoms in women with breast cancer. Mankind Quarterly 63: 617–35. [Google Scholar] [CrossRef]
- Sheydaei Aghdam, Shovan, Farah LotfiKashani, Shahram Vaziri, and Khajevand Khoshli. 2019. Comparison of the effectiveness of integrative psychotherapy, spiritual therapy, and cognitive-behavioral therapy on sexual dysfunction in patients with breast cancer. Thoughts and Behavior in Clinical Psychology 14: 103–11. [Google Scholar]
- Spilka, Bernard, and Daniel N. McIntosh. 1996. Religion and Spirituality: The Known and the Unknown. Toronto: American Psychological Association. [Google Scholar]
- Tahergorabi, Zoya, Mitra Moodi, and Behzad Mesbahzadeh. 2014. Breast cancer: A preventable disease. Journal of Birjand University of Medical Sciences 21: 126–41. [Google Scholar]
- Tanhaye Reshvanloo, Farhad, Marzie Torkamani, Sara Mirshahi, Nafiseh Hajibakloo, and Hossein Kareshki. 2021. Validation and reliability of Persian version of Co-Rumination Questionnaire. Journal of Clinical Psychology 13: 79–87. [Google Scholar] [CrossRef]
- Torabi, Faeze, Maryam Rassouli, Manighea Nourian, Nasrin Borumandnia, Azam Shirinabadi Farahani, and Fatemeh Nikseresht. 2018. The effect of spiritual care on adolescents coping with cancer. Holistic Nursing Practice 32: 149–59. [Google Scholar] [CrossRef] [PubMed]
- Vatvani, Akhil Deepak, Catherine Gunawan, Kalis Waren, and Andree Kurniawan. 2017. Association between illness perception and health-related quality of life in Indonesian cancer patients. Annals of Oncology 28: x163. [Google Scholar] [CrossRef]
- Yapıcı, Asım. 2007. Ruh sağlığı ve din [Mental Health and Religion]. Adana: Karahan Kitabevi [Karahan Bookstore]. [Google Scholar]
- Zinnbauer, Brian J., Kenneth I. Pargament, Brenda Cole, Mark S. Rye, Eric M. Butfer, Timothy G. Belavich, Kathleen Hipp, Allie B. Scott, and Jill L. Kadar. 1997. Religion and spirituality: Unfuzzying the fuzzy. Journal for the Scientific Study of Religion 36: 549–64. [Google Scholar] [CrossRef]
| Session | Goals |
|---|---|
| 1st Session |
|
| 2nd Session |
|
| 3rd Session |
|
| 4th Session |
|
| 5th Session |
|
| 6th Session |
|
| 7th Session |
|
| 8th Session |
|
| Variables | Control (n = 31) | Experiment (n = 32) | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Marital status | Married | 21 | 67.8 | 24 | 75.0 |
| single | 10 | 32.2 | 8 | 25.0 | |
| Education | Elementary school | 8 | 25.8 | 5 | 15.6 |
| High School | 11 | 35.5 | 12 | 37.5 | |
| BA | 8 | 25.8 | 10 | 31.3 | |
| MA and above | 4 | 12.9 | 5 | 15.6 | |
| Work status | Full-time | 9 | 29.0 | 7 | 21.9 |
| Part-time | 5 | 16.2 | 6 | 18.8 | |
| Unemployed | 17 | 54.8 | 19 | 59.3 | |
| Level of income | Good | 11 | 35.5 | 8 | 25.0 |
| Medium | 15 | 48.3 | 20 | 62.5 | |
| Bad | 5 | 16.2 | 4 | 12.5 | |
| Having children | Yes | 16 | 51.6 | 18 | 56.3 |
| No | 15 | 48.4 | 14 | 43.7 | |
| Treatment time | 6 months–2 years | 7 | 22.6 | 9 | 28.1 |
| 3–5 years | 24 | 77.4 | 23 | 71.9 | |
| Groups | Experiment | Control | Follow-Up | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Pre-Test | Post-Test | Pre-Test | Post-Test | |||||||
| Variables | M | SD | M | SD | M | SD | M | SD | M | SD |
| Body Image | 52.3 | 7.28 | 56.78 | 5.10 | 50.64 | 5.40 | 51.10 | 4.83 | 56.78 | 5.10 |
| Sexual Function | 35.40 | 11.3 | 38.01 | 9.21 | 36.11 | 8.78 | 37.01 | 9.10 | 34.58 | 12.90 |
| Illness Perception | 44.28 | 3.73 | 56.7 | 2.10 | 45.3 | 1.32 | 46.9 | 1.08 | 55.7 | 2.17 |
| Intrusive Thoughts | 61.25 | 9.18 | 48.09 | 6.34 | 59.90 | 5.80 | 60.39 | 4.58 | 44.61 | 8.27 |
| Effect | Test | Value | Hypoth. DF | Error. df | F | Sig | |
|---|---|---|---|---|---|---|---|
| Between-Group | Group | Wilks’ lambda | 0.66 | 8 | 21 | 3.67 | 0.001 |
| Time | Wilks’ lambda | 0.29 | 16 | 93 | 9.36 | 0.001 | |
| Intragroup | Interaction of time and group | Wilks’ lambda | 0.13 | 16 | 93 | 8.78 | 0.001 |
| Source | Variable | Stage | Sum of the Squares | df | The Mean of the Squares | F | Sig | The Effect Size |
|---|---|---|---|---|---|---|---|---|
| Time | Body image | Pre-test–Post-test | 341.11 | 1 | 341.11 | 22.24 | 0.00 | 0.48 |
| Post-test–follow-up | 0.63 | 1 | 0.63 | 2.71 | 0.07 | 0.17 | ||
| Sexual Function | Pre-test–Post-test | 501.2 | 1 | 501.2 | 38.65 | 1.00 | 0.11 | |
| Post-test–follow-up | 0.002 | 1 | 0.002 | 0.00 | 0.52 | 0.13 | ||
| Illness Perception | Pre-test–Post-test | 353.11 | 1 | 353.11 | 30.21 | 0.00 | 0.44 | |
| Post-test–follow-up | 0.58 | 1 | 0.58 | 2.72 | 0.00 | 0.64 | ||
| Intrusive Thoughts | Pre-test–Post-test | 67.23 | 1 | 67.23 | 3.19 | 0.04 | 0.33 | |
| Post-test–follow-up | 13.22 | 1 | 13.22 | 0.01 | 0.00 | 0.19 |
| Source | Variable | Stage | Sum of the Squares | df | The Mean of the Squares | F | Sig | The Effect Size |
|---|---|---|---|---|---|---|---|---|
| Interaction of time and group | Body image | Pre-test–Post-test | 528.00 | 1 | 528.00 | 30.11 | 0.00 | 0.51 |
| Post-test–follow-up | 15.13 | 1 | 15.13 | 10.43 | 0.08 | 0.19 | ||
| Sexual Function | Pre-test–Post-test | 203.24 | 1 | 203.24 | 25.31 | 0.78 | 0.19 | |
| Post-test–follow-up | 0.78 | 1 | 0.78 | 12.09 | 1.00 | 0.23 | ||
| Illness Perception | Pre-test–Post-test | 312.56 | 1 | 312.56 | 31.09 | 0.00 | 0.56 | |
| Post-test–follow-up | 0.18 | 1 | 0.18 | 6.70 | 0.00 | 0.23 | ||
| Intrusive Thoughts | Pre-test–Post-test | 61.76 | 1 | 61.76 | 4.13 | 0.00 | 0.19 | |
| Post-test–follow-up | 17.65 | 1 | 17.65 | 1.09 | 0.01 | 0.13 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharifi, M.; Koenig, H.G.; Dadfar, M.; Turan, Y.; Ghorbani, A. The Effectiveness of Spirituality-Centered Cognitive Therapy on Body Image, Sexual Function, Illness Perception and Intrusive Thoughts in Iranian Women after Mastectomy. Religions 2024, 15, 578. https://doi.org/10.3390/rel15050578
Sharifi M, Koenig HG, Dadfar M, Turan Y, Ghorbani A. The Effectiveness of Spirituality-Centered Cognitive Therapy on Body Image, Sexual Function, Illness Perception and Intrusive Thoughts in Iranian Women after Mastectomy. Religions. 2024; 15(5):578. https://doi.org/10.3390/rel15050578
Chicago/Turabian StyleSharifi, Mehdi, Harold G. Koenig, Mahboubeh Dadfar, Yahya Turan, and Alireza Ghorbani. 2024. "The Effectiveness of Spirituality-Centered Cognitive Therapy on Body Image, Sexual Function, Illness Perception and Intrusive Thoughts in Iranian Women after Mastectomy" Religions 15, no. 5: 578. https://doi.org/10.3390/rel15050578
APA StyleSharifi, M., Koenig, H. G., Dadfar, M., Turan, Y., & Ghorbani, A. (2024). The Effectiveness of Spirituality-Centered Cognitive Therapy on Body Image, Sexual Function, Illness Perception and Intrusive Thoughts in Iranian Women after Mastectomy. Religions, 15(5), 578. https://doi.org/10.3390/rel15050578







