Translation and Validation of the Dutch Version of the Spiritual Care Competence Questionnaire (SCCQ-NL)
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants’ Selection
2.3. Measures
2.3.1. Spiritual Care Competence Questionnaire
2.3.2. Additional Variables
2.3.3. Translation
2.3.4. Extra Care for Meaning Competence Items
2.4. Statistical Analyses
3. Results
3.1. Demographics
3.2. Factor Analysis
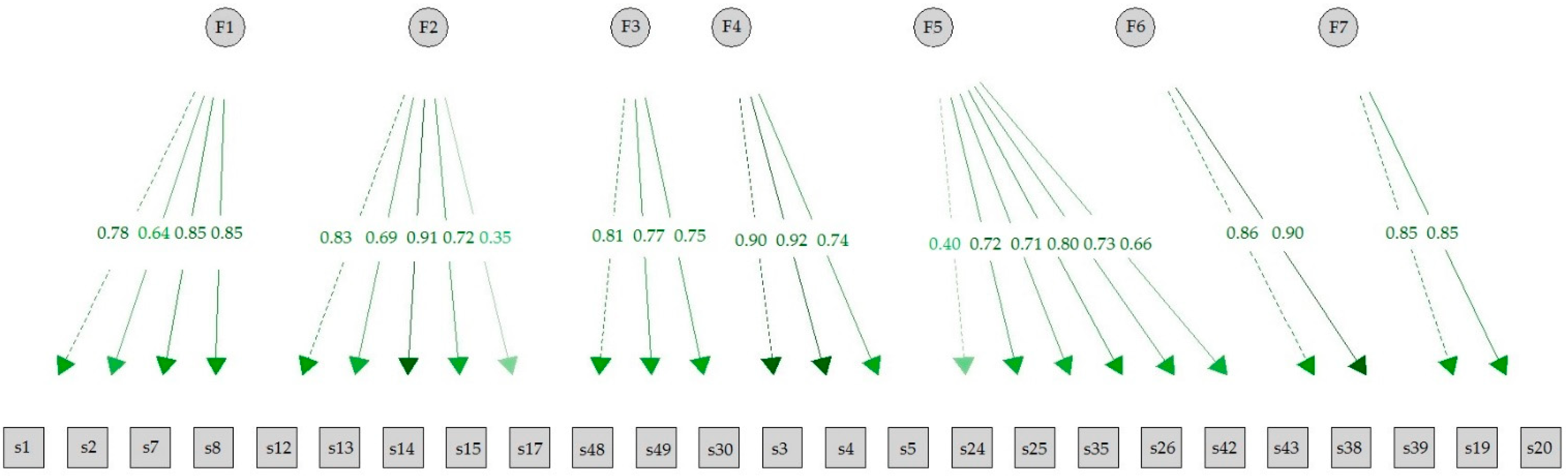
3.2.1. Exploratory Factor Analysis
3.2.2. Confirmatory Factor Analysis
3.3. Distribution of the SCCQ-NL Scores in the Sample
3.4. Hindrances
3.5. Correlation of the SCCQ-NL Factors with Other Variables
3.5.1. Extra Care for Meaning Competence Items
3.5.2. Work-Related Variables
4. Discussion
4.1. Strengths and Limitations
4.2. Recommendations for Further Research
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- AKWA GGZ. 2023. Nieuwe Kwaliteitsstandaard Zingeving in de Psychische Hulpverlening. Available online: https://akwaggz.nl/nieuwe-kwaliteitsstandaard-zingeving-in-de-psychische-hulpverlening (accessed on 15 May 2023).
- Alimujiang, Aliya, Ashley Wiensch, Jonathan Boss, Nancy L. Fleisher, Alison M. Mondul, Karen McLean, Bhramar Mukherjee, and Celeste L. Pearce. 2019. Association between life purpose and mortality among US adults older than 50 Years. JAMA Network Open 2: e194270. [Google Scholar] [CrossRef] [PubMed]
- Bar-Sela, Gill, Michael J. Schultz, Karima Elshamy, Maryam Rassouli, Eran Ben-Arye, Myrna Doumit, Nahla Gafer, Alaa Albashayreh, Ibtasim Ghrayeb, Ibrahim Turker, and et al. 2019. Training for awareness of one’s own spirituality: A key factor in overcoming barriers to the provision of spiritual care to advanced cancer patients by doctors and nurses. Palliat Support Care 17: 345–52. [Google Scholar] [CrossRef] [PubMed]
- Bartlett, Maurice Stevenson. 1954. A Note on the Multiplying Factors for various Chi Square Approximations. Journal of the Royal Statistical Society 16: 296–98. [Google Scholar]
- Bartoli, Eleonora. 2007. Religious and spiritual issues in psychotherapy practice: Training the trainer. Psychotherapy 44: 54–65. [Google Scholar] [CrossRef] [PubMed]
- Bell, Simon. 2011. Art Therapy and Spirituality. Journal for the Study of Spirituality 1: 215–30. [Google Scholar] [CrossRef]
- Best, Megan, Phyllis Butow, and Ian Olver. 2015. Do patients want doctors to talk about spirituality? A systematic literature review. Patient Education and Counseling 98: 1320–28. [Google Scholar] [CrossRef] [PubMed]
- Blom, Herman. 2019. Netherlands-Duitse Culturele Vergelijking als Opstap naar Zelfreflexie. In Rijnland in de Regio. Leeuwarden: Stenden Hogeschool, pp. 97–115. [Google Scholar]
- Bouwhuis-van Keulen, Annette J., Jurrijn Koelen, Liesbeth Eurelings-Bontekoe, Christien Hoekstra-Oomen, and Gerrit Glas. 2023. The evaluation of religious and spirituality-based therapy compared to standard treatment in mental health care: A multi-level meta-analysis of randomized controlled trials. Psychotherapy Research 34: 339–52. [Google Scholar] [CrossRef] [PubMed]
- Brewer-Smyth, Kathleen, and Harold G. Koenig. 2014. Could spirituality and religion promote stress resilience in survivors of childhood trauma? Issues in Mental Health Nursing 35: 251–56. [Google Scholar] [CrossRef]
- Büssing, Arndt, Andreas Michalsen, Hans-Joachim Balzat, Ralf-Achim Grünther, Thomas Ostermann, Edmund A.M. Neugebauer, and Peter F. Matthiessen. 2009. Are spirituality and religiosity resources for patients with chronic pain conditions? Pain Medicine 10: 327–39. [Google Scholar] [CrossRef]
- CBS. 2020. Religie in Nederland. Available online: https://www.cbs.nl/nl-nl/longread/statistische-trends/2020/religie-in-nederland (accessed on 23 March 2023).
- Chen, Ying, and Tyler J. VanderWeele. 2018. Associations of Religious Upbringing with Subsequent Health and Well-Being From Adolescence to Young Adulthood: An Outcome-Wide Analysis. American Journal of Epidemiology 187: 2355–64. [Google Scholar] [CrossRef]
- Clark, Michelle, and Amanda Emerson. 2021. Spirituality in Psychiatric Nursing: A Concept Analysis. Journal of the American Psychiatric Nurses Association 27: 22–32. [Google Scholar] [CrossRef]
- Cohen, Jacob W. 1988. Statistical Power Analysis for the Behavioral Science, 2nd ed. Hillsdale: Lawrence Erlbaum Associates. [Google Scholar]
- Currier, Joseph M., Laura T. Stevens, Stephen L. Isaak, Tracey Smith, and Kimberly Zlomke. 2020. Understanding Preferences for Addressing Spirituality Among Adults Seeking Outpatient Mental Health Care. The Journal of Nervous and Mental Disease 208: 514–16. [Google Scholar] [CrossRef]
- De Brito Sena, Marina Aline, Rodolfo Furlan Damiano, Giancarlo Lucchetti, and Mario Ferando Prieto Peres. 2021. Defining Spirituality in Healthcare: A Systematic Review and Conceptual Framework. Frontiers in Psychology 12: 756080. [Google Scholar] [CrossRef]
- De Bruijn, Line. 2020. Eigenlijk is Mijn Hele Vak daar Gewoon voor. Een Empirische Studie naar Motivatie van Professionals in de Ambulante GGZ om al dan niet Aandacht te Geven aan Spiritualiteit/Zingeving in hun Zorg. Master’s thesis, University of Humanistic Studies, Utrecht, The Netherlands. [Google Scholar]
- De Diego-Cordero, Rocío, Ángeles C. López-Tarrida, Carmen Linero-Narváez, and José María Galan González-Cerna. 2023. More Spiritual Health Professionals Provide Different Care: A Qualitative Study in the Field of Mental Health. Healthcare 11: 303. [Google Scholar] [CrossRef] [PubMed]
- Doherty, Meredith, Lynden Bond, Lauren Jessel, Julie Tennille, and Victoria Stanhope. 2020. Transitioning to Person-Centered Care: A Qualitative Study of Provider Perspectives. Journal of Behavioral Health Services and Research 47: 399–408. [Google Scholar] [CrossRef] [PubMed]
- Edwards, Adrian Gwyn, N. Pang, V. Shiu, and Cecilia Chan. 2010. The understanding of spirituality and the potential role of spiritual care in end-of-life and palliative care: A meta-study of qualitative research. Palliative Medicine 24: 753–70. [Google Scholar] [CrossRef]
- El Hajjar, Said T. 2018. Statistical Analysis: Internal-Consistency, Reliability and Construct validity. International Journal of Quantitative and Qualitative Research Methods 6: 46–57. [Google Scholar]
- Frick, Eckhard. 2017. Spiritual Care—How does it work? Spiritual Care 6: 223–24. [Google Scholar] [CrossRef]
- Frick, Eckhard, and Andreas Schiessl. 2015. Resilienz im ärztlichen Berufsalltag fördern. Zeitschrift für Medizinische Ethik 61: 47–55. [Google Scholar]
- Frick, Eckhard, Mayla Theiss, Daniela Rodrigues Recchia, and Arndt Büssing. 2019. Validierung einer deutschsprachigen Spiritual Care-Kompetenz-Skala: Validation of a spiritual care competence scale in German language. Spiritual Care 8: 193–207. [Google Scholar] [CrossRef]
- Fuchs, Joseph R., Jeffrey W. Fuchs, Joshua M. Hauser, and Marilyn E. Coors. 2021. Patient desire for spiritual assessment is unmet in urban and rural primary care settings. BMC Health Services Research 21: 289. [Google Scholar] [CrossRef] [PubMed]
- Gladding, Samuel T., and Jamie E. Crockett. 2019. Religious and Spiritual Issues in Counseling and Therapy: Overcoming Clinical Barriers. Journal of Spirituality in Mental Health 21: 152–61. [Google Scholar] [CrossRef]
- Glas, Gerrit. 2014. Beyond Professionalism—Once More. Psyche en Geloof 25: 23–30. [Google Scholar]
- Glas, Gerrit. 2017. On the Existential Core of Professionalism in Mental Health Care. Mental Health, Religion & Culture 20: 536–43. [Google Scholar] [CrossRef]
- Glas, Gerrit. 2020. De Behandelaar Zelf. Utrecht: Lemion. [Google Scholar]
- Green, Alexis, Yeoun Soo Kim-Godwin, and Carolyn W. Jones. 2020. Perceptions of Spiritual Care Education, Competence, and Barriers in Providing Spiritual Care Among Registered Nurses. Journal of Holistic Nursing 38: 41–51. [Google Scholar] [CrossRef] [PubMed]
- Greenfield, Emily A., George E. Vaillant, and Nadine F. Marks. 2009. Do Formal Religious Participation and Spiritual Perceptions Have Independent Linkages with Diverse Dimensions of Psychological Well-Being? Journal of Health and Social Behavior 50: 196–212. [Google Scholar] [CrossRef]
- Hengeveld-Sloëtjes, Janneke, Gerrit Glas, Henri Sellies, and Jooske Van Busschbach. 2020. Existentiële Thema’s in de Behandelrelatie. Een Kwalitatief Onderzoek naar de Betekenis van Existentiële Thema’s in de Behandelrelatie (Existential themes in treatment relationships: A qualitative investigation into the role of existential themes in treatment relationships). Psyche en Geloof 31: 51–64. [Google Scholar]
- Hoenders, H.J. Rogier, and Arjan W. Braam. 2020. De Rol van Zingeving in de Psychiatrie: Belangrijk, maar nog Onduidelijk (The Role of Spirituality in Psychiatry: Important but still Unclear). Tijdschrift Voor Psychiatrie 62: 955–59. [Google Scholar]
- Huber, Machteld, and Bert Garssen. 2016. Relaties tussen Zingeving, Gezondheid en Welbevinden. In De Mens Centraal. ZonMw-Signalement over Zingeving in Zorg. Den Haag: ZonMw, pp. 16–23. [Google Scholar]
- Hvidt, Niels C., Kristina Tomra Nielsen, Alex K. Kørup, Christina Prinds, Dorte Gilså Hansen, Dorte Toudal Viftrup, Elisabeth Assing Hvidt, Elisabeth Rokkjær Hammer, Erik Falkø, Flemming Locher, and et al. 2020. What is spiritual care? Professional perspectives on the concept of spiritual care identified through group concept mapping. BMJ Open 10: e042142. [Google Scholar] [CrossRef]
- Kaiser, Henry F. 1970. A Second Generation Little Jiffy. Psychometrika 35: 401–15. [Google Scholar] [CrossRef]
- Kaiser, Henry F. 1974. An Index of Factorial Simplicity. Psychometrika 39: 31–36. [Google Scholar] [CrossRef]
- Koenig, Harold G. 2012. Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry 16: 278730. [Google Scholar] [CrossRef] [PubMed]
- Koenig, Harold G., Faten Al-Zaben, and Tyler J. VanderWeele. 2020. Religion and Psychiatry: Recent Developments in Research. BJPsych Advances 26: 262–72. [Google Scholar] [CrossRef]
- Lansink, Bibejan. 2020. Betekenisverlening in de Psychiatrie. Maak Ruimte voor de Zeggingskracht en Functie van een Psychose. De Psychiater. Available online: https://depsychiater.nl/artikelen/2020/juli/editie-5/maak-ruimte-voor-de-zeggingskracht-en-de-functie-van-een-psychose (accessed on 1 September 2023).
- Laranjeira, Carlos, and Ana Querido. 2023. An in-depth introduction to arts-based spiritual healthcare: Creatively seeking and expressing purpose and meaning. Frontiers in Psychology 14: 1132584. [Google Scholar] [CrossRef]
- Liefbroer, Anke I., Erik Olsman, Ruard R. Ganzevoort, and Faridi S. Van Etten-Jamaludin. 2017. Interfaith Spiritual Care: A Systematic Review. Journal of Religion and Health 56: 1776–93. [Google Scholar] [CrossRef]
- Magaldi, Danielle, and Leora Trub. 2018. (What) do You Believe? Therapist Spiritual/Religious/Non-religious Self-disclosure. Psychotherapy Research 28: 484–98. [Google Scholar] [CrossRef] [PubMed]
- Magaldi-Dopman, Danielle, Jennie Park-Taylor, and Joseph G. Ponterotto. 2011. Psychotherapists’ Spiritual, Religious, Atheist or Agnostic Identity and their Practice of Psychotherapy: A Grounded Theory Study. Psychotherapy Research 21: 286–303. [Google Scholar] [CrossRef]
- Mandelkow, Lars, Eckhard Frick, Arndt Büssing, and Silje Endresen Reme. 2022. Norwegian Psychotherapy: Religiosity Gap and Spiritual Care Competence. Journal of Spirituality in Mental Health 24: 359–80. [Google Scholar] [CrossRef]
- Matise, Miles, Jeffery Ratcliff, and Flavia Mosci. 2017. A Working Model for the Integration of Spirituality in Counseling. Journal of Spirituality in Mental Health 20: 27–50. [Google Scholar] [CrossRef]
- Mohr, Sylvia, and Philippe Huguelet. 2014. The wishes of outpatients with severe mental disorders to discuss spiritual and religious issues in their psychiatric care. Internation Journal of Psychiatry in Clinical Practice 18: 304–7. [Google Scholar] [CrossRef] [PubMed]
- Moreira-Almeida, Alexander, Avdesh Sharma, Bernard Janse van Rensburg, Peter J. Verhagen, and Christopher C.H. Cook. 2016. WPA Position Statement on Spirituality and Religion in Psychiatry. World Psychiatry 15: 87–88. [Google Scholar] [CrossRef] [PubMed]
- Mächler, Ruth, Cornelia Straßner, Noemi Sturm, Johannes Krisam, Regina Stolz, Friederike Schalhorn, Jan Valentini, and Eckhard Frick. 2022. GP’s Personal Spirituality, Their Attitude and Spiritual Competence: A Cross-Sectional Study in German General Practices. Journal of Religion and Health 62: 2436–51. [Google Scholar] [CrossRef] [PubMed]
- Neves Oliviera, Alda. 2019. Spiritual Care—Compétences (Auto-Évalués) Auprès D’infirmièr·e·s aux Cliniques Universitaires Saint-Luc. In Validation Française du Questionnaire «Spiritual Care Competencies Questionnaire». Leuven: Faculté de Santé Publique, Université Catholique de Louvain. [Google Scholar]
- Oxhandler, Holly K., James W. Ellor, and Matthew S. Stanford. 2018. Client Attitudes toward Integrating Religion and Spirituality in Mental Health Treatment: Scale Development and Client Responses. Social Work 63: 337–46. [Google Scholar] [CrossRef] [PubMed]
- Paal, Piret, Yousef Helo, and Eckhard Frick. 2015. Spiritual Care Training Provided to Healthcare Professionals: A Systematic Review. Journal of Pastoral Care & Counseling 69: 19–30. [Google Scholar] [CrossRef]
- Pallant, Julie. 2020. SPSS Survival Manual, a Step by Step Guide to Data Analysis Using IBM SPSS. London: Routledge. [Google Scholar]
- Pastrana, Tania, Eckhard Frick, Alicia Krikorian, Leticia Ascencio, Florencia Galeazzi, and Arndt Büssing. 2021. Translation and Validation of the Spanish Version of the Spiritual Care Competence Questionnaire (SCCQ). Journal of Religion and Health 60: 3621–39. [Google Scholar] [CrossRef] [PubMed]
- Paul Victor, Chitra G., and Judith V. Treschuk. 2020. Critical Literature Review on the Definition Clarity of the Concept of Faith, Religion, and Spirituality. Journal of Holistic Nursing 38: 107–13. [Google Scholar] [CrossRef] [PubMed]
- Pew Research Center. 2012. Available online: https://www.pewresearch.org/religion/2012/12/18/global-religious-landscape-exec (accessed on 25 September 2023).
- Puchalski, Christina, Betty Ferrell, Rose Virani, Shirley Otis-Green, Pamela Baird, Janet Bull, Harvey Chochinov, George Handzo, Holly Nelson-Becker, Maryjo Prince-Paul, and et al. 2009. Improving the Quality of Spiritual Care as a Dimension of Palliative Care: The Report of the Consensus Conference. Journal of Palliative Medicine 12: 885–904. [Google Scholar] [CrossRef] [PubMed]
- Rosmarin, David H., Brent P. Forester, Daniel M. Shassian, Christian A. Webb, and Thröstur Björgvinsson. 2015. Interest in spiritually integrated psychotherapy among acute psychiatric patients. Journal of Consulting and Clinical Psychology 83: 1149–53. [Google Scholar] [CrossRef] [PubMed]
- Ross, Linda, and Wilfred McSherry. 2020. Spiritual Care Charting/Documenting/Recording/Assessment: A Perspective from the United Kingdom. In Charting Spiritual Care: The Emerging Role of Chaplaincy Records in Global Health Care. Edited by Simon Peng-Keller and David Neuhold. Cham: Springer, pp. 97–113. [Google Scholar]
- Rosseel, Yves. 2012. Lavaan: An R Package for Structural Equation Modeling. Journal of Statistical Software 48: 1–36. [Google Scholar] [CrossRef]
- Schep-Akkerman, Annemieke, and René Van Leeuwen. 2009. Spirituele Zorg: Vanzelfsprekend maar Niet Vanzelf (Spiritual Care: Obvious, but Not Natural). Tijdschrift voor Verpleegkundigen 119: 34–39. [Google Scholar]
- Schmeets, Hans, and Marieke Houben. 2023. Religieuze Betrokkenheid in Nederland. Available online: https://www.cbs.nl/nl-nl/longread/statistische-trends/2023/religieuze-betrokkenheid-in-nederland (accessed on 30 September 2023).
- Shimizu, Hiroko, Eckhard Frick, Arndt Büssing, Hoshina Uehara, Akihito Tsuji, and Keiko Matsumoto. 2023. Validation of the Japanese Version of the Spiritual Care Competence Questionnaire. International Journal of Nursing and Health Care Research 6: 1383. [Google Scholar] [CrossRef]
- Stauner, Nick, Julie Exline, and Kenneth Pargament. 2016. Religious and Spiritual Struggles as Concerns for Health and Well-Being. Horizonte 14: 48–75. [Google Scholar] [CrossRef]
- Stevens, James P. 1992. Applied Multivariate Statistics for the Social Sciences, 2nd ed. Hillsdale: Erlbaum. [Google Scholar]
- Stroppa, Andre, Fernando A. Colugnati, Harold G. Koenig, and Alexander Moreira-Almeida. 2018. Religiosity, Depression, and Quality of Life in Bipolar Disorder: A Two-year Prospective Study. Brazilian Journal of Psychiatry 40: 238–43. [Google Scholar] [CrossRef] [PubMed]
- Tavares, Ana Patrícia, Helga Martins, Sara Pinto, Sílvia Caldeira, Patrícia Pontífice Sousa, and Beth Rodgers. 2022. Spiritual Comfort, Spiritual Support and Spiritual Care: A Simultaneous Concept Analysis. Nursing Forum 57: 1559–66. [Google Scholar] [CrossRef]
- Trevino, Kelly M., Aanand D. Naik, and Jennifer Moye. 2016. Perceived and Actual Change in Religion/Spirituality in Cancer Survivors: Longitudinal Relationships with Distress and Perceived Growth. Psychology of Religion and Spirituality 8: 195–205. [Google Scholar] [CrossRef]
- Trochim, William M. K. 2006. Convergent and Discriminant Validity. Research Methods: Knowledge Base. Available online: http://www.socialresearchmethods.net/kb/convdisc.php (accessed on 1 July 2023).
- Van de Loo, Dominique T.M., Nina Saämena, Pauline Janse, Marja van Vliet, and Arjan W. Braam. 2022. De Waardering van de Zes Dimensies van Positieve Gezondheid in de Ggz (The Six Dimensions of Positive Health valued by Different Stakeholders within Mental Health Care). Tijdschrift voor Psychiatrie 64: 87–93. [Google Scholar] [PubMed]
- Van den Bent, Johan, Dominique Van de Loo, and Arjan W. Braam. 2022. Bekwaamheid van Behandelaren in de GGZ ten aanzien van Zingeving. Unpublished. [Google Scholar]
- Van Kleef, Niels, Laura Griffin, Nina Van Lier, and Anne Levah Russchen. 2023. Handreiking LHBTI+ Emancipatie, 10 Vragen over Non-Binaire Personen. Available online: https://www.movisie.nl/sites/movisie.nl/files/2023-03/handreiking-lhbti%2B-10-vragen-non-binair.pdf (accessed on 20 April 2023).
- Van Leeuwen, René, Lucas J. Tiesenga, Berrie Middel, Doeke Post, and Henk Jochemsen. 2009. The validity and reliability of an instrument to assess nursing competencies in spiritual care. Journal of Clinical Nursing 18: 2857–69. [Google Scholar] [CrossRef] [PubMed]
- Van Nieuw Amerongen-Meeuwse, Joke C., Hanneke Schaap-Jonker, Carmen Schuhmann, Christa Anbeek, and Arjan W. Braam. 2018. The “Religiosity Gap” in a Clinical Setting: Experiences of Mental Health Care Consumers and Professionals. Mental Health, Religion and Culture 21: 737–52. [Google Scholar] [CrossRef]
- Van Nieuw Amerongen-Meeuwse, Joke C., Hanneke Schaap-Jonker, Christina Hennipman-Herweijer, Christa Anbeek, and Arjan W. Braam. 2019. Patients’ Needs of Religion/Spirituality Integration in Two Mental Health Clinics in the Netherlands. Issues in Mental Health Nursing 40: 41–9. [Google Scholar] [CrossRef]
- Van Nieuw Amerongen-Meeuwse, Joke C., Hanneke Schaap-Jonker, Gerlise Westerbroek, Christa Anbeek, and Arjan W. Braam. 2020. Conversations and Beyond. Religious/Spiritual Care Needs Among Clinical Mental Health Patients in the Netherlands. The Journal of Nervous and Mental Disease 208: 524–32. [Google Scholar] [CrossRef]
- Verhagen, Piet. 2012. Hoofdstuk 40. Religieuze of Zingevingsanamnese in het Opleidingscurriculum. In Handboek Psychiatrie, Religie en Spiritualiteit. Utrecht: De Tijdstroom Uitgeverij, pp. 515–26. [Google Scholar]
- Vieten, Cassandra, and Shelley Scammell. 2015. Spiritual and Religious Competencies in Clinical Practice: Guidelines for Psychotherapists and Mental Health Professionals. Oakland: New Harbinger Publications. [Google Scholar]
- Villas Boas, Alex, Mary Rute Gomes Esperandio, Sílvia Caldeira, and Fabiano Incerti. 2023. From Selfcare to Taking Care of Our Common Home: Spirituality as an Integral and Transformative Healthy Lifestyle. Religions 14: 1168. [Google Scholar] [CrossRef]
- Watkins, Marley W. 2005. Determining Parallel Analysis Criteria. Journal of Modern Applied Statistical Methods 5: 344–6. [Google Scholar] [CrossRef]
- Woodhead, Linda, Christopher Patridge, and Hiroko Kawanami. 2016. Religions in the Modern World. Traditions and Transformations, 3rd ed. Oxon and New York: Routledge. [Google Scholar]
- Worthington, Everett L., Jr. 1989. Religious faith across the life span: Implications for counseling and research. The Counseling Psychologist 17: 555–612. [Google Scholar] [CrossRef]
| Lentis (N = 338) | Altrecht (N = 392) | Total (N = 730) | |
|---|---|---|---|
| Variable | %/mean ± SD | %/mean ± SD | %/mean ± SD |
| Gender (%) 1 | |||
| Women | 76.0 | 69.6 | 72.6 |
| Men | 23.4 | 30.1 | 27.0 |
| Other | 0.3 | 0.3 | 0.3 |
| Prefer not to answer | 0.3 | - | 0.1 |
| Mean age (years) | 44.6 ± 12.2 | 44.6 ± 12.4 | 44.6 ± 12.3 |
| Marital status (%) | |||
| Married | 45.0 | 45.4 | 45.2 |
| Unmarried, living together | 29.0 | 29.3 | 29.2 |
| Divorced | 7.4 | 5.6 | 6.4 |
| Single | 13.3 | 15.8 | 14.7 |
| Widowed | 0.6 | - | 0.3 |
| Other | 4.7 | 3.8 | 4.2 |
| Work experience (years) | 18.0 ± 11.9 | 16.8 ± 12.0 | 17.3 ± 12.0 |
| Weekly working time (hours) | 30.3 ± 5.4 | 31.0 ± 5.5 | 30.1 ± 5.5 |
| Profession (%) | |||
| Physician | 5.0 | 15.3 | 10.5 |
| Nurse | 47.6 | 32.1 | 39.3 |
| Psychologist | 23.4 | 29.8 | 26.8 |
| Therapist (i.e., creative or psychomotor) | 3.6 | 5.4 | 4.5 |
| Other | 20.4 | 17.4 | 18.9 |
| Discipline (%) | |||
| Internal medicine | 0.3 | - | 0.1 |
| Geriatrics | 1.8 | 0.3 | 1.0 |
| Psychiatry/psychotherapy | 94.7 | 96.2 | 95.5 |
| Other | 3.3 | 3.6 | 3.4 |
| Job satisfaction (1–5) | 4.1 ± 0.6 | 4.2 ± 0.6 | 4.2 ± 0.6 |
| Religious affiliation (%) | |||
| Christianity | 21.9 | 24.7 | 23.4 |
| Judaism | 0 | 0.3 | 0.1 |
| Islam | 0.6 | 1.3 | 1.0 |
| Hinduism | 0.3 | 0.5 | 0.4 |
| Buddhism | 0.6 | 1.5 | 1.1 |
| Other | 12.7 | 11.2 | 12.1 |
| None | 63.9 | 60.5 | 62.1 |
| Believing person (%) | |||
| Not at all/rather not | 73.4 | 75.0 | 74.2 |
| Yes, somewhat/yes, indeed | 26.6 | 25.0 | 25.8 |
| Praying and/or meditating (%) | |||
| No, not at all/rarely | 50.9 | 53.6 | 52.3 |
| Sometimes/yes, regularly | 49.1 | 46.4 | 47.7 |
| Mean [0–3] | Corrected Item-Scale Correlation | Cronbach’s α if Item Deleted | Factor Loading | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | ||||
| Factor 1. Perception of spiritual needs (eigenvalue 6.7, Cronbach’s alpha = 0.810) 1 | ||||||||||
| 1. I am confident I can perceive the spiritual needs of patients | 2.02 ± 0.60 | 0.636 | 0.764 | 0.697 | ||||||
| 2. I am confident I can perceive the spiritual needs of patients’ relatives | 1.96 ± 0.66 | 0.589 | 0.780 | 0.664 | ||||||
| 7. I am able to perceive existential/spiritual needs even if patients have little relation to religion | 1.69 ± 0.77 | 0.665 | 0.744 | 0.594 | ||||||
| 8. I can also talk with nonreligious patients about their existential/spiritual needs | 1.88 ± 0.80 | 0.643 | 0.757 | 0.536 | ||||||
| Factor 2. Team spirit (eigenvalue 2.2, Cronbach’s alpha = 0.753) | ||||||||||
| 14. In the team, we exchange regularly about spirituality in patient support | 0.93 ± 0.71 | 0.687 | 0.654 | 0.806 | ||||||
| 12. In our team, we speak regularly about patient’s spiritual needs | 0.90 ± 0.74 | 0.630 | 0.671 | 0.733 | ||||||
| 13. In our institution there is a great openness to the topic of spirituality | 1.40 ± 0.73 | 0.531 | 0.706 | 0.733 | ||||||
| 15. In the team, we regularly exchange about our own spirituality | 0.92 ± 0.75 | 0.515 | 0.711 | 0.655 | ||||||
| 17. In the team, we have rituals (for example farewell and interruption rituals) to deal with problematic situations | 1.10 ± 0.97 | 0.324 | 0.801 | 0.500 | ||||||
| Factor 3. Spiritual self-awareness (eigenvalue 1.9, Cronbach’s alpha = 0.756) | ||||||||||
| 48. I regularly take care of deepening my own spirituality | 1.23 ± 1.12 | 0.685 | 0.552 | −0.862 | ||||||
| 49. I regularly attend professional development sessions on spiritual topics | 0.53 ± 0.88 | 0.570 | 0.700 | −0.786 | ||||||
| 30. My own spirituality shapes my dealings with others/sick people | 1.50 ± 1.01 | 0.527 | 0.740 | −0.711 | ||||||
| Factor 4. Documentation competencies (eigenvalue 1.5, Cronbach’s alpha = 0.644) | ||||||||||
| 3. I am familiar with instruments (e.g., FICA, HOPE, ELMO) for creating a short spiritual history | 0.14 ± 0.43 | 0.563 | 0.485 | 0.855 | ||||||
| 4. I am familiar with instruments/questionnaires for structurally assessing spiritual needs | 0.17 ± 0.47 | 0.559 | 0.463 | 0.842 | ||||||
| 5. I know how to document the spiritual history of my patients in a comprehensible way | 0.75 ± 0.83 | 0.407 | 0.797 | 0.597 | ||||||
| Factor 5. Empowerment and proactive opening competencies (eigenvalue 1.5, Cronbach’s alpha = 0.731) | ||||||||||
| 25. In the case of therapeutic decisions, I pay attention to religious/spiritual attitudes and convictions of the individual patient | 1.99 ± 0.77 | 0.518 | 0.681 | 0.713 | ||||||
| 35. I pay attention to the appropriate framework for spiritual conversations | 1.21 ± 0.87 | 0.536 | 0.673 | 0.635 | ||||||
| 26. I encourage my patients to reflect their spiritual beliefs and attitudes | 1.74 ± 0.80 | 0.531 | 0.676 | 0.597 | ||||||
| 24. I enable my patients to participate in religious activities/celebrations | 1.85 ± 1.08 | 0.322 | 0.751 | 0.518 | ||||||
| 42. I regularly approach patients to talk with them about their spiritual needs | 1.09 ± 0.77 | 0.478 | 0.692 | 0.429 | ||||||
| 43. I open verbally, but also nonverbally, a “space” in which the patient may bring spiritual concerns—but is not forced to do so | 1.73 ± 0.84 | 0.478 | 0.690 | 0.406 | ||||||
| Factor 6. Knowledge about other religions (eigenvalue 1.1, Cronbach’s alpha = 0.744) | ||||||||||
| 38. I am well aware of the religious characteristics of patients from other religious communities | 1.73 ± 0.66 | 0.592 | NA | 0.850 | ||||||
| 39. I take care that the religious characteristics of patients from other religious communities are adequately considered | 1.88 ± 0.66 | 0.592 | NA | 0.840 | ||||||
| Factor 7. Conversation competencies (eigenvalue 1.0, Cronbach’s alpha = 0.735) | ||||||||||
| 19. I am able to conduct an open discussion on existential issues | 2.46 ± 0.60 | 0.572 | 0.361 | 0.826 | ||||||
| 20. I am able to conduct an open discussion on religious issues | 2.43 ± 0.59 | 0.513 | 0.455 | 0.796 | ||||||
| Deleted item | ||||||||||
| 28. I am able to tolerate the pain/suffering of patients and their relatives | 2.55 ± 0.53 | 0.292 | 0.735 | |||||||
| Perception | Team Spirit | Spiritual Self- Awareness | Documentation | Empowerment | Knowledge Religions | Conversation | Hindrance Items | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 44. Knowledge | 45. Responsible | 46. Time | 47. Space | |||||||||
| All (N = 730) | Mean | 2.07 | 1.03 | 1.14 | 0.34 | 1.61 | 1.80 | 2.42 | 1.40 | 1.06 | 0.92 | 0.62 |
| SD | 0.49 | 0.56 | 0.80 | 0.45 | 0.57 | 0.63 | 0.55 | 0.89 | 0.85 | 0.82 | 0.81 | |
| Institution | ||||||||||||
| MHI 1 (N = 338) | Mean | 1.87 | 0.97 | 1.17 | 0.31 | 1.57 | 1.69 | 2.44 | 1.46 | 0.99 | 0.86 | 0.65 |
| SD | 0.56 | 0.57 | 0.83 | 0.43 | 0.61 | 0.64 | 0.53 | 0.88 | 0.83 | 0.81 | 0.86 | |
| MHI 2 (N= 392) | Mean | 1.92 | 1.08 | 1.12 | 0.36 | 1.65 | 1.898 | 2.51 | 1.35 | 1.11 | 0.97 | 0.59 |
| SD | 0.58 | 0.54 | 0.79 | 0.46 | 0.54 | 0.60 | 0.59 | 0.90 | 0.86 | 0.83 | 0.78 | |
| F value | 0.01 | 3.89 | 0.84 | 0.89 | 5.89 | 7.61 | 1.59 | 0.52 | 4.599 | 0.41 | 3.39 | |
| p-value | n.s. | 0.007 | n.s. | n.s. | n.s. | <0.001 | n.s. | n.s. | n.s. | n.s. | n.s. | |
| Age | ||||||||||||
| 21–37 (N = 249) | Mean | 1.71 | 0.91 | 0.92 | 0.28 | 1.48 | 1.69 | 2.43 | 1.55 | 1.20 | 0.99 | 0.59 |
| SD | 0.55 | 0.49 | 0.73 | 0.36 | 0.53 | 0.61 | 0.53 | 0.87 | 0.84 | 0.83 | 0.799 | |
| 38–52 (N = 248) | Mean | 1.89 | 1.07 | 1.17 | 0.36 | 1.66 | 1.82 | 2.39 | 1.36 | 0.97 | 0.87 | 0.58 |
| SD | 0.56 | 0.57 | 0.78 | 0.47 | 0.58 | 0.59 | 0.55 | 0.89 | 0.799 | 0.82 | 0.79 | |
| >53 (N = 233) | Mean | 2.09 | 1.10 | 1.36 | 0.37 | 1.699 | 1.91 | 2.46 | 1.27 | 1.00 | 0.89 | 0.69 |
| SD | 0.54 | 0.595 | 0.84 | 0.498 | 0.58 | 0.67 | 0.56 | 0.89 | 0.89 | 0.82 | 0.85 | |
| F value | 28.7 | 8.6 | 19.3 | 3.61 a | 10.98 | 7.4 | 0.77 | 10.25 | 7.598 | 2.16 | 1.77 | |
| p-value | <0.001 | <0.001 | <0.001 | 0.03 | <0.001 | <0.001 | n.s. | 0.001 | 0.005 | n.s. | n.s. | |
| Profession | ||||||||||||
| Physician/psychiatrist (N = 77) | Mean | 1.94 | 1.14 | 1.14 | 0.394 | 1.60 | 1.79 | 2.42 | 1.16 | 1.09 | 1.14 | 0.43 |
| SD | 0.51 | 0.54 | 0.76 | 0.52 | 0.51 | 0.65 | 0.51 | 0.92 | 0.85 | 0.87 | 0.72 | |
| Nurse (N = 287) | Mean | 1.94 | 1.05 | 1.17 | 0.36 | 1.68 | 1.85 | 2.38 | 1.40 | 0.89 | 0.86 | 0.77 |
| SD | 0.55 | 0.54 | 0.79 | 0.49 | 0.55 | 0.60 | 0.57 | 0.91 | 0.81 | 0.82 | 0.85 | |
| Psychologist (N = 196) | Mean | 1.72 | 0.91 | 0.94 | 0.31 | 1.53 | 1.69 | 2.45 | 1.55 | 1.22 | 0.98 | 0.47 |
| SD | 0.595 | 0.53 | 0.71 | 0.36 | 0.57 | 0.59 | 0.50 | 0.82 | 0.83 | 0.79 | 0.79 | |
| Therapist (creative/psychomotor) (N = 33) | Mean | 2.00 | 1.10 | 1.495 | 0.13 | 1.59 | 1.68 | 2.47 | 1.39 | 1.27 | 0.79 | 0.52 |
| SD | 0.55 | 0.52 | 0.71 | 0.24 | 0.42 | 0.54 | 0.499 | 0.86 | 0.91 | 0.78 | 0.71 | |
| Other (N = 137) | Mean | 2.01 | 1.06 | 1.299 | 0.35 | 1.61 | 1.90 | 2.49 | 1.30 | 1.09 | 0.85 | 0.66 |
| SD | 0.57 | 0.64 | 0.93 | 0.43 | 0.66 | 0.72 | 0.59 | 0.90 | 0.88 | 0.83 | 0.79 | |
| F value | 6.79 | 3.36 a | 7.00 a | 6.16 a | 2.05 a | 3.36 | 1.16 | 3.35 | 5.26 | 2.51 | 5.43 | |
| p-value | <0.001 | 0.01 | <0.001 | <0.001 | n.s. | 0.01 | n.s. | 0.01 | <0.001 | 0.04 | <0.001 | |
| “I am an (active) believing person” | ||||||||||||
| Believers (N = 188) | Mean | 2.11 | 1.08 | 1.82 | 0.37 | 1.72 | 1.93 | 2.56 | 0.96 | 0.77 | 0.83 | 0.69 |
| SD | 0.54 | 0.58 | 0.69 | 0.49 | 0.59 | 0.64 | 0.52 | 0.83 | 0.82 | 0.81 | 0.82 | |
| Non-believers (N = 542) | Mean | 1.82 | 1.01 | 0.91 | 0.33 | 1.57 | 1.76 | 2.38 | 1.55 | 1.15 | 0.95 | 0.59 |
| SD | 0.56 | 0.55 | 0.71 | 0.43 | 0.56 | 0.62 | 0.55 | 0.86 | 0.84 | 0.83 | 0.81 | |
| F value | 0.07 | 0.68 | 0.77 | 3.196 | 0.36 | 0.02 | 0.59 | 4.86 | 0.43 | 0.84 | 0.03 | |
| p-value | <0.001 | n.s. | <0.001 | n.s. | 0.002 | 0.002 | <0.001 | <0.001 | <0.001 | n.s. | n.s. | |
| “I pray or meditate” | ||||||||||||
| Practicing prayer/meditation (N = 348) | Mean | 2.02 | 1.05 | 1.67 | 0.37 | 1.696 | 1.85 | 2.51 | 1.20 | 0.93 | 0.91 | 0.68 |
| SD | 0.55 | 0.58 | 0.69 | 0.48 | 0.58 | 0.61 | 0.54 | 0.86 | 0.84 | 0.84 | 0.83 | |
| Not practicing prayer/meditation (N = 382) | Mean | 1.79 | 1.00 | 0.67 | 0.31 | 1.53 | 1.76 | 2.35 | 1.58 | 1.18 | 0.92 | 0.57 |
| SD | 0.57 | 0.54 | 0.58 | 0.41 | 0.55 | 0.64 | 0.55 | 0.88 | 0.84 | 0.80 | 0.79 | |
| F value | 1.05 | 2.52 | 5.896 | 3.32 | 0.02 | 1.07 | 1.46 | 0.58 | 0.41 | 4.56 | 1.57 | |
| p-value | <0.001 | n.s. | <0.001 | n.s. | <0.001 | n.s. | <0.001 | <0.001 | <0.001 | n.s. | n.s. | |
| 44. My Knowledge […] | 45. I Do Not Perceive Myself as […] | 46. I Do Not Have Time […] | 47. No Suitable Room […] | |
|---|---|---|---|---|
| 44. My knowledge about religion/spirituality is too poor to get involved in a competent manner | 1.000 | |||
| 45. I do not perceive myself as an appropriate person for religious/spiritual topics | 0.288 ** | 1.000 | ||
| 46. I do not have time for religious/spiritual topics | 0.226 ** | 0.277 ** | 1.000 | |
| 47. No suitable room is available for talking privately about religious/spiritual topics | 0.096 ** | 0.070 | 0.311 ** | 1.000 |
| Perception competencies | −0.488 ** | −0.268 ** | −0.195 ** | −0.012 |
| Team spirit | −0.205 ** | −0.146 ** | −0.121 ** | −0.023 |
| Spiritual self-awareness | −0.358 ** | −0.312 ** | −0.103 ** | 0.094 |
| Documentation competencies | −0.208 ** | −0.149 ** | −0.114 ** | −0.037 |
| Empowerment and proactive opening competencies | −0.390 ** | −0.302 ** | −0.163 ** | −0.010 |
| Knowledge about other religions | −0.340 ** | −0.178 ** | −0.129 ** | −0.033 |
| Conversation competencies | −0.346 ** | −0.165 ** | −0.202 ** | −0.107 ** |
| Perception | Team Spirit | Self- Awareness | Documentation | Empowerment | Knowledge Religions | Conversation | |
|---|---|---|---|---|---|---|---|
| Perception competencies | 1.000 | ||||||
| Team spirit | 0.332 *** | 1.000 | |||||
| Spiritual self-awareness | 0.383 *** | 0.184 *** | 1.000 | ||||
| Documentation competencies | 0.292 *** | 0.298 *** | 0.126 *** | 1.000 | |||
| Empowerment competencies | 0.524 *** | 0.423 *** | 0.335 *** | 0.344 *** | 1.000 | ||
| Knowledge about other religions | 0.357 *** | 0.233 *** | 0.167 *** | 0.157 *** | 0.461 *** | 1.000 | |
| Conversation competencies | 0.471 *** | 0.155 *** | 0.218 *** | 0.159 *** | 0.370 *** | 0.277 *** | 1.000 |
| Care for Meaning Competence (CMC) a | 0.527 *** | 0.221 *** | 0.179 *** | 0.218 *** | 0.472 *** | 0.473 *** | 0.458 *** |
| Working hours | 0.014 | 0.019 | −0.123 *** | 0.090 | 0.006 | 0.077 | 0.085 |
| Job satisfaction | 0.033 | 0.070 | −0.036 | 0.042 | 0.051 | 0.058 | 0.128 *** |
| Working years | 0.193 *** | 0.115 ** | 0.149 *** | 0.028 | 0.114 ** | 0.133 *** | −0.020 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schoot, M.; Bartels-Velthuis, A.A.; Rodrigues Recchia, D.; Frick, E.; Büssing, A.; Hoenders, R. Translation and Validation of the Dutch Version of the Spiritual Care Competence Questionnaire (SCCQ-NL). Religions 2024, 15, 496. https://doi.org/10.3390/rel15040496
Schoot M, Bartels-Velthuis AA, Rodrigues Recchia D, Frick E, Büssing A, Hoenders R. Translation and Validation of the Dutch Version of the Spiritual Care Competence Questionnaire (SCCQ-NL). Religions. 2024; 15(4):496. https://doi.org/10.3390/rel15040496
Chicago/Turabian StyleSchoot, Merel, Agna A. Bartels-Velthuis, Daniela Rodrigues Recchia, Eckhard Frick, Arndt Büssing, and Rogier Hoenders. 2024. "Translation and Validation of the Dutch Version of the Spiritual Care Competence Questionnaire (SCCQ-NL)" Religions 15, no. 4: 496. https://doi.org/10.3390/rel15040496
APA StyleSchoot, M., Bartels-Velthuis, A. A., Rodrigues Recchia, D., Frick, E., Büssing, A., & Hoenders, R. (2024). Translation and Validation of the Dutch Version of the Spiritual Care Competence Questionnaire (SCCQ-NL). Religions, 15(4), 496. https://doi.org/10.3390/rel15040496









