Abstract
From its inception palliative care has been understood as addressing four dimensions: physical, social, emotional/psychological, and spiritual/religious. However, the spiritual and/or religious element is poorly understood and under-researched, and little is known about palliative care professionals’ understandings of spiritual care, or how they seek to implement spiritual care in practice. Members of the European Association of Palliative Care (EAPC) Spiritual Care Taskforce (SCTF) designed and conducted a 28-item survey, supported by the EAPC Board, investigating palliative care professionals’ understandings and attempts to implement spiritual care. Following pilot-testing with 30 participants, the survey ran for a month. It was engaged with by 527 people from 67 countries and most regions of the world, with 502 answering at least two questions, 465 people answering at least one substantive questions, 228 providing examples of spiritual care at Q24, and 115 providing further comments at Q28. We analysed the sociodemographic data descriptively, thematically analysed the diverse, detailed spiritual care examples provided at Q24, and conducted a content analysis of Q28 responses. We identified nine themes from Q24 responses. Of these nine themes, five encompassed interactions between staff and patients, one of these five addressing the character, nature, or quality of care provided by staff; the other four specific content of that care: supporting patients’ wellbeing, supporting patients’ religious faiths, enabling reflection, and facilitating focused discussions. A sixth theme covered staff roles and responsibilities, including specific input from specialist providers. Three smaller themes addressed supporting others than patients: families before patients’ deaths, families during bereavement, and staff.
Keywords:
care; chaplain; palliative; pastoral; professional; spiritual; survey; religion; religious 1. Introduction
Palliative care is generally understood as addressing four aspects or dimensions of need: physical, social, emotional/psychological, and spiritual/religious (Saunders 1967, 1981; Mount 1976; WHO 2020). However, the spiritual and/or religious dimension of palliative care is not well understood and the least researched (Selman et al. 2014; Nissen et al. 2021), and little is known about palliative care professionals’ understandings of spiritual care, or how they seek to implement spiritual care guidelines in practice (Balboni et al. 2013; Best et al. 2016).
Small-scale research studies have explored the understandings of spiritual and/or religious care of palliative care and/or oncology patients (Grant et al. 2005; Schultz et al. 2018) or conducted qualitative research asking palliative care professionals about their understandings of spiritual care (Vivat 2008; Edwards et al. 2010; Koper et al. 2019), but these studies have mostly involved small numbers of participants within individual countries, and often in one or a few cities or localities within those countries. Systematic reviews have been conducted comparing findings between such studies (Edwards et al. 2010; Mesquita et al. 2017; Batstone et al. 2020).
Spiritual care is a complex and contested concept, and there is no single accepted, uncontested definition, although attempts have been made to produce consensual definitions of spiritual care, including by a Consensus Conference in California in 2009 (Puchalski et al. 2009), and by the Spiritual Care Task Force (SCTF) of the European Association of Palliative Care (EAPC) (Nolan et al. 2011), building on that earlier work in the USA, but developed in and for a European context.
Key elements of spiritual care that have been identified include attitudes from staff, including presence, awareness, love and compassion, respect, empathy (Edwards et al. 2010; Walker and Waterworth 2017; Taylor 2021; Morland et al. 2022), and specific actions, such as communicating and connecting, engaging in meaningful conversations, and willingness to act and accompany patients into the unknown (Vivat 2008; Minton et al. 2018; Batstone et al. 2020; Ghorbani et al. 2021), religious or divine-related provision and referrals, and death preparations (Walker and Waterworth 2017). Topics of relevance which are less frequently discussed or considered as spiritual care are whether this care is part of the role for all or requires specialisation, or whether it involves care for others than dying patients, whether families and informal carers before or after bereavement, or professional carers.
Three of the authors (BV, MTGBM, TY), in our roles as members of the EAPC SCTF, developed a survey to explore palliative care professionals’ provision and perceptions of spiritual care. The EAPC Board agreed we could use their SurveyMonkey (SurveyMonkey n.d.) account for this purpose.
This paper presents an overview of the sociodemographic characteristics of all respondents who answered some or all of the core substantive items, a thematic analysis of the examples of spiritual care provided where requested at item 24, and a content analysis of responses to the final item, 28 (any other comments).
2. Materials and Methods
We piloted an initial version of the survey with 30 participants and finalized a set of 28 items (Table 1). The first question asked where respondents had come across the survey, in order to establish how widely and by what means it had been distributed and accessed. The next ten questions (2–11) collected socio-demographic data. Substantive items began at Q12. We entered the items into SurveyMonkey and shared the link by direct email, with some social media outputs also, including LinkedIn and Twitter.

Table 1.
Survey items.
The survey was live for one month. After it closed, we checked and cleaned the response data, and then excluded data from respondents who had not answered any questions beyond the last sociodemographic question (Q11): How long have you worked in this or a similar field?
Questions 12–15 asked respondents whether they personally, or their organisation or service, provided spiritual care or something they considered to be the equivalent of spiritual care but called by a different name. Q16 asked respondents who had answered No to all four of these previous items to provide an explanation if they could, and then skip all following items and go directly to the end of the survey, Q28, which asked for any further comments.
Q17 asked respondents whether they or their organisations followed any local, national, or international spiritual care guidelines. Q18 asked whether any models, such as Dignity Therapy (Chochinov et al. 2005), or the Journey model (Ly et al. 2021), were used. Q19 asked for details.
We conducted a descriptive analysis of the sociodemographic data (questions 2–11), and of the responses to questions regarding spiritual care practices from question 12 onwards, including which, if any, models and/or guidelines respondents said they and/or their organisations followed.
Q24 asked respondents to provide specific examples or illustrations of spiritual care. We deliberately did not provide our own definition of spiritual care, since we were seeking to obtain respondents’ personal understandings, but did give three brief examples, covering three possible areas, drawing from the existing literature: providing a quiet space for reflection, discussing a patient’s religious concerns, enabling a patient to express their feelings about a family member (Table 1).
We analysed responses to Q24 thematically (Clarke and Braun 2021). Q28 asked for additional comments, particularly from those who had answered No to all of questions 12–15. We conducted a content analysis of Q28 responses.
We present all quotes from participants’ responses verbatim, other than some light editing to, for example, correct misspellings and punctuation, or insert missing letters or words (these insertions are indicated in italicised text and square brackets).
3. Results
A total of 527 people engaged with the survey, with numbers gradually reducing across the 28 items. After checking and cleaning the data, we found that 502 people had responded to at least one of its items; the other 26 had opened and looked at the survey, but not provided any responses. Of these 502 respondents, 37 answered only the sociodemographic questions, and did not respond to any of the substantive questions regarding spiritual care (item 12 onwards).
So, 465 people provided their sociodemographic data in response to questions 2–11, and also responded to at least one of the substantive items. We found no significant differences between the 465 respondents who answered at least one substantive question and the 37 who answered only the sociodemographic questions for age, sex, country/place of work, occupation, or for having (or not having) religious beliefs or following spiritual practices.
We agreed to define this set of 465 people who answered at least one of the core substantive items of the survey as the core dataset for this study. This paper focuses on this group, presenting an overview first of their sociodemographic characteristics, and then of their responses to the substantive questions.
All 465 answered questions 12–15 on the provision of spiritual care, 406 answered questions 17–18, on whether any guidelines or models were followed, and 228 responded to item 24, providing examples of their understandings of spiritual care. The last question, 28, asked if respondents had any other comments. This, as well as being an opportunity for any respondent to provide further comments if they wished to do so, was also a skip item to which those who had answered no to all of questions 12–15 were directed.
3.1. Characteristics of Respondents in the Core Dataset
Most respondents (162; 35%) were aged 46–55, and, in all age categories other than the oldest (66 or older), most were women (Figure 1). Over two-thirds of respondents (310/465; 67%) said yes in response to Q4 asking whether they had a religion or followed any personal spiritual practices. Less than a third (133; 29%) said no, and a small number (22; 4%) indicated that they preferred not to say (Figure 2).
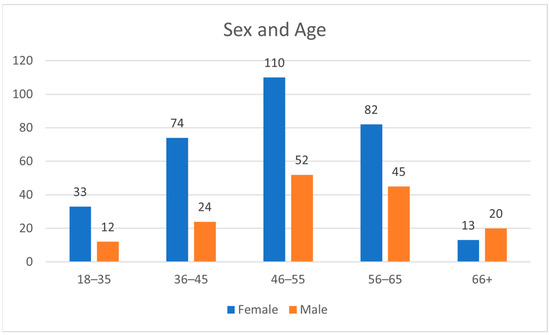
Figure 1.
Numbers of respondents in age bands and by sex (Q2 and Q3).
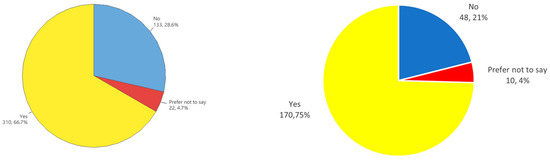
Figure 2.
Religion or personal spiritual practices (Q4); whole group (465) (Left) + subset (228) (Right).
We grouped responses to Q6 and Q7, about country of birth and country of work, by regions (Table 2). Respondents were from 67 countries, which we grouped into 11 regions. Most (42%) had been born in Northern Europe, with the second largest group (19%) born in Southern Europe. Most respondents (385/465; 83%) were working in their birth regions, and mostly the countries of work identified by respondents varied only slightly from their countries of birth. The exception to this was for respondents from Africa, where less than 50% of respondents were working in either their country or region of birth. However, only 13 respondents had been born in Africa, so no significance can be assigned to this finding.

Table 2.
Regions of birth and work (Q6 and Q7).
Over half the respondents (52.1%) were physicians, with the largest single group of these (37.9%) being specifically palliative care physicians (Table 3). The second largest group was nurses (23.5%). For those who stated that they were other physicians, the largest group was oncologists, with 11 identifying as such and another two as psycho-oncologists. Some respondents stated that they had more than one professional role, some physicians identifying other specialties, but most selected researcher as their other role (Table 4).

Table 3.
Respondents’ primary professional roles (Q9).

Table 4.
Additional roles identified (Q9 drop-down options).
Item 10 offered a free-text option for responses from those whose roles were not included in the drop-down options. These additional responses came from 159 respondents, with the largest group (39) being specialists in other clinical roles. Of the others, 20 were trainers, teachers or educators, 14 leaders or developers and/or coordinators or managers of services, and 9 were involved in developing policy and/or advocating for palliative care (Table 5).

Table 5.
Other occupations Q10 (free text responses).
Most respondents (275; 59%) had been working in palliative care for more than ten years. About a third of respondents had been in their current positions for either over ten years (155; 33%) or 1–5 years (156; 34%), with a few (43; 9%) having been in their current positions for over 20 years (Figure 3).
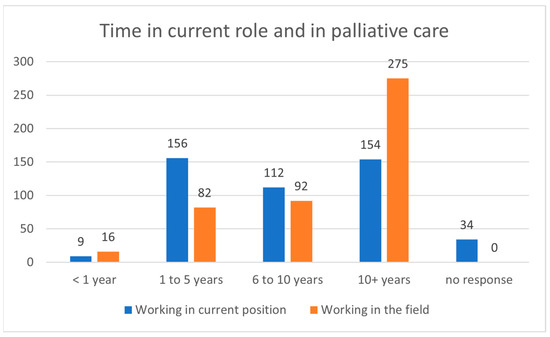
Figure 3.
Time in current role/time in palliative care (Q10 & Q11).
3.2. Spiritual Care Services, Providers, Guidelines, and Models
Survey questions 12 and 13 asked respondents whether they personally provided services or interventions which were called “spiritual care”, or services or interventions which they considered to be so, although under a different name. Questions 14 and 15 were equivalent queries about respondents’ organisations, rather than the respondents themselves.
Overall, 354 (76%) of the set of 465 respondents indicated in their responses to questions 12 and 13 that they personally provided either spiritual care or something equivalent under a different name (or no name) (Table 6).

Table 6.
Responses to questions 12–15 and 24.
Of all 465 respondents, 134, the largest subset (29%), answered Yes to all four of questions 12–15, indicating that both they and their organisation provided both spiritual care and something equivalent with another name. Conversely, 36 respondents (8% of the whole group; 10% of the 354 who said that they personally provided spiritual care or its equivalent) said that they did so, but that their organisation did not.
The other 111 of the 465 respondents (24%) answered No to both questions 12 and 13, indicating that they personally did not provide spiritual care or anything equivalent. Of these, 72 (65%) indicated in their responses to 14 and 15 that, while they personally did not provide either spiritual care or something equivalent with another name, they perceived that their organisation did so. The other 39 respondents answered No to all four questions, 12–15; 17 of these provided reasons in response to Q16, and 11 further comments at Q28.
Q17 asked whether respondents and/or their organisations followed any local, national, or international spiritual care guidelines, and Q18 asked: “Do you and/or your organisation/service/team follow any recognised model for spiritual care or interventions related to spiritual care (e.g., Dignity therapy, the Journey Model)?” In all, 406 respondents indicated that guidelines and/or models were used, and 124 provided further details at Q19.
We found no consensus across these responses, and no single set of guidelines or models was common to all respondents. The approach most frequently identified was Dignity Therapy (Chochinov et al. 2005), named by 30 of the 124 respondents. Fifteen of these stated Dignity Therapy alone; the other half that they used this approach alongside other models, or as a basis for other, local interventions. For example, one of the longer such responses stated:
We use chaplaincy & guidelines and features of Dignity and Meaning based therapy and resources […], bereavement support standards for specialist palliative care services, evidence-based strategies and resources for family carer support […], psychosocial and bereavement support for family caregivers of palliative care patients. Recommendations for health professionals for responding to desire to die statements from patients with advanced disease. Guidelines for the assessment of bereavement risk in family members of people receiving palliative care.(Respondent 98)
Nine respondents identified the ars moriendi model (Leget 2007), four the Journey model (Ly et al. 2021), four FICA (Puchalski and Romer 2000) and one GWish (George Washington institute for spiritual health, founded and directed by Christina Puchalski), three HOPE (Anandarajah and Hight 2001), one SECPAL (Benito et al. 2014), and one the Murata theory (Murata and Morita 2006). Six respondents stated that meaning-based therapy was used, and four person-centred or patient-centred or meaning-centred care. Eight referred to chaplaincy services, with one referencing holy communion.
As indicated above, some respondents, including those identifying specific models, said that they and/or their organisations used multiple models. In all, 26 gave answers to this effect, some lengthy, as above, while one commented simply:
Mixed, since needs are different.(Respondent 111)
One respondent, from Aotearoa/New Zealand, referred to the importance of including indigenous beliefs and perspectives:
I think both of these models [Dignity Therapy and the Journey model] were used in the design of our resource, and within the philosophical framework, although we have also brought in an indigenous perspective in honour of the Treaty of Waitangi, our bi-cultural commitment to working with Maori patients and family/whanau. (Respondent 211).[Note: whanau is a Maori word meaning an extended family or community of related families who live in the same area].
3.3. Meaning and Examples of Spiritual Care
Item 24 asked for examples of spiritual care, and 228 of the 465 respondents (49%) provided these, responding independently of whether they had said that they and/or their organisation provided any kind of spiritual care. The majority (81; 73%) of the subset of 111 respondents who had said that they personally did not provide spiritual care or anything equivalent did not provide any examples of spiritual care. However, 30 (27%) of this subset did, including four of the group of 39 who had answered No to all the questions 12–15.
We looked for any patterns in respondents’ sociodemographic characteristics which might differentiate any of these subsets from any of the others but found no obvious differences. The most noteworthy difference between the sociodemographic characteristics of this subset of 228 and the wider group of 465 was in their answers to Q4 on personal religion or spiritual practices, with 170 of this group answering Yes, a larger percentage than the whole group (75% vs. 66.7%), and 48 answering No, a smaller percentage than the whole group (21% vs. 28.6% of the whole group) (Figure 2). The group of 228 who provided examples at Q24 were also slightly more experienced than the whole group, with 63% (144/228) stating that they had ten or more years’ experience, vs. 59% (275/465) of the whole group.
In our thematic analysis, we identified nine themes, each with between one and four subthemes (Table 7).

Table 7.
Themes and sub-themes for responses to Q24.
We identified five main themes. The first of these, arising from a preponderance of responses, identified spiritual care as attitudes towards patients: attending, non-judgmental, active, non-directive listening, and concepts such as “being with” or “being there”, and “presence”. The other four main themes involved active interventions: promoting wellbeing, supporting religious patients, facilitating focused discussions on thoughts, feelings, and relationships, and discussions specifically on death and dying and the end-of-life, including advanced care and funeral planning. A sixth, slightly less frequent, theme addressed staff roles, including the roles and involvement of the multi-disciplinary team, staff training, and specialist input. Three smaller themes addressed support for families and other loved ones, before bereavement, and afterwards, and support for staff.
Overall, it was rare for one single theme to entirely encompass any one respondent’s answer. A few respondents wrote only a few words or a single sentence, but most provided lengthy, rich responses, with elements of these belonging in more than one category, sub-theme, or theme in the analysis. One example of these lengthy answers (which encompasses all the themes other than support for staff) stated:
[…] listening with patients, families, to concerns, offering active reflection, listening to life review, discussion of family concerns, life issues, illness journey, connections made by illness of self or family, regret, symptoms. Sitting with people in pain, distress, dying. Future and funeral planning; with patient and/or family. Discussions of faith and theology, discussion of how faith has changed, meeting ritual and sacramental needs (communion, anointing), prayer, referral to Priest/pastor etc. of another faith. Providing icons, candles, material for connection—written (poetry, Bible, books), pictures; providing items of nature (shells, sand, stones) to touch, maintaining the chapel for multi faith use. Blessing rooms post death with staff. Occupational therapist: Memory boxes put together with occupational therapist; creation of clay thumb prints of a parent for children; making silk scarves, cards for loved ones. Remembrance services for family post bereavement.(Respondent 217)
3.3.1. Theme 1: Attention/Person-/Patient-Centred/Led
This theme comprised four subthemes: being with or presence, accompaniment, person-centred care and non-judgemental acceptance, active listening or attention or mindfulness. The core of this theme is the understanding that spiritual care entails following the patient’s lead, being mindful and paying active attention; being with or presence, as an action, not something passive, and being available and enabling patients to express their thoughts and feelings, rather than in any way guiding or directing. As noted, many respondents gave lengthy responses, and some of the quotes we provide here span the subthemes of this theme, and also include remarks which fit other themes.
Being with/Presence
[…] just being quiet with people.(Respondent 126)
Just be with someone, with my whole presence, and in that realizing that there is so much more in the other person than “cancer” and allowing this other side to be there too, and laugh … or cry or nothing much, and in that way give space to talk and be seen as who they really are. Expressing my own feelings/concerns sometimes opens a space.(Respondent 176)
Accompaniment
Patients have questions. The aim is to help them find their own answers. Many people have religion but put it on ‘hold’ years ago. Religious doubters want reassurance. Some seek spirituality outside religion. Guidance which reassures can be valuable. They are alone on their personal journey but not alone.(Respondent 1)
Person-/Patient-Centred/-Led, Including Acceptance and Being Non-Judgmental
We follow a person-centred model, so the care we give is about being with the person, and be responsive to his/her needs, without being judgemental. That might include allowing that person to talk about whatever feelings and concerns might arise (family, health care, present, past and future …), supporting in the following of his/her projects and plans, adjusting to realistic goals, providing moments of wellbeing through whatever means are suitable, like going for a walk, listening to music, massage, remembering life story, and in a general way trying to respond, either through own means or referring to a qualified person to whatever concerns have arisen.(Respondent 8)
Active Listening/Attending/Mindfulness
Using a holistic needs assessment to assess concerns. Using active listening and following patient cues, using empathy etc. to provide support. ‘Being with’. Providing comforting touch, e.g., a hug to show acceptance and person to person connection.(Respondent 41)
3.3.2. Theme 2: Wellbeing: Activities and Spaces
This theme comprised two sub-themes: wellbeing and wellbeing activities and providing quiet and/or safe spaces. Responses in this theme conceptualised spiritual care as involving more direct actions, aiming to enable and facilitate patients in improving their wellbeing, and addressing related needs.
Enabling Wellbeing
This subtheme identified spiritual care as relating to a person’s wellbeing, and involving seeking to provide moments of wellbeing, through walks and other interactions with the natural world, writing, singing, music and art therapies, comforting touch, and massage.
[…] providing moments of wellbeing through whatever means are suitable, like going for a walk, listening to music, massage, remembering life story […](Respondent 8)
We used to have a form of dignity therapy, i.e., writing groups, where palliative care patients could express themselves in writing (poems or short texts). This was very much appreciated, and I wish we had the resources to continue this activity. The personal narrative or life story is so important. Now we have a music therapist. Music is also an important part of spiritual care.(Respondent 344)
Providing Suitable (Quiet/ Safe) Spaces
Responses in this subtheme identified spiritual care as providing safe spaces for patients’ thoughts and reflections, and for silence, including physical spaces, such as a room for contemplation, reflection, or prayer:
Listening, providing a safe space for conversation, silence and reflection, discussing religion and spirituality, patients expressing their feeling and concerns.(Respondent 94)
3.3.3. Theme 3: Religion: Beliefs and Activities
Responses in this theme identified spiritual care as related to religion, supporting religion and religious practices, discussing religious beliefs and concerns, providing religious services, prayers, sacraments, and hymns, songs and other religious music, and/or a book or a tree for prayers, messages, memorials and reflections.
Religion: Any Religion Welcome, Identifying and Discussing Religious Beliefs, Concerns, and Their Role in Decision-Making
One exhaustive response which mostly fit this theme (while also including comments which fit other themes) read:
[…] the hospital chapel is open 24/7 for personal reflection, quietness, prayer, rituals—the chaplain on the team and the other hospital chaplains are available for consultations and informal talks. They keep no written record—there are regular services in the hospital chapel, or the patients may watch services on TV or listen to the radio—the chaplains may assist with rituals (lighting a candle, prayer, holy communion, baptism, wedding, burial, religious service in patient’s room, farewell service when a deceased person is moved away from the hospital). The less formal rituals are also practised by nurses when asked for (lighting of candle, reading a prayer, singing a hymn, read a poem, offer a CD to listen to, decorate the room with flowers)—a Buddhist spiritual coun[s]ellor is also employed by the hospital—the team of chaplains have contact information for all types of religious/spiritual coun[s]ellors, from all denominations, and summon them when appropriate—music of the patient’s choice is played on the ward/in the room—patients may decorate the room with art work of their choice—patients and families are offered books to read—they may bring personal photos and items into the room—family members may visit any time of day—the team members and ward staff try to include spiritual issues when taking the patient’s history, and be open to spiritual issues and questions in daily conversations with the patients. We use the HOPE model as a guide for the spiritual assessment.(Respondent 344)
Religious Practices and Activities (e.g., Prayer, Reading Religious Texts, Performing Religious Rituals, Sacraments, Communion)
We have a tree that relatives can hang messages or prayers on for their relative or friend. And a multi faith room with a few candles that people can reflect or pray in.(Respondent 9)
In the hospice there is a quiet space which is well kept by the nurses (photobook, flowers, book in which family members can express their feelings).(Respondent 160)
[…] discussing a person’s religious concerns, participation in service or other forms of prayer, receiving communion and other sacraments, receiving the feeling of support, and safety.(Respondent 156)
Reading passages from religious texts at the patients request. Standing in silence in connection while minister or family say prayers.(Respondent 41)
3.3.4. Theme 4: Focused Discussions
Responses in this theme, and one or more of its four subthemes, identified spiritual care as enabling discussions on specific points, either broadly, as the provision of counselling or psychotherapy, or more specifically as asking patients about what matters, reminiscence and life review, exploring and discussing topics such as patients’ hopes, fears and anxieties, anger, grief and guilt, regrets and forgiveness, and providing reassurance.
Life Review/Reminiscence
Listening to patients’ stories, reminiscing. Encouraging life review. Respecting patients’ wishes and preferences, including when they can no longer express them.(Respondent 41)
Counselling/Psychotherapy
Prayer Supportive psychotherapy Psychodynamic therapy Dignity therapy Art therapy Meaning based therapy Existential counselling and support Bereavement support Social work and chaplaincy interventions Care planning/goal setting Advanced Care Planning Memorial services Rooms for art therapy/family gatherings in the ward/prayer room (multi faith) & chapel in hospital grounds The types of intervention dependent on what the person needs to assist with centredness and to assist maintain the integrity and dignity of the individual.(Respondent 98)
Relationships
Opportunities to discuss feelings, concerns, anxiety regarding family friends, the future. Activities and support groups 1:1 with chaplain. Support from bereavement team. All staff are involved in patients’ care and any can assist patients, family members, friends with their spiritual care needs as appropriate and desired by the patient.(Respondent 235)
Individual contact to explore impact of the illness on the person, their quality of life and relationships. Also an opportunity to discuss concerns about family members and thoughts of death. Funeral plans. Explore fears.(Respondent 37)
Discussing Life after Death/Meaning of Life
Discussing with patient/family member about existential concerns/questions (as Why happen this to me? Is there life after death? Why bad things happen to good people).(Respondent 493)
It includes existential discussions, prayer, meditation, lifestory telling, singing hymns, reading from religious textbooks, talking about the Family situation, loneliness, anxiety, grief, d[e]sire, thoughts about afterlife, resurrection, reincarnation, meditation of different traditions, body exercises, breathing.(Respondent 179)
[…] discussing concerns about life and death and the meaning of it all regardless of any religion.(Respondent 126)
Approach to care explicitly includes care of spiritual needs in broadest definition of term, i.e., issues pertaining to patient and families members’ values, meaning, existential beliefs and religious beliefs and practices.(Respondent 309)
Concerns are not often the point, much more resources (of dignity, meaning, hope) are so.(Respondent 234)
3.3.5. Theme 5: End-of-Life and Advance Care Planning/Discussing Death and Dying
This theme linked to Theme 4, as the quote above from Respondent 37 illustrates, demonstrating the overlap between these two themes. However, Theme 5 is more focused than Theme 4, encompassing an understanding of spiritual care as being particularly focused on talking about death and dying and planning for end-of-life. Respondent 344, who had begun their response by discussing supporting patients’ religious faiths at length (Section 3.3.3), went on to address advance care planning:
[…] advance care planning includes sections on values, hope, strength, support, meaning, coping—all part of spiritual care—spiritual issues are discussed when the end of life is approaching. The patient and family are asked about their wishes, priorities, preferences, and beliefs, what is important to them, what they worry about—in the dying phase, spiritual coun[s]elling is offered.(Respondent 344)
3.3.6. Theme 6: Staff Roles, Training and Input
This theme included which staff and which staff roles were involved in spiritual care, what this meant in relation to specific staff and their roles, and whether the full multi-disciplinary team was involved in assessing and intervening or not. One respondent also went into detail about what the assessment involved, and their response included content encompassed by other themes (above), including engaging with focused discussions, including around relationships, fear, grief, and meaning:
We talk to patients about spiritual issues as part of a consultation. The treating physician refers the patient to our team. We always assess spiritual issues. Questions we can ask?—How do people (patient and family) cope with the incurable disease? Do they have difficulty with ‘letting go’?—What do people experience as quality of life, what is threatening their quality of life? Are there activities people still want to do in life, and can we give support in achieving those?—Do they have a religion and does this give support, or fear?—What do they think about what is after this earthly life?—Do they have fear of the trajectory to death?—Are there issues about end-of-life decisions?—Do they need care from a spiritual worker? Do they need religious rituals—Do they have questions about why they have this disease? Why they have to suffer? What is the meaning of suffering? We always give patients space to talk about all these issues.(Respondent 240)
Responses in this theme most frequently identified the key spiritual care providers as chaplains, or spiritual or pastoral care specialists, and/or religious professionals:
Visiting service by chaplains. If there are situations for intervention (crisis) the chaplain is called immediately by doctors or nurses.(Respondent 106)
Inpatient unit has “Interdenominational Quiet Room/Chapel”. Referrals to pastoral Carers pre and post-bereavement for follow up. Support for family and patients via pastoral care workers. Pastoral Carers are of various faiths and communities are supported via local churches where needed. Service runs monthly commemorative services.(Respondent 247)
Interfaith chapel open 24/7 for all persons for personal prayer, reflection, and meditation; regular religious services for many faith traditions; prayer rugs, t’fillin and prayer shawls available; reading materials and prayer books of many faiths. Chaplains available on request or by coming into the chaplains’ office for help and support.(Respondent 380)
Relatedly, since spiritual care entailed referrals to such specialists, some respondents commented on the difficulty of locating such people, especially in non-hospice-based community services:
[…] especially out of Hospice [it] is not so easy [to] find chaplains or other faith people to help these patients(Respondent 145)
3.3.7. Theme 7: Support for Families/Relatives before Death
The three smaller themes all related to support for other people than the person who was dying or had died: families before death, and after death, during bereavement, and also staff. Many respondents who considered that spiritual care included support for families, linked support before death and during bereavement. Some also linked this to care and support for staff. One respondent began by defining spiritual care as supporting patients, and continued to discuss families, focusing on supporting families before, and also immediately after, patient deaths:
Enough time for patients and their families to discuss religious concerns as well as feelings with all staff members (nurses, doctors, social worker, psychologist …) Signs when someone dies (candle at encounter desk, next to bed, ribbon at room door). Prayers, support, enough time for family to say goodbye when someone has died.(Respondent 71)
Encouraging families to bring in personal items such as special photos, children’s drawings, items which hold personal significance etc. for dying patients. Asking if patients or families would like a visit from the Chaplain or their own minister. […] Advising family members to say goodbye every time they leave the patient’s side, in case they don’t get another chance to say goodbye.(Respondent 41)
3.3.8. Theme 8: Support for Bereaved
Respondent 71 continued their answer by outlining support for families after bereavement:
Families receive a letter from us with wishes about 3 months after patient has died, twice a year meeting with families at PC unit one year after death (for praying, coffee, cake and talk). […] Offer [to family members to take part in a group] hike, but also a cabaret once a year for families.(Respondent 71)
3.3.9. Theme 9: Support for Staff
This theme was the smallest, and addressed supporting and providing support for staff, sometimes with the end of providing better patient care, but also as necessary and a valid need, which was good in itself. The same respondent went on from discussing family support to detail staff support:
Small ceremony thinking of patients that died for staff. […] Time for staff to discuss spiritual needs within team, with professional supervision, with spiritual care worker. Offers from spiritual care team for staff: hikes, preparations for feasts like Christmas or Easter, mails with quotes to think about, possibility for personal talks.(Respondent 71)
3.3.10. Anomalous and Contradictory Responses
Some responses were anomalous, and/or not amenable to coding in full. Two respondents wrote that circumstances prevented them from providing examples of spiritual care. One (Respondent 100) wrote: “Far too many to type on a phone”; another (Respondent 328) began by writing: “It’d take too long, sorry”, yet proceeded to write three vignettes about interactions with patients, the last of which, the longest, described a particularly difficult experience. Such responses did not always or entirely provide explicit examples, because the elements of care were oblique, or the respondent gave examples which they then problematised or denied. Respondent 328 continued to make another, similar comment in answer to Q25, the question following: “Is there any assessment of the outcome?” to which they responded:
Just clinically or subjectively. And also, please make clearer what you mean by spiritual care, as most of the acts I put in place were ‘psychological acts’ in my view. Where spirituality is part of the person I take care of them, my way. Even when I definitely fail as in case 3.(Respondent 328)
3.4. Additional Comments
In all, 115 of the 465 respondents provided a comment at Q28, the last item of the survey, which asked for any additional comments. Of these 115 respondents, 30 provided brief comments: 21 wrote “No” or “Nil” and nine thanked the survey organisers, with three of these asking to be involved in future studies and/or to be informed of the results.
Eleven of the 115 commenters were in the group of 39 who had answered No to all of 12–15. One of these 11 thanked the survey organisers for the survey, and two wrote “No” or “Nil”. The other eight respondents in this group gave a variety of responses. One respondent wrote that their organisation was beginning to implement spiritual care. In contrast another, from Portugal, wrote:
Here in this country [it] is very difficult to think differently about death and dying. Existential issue is a very complex matter but essentially because people don’t know why they [are] living, how can they know why they die?(Respondent 399)
Another respondent wrote:
I originally said yes to [providing] a personal intervention because I think listening to people, connecting with each other is a spiritual act—however this did not seem to fit the questions so I changed my answer to No.(Respondent 272)
This was an interesting and curious comment. Despite this respondent thinking that their understanding did not fit with what the survey was asking, the survey was intentionally designed to offer only minimal directions of possible responses to this item, although giving three brief examples of what might be included: quiet space, discussing religious concerns, enabling a patient to express their feelings about a family member. These might be thought to be examples of listening and connecting, and other respondents gave such activities as their examples of spiritual care.
Another of this group of 11 said simply that they recommended that patients speak to a priest, which other respondents had also identified as the entirety of spiritual care provision.
Three of this group of respondents highlighted the importance and need to address spiritual care, conceptually and in policy terms, and to provide resources. One of these three commented that training and agreeing on definitions and conceptualising spiritual care was very important, and that the necessary resources should be provided to facilitate this aspect of care:
Important to have clear and inclusive definitions of spiritual care. Provision is multidisciplinary but scope of practice for screening (all staff) of spiritual care trained practitioners and chaplains need to be adhered to and expertise recognised. Training, qualifications and ongoing professional development and supervision reflecting scope of practice is essential. Role of volunteers, adequate training, scope of practice and P[ersonal] D[evelopment] and supervision again need to be well defined. It is important to give professional spiritual care the support and resources needed for it to be embedded in Palliative care teams and for spiritual care to meet Palliative care standards beyond a volunteer model.(Respondent 220)
Several other respondents likewise stated that there is a great need for spiritual care, and one respondent highlighted the potential helpfulness of the EAPC including spiritual care in international policies for palliative care:
It would be helpful if EAPC would include spiritual care components in international palliative care policies.(Respondent 423)
Conversely, and echoing comments from others, elsewhere in the survey, e.g., from Respondents 272 and 328 (above), questioning how the spiritual or psychological are differentiated, defined, and understood, Respondent 116 commented on their own disbelief in the existence of the “spirit” and therefore difficulty with the concept of spiritual care:
Personally, since I do not believe in the existence of something that may be called “spirit”, I find difficult to deal with “spiritual assistance”. I think that most of the issues covered by the category “spiritual” are actually psychological, anthropological or religious, and that ought to be dealt [with] in different, specific, ways. The definition “spiritual” in my opinion is misleading, and does surreptitiously take for granted metaphysics as something supplied [sic] of existence, and with which [it] is possible [to] empirically interact: a position that I do not accept.(Respondent 116)
In contrast, Respondent 112 said that spiritual care is broader than religion, and, similarly to others’ calls for more clarity of definition, commented that more awareness of this was needed:
Spiritual care is not only related to religion and I believe this is something that needs more awareness so people who do not identify as religious are not fearful of being inundated with unwanted ideas and practices, but can receive assistance toward individual healing and comfort.(Respondent 112)
Other respondents to item 28, all of whom had said that they and/or their organisations provided spiritual care or its equivalent, provided some lengthy comments. These responses were diverse. In contrast to the above questioning of the very concept “spiritual”, several respondents mentioned a continuity and relationships between some or all of spiritual, psychological, emotional, and social support, and the importance of integration and shared responsibility in addressing this range of needs:
I see spiritual care as an integral part of the care I give, but it is not seen as important. Clinical assessment takes precedence and, though important, by not addressing a person’s spiritual needs their needs have not been met. Understanding a person’s beliefs and wishes can only improve their care and produce positive outcomes.(Respondent 78)
Some addressed specific local and cultural challenges, such as secularism and the difficulties with supporting religious faith in particular in such a context:
Spiritual care is not often referred to as “spiritual care” in a lay hospital in a lay country (e.g., France) where religious beliefs are considered private and not openly discussed. This possibly impedes its formalization.(Respondent 397)
In Italy the understanding of the need for spirituality and the total pain in the end of life is not entirely understood and considered marginal.(Respondent 121)
Several mentioned pressures on time:
Sometime[s] in hospital it is difficult to focus on spirituality with not much time to spend with family and patients.(Respondent 441)
Others commented on the need for continuing, ongoing research, more awareness, and/or more training:
I am hoping that ongoing research into the value of spiritual care as a crucial component to providing palliative care helps to gain recognition for the dearth of training and awareness for many of our palliative care medical teams. And as Dame Cicely pointed out, managing pain (Total Pain) often involves recognition of spiritual angst, existential pain and finding meaning.(Respondent 454)
4. Discussion
The response to our survey was gratifying, indicating the considerable interest in this field, and a remarkable result for a survey that ran for only a month, with no promotion beyond the initial email sharing the link. The detail some respondents provided was also somewhat overwhelming, with some open, heartfelt and moving responses, and we are extremely grateful for the openness and honesty of these.
Respondents were mostly over 45 years old, with the largest group aged 46–55, and about two-thirds were women (65%). Respondents came from a wide range of countries and regions across the world, 67 countries and 11 regions. Most were working in the region, if not the country, where they had been born. The only difference was for respondents from Africa, about half of whom were working in a different region from where they were born. This is an interesting finding, but not an issue our survey was seeking to explore, and, because only small numbers of our respondents were born in Africa, this can only be an observation, and no meaning can be assigned to the difference.
Our aim was to conduct an exploratory, scoping study, seeking qualitative data describing perceptions and understandings of spiritual care, to be contextualised in summaries of the sociodemographic characteristics of respondents. We were not seeking a representative sample on the basis of any of those characteristics, but, if data permitted, we provisionally planned to explore relationships between the responses and themes identified, and respondents’ sociodemographic characteristics, such as age, sex, personal religious faith and/or spiritual practices, length of experience in palliative care, and possibly region or country of work.
In the event, responses varied considerably in length and detail, with some providing considerable depth and detailed content which fit across many if not all the themes, while others gave only brief answers. It was impossible to determine the cause of these differences, whether the brief or less exhaustive answers were due to pressures of time, or technical problems, or the device through which respondents were engaging with the survey (one respondent explicitly said “too much to type on a phone”), or whether brief or missing answers were due to respondents’ lack of knowledge or perception. Hence any associations between respondents’ characteristics and the specific themes they identified would not have been meaningful. We therefore decided to focus solely on the detail of the qualitative data and the content of the themes themselves.
The five main themes we identified from the survey responses conceptualised spiritual care as attitudes towards or actions with patients. Theme 1 encompassed the character of care providers’ behaviour towards patients, or the manner in which care is provided. The four other main themes comprised specific actions: 2: supporting patient wellbeing, including through provision of particular services; 3: supporting patients’ religious beliefs, via provision of suitable services, and also through facilitating and enabling religious practices, rites and rituals; 4: focused discussions, sometimes framed as psychotherapy or counselling by particular specialists, sometimes enabled by all staff, and addressing specific issues of meaning and feelings, including patients’ hopes, fears, regrets, and grief; 5: discussions focused specifically on death and dying and end-of-life care.
The other four, smaller themes broadened the topic beyond direct patient interaction. Theme 6 comprised issues for staff teams and services, including the need for and importance of specialist input, especially from chaplains, and the need for training of all staff, including generalists and non-specialists. The other three smaller themes addressed support for those who are not patients: Theme 7: families before deaths, 8: families after bereavement, and 9: support for staff.
All these themes were consistent with and corroborated those identified in other research studies and systematic reviews of such studies (e.g., Kristeller et al. 1999; Vivat 2008; Edwards et al. 2010; Walker and Waterworth 2017; Minton et al. 2018; Batstone et al. 2020; Ghorbani et al. 2021; Taylor 2021; Morland et al. 2022). Our findings reflect the three broad domains of the EAPC definition of spiritual care (Nolan et al. 2011), that is: existential questions, attitudinal and relational matters, and (where relevant) religious considerations. Our findings strongly resonate with findings from other empirical studies, so contributing to the growing consensus that is building in the field on what spiritual care comprises.
Our first theme: the character or quality of staff’s behaviour, that is, the manner in which care is provided, or the approaches or attitudes of staff towards patients, occurs frequently in the literature. It resonates with Taylor’s discussion of healing communication as an essential tool for spiritual care, highlighting the importance of good quality attention, awareness and empathy (Taylor 2021). A systematic review by Ghorbani et al. (2021) identified presence and therapeutic use of self as two of eight spiritual care interventions. Similarly, a recent focus group study with Norwegian nurses (Morland et al. 2022) identified compassion, love, and mercy, or care with a personal touch, as spiritual care, although pointing out that this can also be understood as good fundamental holistic care, and arguing that more clarity on the distinction, and what makes spiritual care spiritual, is needed.
Other studies (for example Vivat 2008) have previously also questioned whether the manner of care alone is sufficient for that care to be considered spiritual care, or whether specific content is also needed. Our four other main themes address the content of care, and specific actions and interventions; supporting patients’ wellbeing and religions, and discussion of general or particular issues related to the end-of-life, whether broad questions of meaning and relationship, or focused on topics such as advance care planning and end-of-life arrangements including for remembrances and funerals. The study by Minton et al. (2018) and recent systematic reviews by Batstone et al. (2020) and Ghorbani et al. (2021) also identify active behaviours as spiritual care interventions, particularly meaning-centred interventions or explorations of patients’ spiritual perspectives (Ghorbani et al. 2021).
Our four smaller themes: the role and input of staff, and care and support for families before death, for families during bereavement, and for staff address aspects of spiritual care which also occur less frequently in the literature. One recent systematic review (Batstone et al. 2020) identified that some staff in a few included studies considered that referrals to specialist spiritual care providers comprised spiritual care.
Likewise reflecting the less frequent identification of spiritual care as involving spiritual care for families as well as patients, fewer research studies address this either. Most of the few studies which do focus on this tend to be of acute hospital settings (e.g., Hennessy et al. 2020), including ICUs (des Ordons et al. 2020), or paediatric contexts, spiritual care for parents of dying children (e.g., Koch and Jones 2018), although Vigna et al. (2020) address spiritual support for caregivers of adult palliative patients in Brazil. Support for staff is even less frequently identified as a part of spiritual care, but Wasner et al. (2005) demonstrated the benefits of spiritual care training for professionals, and a faith-based teaching hospital in the USA systematically implements spiritual (Christian) care for its staff (McMillan 2016). Our respondents were highly engaged with the survey and its content. Many discussed following established guidelines and models for spiritual care, with some discussing amendments and adaptations that had been made in their local setting. Several respondents, however, when asked if they had any additional comments, observed the challenges and difficulties with providing this kind of care.
Previous studies have often pointed to the issues of staff lacking time and training (Balboni et al. 2013). Other comments focused on the need for definitions, with some disputing the existence of spiritual need at all, and others noting their perception that there was a need to accept a diverse and open definition of spirituality, not necessarily linked to religion. Many respondents commented on the need for staff training and some for staff support, and several stated that more research is necessary, particularly in demonstrating the value of spiritual care.
4.1. Study Strengths
The respondents to our survey were diverse, from 67 countries and most regions of the world, with many participants having lengthy experience in the field. Most of the respondents who began the survey completed it, and were engaged with it in its entirety, and many were extremely generous with their time and the detail they provided, offering rich responses conveying their personal understandings of spiritual care.
This welcome engagement includes those who raised queries regarding where the boundaries lie between spiritual care and other forms of care, psychological, social, and religious. This is not unique to our study, but an ongoing matter of debate in this field of research as it continues to develop, and questions like these are valuable for continuing reflection on definitions and understandings of the complexity involved.
4.2. Study Limitations
There were small numbers of participants in some regions: Africa, Middle East, Far East, Southern Asia, although our study was simply exploratory, and we were not aiming for a representative sample.
Our survey investigated perceptions and understandings, not activities directly, and respondents provided statements about actions, whether their own or those of others. The findings therefore cannot be claimed to directly represent actual practices. However, some examples provided by respondents described or outlined stories of activities by the person and/or members of their team, so were more than abstract statements or assertions.
As a survey, this study is more of a snapshot than an in-depth investigation; there was no possibility of following up responses, asking for clarification or more detail, or discussing or probing responses further, as would be possible in an interview situation. Queries raised by some responses could not be investigated further, so some lack of clarity remained for some.
The survey was designed as an ad hoc tool, and, although we piloted the content of the tool and subsequently revised some of the questions when we developed it, we were not much experienced with online platforms for survey tools and were also limited in the time available for refining technical features. Some weaknesses and omissions in the online design resulted, some of which created some difficulties for the analysis: SurveyMonkey reports results from the fields in the dropdown lists separately, and we did not include all professional roles in the dropdown lists; for example, we did not have a category for professions allied to medicine, or specifically for occupational therapists or physiotherapists, nor for health care assistants, nor leaders of organisations or policymakers. The survey did not oblige responders who answered No to all of questions 12–15 to skip to the end (Q28) either; they were merely requested to do so, and a few did not.
We were not expecting such a large response either. The volume of responses received meant that managing the additional free-text responses for these roles was challenging. The Other item was chosen by 154 respondents, whose professional roles were not any of the listed options; it was an oversight not to include some roles, such as AHPs, including occupational and physiotherapists, or policy makers or service leaders, as response options.
5. Conclusions
Our study gathered data on understandings of spiritual care and related practices from a breadth of participants internationally, 465 respondents across the world, with 228 providing examples of spiritual care, some lengthy and detailed. Most responders were palliative care providers with ten or more years of experience, with a smaller group who were policymakers, researchers, and leaders or coordinators of palliative care provision. We found no differences between the sociodemographic characteristics of the whole group and those of the subset of 228, other than for religious beliefs or personal spiritual practices, which a greater proportion of respondents in the subset than in the whole group stated that they had.
The five main themes we identified conceptualised spiritual care as attitudes towards or actions with patients. Theme 1 encompassed the character of care providers’ behaviour towards patients. The four other main themes comprised specific actions: 2: supporting patient wellbeing; 3: supporting patients’ religions; 4: focused discussions, addressing specific issues of meaning and patients’ feelings; 5: discussions focused specifically on death and dying and end-of-life care. The other four, smaller themes, encompassed issues beyond direct patient interaction. Theme 6 comprised issues for staff teams and services. The other three smaller themes addressed support for others than patients: 7: families before deaths, 8: families after bereavement, and 9: support for staff.
These themes from our survey confirm and corroborate findings from other research studies, ranging from individual small-scale qualitative studies to broader systematic reviews, and contribute to the growing consensus on what spiritual care comprises. Many of our respondents emphasised the critical importance of the spiritual aspect of care and called for more attention to be paid to spiritual care, in policy, in practice, and in research. Further research, particularly larger scale studies, and focusing specifically on the implementation of spiritual care in practice, would be of great value for the field, and several respondents expressed the wish to be involved in such future studies.
Author Contributions
Conceptualization, B.V., T.Y., M.T.G.-B.M.; methodology, B.V., T.Y.; software, B.V., T.Y., R.L.; formal analysis, B.V., T.Y., R.L., M.T.G.-B.M.; data curation, B.V., T.Y.; writing—original draft preparation, B.V.; writing—review and editing, B.V., T.Y., R.L., M.T.G.-B.M.; project administration, B.V., T.Y. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific external funding. B.V.’s post is funded by Marie Curie, grant number MCCC-FPO-16-U.
Institutional Review Board Statement
Ethical review and approval were not required for this survey, since the lead authors are based in the UK, and the UK Health Research Authority categorises surveys of this type, which do not involve patients, as service evaluations, rather than research studies. The Madrid Regional Healthcare Ethics Department also stated that ethical approval was not required when approached by the author based in Spain.
Informed Consent Statement
Informed consent was not taken directly from participants, but was implicit in their participation in the survey after reading the survey introduction which, in addition to outlining the content of the survey and the likely time it would take, guaranteed participant anonymity and the secure protection of their data. Potential participants were initially contacted by the EAPC via a membership mailing list and asked to forward the survey link to colleagues they thought might be interested in participating. The authors had no access to any mailing lists or contact details, other than those which a few respondents chose to supply when responding to the survey.
Data Availability Statement
Participants agreed to participate on the basis of their anonymity being assured. It might be possible to identify some individuals by the combination of the data they provided, so they are not in any public repository. Data are available via the corresponding author on reasonable request.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Anandarajah, Gowri, and Ellen Hight. 2001. Spirituality and medical practice: Using the HOPE questions as a practical tool for spiritual assessment. American Family Physician 63: 81–89. [Google Scholar]
- Balboni, Michael J., Adam Sullivan, Adaugo Amobi, Andrea C. Phelps, Daniel P. Gorman, Angelika Zollfrank, John R. Peteet, Holly G. Prigerson, Tyler J. VanderWeele, and Tracy A. Balboni. 2013. Why is spiritual care infrequent at the end of life? spiritual care perceptions among patients, nurses, and physicians and the role of training. Journal of Clinical Oncology 31: 461–67. [Google Scholar] [CrossRef]
- Batstone, Elizabeth, Cara Bailey, and Nutmeg Hallett. 2020. Spiritual care provision to end-of-life patients: A systematic literature review. Journal of Clinical Nursing 29: 3609–24. [Google Scholar] [CrossRef]
- Benito, Enric, Amparo Oliver, Laura Galiana, Pilar Barreto, Antonio Pascual, Clara Gomis, and Javier Barbero. 2014. Development and Validation of a new tool for the assessment and spiritual care of palliative care patients. Journal of Pain and Symptom Management 47: 1008–18. [Google Scholar] [CrossRef]
- Best, Megan, Phyllis Butow, and Ian Olver. 2016. Palliative care specialists’ beliefs about spiritual care. Supportive Care in Cancer 24: 3295–306. [Google Scholar] [CrossRef]
- Chochinov, Harvey Max, Thomas Hack, Thomas Hassard, Linda J. Kristjanson, Susan McClement, and Mike Harlos. 2005. Dignity therapy: A novel psychotherapeutic intervention for patients near the end of life. Journal of Clinical Oncology 23: 5520–25. [Google Scholar] [CrossRef]
- Clarke, Victoria, and Virginia Braun. 2021. Thematic Analysis: A Practical Guide. London, Thousand Oaks, New Delhi and Singapore: Sage. [Google Scholar]
- des Ordons, Amanda L. Roze, Henry T. Stelfox, Kathleen Grindrod-Millar, Tasnim Sinuff, Jennifer Smiechowski, and Shane Sinclair. 2020. Challenges and enablers of spiritual care for family members of patients in the Intensive Care Unit. Journal of Pastoral Care & Counseling 74: 12–21. [Google Scholar]
- Edwards, Adrian, Nannan Pang, Vanessa Shiu, and Cecilia Chan. 2010. The understanding of spirituality and the potential role of spiritual care in end-of-life and palliative care: A meta-study of qualitative research. Palliative Medicine 24: 753–70. [Google Scholar] [CrossRef]
- Ghorbani, Mojtaba, Eesa Mohammadi, Reza Aghabozorgi, and Monir Ramezani. 2021. Spiritual care interventions in nursing: An integrative literature review. Supportive Care in Cancer 29: 1165–81. [Google Scholar] [CrossRef]
- Grant, Elizabeth, Scott A. Murray, Marilyn Kendall, Kirsty Boyd, Stephen Tilley, and Desmond Ryan. 2005. Spiritual issues and needs: Perspectives from patients with advanced cancer and nonmalignant disease. A qualitative study. Palliative and Supportive Care 2: 371–78. [Google Scholar] [CrossRef]
- Hennessy, Nora, Kathleen Neenan, Vivienne Brady, Melissa Sullivan, Jessica Eustace-Cooke, and Fiona Timmins. 2020. End of life in acute hospital setting—A systematic review of families’ experience of spiritual care. Journal of Clinical Nursing 29: 1041–52. [Google Scholar] [CrossRef]
- Koch, Kendra D., and Barbara L. Jones. 2018. Supporting parent caregivers of children with life-limiting illness. Children 5: 85. [Google Scholar] [CrossRef]
- Koper, Ian, H. Roeline W. Pasman, Bart P. M. Schweitzer, Annemieke Kuin, and Bregje D. Onwuteaka-Philipsen. 2019. Spiritual care at the end of life in the primary care setting: Experiences from spiritual caregivers—A mixed methods study. BMC Palliative Care 18: 9. [Google Scholar] [CrossRef]
- Kristeller, Jean L., Collette Sheedy Zumbrun, and Robert F. Schilling. 1999. ‘I would if I could’: How oncologists and oncology nurses address spiritual distress in cancer patients. Psychooncology 8: 451–58. [Google Scholar] [CrossRef]
- Leget, Carlo. 2007. Retrieving the ars moriendi tradition. Medicine, Health Care and Philosophy 10: 313–19. [Google Scholar] [CrossRef]
- Ly, Stephanie, Fiona Runacres, and Peter Poon. 2021. Journey mapping as a novel approach to healthcare: A qualitative mixed methods study in palliative care. BMC Health Services Research 21: 915. [Google Scholar] [CrossRef]
- McMillan, Kathleen. 2016. Employee Spiritual Care: Supporting those who care for others. Journal of Christian Nursing 33: 98–101. [Google Scholar] [CrossRef] [PubMed]
- Mesquita, Ana Cláudia, Érika de Cássia Lopes Chaves, and Guilherme Antônio Moreira De Barros. 2017. Spiritual needs of patients with cancer in palliative care: An integrative review. Current Opinion in Supportive and Palliative Care 11: 334–40. [Google Scholar] [CrossRef]
- Minton, Mary E., Mary J. Isaacson, Brandon Michael Varilek, Jessica L. Stadick, and Shannon O’Connell-Persaud. 2018. A willingness to go there: Nurses and spiritual care. Journal of Clinical Nursing 27: 173–81. [Google Scholar] [CrossRef] [PubMed]
- Morland, Marianne, Wilfred McSherry, and Linda Rykkje. 2022. Understanding spiritual care—Perspectives from healthcare professionals in a Norwegian nursing home. Religions 13: 239. [Google Scholar] [CrossRef]
- Mount, Balfour M. 1976. The problem of caring for the dying in a general hospital; the palliative care unit as a possible solution. Canadian Medical Association Journal 115: 119–21. [Google Scholar]
- Murata, Hisayuki, and Tatsuya Morita. 2006. Conceptualization of psycho-existential suffering by the Japanese Spiritual Care Task Force: The first step of a nationwide project. Palliative and Supportive Care 4: 279–85. [Google Scholar] [CrossRef] [PubMed]
- Nissen, Ricko Damberg, Dorte Toudal Viftrup, and Niels Christian Hvidt. 2021. The process of spiritual care. Frontiers in Psychology 12: 674453. [Google Scholar] [CrossRef]
- Nolan, Steve, Philip Saltmarsh, and Carlo J. W. Leget. 2011. Spiritual care in palliative care: Working towards an EAPC task force. European Journal of Palliative Care 18: 86–89. [Google Scholar]
- Puchalski, Christina, and Anna L. Romer. 2000. Taking a spiritual history allows clinicians to understand patients more fully. Journal of Palliative Medicine 3: 129–37. [Google Scholar] [CrossRef]
- Puchalski, Christina, Betty Ferrell, Rose Virani, Shirley Otis-Green, Pamela Baird, Janet Bull, Harvey Chochinov, George Handzo, Holly Nelson-Becker, Maryjo Prince-Paul, and et al. 2009. Improving the quality of spiritual care as a dimension of palliative care: The report of the Consensus Conference. Journal of Palliative Medicine 12: 885–904. [Google Scholar] [CrossRef]
- Saunders, Cicely. 1967. The Management of Terminal Illness. London: Edward Arnold. [Google Scholar]
- Saunders, Cicely M. 1981. The founding philosophy. In Hospice: The Living Idea. Edited by Cicely M. Saunders, Dorothy H. Summers and Neville Teller. London: Edward Arnold, p. 4. [Google Scholar]
- Schultz, Michael, Tehilah Meged-Book, Tanya Mashiach, and Gil Bar-Sela. 2018. The cultural expression of spiritual distress in Israel. Supportive Care in Cancer 26: 3187–93. [Google Scholar] [CrossRef]
- Selman, Lucy, Teresa Young, Mieke Vermandere, Ian Stirling, and Carlo Leget. 2014. Research priorities in spiritual care: An international survey of palliative care researchers and clinicians. Journal of Pain and Symptom Management 48: 518–31. [Google Scholar] [CrossRef]
- SurveyMonkey. n.d. Available online: https://www.surveymonkey.co.uk/ (accessed on 28 October 2022).
- Taylor, Elizabeth Johnston. 2021. Healing Communication: A Precision Instrument for Spiritual Care. Seminars in Oncology Nursing 37: 151213. [Google Scholar] [CrossRef]
- Vigna, Paula Menis, Isac de Castro, and Renata Rego Lins Fumis. 2020. Spirituality alleviates the burden on family members caring for patients receiving palliative care exclusively. BMC Palliative Care 19: 77. [Google Scholar] [CrossRef]
- Vivat, Bella. 2008. “Going down” and “getting deeper”: Physical and metaphorical location and movement in relation to death and spiritual care in a Scottish hospice. Mortality 13: 42–64. [Google Scholar] [CrossRef]
- Walker, Hannah, and Susan Waterworth. 2017. New Zealand palliative care nurses’ experiences of providing spiritual care to patients with life-limiting illness. International Journal of Palliative Nursing 23: 18–26. [Google Scholar] [CrossRef]
- Wasner, Maria, Christine Longaker, Martin Johannes Fegg, and Gian Domenico Borasio. 2005. Effects of spiritual care training for palliative care professionals. Palliative Medicine 19: 99–104. [Google Scholar] [CrossRef]
- World Health Organization. 2020. Palliative Care. Available online: https://www.who.int/news-room/fact-sheets/detail/palliative-care (accessed on 28 October 2022).
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).