What Does Joy in Living Mean to Elderly Residents of Nursing Homes in Singapore?
Abstract
:1. Introduction
- (i)
- What does Joy in Living mean to elderly residents of nursing homes in Singapore?
- (ii)
- What are the enabling conditions that are conducive for Joy in Living in nursing homes?
- (iii)
- What are the disenabling conditions that are not conducive for Joy in Living in nursing homes?
- (iv)
- How does Person-centered Care support Joy in Living in nursing homes?
2. Materials and Methods
2.1. Design
2.2. Participants
2.3. Data Collection
- (i)
- Participants’ background and why they are in a nursing home;
- (ii)
- Participants’ day-to-day living experience in the nursing home;
- (iii)
- Participants’ religious/spiritual beliefs, their belief system and purpose in life;
- (iv)
- Participants’ understanding of Joy in Living, their views whether Joy in Living is possible in a nursing home and why if their answer is either yes or no;
- (v)
- If participants are living a joyful life in the nursing home, what are the things contributing to it and vice versa.
2.4. Data Analysis
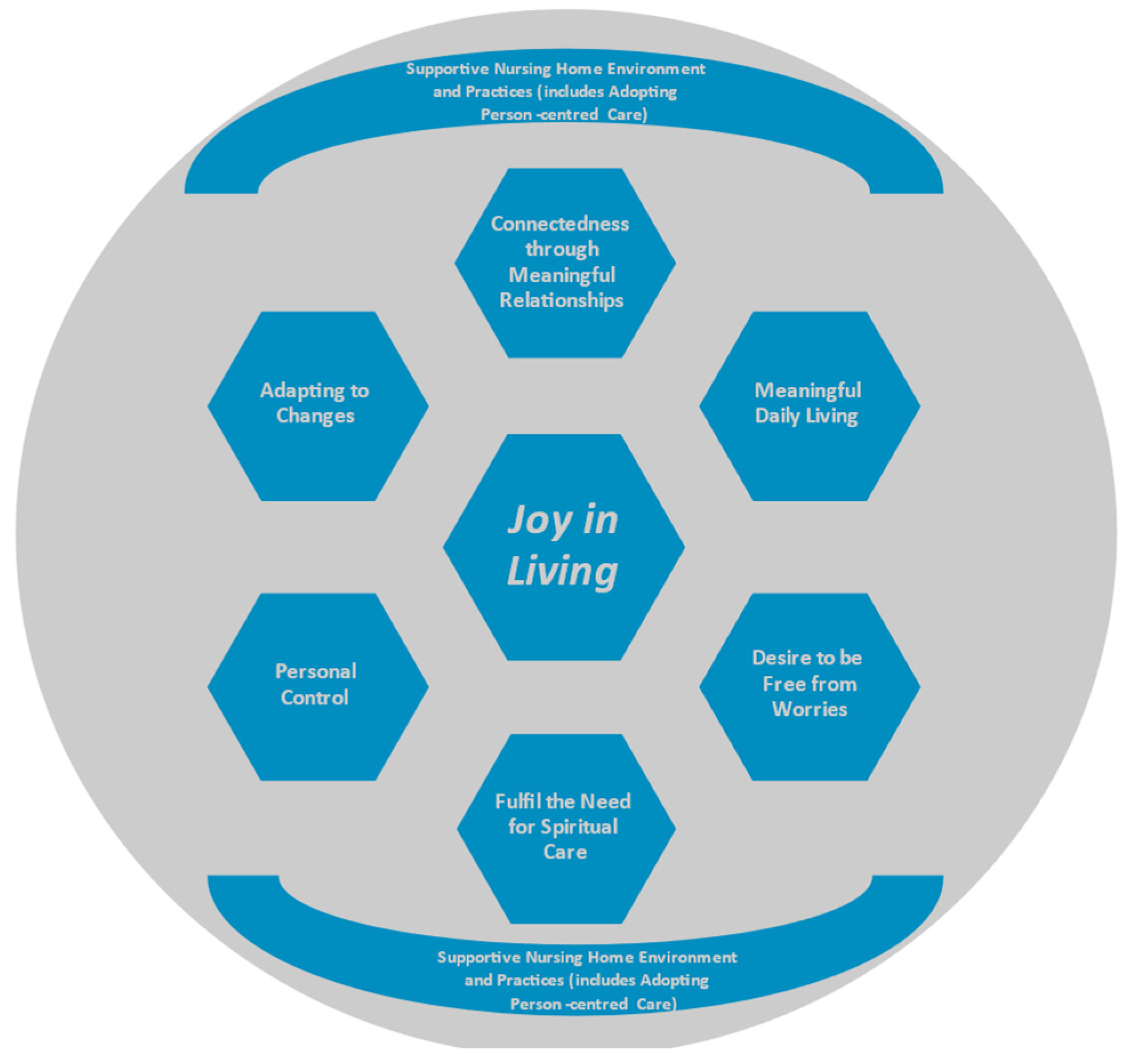
3. Results
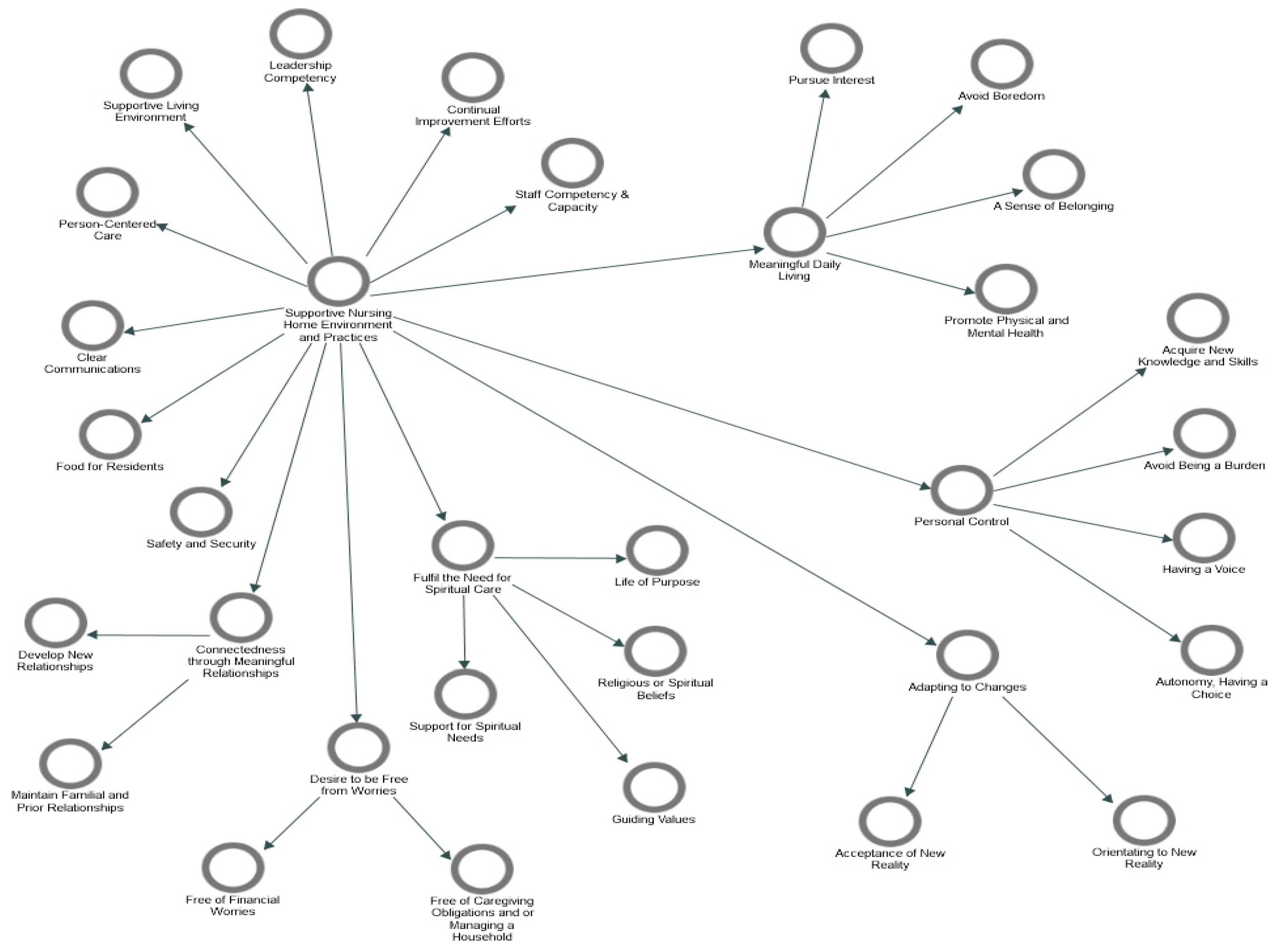
3.1. Supportive Nursing Home Environment and Practices
3.1.1. Person-Centered Care
* xxx is talking to him, cajoling him to finish his meal. He smiles at her and takes a few more spoonful of porridge and the vegetables.(2nd Observation at Nursing Home B)
* To protect the identity of staff, name of staff is replaced with xxx
The Therapy Assistant is sitting next to her and stroking her hair. She speaks to the resident in a Chinese dialect. The Therapy Assistant, who is a local Chinese and a mature staff in either her late forties or fifties, smiles at me and says she is speaking to the resident in Teochew.(1st Observation at Nursing Home A)
“Because I feel that I come here is suit for me. I got the thinking that somebody can look me until old”.(B1, Length of Stay: 3–5 years, Female, Chinese)
“What Joy in Living! Lousy, lousy place. They don’t treat you very well. You want your diaper changed, so hard to get diaper. You lie down, lie down wait for diapers”.(Impromptu Conversation during 1st Observation at Nursing Home C)
3.1.2. Supportive Living Environment
“…peaceful. I don’t how when I see the picture I know I want. My friend gave me the picture of the building. I went to other homes, but I cannot suit, then I see this I like. My sister also say better, this one also nice…They got proper place. All the sleeping place they have water, put water for drinking at hall”.(B1, Length of Stay: 3–5 years, Female, Chinese)
“I like the garden. Our canteen very, very noisy… in my heart is peaceful. I feel happy in my heart when I hear the water, birds and fish swimming… I also pray there, give me joy”.(C6, Length of Stay: 3–5 years, Male, Malay)
“This building is not properly maintained. It’s dirty. Look at all the fence, never clean. Compared to the old place, every week somebody will come clean all the fence”.(A4, Length of Stay: 1–2 years, Male, Chinese)
“This is not as bad as the rats… I got a lot of things, so they say you cannot put on the floor and all that, so they gave but they gave one that’s broken <they gave him a cupboard>. And rats used to go in what from the back. Now they say they fix it”.(A5, Length of Stay: >5 years, Male, Chinese; during an Impromptu Conversation at the 2nd Observation Session)
“Yeah. It’s downstairs. There’s a fishpond and everything. Before we used to go down every day. We’ll go down, see the fish, then we all cannot…Now cannot because the COVID-19. We are not supposed to go down, leave our dormitories”.(C6, Length of Stay: 3–5 years, Male, Indian)
3.1.3. Safety and Security
She asks the residents for their names, refers to a medical records ‘IMR’ folder with residents’ names and their laminated photographs, before giving the medicines. The medication trolley is a mobile cabinet with mini drawers. The mini drawers have names and photos of the residents. The medicines are in the mini drawers.(1st Observation at Nursing Home A)
A consistent practice in all my meal observations is having dedicated staff moving around and watching over residents who are eating on their own in both the living and dining rooms. Staff also go around with a pair of scissors to cut the vegetables and meat/fish to smaller pieces for those who ask for assistance or look like they are struggling with their meals.(2nd Observation at Nursing Home B)
“The other day one man died, he fell off the wheelchair and hit his head. This man, I predicted a long time ago. So, nurse ask me why you talk like that. I said if you look, he goes to the toilet 20 times. So, he’s putting himself in danger. You as nurses need to make sure he keeps safe; they don’t lock the wheelchair. I said I fall never mind, but when he falls and there’s nobody around. That’s the danger”.(A4, Length of Stay: 1–2 years, Male, Chinese)
3.1.4. Staff Competency and Capability
“Some nurses are very observant. Some, not so… I speak frankly, sometimes they are very busy and some of them, they don’t bother”.(A4, Length of Stay: 1–2 years, Male, Chinese)
“A few is very good. They really do the job, they very follow the procedure. Like from bed transfer to this, they really take care of you. Some they just stand down there, like for my case I used to use slide board and slide to my wheelchair. Some stand behind look at you. Anytime I can miss out and I fell down. They just stand down there. Some really good ‘lah’ <simplest and most common Singlish expression like ‘yeah mate’ in Australia> they take my two legs then I slide over very fast. One second. I think less than 20 seconds I go there already. Some they sit down there and slowly do. Some of the nurses they really use their hearts to work, some they just are not really nice”.(A3, Length of Stay: 1–2 years, Male, Chinese)
“They got their problem about the work. How many people go out, already don’t work here”.(B1, Length of Stay: 3–5 years, Female, Chinese)
“Some can, some they will leave them. Because ‘aiya’ <Singlish expression of displeasure or frustration>, I don’t want to say anything because it’s not good. Sometimes nurse and all got visitors, special visitors, if no visitors, then you can see shouting”.(Impromptu Conversation during 2nd Observation Session at Nursing Home C)
3.1.5. Food for Residents
“But I like meat, not fish. When I’m outside I always want some meat. When I’m here I got no choice”.(A2, Length of Stay: 1–2 years, Male, Chinese)
Every day the same thing, rice, veggie those type of fish, white colour but not white one then they put those kind of black sauce, ‘wah lao’ <Singlish expression to profess surprise or shock, like the expression ‘Oh my God!’> the taste, horrible.(A3, Length of Stay: 1–2 years, Male, Chinese)
The Chinese one cancelled already. Sometimes got babi <pork>, don’t want. Now, Malay food. Sometimes can, sometimes cannot. I mean, last time one, the Tuesday ah, the Muslim food, they give me chicken. I vegetarian Tuesday and Friday. Eat rice and vegetable only. Last time I like, one staff Indian cook ‘resam’ <a spicy Indian soup dish>, curry in kitchen give me. Missy <nurse> say cannot, my sugar, eat food they give, cannot special.(A1, Length of Stay: 3–5 years, Female, Indian)
3.1.6. Continual Improvement Efforts
3.1.7. Leadership Competency
At the briefing at the female ward, staff nurse informed the Chief Executive (CE) that there was a new resident who was a little unhappy and having adjustment problem. CE walks over to the ward to speak to the new resident. CE returns shortly after her chat with the new resident. Apparently, according to the home protocol, the resident needs to be isolated for 7 days before she can mingle with rest of the residents at the common areas. She is bored. CE asks staff to give her an iPad to let her watch whatever shows she wishes to watch. A staff quickly follows up on this.(1st Observation at Nursing Home B)
“I know about this one <referring to the vacancy at Nursing Home A> because of the certificate course that * xxx <CE> teach. The trainer is xxx <CE> herself…Yeah, she trains us hopefully we’ll join this company but not all will join ‘lah’”.(Impromptu Conversation at 2nd Observation at Nursing Home A)
* To protect the identity of CE, name of CE is replaced with xxx
“…the food, all you need to do is to get somebody to do quality control. You’re paying for the food…But if you don’t bother about it, they will just give you the same and this is exactly what is happening”.(A5, Length of Stay: >5 years, Male, Chinese)
“They’re doing this as they’re told to do…By the superior, then they treat all as equal <same treatment for dementia and non-dementia residents> which I don’t like.(C4, Length of Stay: 3–5 years, Male, Indian)
Observer:
Have you given this feedback to the management?
Staff:
I’m not sure cos I just joined here. But I don’t like to highlight, this is not my portfolio I mean the <*xxx designation> is the lowest level here. Because we cannot understand that, we cannot do.(Impromptu Conversation at 2nd Observation at Nursing Home A)
* To protect the identity of staff and organisation, designation is replaced with xxx
3.1.8. Clear Communications
Resident: How long, when can I see family? When allow from MOH side?
Observer: I think soon because it’s been too long already. The government intends to allow visits to hospitals and nursing homes from 21st Nov onwards. This is what is announced in the newspapers and TV news. The resident is relieved to hear this.(Impromptu Conversation during 2nd Observation at Nursing Home C)
“But here only your family can come. Outsider cannot cos they have to take your IC everything. Take your IC and see your name, father’s name, mostly they see your father’s name…we are not supposed to use phone <handphone> here”.(C6, Length of Stay: 3–5 years, Male, Indian)
3.2. Connectedness through Meaningful Relationships
“My two sons here, I would say they’re very good. This is why I’m blessed. I think among all the residents here, I’m the luckiest… I got a lot of things to talk to them. You know I see a lot of them when the children come, just leave the food and not spend time talking to them. “Okay Pa, then they go out.” So, it’s a very short visit. They just come with some food and all that. The impression I get is as if they come because they are obligated to. My son can sit here for hours… Because there’s so many things, I can talk with them”.(A5, Length of Stay: >5 years, Male, Chinese)
“My birthday. My lawyer <friend> will come. Every year he will buy a big cake for me and for the residents… Good friend in the case that I have my friends who bring me stuff. I give them a call”.(A4, Length of Stay: 1–2 years, Male, Chinese)
“Morning, morning I cry already. My house. The last one boy, he say, “I want my father house”, he say… My number 1 daughter, her husband say the house sell and then CPF take the money, they give you. You stay in home here… I mean, the boy he don’t like. He want house. I give house to him. I sell already, the boy where go? I stay ‘sini’ <here in Malay>, where the boy go, where?”.(A1, Length of stay: 3–5 years)
“That is what people say. What people do is different. Well, I don’t know why they think this way. I always look after the family. I’ve never been disloyal. When I go back to my home in Melbourne, I’m afraid I don’t know how to say why are you this way. I’ve done nothing wrong. You’ve done wrong with me… My family never contact me”.(A4, Length of Stay: 1–2 years, Male, Chinese)
“Friend, but they never talk. All Chinese. I don’t know Chinese. I speak Malay, English. I Eurasian”.(B5, Length of Stay: 3–5 years, Male, Eurasian)
“Here, you get to meet with them often and get to know them closely… But generally, it probably is a lot of them is from other countries like Myanmar that they can’t talk and understand English well <referring to foreign staff>”.(B4, Length of Stay: 1–2 years, Male, Chinese)
“Because sometimes you talk the words can become, cause problems with other resident, even staff, I don’t talk so much”.(B1, Length of Stay: 3–5 years, Female, Chinese)
“Actually staff, they are not supposed to chit chat with us all. Cos this is a government place”.(C5, Length of Stay: 3–5 years, Male, Indian)
“Their temperament is bad. Because other things, certain things you cannot complain. You ‘pangsai’ <pass motion> they want to wash you up, is very good. I think most of them are annoyed because of the washing up, they have to wash our backside or shower us, and they’re not happy with that… They talk among themselves and show their face”.(B3, Length of Stay: 3–5 years, Male, Chinese)
“I don’t want to trouble them, all busy. All okay ‘lah’ here. I just watch TV ‘lah’. They put me to sit facing the TV with Chinese shows. Chinese TV also watch”.(C6, Length of Stay: 3–5 years, Male, Malay)
“But most of them are quite busy… More I would say that nobody’s perfect. So, they have to be more relaxed to be able to talk to us, at the same time, it is a balance that they cannot be too relaxed and not get things done”.(B4, Length of Stay: 1–2 years, Male, Chinese)
“Actually, the staff are quite good the staff. I mean quite good to the residents. They don’t shout around or bully them. They are very gentle to them and always attend to their requests. …Yeah, we get along quite well. I trust them. Nothing very personal…. Just the daily needs and all that. One or two only that are willing to buy for me. Close to me”.(C3, Length of Stay: 1–2 years, Male, Chinese)
While the staff are courteous and patient, there is no interaction beyond the task of feeding them safely without choking…The interaction is mechanical. Although the staff uses a few words of Malay, it is mainly to ask what colours the resident wants from the colour pencil set.(2nd Observation at Nursing Home A)
3.3. Meaningful Daily Living
“I do join the group exercise. It is good for my strength. I like the individual therapy better”.(A4, Length of Stay: 1–2 years, Male, Chinese)
“I go swimming you know. Here in the home”.(A1, Length of Stay: 3–5 years, Female, Indian)
The activities include stacking and rearranging cups, identifying matching items in 3-d game sets, completing jigsaw puzzles and colouring pre-printed drawings. One staff… walks around and supervises the residents…. For selected residents, he works on the range of motion of their upper limbs: the arm, forearm, and hands, while they are working on their assigned tasks.(1st Observation at Nursing Home C)
“Now, down here, there is not much activity. And then we are sort of restricted living here… My closest thing is a newspaper and the television… Plan all these activities that I can participate, I find that it’s very interesting. Because I don’t like to be bored you see. Anything that I can do I like to do. I’m not particular”.(C3. Length of Stay: 1–2 years, Male, Chinese)
“Down here, cannot, nothing. By 5 o’clock I call it a day. I just lie down”.(A2, Length of Stay: 1–2 years, Male, Chinese)
“Tamil don’t have”.(A1, Length of Stay: 3–5 years, Female, Indian)
“<Resident’s wish for volunteer visits to resume> Make me happy. Not lonely”.(C1, Length of Stay: >5 years, Male, Chinese)
“Then the rest of the time I read, I got a lot of books there, and I play ‘Sudoku’. You will be surprised”.(A5, Length of Stay: >years, Male, Chinese)
“Because I came into this place, I study more and more <the bible>, I pray every day…cos now I stay in this home even if I don’t go out is a heaven to me”.(C5, Length of Stay: 3–5 years, Male, Indian)
“Fits improved, upgraded by God. I can pour water for the plants.,. So, if you have a sincere heart, pour water for the plant…Because I came into this place; and I thank God”.(C5, Length of Stay: 3–5 years, Male, Indian)
Staff: You notice this lady sitting right in front of me…She always also when we give them medication they refuse to take, she’ll support us by asking them to eat. She’ll help us, do a bit of the chores, dry the medicine cups and all that…
Observer: She offered to help?
Staff: She offered to help. The residents they offer to help, you let them do some things.(Impromptu Conversation during 1st Observation at Nursing Home B)
A male resident sitting nearby is busy folding plastic trash bags. He is the only one doing this.
Observer: Why are you folding the trash bags?
Resident: I like to do. I like work, not boring.(Impromptu Conversation during 2nd Observation at Nursing Home C)
“I got more people to talk to… More of the staff… They have interesting hobbies and interests that I can talk to them”.(B4, Length of Stay: 1–2 years, Male, Chinese)
3.4. Fulfil the Need for Spiritual Care
“You know one thing which is very lacking here, pastoral care, this is totally lacking. They may say they have a pastor and all that… If he does come down because it is to preach. If you go in and look there are a lot of them there waiting to die. They’ve got nothing to do. Pastoral care should be more than just preaching. It should be really getting to know and understand how the elderly feel and communicate with him”.(A5, Length of Stay: >5 years, Male, Chinese)
“… you can pray but must go toilet, use clean water wash face, mouth, nose, ears, hair, arms, feet. Nobody got time take me toilet five times, wash clean before pray <referring to ritual washing called ‘wudu’ by Muslims before praying >”.(C6 Length of Stay: 3–5 years, Male, Malay)
“That time I stay at my nephew’s house, Neptune court, Holy family. I can walk, go church. <Now>, No. Just stay at home and pray at bed”.(B2, Length of Stay: >5 years, Female, Chinese)
“Got the photo God, I put on top small cabinet near my bed and I pray. All God photo, Vinayagar, Lord Shiva <Hindu dieties>, got ah, pray. I Hindu must pray in the morning after bathing… Before I sleep, I pray”.(A1, Length of Stay: 3–5 years, Female, Indian)
“…more cooling outside, a lot of leaves. I like to look at the leaves, green leaves all these… I just concentrate, close my eyes for one minute. Then I pray ah, just pray. Enjoy praying”.(A3, Length of Stay: 1–2 years, Male, Chinese)
“… never go to church after my father die when I young… Yeah, baptised. One day go to church after my father die. When young, If I never go, my father beat us go to church. My mother never beat. My dad beat… I don’t know. I never go to church. I devil. It is written. Written that I do plenty sin. Drink beer…go hell”.(B5, Length of Stay: 3–5 years, Male, Eurasian)
“I believe now got 2 religions inside my body, one Jesus Christ and amulets ‘lah’… See now, when I pray, I want to concentrate more on Jesus. Even the amulet to come and disturb me, I just don’t want to think… For those Thai amulets, they do have this type of amulet to heal. Heal the sickness. … All similar, basically all the same—don’t cheat people, don’t kill people, don’t do bad things, all the same thing but how come for Christian they say all these is not real. This is all demon, but it’s true ‘lah’ those amulets, when I wear that time I feel very happy, I feel very safe.(A3, Length of Stay: 1–2 years, Male, Chinese)
“I cannot kneel on floor. I sit in the wheelchair and always praying in my heart, always praying in my heart the Quran. Anytime I pray… Give me joy pray Allah… Pray Allah really make me healthy. Bless family with health and money”.(C6, Length of Stay: 3–5 years, Male, Malay)
“I pray every day in the room. My heart I pray, chant. I pray in the morning, before breakfast.
I don’t have a wicked heart. I don’t hurt people. I think nothing wrong. If you do something evil maybe you scared…I believe that if there is no God, we cannot come to this world. There is a God then you come to this world… Whatever the world is given we take. You make good karma, so you can get good things. Good karma is a blessing… I believe that whatever I want, God give me, that one I believe”.(B1, Length of Stay; 3–5 years, Female, Chinese)
3.5. Personal Control
“No. What is there to feedback because when you are given what he called the status of resident. So, in this thing, they are not accepting anything”.(C4, Length of Stay: 3–5 years, Male, Indian)
“This one, they got totally nothing here. They’ll lock you in, lock within the area. Can’t even go out. Can’t even come out here”.(A2, Length of Stay: 1–2 years, Male, Chinese)
“Here they are telling you what to do. You have no freedom to do. So, it bugs me. I make my coffee, I come out and read and drink, and they say why you come here for, so you get very frustrated…”.(C4, Length of Stay: 3–5 years, Male, Indian)
“But no matter how, ‘die die’ <Singlish phrase that it is a must have even if you have to die for it> I still need to do. I cannot skip my exercise”.(A3, Length of Stay: 1–2 years, Male, Chinese)
“They will show us the TV <exercise video>, last time my leg cannot carry but after this one I see is very good, I can move my legs. Like this one very good, American exercise. Or Australia, Australia one, not sure”.(B1, Length of Stay: 3–5 years, Female, Chinese)
“I am married. I have been here two to three years okay. I come here to relieve my wife. She runs around do the errands, cook, then go see doctor, go to the bank, take me to see doctor because of my Parkinson’s. And she has cancer… Here I can be more relaxed”.(B4, Length of Stay: 1–2 years, Male, Chinese)
“Want to learn <to go on internet and use the various functions>. But how to learn?”.(C2, Length of Stay: 1–2 years, Male, Chinese)
“I want to learn how to how to do Zoom and I would like to do tuition again and I can give tuition for free”.(A5, Length of Stay: >5 years, Male, Chinese)
“Yeah, I would like to <learn to use a smartphone and surf the internet>. I’m still very alive”.(C3. Length of Stay: 1–2 years, Male, Chinese)
3.6. Desire to Be Free from Worries
“I think my brother is arranging that… I don’t know. I simply pass my time like that, no problem. I never go and check whether many more money left or what. I never go and check”.(C3. Length of Stay: 1–2 years, Male, Chinese)
“Young time I was worried…Everything I worry. If have enough money for rent, food, and everything. <Now> Everything is free. Just don’t want to worry”.(C2, Length of Stay: 1–2 years, Male, Chinese)
“I stay here, no need to do work. I stay here good…Now, I no need to walk, and just lie down. Last time in my home, cook, cook, cook then scold. At my nephew’s house, he got so many things, too many things, the plate too many to wash”.(B2, Length of stay: >5 years, Female, Chinese)
3.7. Adapting to Changes
“I stay here quite long already. I use to”.(C6, Length of Stay: 3–5 years, Male, Malay)
“I was sick, I fall down. Yeah, so my friends say it’s very difficult, you two stay and no people to look after I and my sister…I see the home is quite good, my friend told me, so they let me think over around three days… I think to make sure my sister also wants to go. My sister says okay, we go in a home better”.(B1, Length of Stay: 3–5 years, Female, Chinese)
“For me, I can take care of myself so many years all along. Why should I need to be in a home? I know the reason simple, they didn’t accept me, but I didn’t expect it to be all the way you know. They took my freedom; they took my freaking life away”.(C4, Length of stay: 3–5 years, Male, Indian)
“Nothing. Nothing. My hand and legs no good. Nothing can do… My dream is 80 pass away. Now 76. 4 more <years>”.(B5, Length of Stay: 3–5 years, Male, Eurasian)
“Now I cannot walk. I cannot go out. I happen to go out, my eyes will be gone…”.(B3, length of Stay: 3–5 years, Male, Chinese)
4. Discussion
5. Conclusions and Recommendations
5.1. Supportive Nursing Home Environment and Practices
5.2. Meaningful Daily Living
5.3. Fulfil the Need for Spiritual Care
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
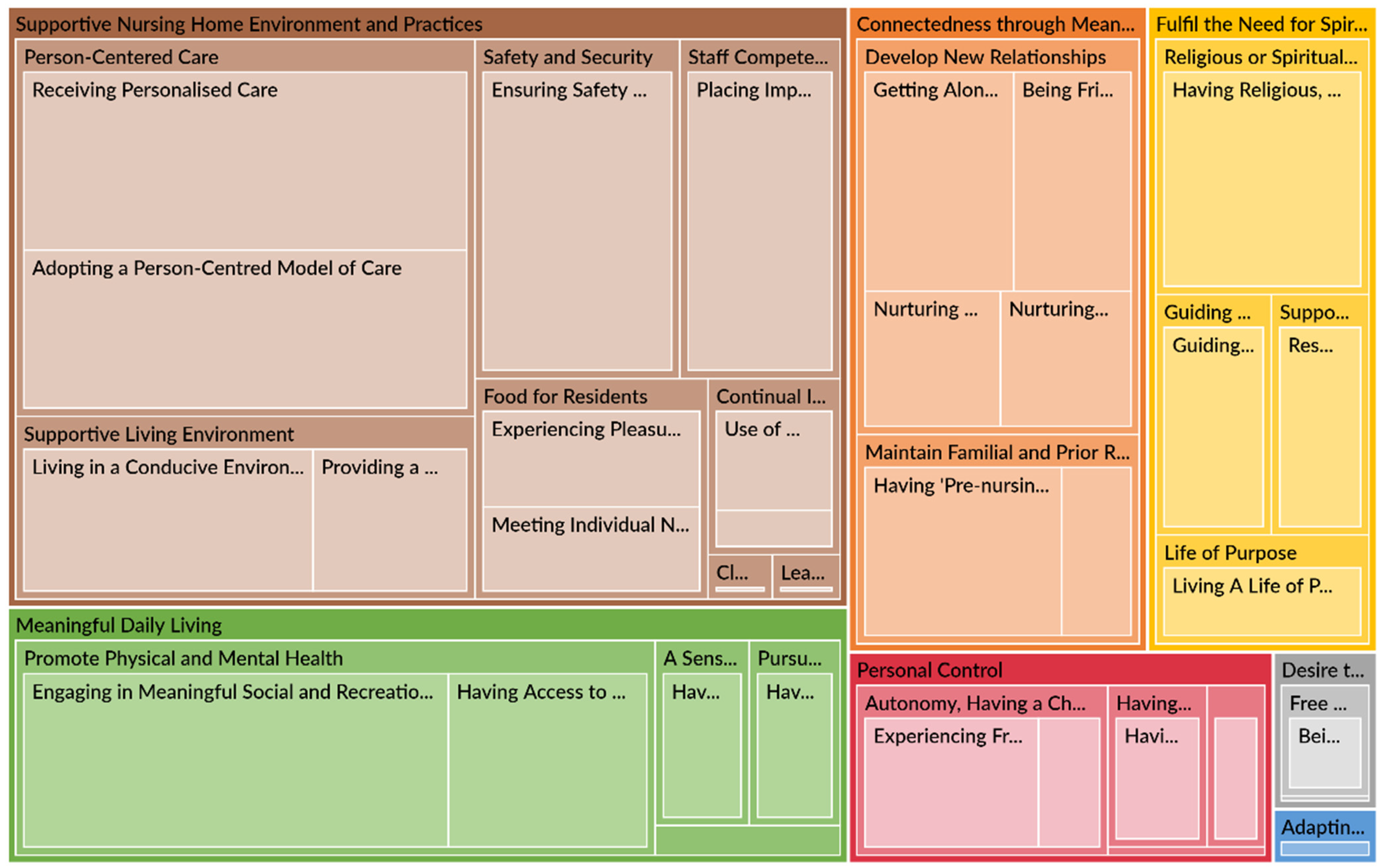
| Theme | Sub-Theme | Description |
|---|---|---|
| 1. Supportive Nursing Home Environment and Practices | Person-centered Care | Implementing a holistic care approach that emphasizes the well-being of the elderly as a whole person beyond just nursing and medical care. This includes residents receiving care that is tailored to their needs. Nursing homes use various person-centred care approaches such as Person-centred Care Model or its variations Person-directed Care or Eden Alternative Model to guide the delivery of care for elderly residents. |
| Supportive Living Environment | Creating a good living space in the nursing home for residents’ comfort and an experience of living in their own homes. | |
| Safety and Security | Systems, processes, and practices that protect residents from harm or injury. | |
| Staff Competency & Capacity | Building staff professional competencies, personal leadership, inter-personal and soft skills and knowledge. At the same time, ensuring that staff have sufficient bandwidth by hiring adequate headcount and rostering of duties. | |
| Food for Residents | Meals in nursing homes fulfil each resident’s dietary needs (e.g., vegetarian diet on certain days, diabetic calorie control, “Halal” meals etc.,) and ethnic dietary preference of what they enjoy most and find satisfying. And/or Giving residents opportunities to eat food that has nostalgia associated with it based on the social and celebratory deep memories that can include caring and love. | |
| Continual Improvement Efforts | Innovative or improved resident care policies, systems, processes, products, or services and care delivery approaches that improve nursing home residents’ lives. And/or reaping cost savings by bringing activities together in one place (e.g., a central kitchen, centralized laundry services) or outsourcing and using technology to simplify time-consuming tasks of staff. | |
| Leadership Competency | Management of the nursing home shows by example and/or implements systems, processes and practices that place the needs of the residents at the heart of design and delivery of services. | |
| Clear Communications | Residents receiving up-to-date and clear information on COVID-19 situation, national policies and programmes, and rules of the nursing home. | |
| 2. Connectedness through Meaningful Relationships | Develop New Relationships | Systems (i.e., the structure of how an organization is set up), processes (i.e., activities and tasks that need to be carried out to achieve the outcomes), and practices (i.e., the behaviors and actions of staff) that encourage bonding between residents and care staff (including volunteers). As a result of the bonding, residents feel that staff/volunteers genuinely care and support them throughout their stay in the nursing home. And/or Systems, processes and practices that encourage bonding and friendship among residents. |
| Maintain Familial and Prior Relationships | Proactively exploring opportunities (e.g., counselling by social workers from the nursing home) to mend and/or improve relations with residents’ families. Also, residents can communicate and see their family members and friends as easily as when they were living in the community. | |
| 3. Meaningful Daily Living | Pursue Interest | Setting aside time for residents to take up leisure activities of their choice and have sufficient rest. |
| Avoid Boredom | Boredom is a state of being weary and restless when there is too much time and limited or no opportunities to be engaged in social and recreational activities or pursue interests. | |
| A Sense of Belonging | Having a feeling of acceptance, inclusion and identity as a valued member of the nursing home. | |
| Promote Physical and Mental Health | Residents participating in leisure activities and activities that involve communication and interaction with others that are tailored to the needs and preferences of individual residents. And Residents participating in exercises and activities with movement (either solo or group activities) that have benefits for health, both physical and mental health; including occupational therapy activities that help to maintain health and promote independence of the elderly residents. | |
| 4. Fulfil the Need for Spiritual Care | Support for Spiritual Needs | Meeting residents’ need for inner awakening beyond everyday existence or * Gerotranscendence. * Gerotranscendence is a theory that older people transcend the limited opinions and views of life they once held, and develop new understanding of the self, relationships to others and fundamental existential questions. Support for spiritual growth includes tapping on the resources of the nursing home in the pursuit of God-consciousness and the gerotranscendence theory on self-awareness, relationship with others, and the cosmos. |
| Guiding Values | Moral standards, an ideology or religious views that dictate behaviors and attitudes in the lives of residents. | |
| Religious or Spiritual Beliefs | Relating to a particular religion and its ways or relating to matters of the human spirit or soul. | |
| A Life of Purpose | A central motivation in a resident’s life that gives him/her a reason to carry on living to achieve personal aspirations. | |
| 5. Personal Control | Having a Voice | Giving residents an active and participatory role in either deciding or influencing a decision on their care plans and daily activities. |
| Autonomy, Having a Choice | Residents having opportunities and autonomy to perform actions and move around without being constrained by staff or other parties. And/or Residents having a feeling of autonomy (i.e., freedom from external control or influence; independence) in taking actions to improve their health. | |
| Avoid Being a Burden | Residents not wanting to cause others (especially their loved ones and caregivers) a lot of difficulty, worry or hard work in their care. | |
| Acquire New Knowledge and Skills | Growth opportunities provided or supported by the nursing home for residents to acquire new knowledge and skills. | |
| 6. Desire to be Free from Worries | Free of Financial Worries | Residents not wanting to feel troubled or being required to do something about their finances. |
| Free of Caregiving Obligations and/or Managing a Household | Residents not wanting to feel troubled of caregiving obligations to children, grandchildren or spouses, and/or managing a household. | |
| 7. Adapting to Changes | Orientating to New Reality | Residents adjusting their lives toward the established norms of communal living in a nursing home. |
| Acceptance of New Reality | Residents can accept their diminished health functions. |
| Summary of Studies on Person-Centred Care and the Findings | |||
|---|---|---|---|
| Item Number | Theme | Summary of the Study Findings | References |
| 1 | Improved health outcomes in clinical settings | Patient-centred care is associated with better care process with positive outcomes, such as clinical effectiveness, satisfaction ratings, and improved QOL. | (Doyle et al. 2013; Fors et al. 2015; Lowther et al. 2018) |
| 2 | Effectiveness of Person-centred Care of people with dementia | Person-centred care is associated with positive impact on well-being, QOL, improvements to degree of depression severity, and reduced behavioral symptom of agitation in persons with dementia. | (Kitwood 1997; Edvardsson et al. 2014; Barbosa et al. 2015; Kim and Park 2017) |
| 3 | Reduction in cost to healthcare organisations | Patient-centred care interventions in intensive care units and hospital treatments that resulted in cost savings from reduced length of hospital stay and improvements to discharge process. | (Ulin et al. 2016; Goldfarb et al. 2017) |
| 4 | Effectiveness of Person-centred Care of elderly in nursing homes and home care services | Person-centred Care associated with positive impact on well-being, mental and physical health, and QOL. | (Byrne et al. 2012; Edvardsson et al. 2017; Wilberforce et al. 2017) |
| 5 | Barriers and facilitators for the implementation of Person-centred Care | Organisational conditions such as culture, structures, processes, leadership, and HR practices that facilitate or hinder implementation of Person-centred Care | (Braithwaite et al. 2017; Cho et al. 2016; Moore et al. 2017; Ree 2020) |
References
- Aryana, I. G. P. Suka, and R. A. Tuty Kuswardhani. 2018. Sarcopenia in elderly. International Journal of Geriatrics and Gerontology 1: 1–4. [Google Scholar] [CrossRef]
- Atchley, Robert C. 1989. A continuity theory of normal aging. The Gerontologist 29: 183–90. [Google Scholar] [CrossRef] [PubMed]
- Baker, David C. 2003. Studies of the inner life: The impact of spirituality on quality of life. Quality of Life Research 12: 51–57. [Google Scholar] [CrossRef] [PubMed]
- Baltes, Paul B, and Margret M. Baltes. 1990. Successful Ageing: Perspectives from the Behavioural Sciences. Cambrideg: Cambrideg University Press. [Google Scholar] [CrossRef]
- Barbosa, Ana, Liliana Sousa, Mike Nolan, and Daniela Figueiredo. 2015. Effects of person-centered care approaches to dementia care on staff: A systematic review. American Journal of Alzheimer’s Disease & Other Dementias® 30: 713–22. [Google Scholar] [CrossRef] [Green Version]
- Basu, Radha. 2016. Safe but soulless. Lien Foundation. Available online: https://www.lienfoundation.org (accessed on 15 December 2020).
- Borkovec, Thomas D. 1988. Comments on “Worry as a phenomenon relevant to the elderly”. Behavior Therapy 19: 381–83. [Google Scholar] [CrossRef]
- Bowers, Helen, Angela Clark, Gilly Crosby, Lorna Easterbrook, Alison Macadam, Rosemary MacDonald, Ann Macfarlane, Mairi Maclean, Meena Patel, Dorothy Runnicles, and et al. 2009. Older People’s Vision for Long-Term Care. York: Joseph Rowntree Foundation. [Google Scholar]
- Braithwaite, Jeffrey, Jessica Herkes, Kristiana Ludlow, Luke Testa, and Gina Lamprell. 2017. Association Between Organisational and Workplace Cultures, and Patient Outcomes: Systematic Review. BMJ Open 7: e017708. [Google Scholar] [CrossRef] [Green Version]
- Braun, Virginia, and Victoria Clarke. 2006. Using thematic analysis in psychology. Qualitative Research in Psychology 3: 77–101. [Google Scholar] [CrossRef] [Green Version]
- Braun, Virginia, and Victoria Clarke. 2019. Reflecting on reflexive thematic analysis. Qualitative Research in Sport, Exercise and Health 11: 589–97. [Google Scholar] [CrossRef]
- Braun, Virginia, and Victoria Clarke. 2021. One size fits all? What counts as quality practice in (reflexive) thematic analysis? Qualitative Research in Psychology 18: 328–52. [Google Scholar] [CrossRef]
- Brownie, Sonya, and Susan Nancarrow. 2013. Effects of person-centered care on residents and staff in aged-care facilities: A systematic review. Clinical Interventions in Aging 8: 1. [Google Scholar] [CrossRef] [Green Version]
- Byrne, Kerry, Krista Frazee, Joanie Sims-Gould, and Anne Martin-Matthews. 2012. Valuing the older person in the context of delivery and receipt of home support: Client perspectives. Journal of Applied Gerontology 31: 377–401. [Google Scholar] [CrossRef]
- Carstensen, Laura L., Susanne Scheibe, Hal Ersner-Hershfield, Kathryn P. Brooks, Bulent Turan, Nilam Ram, Gregory R. Samanez-Larkin, and John R. Nesselroade. 2011. Emotional Experience Improves With Age: Evidence Based on Over 10 Years of Experience Sampling. Psychology and Aging 26: 21–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chaturvedi, Santosh K., and Krishna Prasad Muliyala. 2016. The Meaning in Quality of Life. Journal of Psycho Social Rehabilitation and Mental Health 3: 47–49. [Google Scholar] [CrossRef] [Green Version]
- Chinnakkaruppan, Adaikkan, Marie E. Wintzer, Thomas J. McHugh, and Kobi Rosenblum. 2014. Differential Contribution of Hippocampal Subfields to Components of Associative Taste Learning. The Journal of Neuroscience 34: 11007–15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cho, Eunhee, Nam-Ju Lee, Eun-Young Kim, Sinhye Kim, Kyongeun Lee, Kwang-Ok Park, and Young Hee Sung. 2016. Nurse staffing level and overtime associated with patient safety, quality of care, and care left undone in hospitals: A cross-sectional study. International Journal of Nursing Studies 60: 263–71. [Google Scholar] [CrossRef] [PubMed]
- Cohen, Marlene Zichi, David L. Kahn, and Richard H. Steeves. 2000. Hermeneutic Phenomenological Research: A Practical Guide for Nurse Researchers. Thousand Oaks: Sage Publications, Inc. [Google Scholar] [CrossRef]
- Creswell, John W. 2007. Qualitative Inquiry and resEarch Design: Choosing among Five Approaches, 2nd ed. Thousand Oaks: Sage Publications, Inc. [Google Scholar]
- Department of Statistics Singapore. 2021. Population Trends. SingStat Website. Available online: https://www.singstat.gov.sg/publications/population-trends (accessed on 18 March 2022).
- Dorner, T. E., Eva Luger, J. Tschinderle, K. V. Stein, S. Haider, A. Kapan, C. Lackinger, and K. E. Schindler. 2014. Association between nutritional status (MNA®-SF) and frailty (SHARE-FI) in acute hospitalised elderly patients. The Journal of Nutrition, Health & Aging 18: 264–69. [Google Scholar] [CrossRef]
- Doyle, Cathal, Laura Lennox, and Derek Bell. 2013. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open 3: e001570. [Google Scholar] [CrossRef]
- Edvardsson, David, Karin Sjögren, Qarin Lood, Ådel Bergland, Marit Kirkevold, and Per-Olof Sandman. 2017. A person-centred and thriving-promoting intervention in nursing homes-study protocol for the U-Age nursing home multi-centre, non-equivalent controlled group before-after trial. BMC Geriatrics 17: 1–9. [Google Scholar] [CrossRef] [Green Version]
- Edvardsson, David, P. O. Sandman, and Lena Borell. 2014. Implementing national guidelines for person-centered care of people with dementia in residential aged care: Effects on perceived person-centeredness, staff strain, and stress of conscience. International Psychogeriatrics 26: 1171–79. [Google Scholar] [CrossRef] [Green Version]
- Engel, George L. 1977. The need for a new medical model: A challenge for biomedicine. Science 196: 129–36. [Google Scholar] [CrossRef]
- Fisher, John W. 2001. Comparing Levels of Spiritual Well-Being in State, Catholic and Independent Schools in Victoria, Australia. Journal of Beliefs and Values 22: 99–105. [Google Scholar] [CrossRef]
- Fisher, John W. 2011. The Four Domains Model: Connecting Spirituality, Health and Well-Being. Religions 2: 17–28. [Google Scholar] [CrossRef]
- Fors, Andreas, Inger Ekman, Charles Taft, Cecilia Björkelund, Kerstin Frid, Maria E. H. Larsson, Jörgen Thorn, Kerstin Ulin, Axel Wolf, and Karl Swedberg. 2015. Person-centred care after acute coronary syndrome, from hospital to primary care—a randomised controlled trial. International Journal of Cardiology 187: 693–99. [Google Scholar] [CrossRef] [PubMed]
- Frankl, Viktor. 1962. Man’s Search for Meaning, trans. Ilse Lasch, rev. ed. New York: Simon and Schuster, vol. 65, p. 22. [Google Scholar]
- Gabriel, Zahava, and A. N. N. Bowling. 2004. Quality of life from the perspectives of older people. Ageing & Society 24: 675–91. [Google Scholar] [CrossRef] [Green Version]
- Giele, Janet Z., and Glen H. Elder Jr., eds. 1998. Methods of Life Course Research: Qualitative and Quantitative Approaches. Thousand Oaks: Sage Publications, Inc., ISBN 0 761914374. [Google Scholar]
- Goh, Lee Gan, Ee Heok Kua, and Hai Ding Chiang. 2015. Ageing in Singapore: The Next 50 Years. Singapore: Spring Publishing Pte Ltd. [Google Scholar]
- Goldfarb, Michael J., Lior Bibas, Virginia Bartlett, Heather Jones, and Naureen Khan. 2017. Outcomes of patient-and family-centered care interventions in the ICU: A systematic review and meta-analysis. Critical Care Medicine 45: 1751–61. [Google Scholar] [CrossRef] [PubMed]
- Granier, Katie L., and Daniel L. Segal. 2021. Diverse Aspects of Worry among Younger and Older Adults: A Multifaceted Approach. Psychology 12: 441. [Google Scholar] [CrossRef]
- Gray, Rossarin Soottipong, Pungpond Rukumnuaykit, Sirinan Kittisuksathit, and Varachai Thongthai. 2008. Inner Happiness Among Thai Elderly. Journal of Cross-Cultural Gerontology 23: 211–24. [Google Scholar] [CrossRef]
- Hirschmann, Raudhah. 2020. Forecasted Share of the Population Aged 65 Years and above in Singapore in 2019, 2030 and 2050. Statista. Available online: https://www.statista.com/statistics/713663/singapore-forecast-ageing-population/ (accessed on 18 March 2022).
- Hohls, Johanna Katharina, Hans-Helmut König, Eleanor Quirke, and André Hajek. 2019. Association between anxiety, depression and quality of life: Study protocol for a systematic review of evidence from longitudinal studies. BMJ Open 9: e027218. [Google Scholar] [CrossRef]
- Iwarsson, Susanne, and Agneta Ståhl. 2003. Accessibility, usability and universal design—positioning and definition of concepts describing person-environment relationships. Disability and Rehabilitation 25: 57–66. [Google Scholar] [CrossRef]
- Katz, Jeanne, Caroline Holland, Sheila Peace, and Emily Taylor. 2011. A Better Life-What Older People with High Support Needs Value. York: Joseph Rowntree Foundation, Available online: www.jrf.org.uk/publications/older-people-high-suppport-needs.full.pdf (accessed on 15 December 2020).
- Kim, Sun Kyung, and Myonghwa Park. 2017. Effectiveness of person-centered care on people with dementia: A systematic review and meta-analysis. Clinical Interventions in Aging 12: 381. [Google Scholar] [CrossRef] [Green Version]
- Kitwood, Thomas Marris. 1997. Dementia Reconsidered: The Person Comes First. Buckingham: Open University Press, vol. 20. [Google Scholar]
- Koenig, Harold G. 2012. Religion, Spirituality, and Health: The Research and Clinical Implications. ISRN Psychiatry 2012: 278730–33. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lawton, M. Powell, and Lucille Nahemow. 1973. Ecology and the aging process. In The Psychology of Adult Development and Aging. Washington, DC: American Psychological Association, pp. 619–74. [Google Scholar] [CrossRef]
- Leedy, Paul D., and Jeanne Ellis Ormrod. 2001. Practical Research: Planning and Design, 7th ed. Hoboken: Merrill Prentice Hall. [Google Scholar]
- Leplege, Alain, Fabrice Gzil, Michele Cammelli, Celine Lefeve, Bernard Pachoud, and Isabelle Ville. 2007. Person-centredness: Conceptual and historical perspectives. Disability and Rehabilitation 29: 1555–65. [Google Scholar] [CrossRef] [PubMed]
- Lowther, Keira, Richard Harding, Victoria Simms, Aabid Ahmed, Zipporah Ali, Nancy Gikaara, Lorraine Sherr, Hellen Kariuki, Irene J. Higginson, and Lucy Ellen Selman. 2018. Active ingredients of a person-centred intervention for people on HIV treatment: Analysis of mixed methods trial data. BMC Infectious Diseases 18: 1–9. [Google Scholar] [CrossRef] [Green Version]
- MacKinlay, Elizabeth. 2021. Ageing and frailty: A spiritual perspective of the lived experience. Journal of Religion, Spirituality & Aging 33: 236–49. [Google Scholar] [CrossRef]
- Marques, M., Ana Faria, and Marisa Cebola. 2019. Body mass index and body composition in institutionalized older adults with malnutrition, sarcopenia and frailty. European Journal of Public Health 29: ckz034-070. [Google Scholar] [CrossRef]
- McCormack, Brendan, Jan Dewing, and Tanya Mccance. 2011. Developing person-centred care: Addressing contextual challenges through practice development. Online Journal of Issues in Nursing 16: 1–12. [Google Scholar] [CrossRef]
- Minney, Melissa J., and Rob Ranzijn. 2016. “We Had a Beautiful Home… But I Think I’m Happier Here”: A Good or Better Life in Residential Aged Care. The Gerontologist 56: 919–27. [Google Scholar] [CrossRef] [Green Version]
- Moore, Lucy, Nicky Britten, Doris Lydahl, Öncel Naldemirci, Mark Elam, and Axel Wolf. 2017. Barriers and facilitators to the implementation of person-centred care in different healthcare contexts. Scandinavian Journal of Caring Sciences 31: 662–73. [Google Scholar] [CrossRef]
- Pargament, Kenneth I. 2001. The Psychology of Religion and Coping: Theory, Research, Practice. New York: The Guilford Press. [Google Scholar]
- Pattison, Stephen, Ben Hannigan, and Roisin Pill. 2010. Emerging Values in Health Care: The Challenge for Professionals. Philadelphia: Jessica Kingsley Publishers. [Google Scholar]
- Potter, Charlotte. 2009. What quality healthcare means to older people: Exploring and meeting their needs. Nursing Times 105: 14–18. [Google Scholar]
- Puchalski, Christina M. 2008. Spirituality and the Care of Patients at the End-of-Life: An Essential Component of Care. OMEGA Journal of Death and Dying 56: 33–46. [Google Scholar] [CrossRef] [Green Version]
- Puchalski, Christina, Betty Ferrell, Rose Virani, Shirley Otis-Green, Pamela Baird, Janet Bull, Harvey Chochinov, George Handzo, Holly Nelson-Becker, Maryjo Prince-Paul, and et al. 2009. Improving the Quality of Spiritual Care as a Dimension of Palliative Care: The Report of the Consensus Conference. Journal of Palliative Medicine 12: 885–904. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ree, Eline. 2020. What is the role of transformational leadership, work environment and patient safety culture for person-centred care? A cross-sectional study in Norwegian nursing homes and home care services. Nursing Open 7: 1988–96. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, Oscar, Laetitia Teixeira, Lia Araújo, Carmen Rodríguez-Blázquez, Amaia Calderón-Larrañaga, and Maria João Forjaz. 2020. Anxiety, depression and quality of life in older adults: Trajectories of influence across age. International Journal of Environmental Research and Public Health 17: 9039. [Google Scholar] [CrossRef] [PubMed]
- Rinnan, Eva, Beate André, Jorunn Drageset, Helge Garåsen, Geir Arild Espnes, and Gørill Haugan. 2018. Joy of life in nursing homes: A qualitative study of what constitutes the essence of joy of life in elderly individuals living in Norwegian nursing homes. Scandinavian Journal of Caring Sciences 32: 1468–76. [Google Scholar] [CrossRef] [Green Version]
- Rogers, Carl Ransom. 1961. On Becoming a Person: A Therapist’s View of Psychotherapy. Boston: Houghton Mifflin Harcourt. [Google Scholar]
- Saguil, Aaron, and Karen Phelps. 2012. The spiritual assessment. American Family Physician 86: 546–50. [Google Scholar]
- Sousa, Rute Dinis de, Ana Maria Rodrigues, Maria João Gregório, Jaime Da Cunha Branco, Maria João Gouveia, Helena Canhão, and Sara Simões Dias. 2017. Anxiety and depression in the Portuguese older adults: Prevalence and associated factors. Frontiers in Medicine 4: 196. [Google Scholar] [CrossRef]
- Tew, Chee-Wee, Siew Pei Ong, Philip Lin Kiat Yap, Amber Yew Chen Lim, Nan Luo, Gerald C. H. Koh, Tze Pin Ng, and Shiou Liang Wee. 2021. Quality of Life, Person-Centred Care and Lived Experiences of Nursing Home Residents in A Developed Asian Urban Country: A Cross-Sectional Study. The Journal of Nursing Home Research 7: 1–8. [Google Scholar] [CrossRef]
- Thomas, William H. 2003. Evolution of Eden. Journal of Social Work in Long-Term Care 2: 141–57. [Google Scholar] [CrossRef]
- Tornstam, Lars. 1997. Gerotranscendence: The contemplative dimension of aging. Journal of Aging Studies 11: 143–54. [Google Scholar] [CrossRef]
- Ulin, Kerstin, Lars-Eric Olsson, Axel Wolf, and Inger Ekman. 2016. Person-centred care–An approach that improves the discharge process. European Journal of Cardiovascular Nursing 15: e19–e26. [Google Scholar] [CrossRef]
- van Manen, Max. 1990. Researching Lived Experience: Human Science for an Action Sensitive Pedagogy. Albany: University New York Press. [Google Scholar]
- Waaijman, Kees. 2007. Spirituality-A multifaceted phenomenon: Interdisciplinary explorations. Studies in Spirituality 17: 1–113. [Google Scholar] [CrossRef] [Green Version]
- Wang, Pei, Philip Yap, Gerald Koh, Jia An Chong, Lucy Jennifer Davies, Mayank Dalakoti, Ngan Phoon Fong, Wei Wei Tiong, and Nan Luo. 2016. Quality of life and related factors of nursing home residents in Singapore. Health and Quality of Life Outcomes 14: 1–9. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wee, Shiou-Liang, Athel J. Hu, Joel Yong, Wayne F. Chong, Prassanna Raman, and Angelique Chan. 2015. Singaporeans’ perceptions of and attitudes toward long-term care services. Qualitative Health Research 25: 218–27. [Google Scholar] [CrossRef] [PubMed]
- Werngren-Elgström, Monica, Gunilla Carlsson, and Susanne Iwarsson. 2009. A 10-year follow-up study on subjective well-being and relationships to person–environment (P–E) fit and activity of daily living (ADL) dependence of older Swedish adults. Archives of Gerontology and Geriatrics 49: e16–e22. [Google Scholar] [CrossRef] [Green Version]
- White, Diana L., Linda Newton-Curtis, and Karen S. Lyons. 2008. Development and initial testing of a measure of person-directed care. The Gerontologist 48: 114–23. [Google Scholar] [CrossRef] [Green Version]
- Wilberforce, Mark, David Challis, Linda Davies, Michael P. Kelly, Chris Roberts, and Paul Clarkson. 2017. Person-centredness in the community care of older people: A literature-based concept synthesis. International Journal of Social Welfare 26: 86–98. [Google Scholar] [CrossRef] [Green Version]
- Williamson, Toby. 2010. My Name Is Not Dementia: People with Dementia Discuss Quality of Life Indicators. London: Alzheimer’s Society. [Google Scholar]
- World Health Organisation (WHO). 2022. “Malnutrition”. WHO Website. Available online: https://www.who.int/news-room/questions-and-answers/item/malnutrition (accessed on 18 March 2022).
| Name of Resident | Gender | Ethnicity | Length of Stay |
|---|---|---|---|
| Nursing Home A | |||
| A1 | Female | Indian | 3–5 years |
| A2 | Male | Chinese | 1–2 years |
| A3 | Male | Chinese | 1–2 years |
| A4 | Male | Chinese | 1–2 years |
| A5 | Male | Chinese | >5 years |
| Nursing Home B | |||
| B1 | Female | Chinese | 3–5 years |
| B2 | Female | Chinese | >5 years |
| B3 | Male | Chinese | 3–5 years |
| B4 | Male | Chinese | 1–2 years |
| B5 | Male | Eurasian | 3–5 years |
| Nursing Home C | |||
| C1 | Male | Chinese | >5 years |
| C2 | Male | Chinese | 1–2 years |
| C3 | Male | Chinese | 1–2 years |
| C4 | Male | Indian | 3–5 years |
| C5 | Male | Indian | 3–5 years |
| C6 | Male | Malay | 3–5 years |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dayanandan, S.; Mehta, K. What Does Joy in Living Mean to Elderly Residents of Nursing Homes in Singapore? Religions 2022, 13, 469. https://doi.org/10.3390/rel13050469
Dayanandan S, Mehta K. What Does Joy in Living Mean to Elderly Residents of Nursing Homes in Singapore? Religions. 2022; 13(5):469. https://doi.org/10.3390/rel13050469
Chicago/Turabian StyleDayanandan, Swapna, and Kalyani Mehta. 2022. "What Does Joy in Living Mean to Elderly Residents of Nursing Homes in Singapore?" Religions 13, no. 5: 469. https://doi.org/10.3390/rel13050469
APA StyleDayanandan, S., & Mehta, K. (2022). What Does Joy in Living Mean to Elderly Residents of Nursing Homes in Singapore? Religions, 13(5), 469. https://doi.org/10.3390/rel13050469







