Abstract
Attention has been given to the experience of individuals undergoing assisted reproductive techniques. However, only recent literature has focused on the spiritual journey triggered by such an event and highlighted the nurses and midwives’ roles in the assessment of the spiritual needs of those living with infertility. This study aimed to perform a psychometric test of the factor structure of the Portuguese version of the Spiritual Well-being Questionnaire in a sample of people undergoing assisted reproductive techniques. This descriptive cross-sectional study was conducted between September 2019 and June 2020 on a sample of 104 Portuguese adults attending fertility treatment. An online questionnaire was released on fertility-related websites. A confirmatory factor analysis was conducted on six hypothesized models of the instrument. The findings provided evidence of an adequate internal consistency of the instrument, and the validity and reliability of the oblique four-factor model was confirmed. Spiritual well-being had a significant association with the nature of infertility and a higher score was achieved by participants that perceived religion as very important. This study provides a validated tool for nurses and midwives to assess spiritual well-being and promote an integrated reproductive healthcare approach. Further longitudinal research with bigger samples would provide more evidence of the spiritual needs of people living with this condition.
1. Introduction
The International Glossary on Infertility and Fertility Care defines infertility as a disease caused by a failure to successfully achieve a clinical pregnancy in 12 months of regular sexual intercourse without the use of any birth control method or as a result of an impaired capacity of a person or a couple to reproduce (Zegers-Hochschild et al. 2017). This health condition is recognized as a public health issue due to its wide impact and was estimated to have affected 48.5 million couples worldwide in 2010 (Centers for Disease Control and Prevention 2014; Mascarenhas et al. 2012; Roudsari et al. 2007).
Early studies identified a profound effect of infertility in the physical, psychological, social, and spiritual dimensions of a human being. Meanwhile, infertility forces the individual to face an uncertain path towards parenthood, along with extensive, expensive, exhaustive, and demanding treatment protocols (Romeiro et al. 2017a, 2017b).
The exponential growth of assisted reproductive techniques (ART) reflects the increased requests for treatment. This poses the need for addressing such healthcare demands and for integrating a more spiritual-focused perspective that is critical for a holistic and patient-centered approach (Romeiro et al. 2017b; Romeiro and Caldeira 2020).
Spirituality is described as “a way of being in the world in which a person feels a sense of connectedness to self, others, and/or a higher power or nature; a sense of meaning in life; and transcendence beyond self, everyday living, and suffering” (Weathers et al. 2016, p. 15). Recently, a systematic, qualitative review synthesized the spiritual aspects of those living with infertility, such as transcendence, connectedness, and meaning in life (Romeiro et al. 2017b). Earlier, Etemadifar and collaborators (Etemadifar et al. 2016) uncovered a positive relationship between spiritual well-being (existential and religious dimensions) and life satisfaction in women with infertility. Yet, evidence remains scarce relating both spirituality and the experience of living with infertility (Romeiro and Caldeira 2020).
A timely assessment could provide a deeper understanding of individuals’ spiritual needs and an early intervention capable of supporting the journey could increase the quality of life, evoke compliance, and prevent fertility treatment desertion (Romeiro et al. 2017a; Romeiro and Caldeira 2018b). In fact, there is a fertile ground for the provision of spiritual care in this setting, and previous studies have emphasized the importance of nurses’ roles (Caldeira et al. 2019b; Romeiro and Caldeira 2018b).
Seeking instruments to measure spiritual well-being in different healthcare contexts is not new, but an approach to early-life events such as infertility is quite innovative (Caldeira et al. 2019a; Romeiro et al. 2017b; Romeiro and Caldeira 2018a).
A valid instrument is a critical condition for nursing assessment and diagnosis, as it is for planning and implementing nursing interventions and achieving positive health outcomes (Alfaro-LeFevre 2012; Caldeira et al. 2019b; Romeiro and Caldeira 2018b). In addition, these are essential for the effective spiritual and self-healing process of individuals during fertility treatments (Caldeira et al. 2019a).
The Spiritual Well-Being Questionnaire (SWBQ), originally developed by Gomez and Fisher (2003, 2005a, 2005b), is an instrument commonly used to identify the four domains of spiritual health (personal, communal, environmental, and transcendental) (Fisher 2010). The SWBQ was based on Fisher’s theoretical assumptions about the spiritual well-being concept (Fisher 1998) and it is the “lived-experience” component of the Spiritual Health And Life-Orientation Measure (SHALOM). The SWBQ was first tested on Australian teachers and students (Gomez and Fisher 2003, 2005a, 2005b), with good original reliability and a Cronbach’s alpha of between 0.76 and 0.95 (Gomez and Fisher 2003, 2005b). This instrument has been improved over the years and validated in different settings and countries. Currently, it includes 20 items, with levels of response ranging from one (“very low”) to a maximum of five (“very high”) on a five-point Likert scale. The personal domain relates to self-awareness, meaning, purpose, and one’s own values. On the other hand, the communal component explores relationships with others and with morality, culture, and religion. The environmental domain accounts for connection with nature and one’s surroundings. Finally, the transcendental domain refers to a relationship with a higher entity (God, a cosmic force, the supernatural, a higher power, or the universe), beyond the physical experiences. Each domain contains five items to be answered by participants based on how they perceive it. The scores represent the levels of spiritual well-being (SWB) per domain (Fisher et al. 2000; Gouveia et al. 2009), and the total mean of all domains reveals a global SWB measure (Gouveia et al. 2009). Respondents’ spiritual health is expressed by the positive relationship to each of the domains as more domains are included (Fisher et al. 2000). In fact, there is a dynamic retroaction named ‘positive synergism’ in which the quality of relationships in one domain enhances the others (Fisher et al. 2000). Yet, higher scores do not necessarily imply SWB, but rather a dispositional measure of an individual towards it (Gouveia 2011).
The SWBQ has been previously considered suitable for implementation in clinical nursing practice in comparison to other available spirituality tools (de Jager Meezenbroek et al. 2012) because of its benefits as an easy and short administration that is not restricted to religious features (Fisher 2010).
The SWBQ was the target of cultural and Portuguese language adaptation by Gouveia and collaborators (2009). The same authors originally validated the instrument in a sample of 439 Portuguese adults from the general population (Gouveia et al. 2009). Afterwards, this Portuguese version of the SWBQ (SWBQp) was used in other studies, frequently for academic purposes, and mainly in individuals with cancer (Caldeira et al. 2017a, 2017b). Satisfactory results proposed a four-factor structure to be the best fit in several samples, although with some inconsistency in the elderly (Caldeira et al. 2014; Neves et al. 2017; Rodrigues 2013). In addition, calls to test its equivalent validity in distinct ages were released (Gomez and Fisher 2005b), along with growing interest in spiritual research in people with non-terminal illness (Romeiro et al. 2018; Romeiro and Caldeira 2018a). In fact, a synthesis of Portuguese studies about people living with infertility highlighted the absence of evidence beyond the psychosocial aspects of having such a reproductive condition (Romeiro and Caldeira 2018a).
Despite its wide use in research, to date, no published studies were found that confirmed the factor structure of SWBQp in an adult Portuguese sample going through fertility treatment. This will bring stronger confidence in the validity of the results and increase nurses’ awareness of SWB when caring for individuals having a fertility condition, and it will serve as a facilitator in overcoming barriers to the provision of preconception care.
Therefore, the purpose of this study was to validate and to test the factor structure of the SWBQp by using confirmatory factor analysis (CFA) in a sample of people going through assisted reproductive technologies. This article also provides results not only for the SWB construct, but for its association with some sociodemographic and clinical factors in terms of the reproductive health of the sample.
2. Materials and Methods
2.1. Research Design
Descriptive cross-sectional design was conducted between September 2019 and June 2020.
2.2. Participants
A non-probabilistic sample of people with internet access was included. The inclusion criteria were: (1) adult men and women (aged 18 years or older); (2) Portuguese nationality; (3) in the process of engaging or during any stage of a fertility treatment; (4) willing to participate in this study; (5) agreed and signed an electronic informed consent. Incomplete questionnaires were excluded.
Considering that psychometric tests appeal to participants that exceed three times the number of items in the analysis (Kline 2000), a minimum of 60 individuals to take part in this study was required. A sample-size with a ratio equal to or higher than 5 or equal to and higher than 10 by each variable of the model with a minimum of 200 individuals is widely implemented (Myers et al. 2011). Nevertheless, while other authors defend broader samples, some are more cautious and defend that sample size restrictions may be overcome under the use of a measurement instrument already validated in a resembling population (Knekta et al. 2019), as is the case of the SWBQp, which has been validated in several samples of the Portuguese adult population. Moreover, a sample size of 100 would yield a sampling error of 10 percent at the 95 percent confidence level, compared with the slightly lower 7 percent sampling error if 200 respondents were sought/used.
Recruitment took place through online invitations on fertility-related websites. This involved the release of periodical advertisements with potential participants asked to access a web-based questionnaire by clicking on an electronic link, which directed them to the informed consent of the study.
The final sample of this research comprised 104 individuals.
2.3. Data Collection
A web-based survey was designed using Google Forms for online surveys (Google 2019). Individuals were asked to answer questions including demographic information (gender, age, marital situation, location, educational level, and occupation) and spiritual and religious beliefs, as well as clinical health data (the type of infertility, nature, time trying to conceive, time of infertility diagnosis, and duration of fertility assistance) and details about fertility treatments (time on treatment, previous treatments, phase, type, and time on current treatment).
The measure of SWB was calculated in each of the four subscales of the SWBQp. The measure of SWB was calculated through the mean of the scores obtained per item assigned to each subscale. It was also possible to assess a global SWB from the addition of the domains scores (Fisher et al. 2000; Gouveia et al. 2009).
The total Cronbach’s alpha (α) of the first SWBQp version was 0.89 (Gouveia et al. 2009) and ranged between 0.74 and 0.88 (personal domain α = 0.75; communal domain α = 0.74; environmental domain α = 0.84; and transcendental domain α = 0.89). These measures were similar to the SWBQ English version (α = 0.76–0.95) (Gomez and Fisher 2003, 2005a, 2005b).
The length of time estimated for completion of the SWBQp was 10 to 15 minutes, including the time of browsing the specified website. This part of the study was carried out in two phases. Phase 1 included a pilot study previously reviewed by nursing experts before data collection to identify possible computer survey errors and test the content validity and comprehensiveness of the tool. Afterwards, 30 participants were asked to complete the questionnaire, which was available for 3 months (March to July 2019), to evaluate the feasibility of the study design and protocol. A final version of the survey was achieved and implemented in Phase 2 (September 2019 to June 2020). Data were stored in a private access Microsoft Excel 2020 file (Microsoft 2020).
2.4. Ethical Considerations
This study was approved by the Ethics Committee of The Institute of Health Sciences of Universidade Católica Portuguesa. The research ethics clearance certificate is dated 13 March 2019.
Participants were informed about the purpose, methodology, duration, risks, and benefits of the study. In addition, anonymity and confidentiality were guaranteed to participants. Individuals interested in participating gave informed consent through an electronic, online positive answer that was required to access the questionnaire. Additionally, participants were informed of the voluntary nature of the survey and about the option to refuse or quit at any time, with the assured statement that no negative outcomes would result from it or would influence their medical treatment and/or care. It was clearly stated that the research was not related to any health care institution. Due to the nature and sensitivity of the theme, counseling was facilitated to participants through resources provided by The Portuguese Fertility Association.
All data will be kept in a restricted access computer file for a period that will not exceed five years after research is terminated. Researchers assured that only the authors would have access to the data through a password only held by them. Permission to use findings and conclusions for academic purposes, namely thesis presentation and scientific papers, was given in the consent form.
2.5. Data Analysis
Statistical analyses were carried out using SPSS version 26.0 (IBM 2018).
Descriptive statistics were performed for demographic and clinical data. Frequency and percentage described categorical variables, and mean and standard deviation (SD) were used for continuous variables. Since all participants gave complete answers, there were no missing values, and no cases were therefore removed.
The 20 items of the SWBQp were subjected to preliminary data checks to confirm their suitability in further analysis. The variables were screened using skewness and kurtosis to gather information about the distribution of the data. This information was used in the parametric statistic techniques applied. Furthermore, the independent sample t-tests and the one-way ANOVA were used to detect differences in SWBQp means between the subgroups of our sample (Table 1) following Pestana and Gageiro’s (2003) assumptions of data normality in samples with 30 or more participants.

Table 1.
Characteristics of participants and mean scores of the SWBQ (N = 104).
Cronbach’s alpha was used to assess the internal consistency of the instrument and a value of more than 0.70 was considered acceptable (Nunnally and Bernstein 1994).
The suitability of using factor analysis was obtained through Bartlett’s Test of Sphericity (p < 0.05) (Hair et al. 2010) and the Kaiser–Meyer–Olkin (KMO) sampling adequacy test (recommended minimum value of 0.6) (Tabachnick and Fidell 2007).
A CFA was performed, taking into consideration the general rule that there was previous knowledge related to what was intended to be measured (Babyak and Green 2010); in this case, the intention to measure six versions of the high-factor, multidimensional SWBQ model. Previous researchers had performed exploratory factor analysis (EFA) on SWBQp, supporting the proposed model, and so CFA seemed to be the most suitable factor analysis in this case, following the recommendations of Knekta and colleagues (2019). Analysis of the factor structure of the SWBQp was conducted using AMOS SPSS (Analysis of Moment Structures) version 26.0 (IBM 2018), following Byrne’s (Byrne 2010) references.
Four versions of the SWBQp model were previously proposed by Gomez and Fisher (2003), and two other modified four-factor oblique models were based on the early results of Gouveia and collaborators (2009). In Model 1 (the four-factor oblique model), it was estimated that items would load on four first-order factors correlated with each other (Gomez and Fisher 2003). Under a similar structure, in Model 2 (a modified four-factor oblique), items 6, 8, and 9 were excluded (Gouveia et al. 2009). Model 3 was a modified four-factor oblique structure without items 8, 9, and 15 (Gouveia et al. 2012). Model 4 was a four-factor orthogonal model where all four first-order factors were considered independent from each other (Gomez and Fisher 2003). Meanwhile, a one-factor, first-order model (Model 5) where all 20 items would load reliably on a single first-order factor (the SWB) was also considered for CFA (Gomez and Fisher 2003). Lastly, in Model 6, it was estimated that four first-order orthogonal factors would be explained by one single higher-order SWB factor (a hierarchical second-order model) (Gomez and Fisher 2003).
The implementation of CFA helps researchers to identify to what extent the data collected through the instrument supports and confirms the hypothesized model (already based on knowledge of theory and/or empirical research, or both), as well as how different items and factors relate with each other (Knekta et al. 2019). In the identification of the model, it was assumed that each observable variable (item/question) would load exclusively on the factor it was intended to measure.
A high factor structure would be considered inadequate by the researchers if standardized factor loadings were not equal to or higher than 0.60 (Awang 2012).
The assessment of the fitness index comprised three categories: parsimonious fit, absolute fit, and incremental fit. Indeed, AMOS provides several models of fit, and researchers are encouraged to use at least one fitness index from each category (Afthanorhan 2013). To assess the fit of the SWBQp models, an estimation of maximum likelihood with a chi-square statistic (X2) was performed (Winters et al. 2010; Alavi et al. 2020). In this study, the differences between the X2 tests of the SWBQp models were analyzed. Usually, X2 is applied as an absolute fit index (Alavi et al. 2020), and given the fact that it is affected by large samples, researchers opt for the analysis of the ratio of X2 to the respective degrees of freedom (X2/df), which is known as a parsimonious fit (Marsh and Hocevar 1985). An X2/df ratio of lower than 3 is considered a good fit (Hu and Bentler 1998).
Furthermore, the absolute fit was tested with RMSEA (root-mean-square error of approximation) and SRMR (standardized root-mean-square residual), and the incremental fit index was tested with CFI (comparative fit index). Desirable values were associated with a satisfactory structure of the model: an SRMR below 0.09; a CFI greater than 0.90–0.95; and RMSEA values of 0.01 (excellent fit), below 0.05 (good fit), lower than 0.08 (good fit), between 0.05–0.10 (moderate fit), and higher than 0.10 (bad fit) (Awang 2012; Hooper et al. 2008; Hu and Bentler 1998).
Afterwards, a closer look at the model with the better fit to the data was given through analysis of factor loadings, correlational residuals, and modification indices (MI). An MI over 15 would reflect a high multicollinearity problem (Awang 2012).
After construct validity was indicated by fitness indexes, for determination of how good the items were in measuring their respective latent constructs, convergent and discriminant validity were assessed using CFA (Awang 2012; Campbell and Fiske 1959). Convergent validity was verified using average variance extracted (AVE) (a recommended value of > 0.5) (Hair et al. 2010). Discriminant validity required that the correlation between exogenous constructs didn’t go over 0.85. If the correlation value went over 0.85, this demonstrated that the two constructs were redundant or had a multicollinearity issue (MSV < AVE; ASV < AVE). MSV related to maximum shared variance and ASV related to average shared variance (Awang 2012).
If discriminant validity issues were detected, variables correlated more highly with other variables outside the factor than with variables included in the same factor. If there were convergent validity problems, then the variables did not correlate well with each other within the factor they shared. This meant that the latent factor was not well explained by the variables (Awang 2012).
Reliability was assessed by means of Cronbach’s alpha (>0.7), composite reliability (CR) (recommended CR ≥ 0.6), and AVE (recommended > 0.5) (Awang 2012). CR and AVE were calculated based on the formula of Hair and collaborators (Hair et al. 2010).
3. Results
3.1. Sample Characteristics
One hundred and four individuals undergoing fertility treatment participated in this study. Results of the social, demographic, and clinical data are presented in Table 1.
Briefly, the participants were predominantly female (98.1%), the mean age was 35.4 (SD = 4.8; 95% CI = 34.49–36.34), though age ranged from 26 to 54 years old (Table 1), and participants were living in the north of Portugal (33.3%). Over half (57.7%) were married and in a relationship for at least one year and had spent a maximum of 22 years together, with a mean time of living together for 7.97 years (SD = 4.80; 95% CI = 7.03–8.91). Most had a high education level (65.4%), were employed (87.5%), and were intellectual and scientific experts (35.6%).
In general, 76% of the individuals identified themselves as being spiritual, and about 67.3% reported to be religious, although only 56.7% had a religious affiliation and most were Catholic (87.0%). Furthermore, most participants felt no change in their spirituality during the diagnosis of infertility (50.0%) or treatment (51.0%). On the other hand, religion changed, becoming less important when infertility was diagnosed (26.9%), but gained an increased significance during treatment (31.7%). Regarding clinical data, the primary form of infertility predominated in the sample (86.5%) and most individuals described they had never been pregnant (55.8%). The most common cause of infertility was the female factor (42.3%) (Table 1). Participants were facing an infertility diagnosis between 3 years and 20 years (M (years) = 3.62; SD = 3.34; 95% CI = 2.97–4.27). Similarly, most of the sample had attended a fertility consultation as short as one week and as long as 20 years (M (years) = 3.10; SD = 3.31; 95% CI = 2.45–3.74). Treatment lasted for 2 months to 10 years (M (months) = 32.49; SD = 3.93; 95% CI = 24.63–40.36) and repeated treatment cycles were common (54.8%).
Meanwhile, about 47.1% of the respondents were on the edge of starting a new medical fertility procedure. In vitro fertilization (IVF) was the most common ART procedure (52.6%).
3.2. Descriptive Analysis of SWBQp
There were no missing or incomplete answers. The results of the statistical analysis revealed a significant association of SWB with the nature of infertility (p = 0.007), religion/spiritual change with treatment (p = 0.026), and phase of current treatment (p = 0.046) (Table 1). This means that SWB was more relevant in people who had been pregnant with treatment and were not able to have another child (M = 3.23, SD = 0.79), in people that perceived no change in their spirituality/religion during fertility treatment (M = 3.27, SD = 0.66), and in individuals that were in a treatment cycle (M = 3.16, SD = 0.69).
Nevertheless, higher mean scores of total SWBQ were presented by people who considered religion and spirituality as very important (religion: M = 3.80, SD = 0.30; spirituality: M = 3.68, SD = 0.52).
Additionally, the assessment of the Cronbach’s α coefficient and descriptive statistics of the four factors is reported in Table 2. For the overall instrument, Cronbach’s alpha was 0.947 and each domain revealed acceptable values higher than 0.7 (Tabachnick and Fidell 2007), indicating a high internal consistency or homogeneity of the scale. Internal consistency for the subscales ranged between 0.877 (personal domain) and 0.930 (transcendental domain) (Table 2). Cronbach’s alpha would not be improved by the deletion of any item. The corrected item-total correlations ranged from 0.59 to 0.76. Item means and standard deviations within the four dimensions were roughly equivalent, with one exception, as the total mean of the transcendental domain had a slightly lower value (2.69). The mean scores of responses per item ranged from 2.47 (item 15) to 3.65 (item 17).

Table 2.
Descriptive statistics, Cronbach’s alpha coefficient of the SWBQp factors/domains, and CFA assessment of normality of items.
The item means of the SWBQp subscales scores were higher in the communal (M = 3.36; SD = 0.854; 95% CI = 3.19–3.52) and environmental domains (M = 3.26; SD = 0.957; 95% CI = 3.08–3.45). The transcendental domain registered the lowest score (M = 2.69; SD = 1.099; 95% CI = 2.47–2.90).
Overall, the response items’ mean in the total SWBQp scale was 3.08 (SD = 0.79; 95% CI = 2.93–3.23) and the mean score of the general SWBQp scale was 61.55 (SD = 15.75; variance= 248.134).
3.3. Confirmatory Factor Analysis (CFA)
Appropriateness to proceed with a factor analysis was confirmed with a KMO sampling adequacy test value of 0.895 and Bartlett’s Test of Sphericity at 0.000 (p < 0.05). The structural validity of the original SWBQp instrument was further analyzed using a CFA. A test for normality was conducted (Table 3).

Table 3.
CFA goodness-of-fit indices for the six SWBQp models (N = 104).
Skewness and kurtosis absolute values fell mostly within an interval associated with normal distribution, with a skewness estimate of 1.0 or lower, a critical region (c.r.) for skewness that did not exceed 8.0, and a kurtosis that did not exceed 3.0 (Awang 2012; Westfall and Henning 2013). Thus, the variables were normally distributed, and additionally, no post hoc modifications (from AMOS) were indicated.
3.4. Construct Validity
First, an assessment of the best-fitting model within the six SWBQp models was conducted through CFA and is shown in Table 4. No item was deleted from the models, except the ones previously determined to be excluded in Model 2 and Model 3.

Table 4.
Construct validity and reliability of the SWBQp factors.
Model 1 (X2/df = 413/164; RMSEA = 0.122; SMRS = 0.098; CFI = 0.854) and Model 6 (X2/df = 418/166; RMSEA = 0.121; SMRS = 0.099; CFI = 0.853) yielded the best goodness-of-fit results. Still, the four-factor oblique model (Model 1) had a lower AIC, suggesting a slightly better fit and a satisfactory structure to the data (Nunes et al. 2018). A CFA diagram of Model 1 can be further seen in Figure 1.
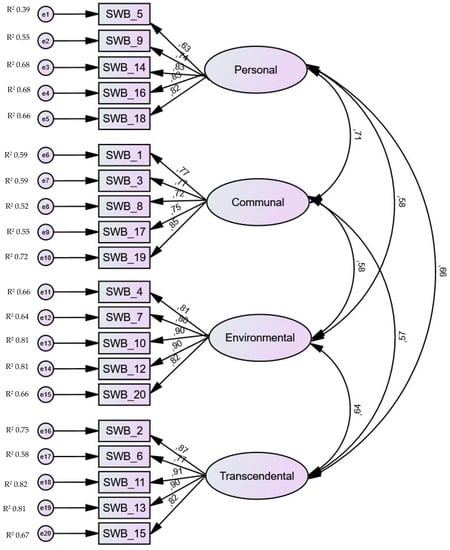
Figure 1.
Confirmatory factor analysis (CFA) of the SWBQp four-factor oblique model (Model 1).
All the items had approximate estimate values, further confirming they all contributed with similar weight to the study (Figure 1), and the most important ones were item 11, item 13, item 10, and item 12 (with a 0.9 value each). Item 5 (0.63) was the least important among them all. Figure 1 presents standardized factor loadings for each item and all measuring items had acceptable values equal to or higher than 0.6 (Awang 2012) for the respective latent factor. This finding indicated that the factors explained these items well, and around 50% of the variance was explained (squared multiple correlations (R2) ≈ 0.5) by the predicted variables. As such, the factors explained all the items well. Therefore, no item was deleted, and the measurement model was found to be appropriate. Standardized factor correlations were highest between the personal and communal factors (0.71). The lowest factor correlation found was between the communal and transcendental factors (0.57). The standardized factor loadings were statistically significant (p < 0.01).
Standardized residual covariances were smaller and no greater than 4, and items were considered suitable and not problematic to the model. Moreover, analysis of correlational residuals did not point out any item–pair correlation as especially problematic; rather, most correlational residuals were residuals greater than |0.10|.
Together, these patterns indicate that the data were well represented by the four-factor SWBQp model. Since the fitness index met requirements, a closer look was given to MI. The deletion of one or more factor loadings based on the cut-off value did not happen since there was no need to resolve possible multicollinearity issues (Awang 2012; Knekta et al. 2019). Although the largest MI values were 22.71 (item 5–item 10), 21.25 (e1 – environmental factor), 21.04 (item 5–item 12), and 17.19 (item 5–environmental factor), it was concluded that the elimination of some items/factors for this study would not improve Model 1, which had already shown a good fit, and thus no post hoc change was made to its structure.
3.5. Convergent and Discriminant Validity
Convergent validity (Table 4) and discriminant validity (Table 5) were verified. Model 1 had acceptable convergent validity (AVE > 0.50), as well as evidence of discriminant validity (MSV < AVE; ASV < AVE; the correlation between factors didn’t go over 0.85 and an √AVE was higher than the correlation between factors).

Table 5.
Discriminant validity of the SWBQp factors.
3.6. Reliability
4. Discussion
This study is the first to validate and test the structure of the SWBQp scale in a sample of Portuguese men and women attending fertility treatment. The six versions of the SWBQp model were examined by CFA, which confirmed the good fit of the four first-order oblique factor (Model 1) and the four first-order orthogonal factor (Model 6), although, with little difference, Model 1 had the best fit to the observed data. The additional statistical analysis supported Model 1’s configuration, which was found to be valid on the structural (factorial) and external (discriminant and convergent) levels, supporting the original version of Gomez and Fisher (Gomez and Fisher 2003; Gouveia et al. 2009; Gouveia 2011; Gouveia et al. 2012).
The use of a CFA approach to deepen the usefulness and suitability of the SWBQp structure was not new, and it corroborated the previous EFA results obtained in other settings (Gouveia 2011; Gouveia et al. 2012). In fact, because it is at the mercy of culture, beliefs, and values, the study of the psychometric properties of the SWBQp was previously suggested to be tested in different contexts (Gouveia et al. 2012). The internal consistency of the total scale in the present study (0.94) was as strong as that reported by other scholars, who estimated a Cronbach’s for the same instrument of approximately 0.76 and 0.95 (Gomez and Fisher 2003, 2005b). Nevertheless, discrepancies were found between the four domains, with an internal consistency higher on the transcendental domain (0.930) and lower on the personal domain (0.877). Significant correlations were shown between the four SWBQ domains, confirming early psychometric studies (Gomez and Fisher 2005b; Gouveia et al. 2009; Gouveia 2011).
All 20 items had strong factor loadings in their latent constructs, and the overall instrument was found to be reliable and suitable to measure SWB in adult Portuguese people going through ART. In general, the results of this paper are in line with the literature that relates infertility and spirituality (Romeiro et al. 2017a), while exceeding existing evidence and providing new knowledge about the spiritual well-being of people living with infertility.
The results highlighted the significant difference in the gender of respondents, with women (n = 102) participating more than men (n = 2). Women often play a more proactive role in the completion of questionnaires and participation in fertility-related studies (Romeiro et al. 2017a). Indeed, Ying and collaborators (Ying et al. 2016) described an increased willingness in women compared to men to address fertility issues and to seek fertility treatment.
It is also not surprising that participants of 52 years or older presented low SWB scores (M = 2.55; SD = 0.00). as infertility is known to affect spiritual needs and to generate long-term effects (Romeiro et al. 2017a, 2017b). In fact, a sense of failure, loss of control, grief, hopelessness, anxiety, stress, and lack of meaning and purpose in life was earlier associated with experiencing infertility (Romeiro et al. 2017a; Ying et al. 2016). In addition to that, the biological limitations caused by an advanced age disturb the timeframe established by couples to build a family and to pursue parenthood (Cooke et al. 2012; Romeiro et al. 2017a). This defies individuals’ and couples’ natural and biological expectations to reach the so longed-for transcendental state of motherhood (Romeiro et al. 2017a), which can explain the disturbance registered in the SWB of older people and of women trying to conceive for the second time. The inability to correspond to the social duty to become mothers and provide a bloodline family (Romeiro et al. 2017a, 2017b) might have conditioned participants’ answers in our study. This is supported by the notion that cultural and social backgrounds play an essential part in perceived well-being, and former patriarchal ideas are still a mindset) (Romeiro et al. 2017a) which affects Portuguese assumptions regarding gender roles and parenthood (SIRC 2012). Furthermore, women’s testimonies of being ready to become a mother as soon as they found the right partner, got married, completed their studies, and reached financial stability reflected our sample specificities (Cooke et al. 2012; SIRC 2012). In fact, over half (57.7%) of the participants in this study were married and in a relationship for at least one year, and most had higher education (65.4%) and were employed (87.5%). Indeed, a preference for postponing plans to start a family over personal goals fulfillment and socio-economic stability have been frequently associated with an advanced age and a decrease of a couple’s fertility (Cooke et al. 2012). In fact, primary infertility predominated in the sample (86.5%), with most women pursuing fertility treatment to become mothers for the first time. Yet, secondary infertility was described to be more prevalent in several countries, although the accuracy of these numbers has been questioned with aspects such as socio-cultural stigma and intimacy playing a determinant role in the available information concerning the fertility of couples (Mascarenhas et al. 2012).
In other countries such as Brazil, the mean of the SWBQ scores was close to the results obtained in Portugal, with one of the highest scores in the communal subscale and the lowest in the transcendental domain (Nunes et al. 2018). These results are similar to findings obtained in other Portuguese settings (Gouveia et al. 2012; Martins 2011; Neves et al. 2017).
Cycles of hope and despair are known to respectively arise at the beginning of treatment and again afterwards, when the results of pregnancy failure are known (Romeiro et al. 2017a). Indeed, in the current study, respondents going through ART had higher SWB scores (M = 3.16, SD = 0.69) than those who were in other stages of the fertility treatment. On the contrary, individuals who had concluded ART procedures and were waiting for tests results revealed lower SWB scores. Further, people going through consecutive cycles of treatment presented with lower SWB, providing an additional understanding and possible reason as to why couples quit treatment after repetitive ART procedures (Van den Broeck et al. 2009). After all, the mean of the transcendental dimension was lower than the other SWBQ subscales, providing a clear view of the imbalance provoked by infertility to an individual’s spiritual living. Meanwhile, Portuguese people with infertility that reported no shift in their religious and/or spiritual beliefs during treatment reported higher SWB scores. This is in line with previous research, as spirituality and not only religion were considered important resources in helping couples dealing with this health issue and coping with ART’s demands (Romeiro et al. 2017a). In accordance with the definition provided by Weathers and collaborators (Weathers et al. 2016), spirituality is a wider and broader concept that embraces religious beliefs and practices. This assumption was also demonstrated in the sample of the study by a higher number of respondents that identified themselves as spiritual against a lower number with a religious affiliation.
Although providing, crucial findings, this study had some limitations. First, the sample included participants with internet access going through ART. Nevertheless, it has been stated by other researchers that the internet is a privileged way for people to express more realistically, and with fewer constraints, their feelings and emotions triggered by infertility (Toscano and Montgomery 2009). Second, it was the only known study that implemented the SWBQ tool in Portuguese individuals with infertility, and as such, the comparability of findings was limited. Further, it is a cross-sectional study that explored SWB in a specific timeline, and fluctuations in SWB could happen at different times (Martins et al. 2017) of treatment. Third, the sample size was relatively small. Yet, the sample size seems to fit the type of study, and researchers remained cautious and aware of possible statistical biases, as recommended by Zhang and collaborators (Zhang et al. 2020). Fourth, the gender of the respondents still reflects the overrepresentation of women, although previous research calls mentioned the scarcity of evidence related to men’s experiences with infertility and ART and the effect of a couple’s dyadic relationship in SWB scores (Ying et al. 2016). Lastly, there was some initial hesitation of researchers in fulfilling the knowledge gap in this reproductive health setting due to the sensitive nature of it. Though previous evidence highlighted that the ethical concerns of conducting a study with such samples held more benefits than risks for individual spiritual healing (Caldeira et al. 2019b).
5. Conclusions
Although there was interest in studying infertility, the attributes of spirituality (transcendental, connectedness, and meaning in life) are still far from being fully comprehended. Yet, the data from this study provided evidence supporting the so-needed link between infertility and spirituality in the Portuguese context and in people undergoing ART.
SWBQp had good reliability and validity and these findings suggest the great sensitivity of this instrument to the data. Its internal consistency was good, with a Cronbach’s alpha of 0.94, and CFA supported the structure of the four first-order factor oblique model. Therefore, it is recommended to use this structural model in future research using similar samples, as well as in different reproductive health contexts. For instance, future studies evaluating SWBQp, specifically in individuals being diagnosed with infertility and/or after treatment, are suggested. It would also be beneficial if other researchers using this instrument provided the results of CFA to further validate it. This would provide more evidence and a necessary base for comparison to others (Fisher 2016).
The stability of the SWBQp over a longer period was not studied. Therefore, longitudinal studies are advised to explore if SWB scores remain constant over time. Furthermore, a wider sample and face-to-face interviews in other settings and not exclusively through the internet might be useful to access other people with infertility and to provide broader results, increasing the statistical power of findings more suitable to generalization.
A focus on men’s perceptions and on couples would also allow researchers to have a more detailed understanding of the individuals’ circumstances, helping in the assessments made by nurses and midwives of the patients’ spiritual needs. These suggestions are relevant to overcoming the likelihood of certain features in infertility-related studies, helping to overcome problematic or absent nursing practices, and raising awareness of the importance of the spiritual dimension of care. Further research is advised to expand the implementation of the SWBQp and other available spiritual tools. Systematic validation of such measurement tools would propel the engagement of nurses and midwives in a more standardized, holistic, and patient-centered care, which is crucial to empower individuals and monitor their well-being and healing process.
Inspired by findings of this research, nurses and midwives working with individuals with infertility are encouraged to overcome barriers and embrace the spiritual dimension of caring; hospital managers and policymakers are encouraged to create the tailored policies needed for the appropriate implementation of the best spiritual practices in the health system; and the education and training of nurses and midwives should guide and instigate an accurate spiritual assessment with tools adequately and thoroughly validated so as to improve quality of care in such reproductive environment. All of the aforementioned would allow the implementation of a more sustainable development of nurses and midwives.
Author Contributions
Conceptualization, J.R. and S.C.; methodology, J.R. and S.C.; validation, J.R., P.J.N., J.F. and S.C.; formal analysis, investigation, resources, data curation, writing—original draft preparation, writing—review and editing, visualization, supervision, and project administration, J.R., P.J.N., J.F. and S.C.; funding acquisition, J.R. and S.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by the NANDA-International, Inc. through a Foundation Grant Award granted to the first author’s doctoral project. This work was financially supported by national funds through the FCT–Fundação para a Ciência e a Tecnologia, I.P. under the project UIDB/04279/2020.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Afthanorhan, Asyraf. 2013. A Comparison Of Partial Least Square Structural Equation Modeling (PLS-SEM) and Covariance Based Structural Equation Modeling (CB-SEM) for Confirmatory Factor Analysis. Certified International Journal of Engineering Science and Innovative Technology 2: 198–205. [Google Scholar] [CrossRef]
- Alavi, Mousa, Denis C. Visentin, Deependra K. Thapa, Glenn E. Hunt, Roger Watson, and Michelle Cleary. 2020. Chi-Square for Model Fit in Confirmatory Factor Analysis. Journal of Advanced Nursing 76: 2209–11. [Google Scholar] [CrossRef]
- Alfaro-LeFevre, Rosalinda. 2012. Nursing Process and Clinical Reasoning. Nursing Education Perspective 33: 7. [Google Scholar] [CrossRef]
- Awang, Zainudin. 2012. The second order Confirmatory Factor Analysis. In A Handbook on SEM, 4th ed. Kuala Terengganu: Universiti Sultan Zainal Abidin, pp. 163–81. Available online: https://idocslide.org/document/a-handbook-on-sem-zainudin-awang-universiti-sultan-zainal-abidin-the-models-involved-in-structural-equation-modeling (accessed on 22 December 2020).
- Babyak, Michael A., and Samuel B. Green. 2010. Confirmatory Factor Analysis: An Introduction for Psychosomatic Medicine Researchers. Psychosomatic Medicine 72: 587–97. [Google Scholar] [CrossRef]
- Byrne, Barbara M. 2010. Structural Equation Modeling with AMOS: Basic Concepts, Applications, and Programming, 2nd ed. New York: Routledge/Taylor & Francis Group. [Google Scholar]
- Caldeira, Silvia, Emilia Campos de Carvalho, and Margarida Vieira. 2014. Entre o Bem-Estar Espiritual e a Angustia Espiritual: Possiveis Fatores Relacionados a Idosos Com Cancro. Revista Latino-Americana de Enfermagem 22: 28–34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Caldeira, Sílvia, Fiona Timmins, Emília Campos de Carvalho, and Margarida Vieira. 2017a. Clinical Validation of the Nursing Diagnosis Spiritual Distress in Cancer Patients Undergoing Chemotherapy. International Journal of Nursing Knowledge 28: 44–52. [Google Scholar] [CrossRef] [Green Version]
- Caldeira, Sílvia, Fiona Timmins, Emília Campos de Carvalho, and Margarida Vieira. 2017b. Spiritual Well-Being and Spiritual Distress in Cancer Patients Undergoing Chemotherapy: Utilizing the SWBQ as Component of Holistic Nursing Diagnosis. Journal of Religion and Health 56: 1489–502. [Google Scholar] [CrossRef] [PubMed]
- Caldeira, Sílvia, Joana Romeiro, and Helga Martins. 2019b. The Role of the Nurse in Providing Spiritual Care: A Case Study Approach to Exploring Specific Care Provision by Healthcare Workers in the Context of an Interdisciplinary Healthcare Team. In Spirituality in Healthcare: Perspectives for Innovative Practice. Edited by Fiona Timmins and Sílvia Caldeira. Cham: Springer International Publishing, pp. 117–42. [Google Scholar] [CrossRef]
- Caldeira, Sílvia, Joana Romeiro, Helga Martins, and Tiago Casaleiro. 2019a. The Therapeutic Dimension of Research about Spirituality: Particularities of Cancer, Mental Health and Infertility. Nursing Forum 54: 488–91. [Google Scholar] [CrossRef] [PubMed]
- Campbell, Donald T., and Donald W. Fiske. 1959. Convergent and discriminant validation by the multitrait-multimethod matrix. Psychological Bulletin 56: 81–105. [Google Scholar] [CrossRef] [Green Version]
- Centers for Disease Control and Prevention. 2014. National Public Health Action Plan for the Detection, Prevention, and Management of Infertility; Atlanta: Centers for Disease Control and Prevention. Available online: https://www.cdc.gov/reproductivehealth/infertility/publichealth.htm (accessed on 22 December 2020).
- Cooke, Alison, Tracey A. Mills, and Tina Lavender. 2012. Advanced Maternal Age: Delayed Childbearing Is Rarely a Conscious Choice a Qualitative Study of Women’s Views and Experiences. International Journal of Nursing Studies 49: 30–39. [Google Scholar] [CrossRef]
- de Jager Meezenbroek, Eltica, Bert Garssen, Machteld van den Berg, Dirk van Dierendonck, Adriaan Visser, and Wilmar B. Schaufeli. 2012. Measuring Spirituality as a Universal Human Experience: A Review of Spirituality Questionnaires. Journal of Religion and Health 51: 336–54. [Google Scholar] [CrossRef] [Green Version]
- Etemadifar, S., R. Hosseiny, Akram Ziraki, Atefeh Omrani, and M. Alijanpoor. 2016. The Relationship between Spiritual Well-Being and Life Satisfaction in Females with Infertility. Available online: https://www.semanticscholar.org/paper/The-Relationship-Between-Spiritual-Well-Being-and-Etemadifar-Hosseiny/fdd00afe3038850dc34d7c96aadaedb831d92d13 (accessed on 22 December 2020).
- Fisher, John W. 1998. Spiritual Health: Its Nature and Place in the School Curriculum. Ph.D. dissertation, University of Melbourne, Parkville, VIC, Australia. [Google Scholar]
- Fisher, John W., Leslie J. Francis, and Peter Johnson. 2000. Assessing Spiritual Health via Four Domains of Spiritual Wellbeing: The SH4DI. Pastoral Psychology 49: 133–45. [Google Scholar] [CrossRef]
- Fisher, John. 2010. Development and Application of a Spiritual Well-Being Questionnaire Called SHALOM. Religions 1: 105–21. [Google Scholar] [CrossRef] [Green Version]
- Fisher, John. 2016. Selecting the Best Version of SHALOM to Assess Spiritual Well-Being. Religions 7: 45. [Google Scholar] [CrossRef]
- Gomez, Rapson, and John W. Fisher. 2003. Domains of spiritual well-being and development and validation of the Spiritual Well-Being Questionnaire. Personality and Individual Differences 35: 1975–91. [Google Scholar] [CrossRef] [Green Version]
- Gomez, Rapson, and John W. Fisher. 2005a. Item Response Theory Analysis of the Spiritual Well-Being Questionnaire. Personality and Individual Differences 38: 1107–21. [Google Scholar] [CrossRef] [Green Version]
- Gomez, Rapson, and John W. Fisher. 2005b. The Spiritual Well-Being Questionnaire: Testing for Model Applicability, Measurement and Structural Equivalencies, and Latent Mean Differences across Gender. Personality and Individual Differences 39: 1383–93. [Google Scholar] [CrossRef] [Green Version]
- Google. 2019. Google Forms. Available online: https://www.google.com/forms/about/ (accessed on 22 December 2020).
- Gouveia, Maria J., Marta Marques, and José L. Pais Ribeiro. 2009. Versão portuguesa do questionário de bem-estar espiritual (SWBQ): Análise confirmatória da sua estrutura factorial. Psicologia, Saúde & Doenças 10: 285–93. [Google Scholar]
- Gouveia, Maria João Pinheiro Morais, José Luís Pais Ribeiro, and Marta Moreira Marques. 2012. Estudo da invariância fatorial do Questionário de Bem-estar espiritual (SWBQ) em praticantes de atividades físicas de inspiração oriental. Psychology, Community & Health 1: 140–50. [Google Scholar]
- Gouveia, Maria João Pinheiro Morais. 2011. Flow Disposicional e o bem-estar Espiritual em Praticantes de Actividades Físicas de Inspiração Oriental. Tese de Doutoramento em Psicologia. Lisboa: ISPA–Instituto Universitário, Available online: http://repositorio.ispa.pt/handle/10400.12/1226 (accessed on 22 December 2020).
- Hair, Joseph F., William C. Black, Barry J. Babin, and Rolph E. Anderson. 2010. Multivariate Data Analysis. Hoboken: Prentice Hall. [Google Scholar]
- Hooper, Daire, Joseph Coughlan, and Michael Mullen. 2008. Structural Equation Modelling: Guidelines for Determining Model Fit. The Electronic Journal of Business Research Methods 6: 53–60. [Google Scholar] [CrossRef]
- Hu, Li-tze, and Peter M. Bentler. 1998. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods 3: 424–53. [Google Scholar] [CrossRef]
- IBM. 2018. SPSS Version 26.0. 13 de Junho de 2018. Available online: https://www.ibm.com/us-en/ (accessed on 22 December 2020).
- Kline, Paul. 2000. A Psychometrics Primer. London: Free Association Books. [Google Scholar]
- Knekta, Eva, Christopher Runyon, and Sarah Eddy. 2019. One Size Doesn’t Fit All: Using Factor Analysis to Gather Validity Evidence When Using Surveys in Your Research. CBE Life Sciences Education 18: rm1. [Google Scholar] [CrossRef] [PubMed]
- Marsh, Herbert W., and Dennis Hocevar. 1985. Application of confirmatory factor analysis to the study of self-concept: First- and higher order factor models and their invariance across groups. Psychological Bulletin 97: 562–82. [Google Scholar] [CrossRef]
- Martins, Helga, Joana Romeiro, and Sílvia Caldeira. 2017. Spirituality in Nursing: An Overview of Research Methods. Religions 8: 226. [Google Scholar] [CrossRef] [Green Version]
- Martins, Vilma Raquel Ferreira. 2011. Caracterização e Abordagem das Necessidades Espirituais do Doente em Final de Vida: Visão Integrada dos Profissionais de Cuidados Paliativos. Master’s thesis, Faculdade de Medicina, Universidade de Lisboa, Lisboa, Portugal. Available online: http://repositorio.ul.pt/handle/10451/6290 (accessed on 22 December 2020).
- Mascarenhas, Maya N., Seth R. Flaxman, Ties Boerma, Sheryl Vanderpoel, and Gretchen A. Stevens. 2012. National, Regional, and Global Trends in Infertility Prevalence since 1990: A Systematic Analysis of 277 Health Surveys. PLoS Medicine 9: e1001356. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Microsoft. 2020. Microsoft Excel (versão Version 2020). Available online: https://www.microsoft.com/en-us/microsoft-365/excel (accessed on 22 December 2020).
- Myers, Nicholas D., Soyeon Ahn, and Ying Jin. 2011. Sample Size and Power Estimates for a Confirmatory Factor Analytic Model in Exercise and Sport: A Monte Carlo Approach. Research Quarterly for Exercise and Sport 82: 412–23. [Google Scholar] [CrossRef]
- Neves, Mariana Gomes das, Helena (Orientadora) Espirito-Santo, and Inês Queiroz (Coorientadora) Garcia. 2017. Bem-estar Espiritual, Sintomas Depressivos e Ansiosos nos Idosos. Master’s thesis, ISMT, Coimbra, Portugal. Available online: http://repositorio.ismt.pt:8080/jspui/handle/123456789/724 (accessed on 22 December 2020).
- Nunes, Sandra Adriana Neves, Helder Miguel Fernandes, John Wayne Fisher, and Marcos Gimenes Fernandes. 2018. Psychometric Properties of the Brazilian Version of the Lived Experience Component of the Spiritual Health And Life-Orientation Measure (SHALOM). Psicologia: Reflexão e Crítica 31: 2. [Google Scholar] [CrossRef] [Green Version]
- Nunnally, Jum C., and Ira H. Bernstein. 1994. The Assessment of Reliability. In Psychometric Theory. New York: McGraw-Hill, vol. 3, pp. 248–92. [Google Scholar]
- Pestana, Maria Helena, and João Nunes Gageiro. 2003. Análise de Dados para Ciências Sociais: A Complementariedade do SPSS. Lisboa: Sílabo. [Google Scholar]
- Rodrigues, Lia Carina Proença. 2013. A Mulher Idosa Institucionalizada: Saúde Mental e Bem-Estar Espiritual. Master’s thesis, ISPA-Instituto Universitário, Lisboa, Portugal. Available online: http://repositorio.ispa.pt/handle/10400.12/2759 (accessed on 22 December 2020).
- Romeiro, Joana, and Silvia Caldeira. 2018a. A synthesis of Portuguese studies regarding infertile patients. BMC Health Services Research 18: 684. [Google Scholar] [CrossRef]
- Romeiro, Joana, and Sílvia Caldeira. 2018b. The Human Responses and Nursing Diagnoses of Those Living With Infertility: A Qualitative Systematic Review. International Journal of Nursing Knowledge 30: 173–89. [Google Scholar] [CrossRef]
- Romeiro, Joana, and Sílvia Caldeira. 2020. Fertile Ground for the Provision of Spiritual Care: Commentary on a Qualitative Systematic Review Protocol of the Experiences of Adults Participating in Infertility Support Groups. JBI Evidence Synthesis 18: 640–41. [Google Scholar] [CrossRef]
- Romeiro, Joana, Helga Martins, Sara Pinto, and Sílvia Caldeira. 2018. Review and Characterization of Portuguese Theses, Dissertations, and Papers about Spirituality in Health. Religions 9: 271. [Google Scholar] [CrossRef] [Green Version]
- Romeiro, Joana, Sílvia Caldeira, Vivienne Brady, Fiona Timmins, and Jenny Hall. 2017a. Spiritual aspects of living with infertility: A synthesis of qualitative studies. Journal of Clinical Nursing 26: 3917–35. [Google Scholar] [CrossRef] [Green Version]
- Romeiro, Joana, Sílvia Caldeira, Vivienne Brady, Jenny Hall, and Fiona Timmins. 2017b. The Spiritual Journey of Infertile Couples: Discussing the Opportunity for Spiritual Care. Religions 8: 76. [Google Scholar] [CrossRef]
- Roudsari, Robab Latifnejad, Helen T. Allan, and Pam A. Smith. 2007. Looking at Infertility through the Lens of Religion and Spirituality: A Review of the Literature. Human Fertility (Cambridge, England) 10: 141–49. [Google Scholar] [CrossRef] [PubMed]
- SIRC. 2012. The Changing Face of Motherhood in Western Europe. Available online: http://www.sirc.org/publik/motherhood_in_western_europe.shtml (accessed on 22 December 2020).
- Tabachnick, Barbara G., and Linda S. Fidell. 2007. Using Multivariate Statistics, 5th ed. Boston: Allyn & Bacon/Pearson Education. [Google Scholar]
- Toscano, Sheryl Eve, and Rebeca M. Montgomery. 2009. The Lived Experience of Women Pregnant (Including Preconception) Post In Vitro Fertilization Through the Lens of Virtual Communities. Health Care for Women International 30: 1014–36. [Google Scholar] [CrossRef]
- Van den Broeck, U., L. Holvoet, P. Enzlin, E. Bakelants, K. Demyttenaere, and T. DHooghe ’. 2009. Reasons for Dropout in Infertility Treatment. Gynecologic and Obstetric Investigation 68: 58–64. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Weathers, Elizabeth, Geraldine McCarthy, and Alice Coffey. 2016. Concept Analysis of Spirituality: An Evolutionary Approach. Nursing Forum 51: 79–96. [Google Scholar] [CrossRef]
- Westfall, Peter, and Kevin S. S. Henning. 2013. Understanding Advanced Statistical Methods. Boca Raton: Taylor & Francis. [Google Scholar]
- Winters, Ryan, Andrew Winters, and Ronald G. Amedee. 2010. Statistics: A Brief Overview. The Ochsner Journal 10: 213–16. [Google Scholar]
- Ying, Liying, Lai Har Wu, and Alice Yuen Loke. 2016. Gender Differences in Emotional Reactions to in Vitro Fertilization Treatment: A Systematic Review. Journal of Assisted Reproduction and Genetics 33: 167–79. [Google Scholar] [CrossRef] [Green Version]
- Zegers-Hochschild, Fernando, G. David Adamson, Silke Dyer, Catherine Racowsky, Jacques de Mouzon, Rebecca Sokol, Laura Rienzi, Arne Sunde, Lone Schmidt, Ian D Cooke, and et al. 2017. The International Glossary on Infertility and Fertility Care, 2017. Fertility and Sterility 108: 393–406. [Google Scholar] [CrossRef] [Green Version]
- Zhang, Mary F., Jeremy F. Dawson, and Rex B. Kline. 2020. Evaluating the Use of Covariance-Based Structural Equation Modelling with Reflective Measurement in Organizational and Management Research: A Review and Recommendations for Best Practice. British Journal of Management 32: 257–72. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).