Current Mental Health Clients’ Attitudes Regarding Religion and Spirituality in Treatment: A National Survey
Abstract
1. Introduction
Clients can’t check their worldviews, spirituality, or values at our door any more than we can choose to leave our hands and feet behind when we go to work. A religious identity and worldview are integral aspects of how religious clients think about, experience, respond to, and take action upon their world.
1.1. Client Attitudes toward RS in Mental Health Treatment
1.1.1. Client Characteristics That Influence Client Preference
1.1.2. Limitations of Previous Studies
1.2. Current Study
2. Methods
3. Results
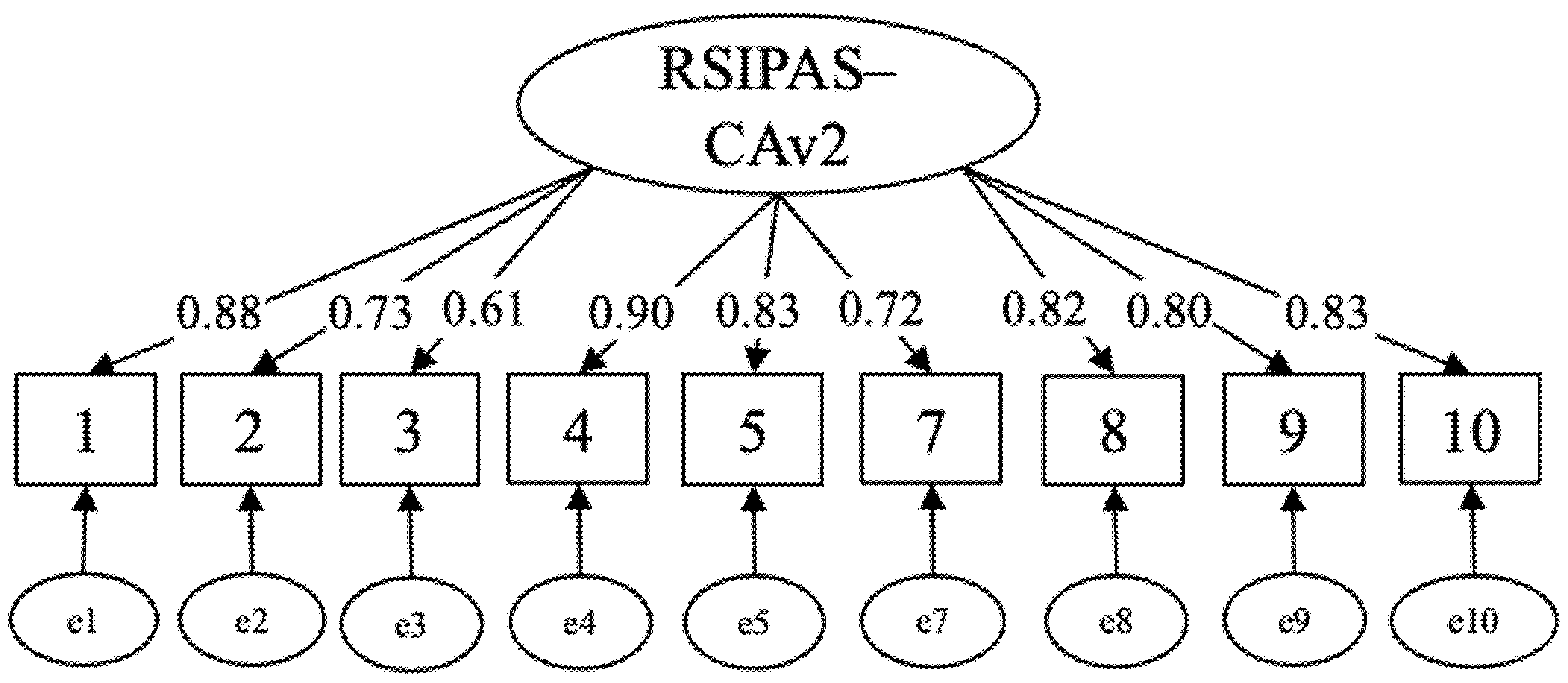
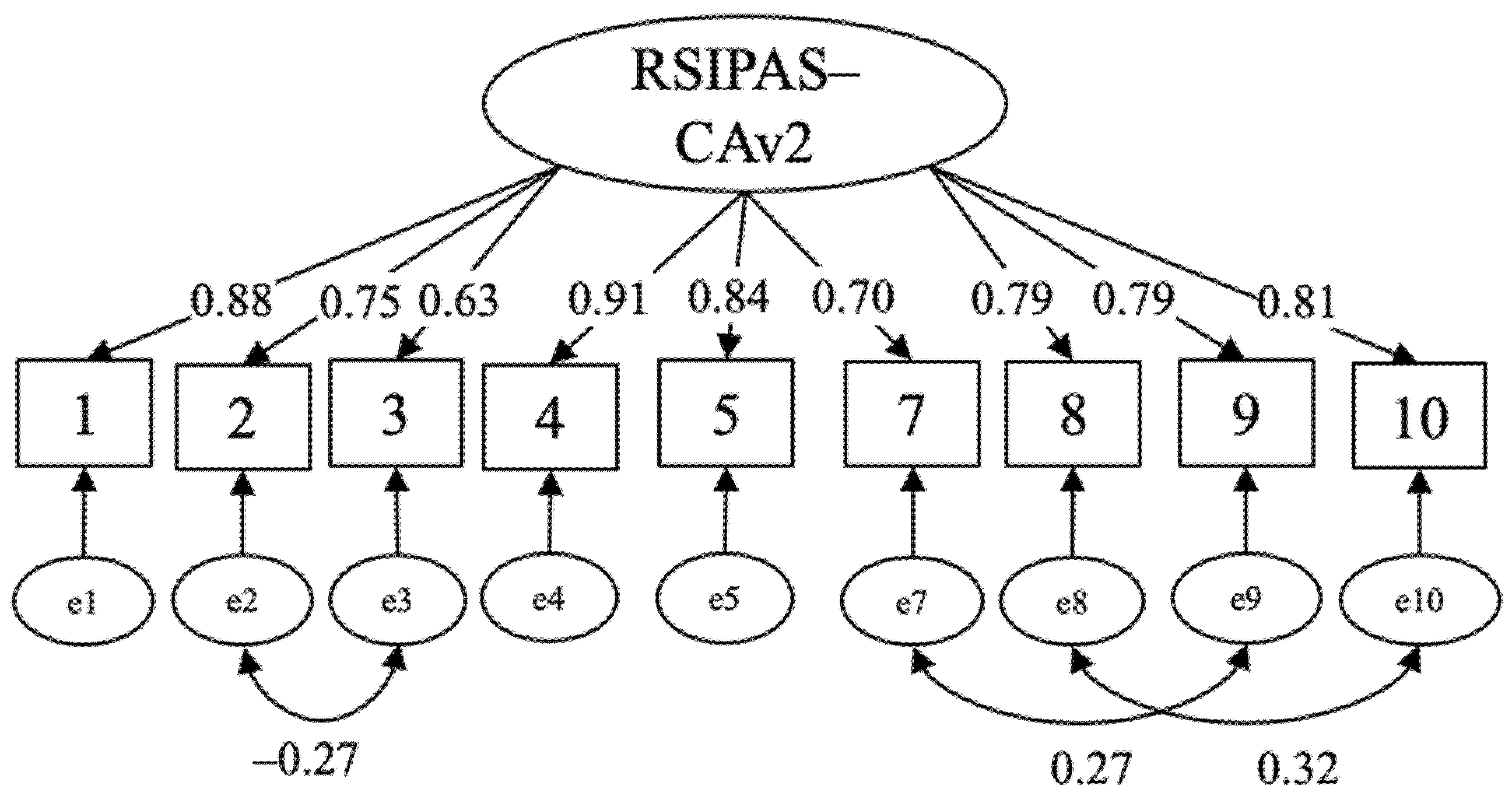
3.1. Reliability and Validity of RSIPAS-CAv2
3.2. Client Attitudes toward RS Integration
3.3. Client Characteristics That Predict Positive Attitudes toward Integrating RS
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Allport, Gordon W., and J. Michael Ross. 1967. Personal religious orientation and prejudice. Journal of Personality and Social Psychology 5: 432–43. [Google Scholar] [CrossRef] [PubMed]
- American Association for Marriage and Family Therapy. 2012. Code of Ethics. Available online: https://www.aamft.org/Legal_Ethics/Code_of_Ethics.aspx (accessed on 31 March 2021).
- American Counseling Association. 2014. Code of Ethics. July 1. Available online: www.counseling.org/Resources/aca-code-of-ethics.pdf (accessed on 31 March 2021).
- American Nurses Association. 2015. Code of Ethics for Nurses with Interpretive Statements. Available online: http://nursingworld.org/codeofethics (accessed on 31 March 2021).
- American Psychological Association. 2010. Ethical Principles of Psychologists and Code of Conduct: Including 2010 Amendments. June 1. Available online: www.apa.org/ethics/code (accessed on 31 March 2021).
- Arnold, Ruth M., S. Kelly Avants, Arthur Margolin, and David Marcotte. 2002. Patient attitudes concerning the inclusion of spirituality into addiction treatment. Journal of Substance Abuse Treatment 23: 319–26. [Google Scholar] [CrossRef]
- Atkinson, Donald R., and Ruth H. Gim. 1989. Asian-American cultural identity and attitudes toward mental health services. Journal of Counseling Psychology 36: 209–12. [Google Scholar] [CrossRef]
- Baker, Paul, and James Cruickshank. 2009. I am happy in my faith: The influence of religious affiliation, saliency, and practice on depressive symptoms and treatment preference. Mental Health, Religion & Culture 12: 339–57. [Google Scholar] [CrossRef]
- Bannister, Shaynah N., Hae S. Park, Stephanie Taylor, and Emily N. Bauerie. 2015. Clients’ expectations and preferences for marital Christian counseling. A chronological literature review and a contemporary evaluation. Social Work & Christianity 42: 63–95. [Google Scholar]
- Belaire, Christine, and J. Scott Young. 2002. Conservative Christians’ expectations of non-Christian counselors. Counseling and Values 46: 175–87. [Google Scholar] [CrossRef]
- Belaire, Christine, J. Scott Young, and Anastasia Elder. 2005. Inclusion of religious behaviors and attitudes in counseling: Expectations of conservative Christians. Counseling and Values 49: 82–94. [Google Scholar] [CrossRef]
- Carlisle, Patricia. 2015. Religion and spirituality as troublesome knowledge: The views and experiences of mental health social workers in Northern Ireland. British Journal of Social Work 46: 583–98. [Google Scholar] [CrossRef]
- Cashwell, Craig S., J. Scott Young, Tammy H. Cashwell, and Christine Belaire. 2001. The inclusion of spiritual process in counseling and perceived counselor effectiveness. Counseling and Values 45: 145–53. [Google Scholar] [CrossRef]
- Colbert, Linda K., Joseph L. Jefferson, Ralph Gallo, and Ronnie Davis. 2009. A study of religiosity and psychological well-being among African Americans: Implications for counseling and psychotherapeutic processes. Journal of Religious Health 48: 278–89. [Google Scholar] [CrossRef]
- Comrey, Andrew L., and Howard B. Lee. 1992. A First Course in Factor Analysis, 2nd ed. Mahwah: Lawrence Erlbaum. [Google Scholar]
- Crabtree, Sarah A., Chance A. Bell, David A. Rupert, Steven J. Sandage, Nancy G. Devor, and George Stavros. 2020. Humility, differentiation of self, and clinical training in spiritual and religious competence. Journal of Spirituality in Mental Health, 1–21. [Google Scholar] [CrossRef]
- Cragun, Carrie L., and Myrna L. Friedlander. 2012. Experiences of Christian clients in secular psychotherapy: A mixed-methods investigation. Journal of Counseling Psychology 59: 379–91. [Google Scholar] [CrossRef] [PubMed]
- Crosby, James W., and Natasha Bossley. 2012. The religiosity gap: Preferences for seeking help from religious advisors. Mental Health, Religion, and Culture 15: 141–59. [Google Scholar] [CrossRef]
- D’Souza, Russell. 2002. Do patients expect psychiatrists to be interested in spiritual issues? Australian Psychiatry 10: 44–47. [Google Scholar] [CrossRef]
- Daaleman, Timothy P., and Donald E. Nease. 1994. Patient attitudes regarding physician inquiry into spiritual and religious issues. The Journal of Family Practice 39: 564–68. [Google Scholar] [PubMed]
- Erickson, Martin J., Lorna Hecker, Dwight Kirkpatrick, Mark Killmer, and Edassery James. 2002. Clients’ perceptions of marriage and family therapists addressing the religious and spiritual aspects of clients’ lives: A pilot study. Journal of Family Psychotherapy 12: 109–25. [Google Scholar] [CrossRef]
- Exline, Julie J. 2013. Religious and spiritual struggles. In APA Handbook of Psychology, Religion, and Spirituality: Context, Theory and Research. Edited by Julie J. Exline, James W. Jones and Kenneth Ira Pargament. Washington, DC: American Psychological Association, pp. 459–75. [Google Scholar]
- Gass, Carlton S. 1984. Orthodox Christian values related to psychotherapy and mental health. Journal of Psychology and Theology 12: 230–37. [Google Scholar] [CrossRef]
- Godwin, Tony C., and Joyce G. Crouch. 1989. Subjects’ religious orientation, counselor’s orientation and skill, and expectations for counseling. Journal of Psychology and Theology 17: 284–92. [Google Scholar] [CrossRef]
- Guinee, James P., and Terence J. G. Tracey. 1997. Effects of religiosity and problem type on counselor description ratings. Journal of Counseling and Development 76: 65–73. [Google Scholar] [CrossRef]
- Harris, Kevin A., Brooke E. Randolph, and Timothy D. Gordon. 2016. What do clients want? Assessing spiritual needs in counseling: A literature review. Spirituality in Clinical Practice 3: 250–75. [Google Scholar] [CrossRef]
- Hathaway, Stefani. L. 2005. Religious Involvement, Attitudes toward Seeking Professional Psychological Help, and Preferences for Alternative Mental Health Setting. Doctoral dissertation, University of Missouri-Columbia, Columbia, MO, USA, December. Available online: https://pdfs.semanticscholar.org/6fc5/14012d95d34840d56bc3f663cb89faa3a5db.pdf (accessed on 31 March 2021).
- Hill, Peter C., Kenneth I. Pargament, Ralph W. Hood, Michael E. McCullough, James P. Swyers, David B. Larson, and Brian J. Zinnbauer. 2000. Conceptualizing religion and spirituality: Points of commonality, points of departure. Journal for the Theory of Social Behaviour 30: 51–77. [Google Scholar] [CrossRef]
- Hodge, David R. 2006. Spiritually modified cognitive therapy: A review of the literature. Social Work 51: 157–66. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hook, Joshua N., Everett L. Worthington, Jr., Don E. Davis, David J. Jennings, Aubrey L. Gartner, and Jan P. Hook. 2010. Empirically supported religious and spiritual therapies. Journal of Clinical Psychology 66: 46–72. [Google Scholar] [CrossRef]
- Kelly, Eugene W., Amany Aridi, and Laleh Bakhiar. 1996. Muslims in the United States: An exploratory study of universal and mental health values. Counseling and Values 40: 206–18. [Google Scholar] [CrossRef]
- King, Dana E., and Bruce Bushwick. 1994. Beliefs and attitudes of hospital inpatients about faith healing and prayer. Journal of Family Practice 39: 349–52. [Google Scholar]
- Kline, Rex B. 2016. Principles and Practice of Structural Equation Modeling, 4th ed. New York: Guilford. [Google Scholar]
- Knox, Sarah, Lynn Catlin, Margaret Casper, and Lewis Z. Schlosser. 2005. Addressing religion and spirituality in psychotherapy: Clients’ perspectives. Psychotherapy Research 15: 287–303. [Google Scholar] [CrossRef]
- Koenig, Harold G., and Arndt Büssing. 2010. The Duke University Religion Index (DUREL): A five-item measure for use in epidemiological studies. Religions 1: 78–85. [Google Scholar] [CrossRef]
- Koenig, Harold G., Dana E. King, and Verna B. Carson. 2012. Handbook of Religion and Health, 2nd ed. Oxford: Oxford University Press. [Google Scholar]
- Koenig, Harold G., Michael E. McCullough, and David B. Larson. 2001. Handbook of Religion and Health. Oxford: Oxford University Press. [Google Scholar]
- Laudet, Alexandre B. 2003. Attitudes and beliefs about 12-step groups among addiction treatment clients and clinicians: Toward identifying obstacles to participation. Substance Use and Misuse 38: 2017–47. [Google Scholar] [CrossRef]
- Leitz, Cynthia A., and David R. Hodge. 2013. Incorporating spirituality into substance abuse counseling: Examining the perspectives of service recipients and providers. Journal of Social Service Research 39: 498–510. [Google Scholar] [CrossRef]
- Leondari, Angeliki, and Vasilios Gialamas. 2009. Religiosity and psychological well-being. International Journal of Psychology 44: 241–48. [Google Scholar] [CrossRef]
- Levin, Jeff. 2016. Prevalence and religious predictors of healing prayer use in the USA: Findings from the Baylor Religion Survey. Journal of Religion and Health 55: 1136–58. [Google Scholar] [CrossRef] [PubMed]
- Lindgren, Karen N., and Robert D. Coursey. 1995. Spirituality and serious mental illness: A two-part study. Psychosocial Rehabilitation Journal 18: 93–111. [Google Scholar] [CrossRef]
- Lukoff, David, Robert Turner, and Francis Lu. 1992. Transpersonal psychology research review: Psychoreligious dimensions of healing. Journal of Transpersonal Psychology 24: 41–60. [Google Scholar]
- Lyon, Rachel E. C., and Christian L. Wimmer. 2005. Spirituality and dream work in counseling: Clients’ experiences. Pastoral Psychology 54: 35–45. [Google Scholar] [CrossRef]
- Mayers, Claire, Gerard Leavey, Christina Valliantou, and Chris Barker. 2007. How clients with religious or spiritual beliefs experience psychological help-seeking and therapy: A qualitative study. Clinical Psychology and Psychotherapy 14: 317–27. [Google Scholar] [CrossRef]
- Morrison, Julie Q., Stacy M. Clutter, Elaine M. Pritchett, and Alan Demmitt. 2009. Perceptions of clients and counseling professionals regarding spirituality in counseling. Counseling and Values 53: 183–94. [Google Scholar] [CrossRef]
- Morrow, David, Everett L. Worthington, Jr., and Michael E. McCullough. 1993. Observers’ perceptions of a counselor’s treatment of a religious issue. Journal of Counseling and Development 71: 452–56. [Google Scholar] [CrossRef]
- National Association of Social Workers. 2017. Code of Ethics. Available online: https://www.socialworkers.org/About/Ethics/Code-of-Ethics/Code-of-Ethics-English (accessed on 31 March 2021).
- Oxhandler, Holly K., and Kenneth I. Pargament. 2014. Social work practitioners’ integration of clients’ religion and spirituality in practice: A literature review. Social Work 59: 271–79. [Google Scholar] [CrossRef]
- Oxhandler, Holly K., Danielle E. Parrish, Luis R. Torres, and W. Andrew Achenbaum. 2015. The integration of clients’ religion/spirituality in social work practice: A national survey. Social Work 60: 228–37. [Google Scholar] [CrossRef]
- Oxhandler, Holly K., and Danielle E. Parrish. 2016. The development and validation of the Religious/Spiritually Integrated Practice Assessment Scale. Research on Social Work Practice 26: 295–307. [Google Scholar] [CrossRef]
- Oxhandler, Holly K., and Traber D. Giardina. 2017. Social workers’ perceived barriers to and sources of support with integrating clients’ religion/spirituality in practice. Social Work 62: 323–32. [Google Scholar] [CrossRef]
- Oxhandler, Holly K. 2017. Namaste theory: A quantitative grounded theory on religion and spirituality in mental health treatment. Religions 8: 168. [Google Scholar] [CrossRef]
- Oxhandler, Holly K., and Danielle E. Parrish. 2018. Integrating clients’ religion/spirituality in clinical practice: A comparison among social workers, psychologists, counselors, marriage and family therapists, and nurses. Journal of Clinical Psychology 74: 680–94. [Google Scholar] [CrossRef]
- Oxhandler, Holly K., Edward C. Polson, and W. Andrew Achenbaum. 2018a. The religiosity and spiritual beliefs and practices of clinical social workers: A national survey. Social Work 63: 47–56. [Google Scholar] [CrossRef] [PubMed]
- Oxhandler, Holly K., James W. Ellor, and Matthew S. Stanford. 2018b. Client attitudes toward integrating religion/spirituality in mental health treatment: Scale development and client responses. Social Work 63: 337–46. [Google Scholar] [CrossRef]
- Oxhandler, Holly K., Edward C. Polson, and Kelsey M. Moffatt. 2021a. The Religious/Spiritually Integrated Practice Assessment Scale for Educators: A national survey of social work faculty. Journal of Social Work Education. In press. [Google Scholar]
- Oxhandler, Holly K., Kenneth I. Pargament, Michelle J. Pearce, Cassandra Vieten, and Kelsey M. Moffatt. 2021b. The perceived relevance of religion/spirituality and mental health to one another: A national survey of current clients’ views and scale development. Social Work. In press. [Google Scholar]
- Oxhandler, Holly K., Kelsey M. Moffatt, and Traber D. Giardina. 2019. Clinical helping professionals’ perceived support, barriers, and training to integrate clients’ religion/spirituality in practice. Spirituality in Clinical Practice 6: 279–91. [Google Scholar] [CrossRef]
- Pargament, Kenneth I. 2007. Spiritually Integrated Psychotherapy: Understanding and Addressing the Sacred. New York: Guilford Press. [Google Scholar]
- Pargament, Kenneth I., Annette M. Mahoney, Julie J. Exline, James W. Jones, and Edward P. Shafranske. 2013. Envisioning an integrative paradigm for the psychology of religion and spirituality. In APA Handbook of Psychology, Religion, and Spirituality: Context, Theory and Research. Edited by Kenneth I. Pargrament, Julie J. Exline and James W. Jones. Washington, DC: APA, pp. 3–19. [Google Scholar]
- Pearce, Michelle J. 2016. Cognitive Behavioral Therapy for Christians with Depression: A Practical Tool-Based Primer. West Conshohocken: Templeton Press. [Google Scholar]
- Pearce, Michelle J., Kenneth I. Pargament, Holly K. Oxhandler, Cassandra Vieten, and Serena Wong. 2020. Novel online training program improves spiritual competence in mental health care. Spirituality in Clinical Practice 7: 145–61. [Google Scholar] [CrossRef]
- Pew Research Center. 2012. “Nones” on the Rise. Available online: https://www.pewforum.org/2012/10/09/nones-on-the-rise/ (accessed on 31 March 2021).
- Pew Research Center. 2015. U.S. Religious Landscape Study. Available online: http://www.pewforum.org/religious-landscape-study/ (accessed on 31 March 2021).
- Post, Brian C., and Nathaniel G. Wade. 2009. Religion and spirituality in psychotherapy: A practice-friendly review of research. Journal of Clinical Psychology 65: 131–46. [Google Scholar] [CrossRef]
- Post, Brian C., Nathaniel G. Wade, and Marilyn A. Cornish. 2014. Religion and spirituality in group counseling: Beliefs and preferences of university counseling center clients. Group Dynamics: Theory, Research, and Practice 18: 53–68. [Google Scholar] [CrossRef]
- Privette, Gayle, Stephen Quackenbos, and Charles M. Bundrick. 1994. Preferences for religious or nonreligious counseling and psychotherapy. Psychological Reports 75: 539–46. [Google Scholar] [CrossRef] [PubMed]
- Rogers, Edward B., Matthew Stanford, and Diana R. Garland. 2012. The effects of mental illness on families within faith communities. Mental Health, Religion & Culture 15: 301–13. [Google Scholar] [CrossRef]
- Rose, Elizabeth M., John S. Westefeld, and Timothy N. Ansley. 2001. Spiritual issues in counseling: Client’s beliefs and preferences. Journal of Counseling Psychology 48: 61–71. [Google Scholar] [CrossRef]
- Schaffner, Angela D., and David N. Dixon. 2003. Religiosity, gender, and preferences for religious interventions in counseling: A preliminary study. Counseling and Values 48: 24–33. [Google Scholar] [CrossRef]
- Smith, Timothy B., Jeremy Bartz, and P. Scott Richards. 2007. Outcome of religious and spiritual adaptations to psychotherapy: A meta-analytic review. Psychotherapy Research 17: 643–55. [Google Scholar] [CrossRef]
- Smith, Tom W., Michael Hout, and Peter Marsden. 2016. General Social Surveys, 1972–2014 Cumulative File. Chicago: National Opinion Research Center, University of Chicago. [Google Scholar]
- Stanley, Melinda A., Amber L. Bush, Mary E. Camp, John P. Jameson, Laura L. Philips, Catherine R. Barber, Darrell Zeno, James W. Lomax, and Jeffrey A. Cully. 2011. Older adults’ preferences for religion/spirituality in treatment for anxiety and depression. Aging and Mental Health 15: 334–43. [Google Scholar] [CrossRef] [PubMed]
- Tepper, Leslie, Steven A. Rogers, Esther M. Coleman, and H. Newton Malony. 2001. The prevalence of religious coping among persons with persistent mental illness. Psychiatric Services 52: 660–65. [Google Scholar] [CrossRef]
- van Nieuw Amerongen-Meeuse, Joke C., Hanneke Schaap-Jonker, Christa Anbeek, and Arjan W. Braam. 2020. Religious/spiritual care needs and treatment alliance among clinical mental health patients. Journal of Psychiatric and Mental Health Nursing 28: 370–83. [Google Scholar] [CrossRef]
- Vieten, Cassandra, and Shelley Scammell. 2015. Spiritual and Religious Competencies in Clinical Practice: Guidelines for Psychotherapists and Mental Health Professionals. Oakland: New Harbinger. [Google Scholar]
- Wade, Nathaniel G., Everett L. Worthington, Jr., and David L. Vogel. 2007. Effectiveness of religiously tailored interventions in Christian therapy. Psychotherapy Research 17: 91–105. [Google Scholar] [CrossRef]
- Walker, Donald F., Everett L. Worthington, Jr., Aubrey L. Gartner, Richard L. Gorsuch, and Evalin R. Henshew. 2011. Religious commitment and expectations about psychotherapy among Christian clients. Psychology of Religion and Spirituality 3: 98–114. [Google Scholar] [CrossRef]
- Wang, Philip S., Michael Lane, Mark Olfson, Harold A. Pincus, Kenneth B. Wells, and Ronald C. Kessler. 2005. Twelve-month use of mental health services in the United States: Results from the national comorbidity survey replication. Archive of General Psychiatry 62: 629–40. [Google Scholar] [CrossRef] [PubMed]
- Weld, Chet, and Karen Eriksen. 2007. The ethics of prayer in counseling. Counseling and Values 51: 121–38. [Google Scholar] [CrossRef]
- Wikler, Meir. 1989. The religion of the therapist: Its meaning to Orthodox Jewish clients. The Hillside Journal of Clinical Psychiatry 11: 131–46. [Google Scholar] [PubMed]
- Worthington, Everett L., Jr., Joshua N. Hook, Don E. Davis, and Michael A. McDaniel. 2011. Religion and spirituality. Journal of Clinical Psychology 67: 204–14. [Google Scholar] [CrossRef]
| Characteristic | M | SD |
|---|---|---|
| Age (years) | 45.6 | 16.3 |
| n | % | |
| Gender | ||
| Female | 471 | 47.6 |
| Male | 516 | 52.2 |
| Other | 2 | 0.2 |
| Race/Ethnicity | ||
| African American/Black | 118 | 11.9 |
| American Indian/Alaskan Native | 18 | 1.8 |
| Asian/Pacific Islander | 22 | 2.2 |
| Hispanic/Latinx | 63 | 6.4 |
| White | 760 | 76.8 |
| Other | 8 | 0.8 |
| Religious preference | ||
| Protestant | 319 | 32.3 |
| Catholic | 207 | 20.9 |
| Jewish | 51 | 5.2 |
| Buddhist | 15 | 1.5 |
| Hindu | 6 | 0.6 |
| Other Eastern Religion | 2 | 0.2 |
| Muslim | 19 | 1.9 |
| Orthodox–Christian | 86 | 8.7 |
| Native American | 17 | 1.7 |
| Inter-Nondenominational | 53 | 5.4 |
| Don’t Know/Other | 50 | 5.1 |
| Other | 58 | 5.9 |
| None | 106 | 10.7 |
| Were your RS beliefs brought up in therapy? | ||
| Yes, brought up by client | 415 | 42.0 |
| Yes, brought up by therapist | 256 | 25.9 |
| No, but wish they had been discussed | 94 | 9.5 |
| No, glad they were not discussed | 224 | 22.6 |
| To what extent do you consider yourself a religious person? | ||
| Moderately/very religious | 550 | 55.6 |
| To what extent do you consider yourself a spiritual person? | ||
| Moderately/very spiritual | 696 | 70.4 |
| Do you believe in God or a Higher Power?: Yes | 821 | 83.0 |
| Model | Items | df | χ2 | p | χ²/df | RMSEA [90% CI] | CFI | TLI |
|---|---|---|---|---|---|---|---|---|
| Baseline CFA | 9 | 27 | 485.89 | 0.00 | 18.00 | 0.131 [0.121, 0.141] | 0.974 | 0.965 |
| Final CFA | 9 | 24 | 249.33 | 0.00 | 10.39 | 0.097 [0.087, 0.109] | 0.987 | 0.981 |
| RSIPAS-CAv2 Items | Strongly Disagree/ Disagree n (%) | Neutral n (%) | Strongly Agree/ Agree n (%) |
|---|---|---|---|
| 1. It is important for my therapist to know how to discuss my religion/spirituality in mental health therapy. | 204 (20.6) | 202 (20.4) | 583 (58.9) |
| 2. My therapist should ask about my religion/spirituality, rather than wait for me to bring it up. | 317 (32.1) | 242 (24.5) | 430 (43.5) |
| 3. I would prefer to bring up my religion/spirituality, rather than wait for my therapist to ask about it. | 205 (20.7) | 282 (28.5) | 502 (50.8) |
| 4. Discussing my religious/spiritual beliefs in therapy helps improve my mental health. | 145 (24.8) | 238 (24.1) | 506 (51.2) |
| 5. When my therapist takes time to understand my religious/spiritual beliefs, they show greater concern for my well-being rather than not taking the time to understand my religious/spiritual beliefs. | 172 (17.4) | 247 (25.0) | 570 (57.6) |
| 6. I am open to working with a therapist who has a different belief system than I do. a | 119 (12.0) | 197 (19.9) | 673 (68.0) |
| 7. A good therapist is sensitive to clients’ religious/spiritual beliefs. | 72 (7.3) | 169 (17.1) | 748 (75.6) |
| 8. I am open to being referred to religious or pastoral counseling if my therapist thinks it would be helpful. | 263 (26.6) | 175 (17.7) | 551 (55.7) |
| 9. I would be open to discussing my religious/spiritual beliefs in therapy. | 119 (12.0) | 168 (17.0) | 702 (71.0) |
| 10. My religious/spiritual beliefs are important to me during difficult times. | 181 (18.3) | 156 (15.8) | 652 (65.9) |
| Variable | r | |||
| Age (Continuous) | −0.140 *** | |||
| Race (White or Non-White) | −0.118 *** | |||
| Gender (Female or Non-Female) | −0.137 *** | |||
| Organizing Religious Activity (At least a few times a month or Never/Rarely) | 0.477 *** | |||
| Non-Organized Religious Activity (At least once a week or Never/Rarely) | 0.495 *** | |||
| Intrinsic Religiosity Score (Continuous) | 0.698 *** | |||
| Belief in God/Higher Power (Yes/Unsure or No) | 0.391 *** | |||
| Frequency of Seeing Provider (At least a few times a month or Never/Rarely) | 0.092 ** | |||
| Faith Tradition (Abrahamic or Non-Abrahamic/None) | 0.288 *** | |||
| Have Discussed RS with Current Provider (Yes or No) | 0.471 *** | |||
| Predictors | B | SE | β | t-Value |
| Intrinsic Religiosity Score | 1.02 | 0.06 | 0.50 | 16.78 *** |
| Have Discussed RS with Current Provider | 3.79 | 0.38 | 0.23 | 10.00 *** |
| Age | −0.05 | 0.01 | −0.10 | −4.51 *** |
| Gender (Female) | −1.38 | 0.33 | −0.09 | −4.22 *** |
| Organizing Religious Activity | 1.26 | 0.40 | 0.08 | 3.18 ** |
| Non-Organized Religious Activity | 1.17 | 0.41 | 0.08 | 2.84 ** |
| Frequency of Seeing Provider | 0.82 | 0.35 | 0.05 | 2.35 * |
| Belief in God/Higher Power | 1.54 | 0.70 | 0.05 | 2.21 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oxhandler, H.K.; Pargament, K.I.; Pearce, M.J.; Vieten, C.; Moffatt, K.M. Current Mental Health Clients’ Attitudes Regarding Religion and Spirituality in Treatment: A National Survey. Religions 2021, 12, 371. https://doi.org/10.3390/rel12060371
Oxhandler HK, Pargament KI, Pearce MJ, Vieten C, Moffatt KM. Current Mental Health Clients’ Attitudes Regarding Religion and Spirituality in Treatment: A National Survey. Religions. 2021; 12(6):371. https://doi.org/10.3390/rel12060371
Chicago/Turabian StyleOxhandler, Holly K., Kenneth I. Pargament, Michelle J. Pearce, Cassandra Vieten, and Kelsey M. Moffatt. 2021. "Current Mental Health Clients’ Attitudes Regarding Religion and Spirituality in Treatment: A National Survey" Religions 12, no. 6: 371. https://doi.org/10.3390/rel12060371
APA StyleOxhandler, H. K., Pargament, K. I., Pearce, M. J., Vieten, C., & Moffatt, K. M. (2021). Current Mental Health Clients’ Attitudes Regarding Religion and Spirituality in Treatment: A National Survey. Religions, 12(6), 371. https://doi.org/10.3390/rel12060371







