Prevalence of Migraine and Neuropathic Pain in Rheumatic Diseases
Abstract
1. Introduction
2. Methods
2.1. Ethical Considerations
2.2. Patients
2.3. Survey
2.4. Statistical Analysis
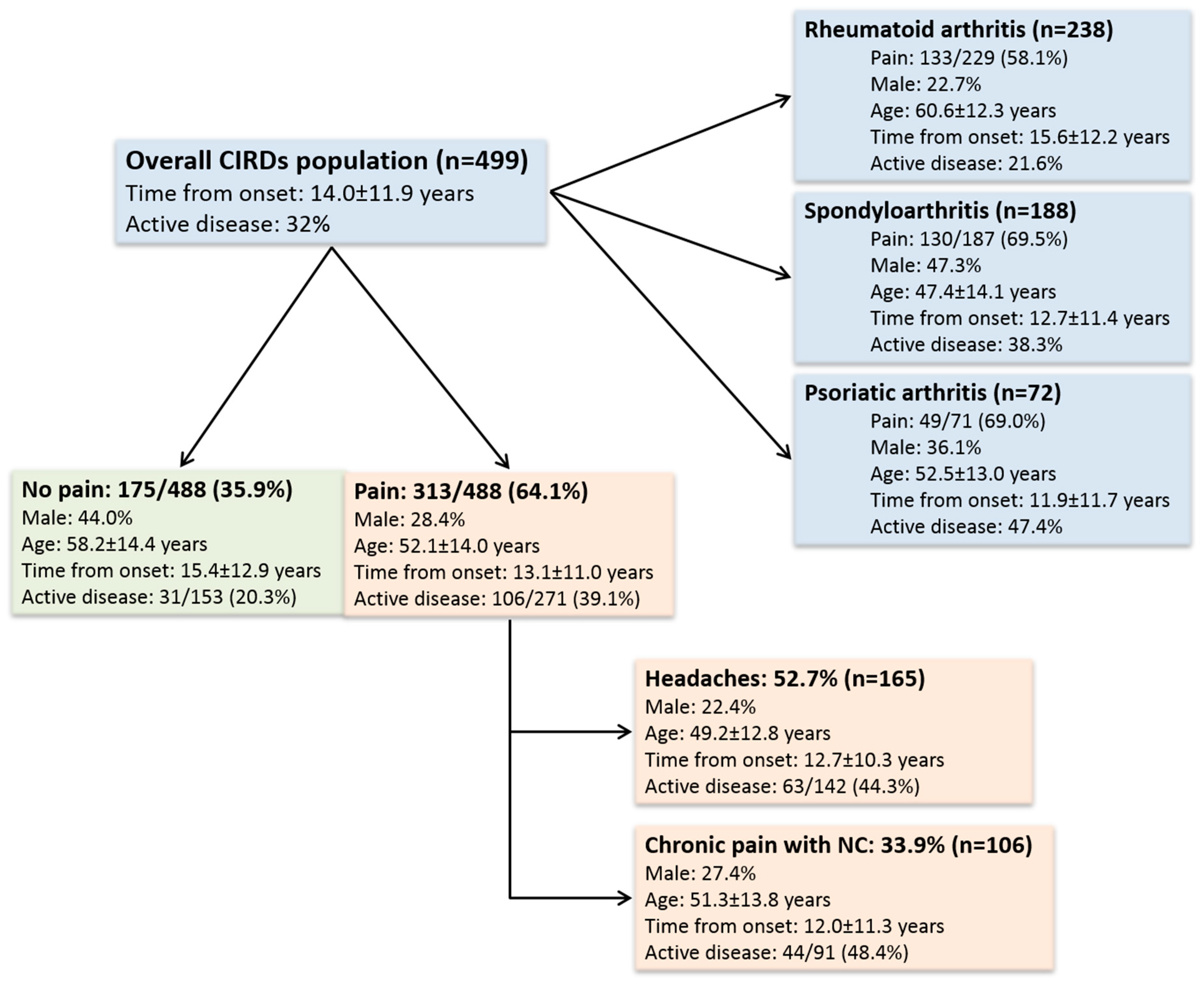
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| ACPA | Anti-citrullinated peptides’ antibodies |
| ASAS | Assessment of SpondyloArthritis International Society |
| BASDAI | Bath Ankylosing Spondylitis Disease Activity Index |
| BPI | Brief pain inventory |
| CIRDs | Chronic inflammatory rheumatic diseases |
| CRP | C-reactive protein |
| DAS28 | Disease Activity Score in 28 joints |
| ESR | Erythrocyte sedimentation rate |
| HAD | Hospital anxiety and depression |
| HAQ | Health assessment questionnaire |
| HIT-6 | Six-item Headache Impact Test |
| IHS | International Headache Society |
| IQR | Interquartile range |
| NSAID | Non-steroidal anti-inflammatory drug |
| PCS | Pain catastrophizing scale |
| PsA | Psoriatic arthritis |
| RA | Rheumatoid arthritis |
| RF | Rheumatoid factor |
| SD | Standard deviation |
| SpA | Spondyloarthritis |
| TNF | Tumor necrosis factor |
| VAS | Visual analogue scale |
References
- Smolen, J.S.; Landewe, R.; Breedveld, F.C.; Buch, M.; Burmester, G.; Dougados, M.; Emery, P.; Gaujoux-Viala, C.; Gossec, L.; Nam, J.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann. Rheum Dis. 2014, 73, 492–509. [Google Scholar] [CrossRef]
- Gaujoux-Viala, C.; Gossec, L.; Cantagrel, A.; Dougados, M.; Fautrel, B.; Mariette, X.; Nataf, H.; Saraux, A.; Trope, S.; Combe, B. Recommendations of the French Society for Rheumatology for managing rheumatoid arthritis. Jt. Bone Spine 2014, 81, 287–297. [Google Scholar] [CrossRef] [PubMed]
- Clauw, D.J. Fibromyalgia: A clinical review. JAMA 2014, 311, 1547–1555. [Google Scholar] [CrossRef] [PubMed]
- Fan, A.; Pereira, B.; Tournadre, A.; Tatar, Z.; Malochet-Guinamand, S.; Mathieu, S.; Couderc, M.; Soubrier, M.; Dubost, J.J. Frequency of concomitant fibromyalgia in rheumatic diseases: Monocentric study of 691 patients. Semin. Arthritis Rheum. 2017, 47, 129–132. [Google Scholar] [CrossRef]
- Duffield, S.J.; Miller, N.; Zhao, S.; Goodson, N.J. Concomitant fibromyalgia complicating chronic inflammatory arthritis: A systematic review and meta-analysis. Rheumatology 2018, 57, 1453–1460. [Google Scholar] [CrossRef]
- Pollard, L.C.; Kingsley, G.H.; Choy, E.H.; Scott, D.L. Fibromyalgic rheumatoid arthritis and disease assessment. Rheumatology 2010, 49, 924–928. [Google Scholar] [CrossRef]
- Almodovar, R.; Carmona, L.; Zarco, P.; Collantes, E.; Gonzalez, C.; Mulero, J.; Sueiro, J.L.; Gratacós, J.; Torre-Alonso, J.C.; Juanola, X.; et al. Fibromyalgia in patients with ankylosing spondylitis: Prevalence and utility of the measures of activity, function and radiological damage. Clin. Exp. Rheumatol. 2010, 28, S33–S39. [Google Scholar] [PubMed]
- Rifbjerg-Madsen, S.; Christensen, A.W.; Christensen, R.; Hetland, M.L.; Bliddal, H.; Kristensen, L.E.; Danneskiold-Samsøe, B.; Amris, K. Pain mechanisms in patients with inflammatory arthritis: A nationwide cross-sectional DANBIO registry survey. PLoS ONE 2017, 12, e0180014. [Google Scholar] [CrossRef] [PubMed]
- Koop, S.M.; Ten Klooster, P.M.; Vonkeman, H.E.; Steunebrink, L.M.; van de Laar, M.A. Prevalence and Cross-Sectional Associations of Neuropathic-Like Pain Features in Rheumatoid Arthritis. Arthritis Res. Ther. 2015, 17, 237. [Google Scholar] [CrossRef] [PubMed]
- Moisset, X.; Ouchchane, L.; Guy, N.; Bayle, D.J.; Dallel, R.; Clavelou, P. Migraine headaches and pain with neuropathic characteristics: Comorbid conditions in patients with multiple sclerosis. Pain 2013, 154, 2691–2699. [Google Scholar] [CrossRef]
- Dimitrova, A.K.; Ungaro, R.C.; Lebwohl, B.; Lewis, S.K.; Tennyson, C.A.; Green, M.W.; Babyatsky, M.W.; Green, P.H. Prevalence of migraine in patients with celiac disease and inflammatory bowel disease. Headache 2013, 53, 344–355. [Google Scholar] [CrossRef] [PubMed]
- Lantéri-Minet, M.; Valade, D.; Géraud, G.; Chautard, M.H.; Lucas, C. Migraine and probable migraine-results of FRAMIG 3, a French nationwide survey carried out according to the 2004 IHS classification. Cephalalgia 2005, 25, 1146–1158. [Google Scholar] [CrossRef] [PubMed]
- Bouhassira, D.; Lantéri-Minet, M.; Attal, N.; Laurent, B.; Touboul, C. Prevalence of chronic pain with neuropathic characteristics in the general population. Pain 2008, 136, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Zigmond, A.S.; Snaith, R.P. The hospital anxiety and depression scale. Acta Psychiatr. Scand. 1983, 67, 361–370. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, M.J.L.; Bishop, S.R.; Pivik, J. The Pain Catastrophizing Scale: Development and Validation. Psychol. Assess. 1995, 7, 524–532. [Google Scholar] [CrossRef]
- Moisset, X.; Bommelaer, G.; Boube, M.; Ouchchane, L.; Goutte, M.; Dapoigny, M.; Dallel, R.; Guttmann, A.; Clavelou, P.; Buisson, A. Migraine prevalence in inflammatory bowel disease patients: A tertiary-care centre cross-sectional study. Eur. J. Pain 2017, 21, 1550–1560. [Google Scholar] [CrossRef]
- Headache Classification Committee of the International Headache Society (IHS). The International Classification of Headache Disorders, 3rd edition (beta version). Cephalalgia 2013, 33, 629–808. [Google Scholar] [CrossRef]
- Kosinski, M.; Bayliss, M.S.; Bjorner, J.B.; Ware, J.E.; Garber, W.H.; Batenhorst, A.; Cady, R.; Dahlöf, C.G.; Dowson, A.; Tepper, S. A six-item short-form survey for measuring headache impact: The HIT-6. Qual. Life Res. 2003, 12, 963–974. [Google Scholar] [CrossRef]
- Finnerup, N.; Haroutounian, S.; Kamerman, P.; Baron, R.; Bennett, D.; Bouhassira, D.; Cruccu, G.; Freeman, R.; Hansson, P.; Nurmikko, T.; et al. Neuropathic Pain: An Updated Grading System for Research and Clinical Practice. Pain 2016, 157, 1599–1606. [Google Scholar] [CrossRef]
- Bouhassira, D.; Attal, N.; Alchaar, H.; Boureau, F.; Brochet, B.; Bruxelle, J.; Cunin, G.; Fermanian, J.; Ginies, P.; Grun-Overdyking, A.; et al. Comparison of pain syndromes associated with nervous or somatic lesions and development of a new neuropathic pain diagnostic questionnaire (DN4). Pain 2005, 114, 29–36. [Google Scholar] [CrossRef]
- Cleeland, C.S.; Ryan, K.M. Pain assessment: Global use of the Brief Pain Inventory. Ann. Acad. Med. Singap. 1994, 23, 129–138. [Google Scholar] [PubMed]
- Le, H.; Tfelt-Hansen, P.; Russell, M.B.; Skytthe, A.; Kyvik, K.O.; Olesen, J. Co-morbidity of migraine with somatic disease in a large population-based study. Cephalalgia 2011, 31, 43–64. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; Huang, Y.P.; Wang, M.T.; Wang, H.I.; Pan, S.L. Increased risk of rheumatoid arthritis in patients with migraine: A population-based, propensity score-matched cohort study. Rheumatol. Int. 2017, 37, 273–279. [Google Scholar] [CrossRef] [PubMed]
- Möhrke, J.; Kropp, P.; Zettl, U.K. Headaches in multiple sclerosis patients might imply an inflammatorial process. PLoS ONE 2013, 8, e69570. [Google Scholar] [CrossRef] [PubMed]
- Graziano, E.; Hagemeier, J.; Weinstock-Guttman, B.; Ramasamy, D.P.; Zivadinov, R. Increased contrast enhancing lesion activity in relapsing-remitting multiple sclerosis migraine patients. Neuroimage Clin. 2015, 9, 110–116. [Google Scholar] [CrossRef]
- Soubrier, M.; Haïk, S.; Hauw, J.J.; Corvol, J.C.; Lyon-Caen, O.; Dougados, M. Creutzfeldt-Jakob disease in a patient treated by etanercept for rheumatoid arthritis (RA): Just a coincidence? Jt. Bone Spine 2010, 77, 174–175. [Google Scholar] [CrossRef]
- Kumar, N.; Abboud, H. Iatrogenic CNS demyelination in the era of modern biologics. Mult. Scler. 2019, 25, 1079–1085. [Google Scholar] [CrossRef]
- Liedorp, M.; Voskuyl, A.E.; Van Oosten, B.W. Axonal neuropathy with prolonged sulphasalazine use. Clin. Exp. Rheumatol. 2008, 26, 671–672. [Google Scholar]
- Price, T.R. Sensorimotor neuropathy with sulphasalazine. Postgrad. Med. J. 1985, 61, 147–148. [Google Scholar] [CrossRef][Green Version]
- Smith, M.D.; Gibson, G.E.; Rowland, R. Combined hepatotoxicity and neurotoxicity following sulphasalazine administration. Aust. N. Z. J. Med. 1982, 12, 76–80. [Google Scholar] [CrossRef]
- Berti-Mattera, L.N.; Kern, T.S.; Siegel, R.E.; Nemet, I.; Mitchell, R. Sulfasalazine blocks the development of tactile allodynia in diabetic rats. Diabetes 2008, 57, 2801–2808. [Google Scholar] [CrossRef]
- Ryu, B.R.; Lee, Y.A.; Won, S.J.; Noh, J.H.; Chang, S.Y.; Chung, J.M.; Choi, J.S.; Joo, C.K.; Yoon, S.H.; Gwag, B.J. The novel neuroprotective action of sulfasalazine through blockade of NMDA receptors. J. Pharmacol. Exp. Ther. 2003, 305, 48–56. [Google Scholar] [CrossRef]
- Salaffi, F.; Di Carlo, M.; Carotti, M.; Sarzi-Puttini, P. The Effect of Neuropathic Pain Symptoms on Remission in Patients with Early Rheumatoid Arthritis. Curr. Rheumatol Rev. 2019, 15, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Ifergane, G.; Buskila, D.; Simiseshvely, N.; Zeev, K.; Cohen, H. Prevalence of fibromyalgia syndrome in migraine patients. Cephalalgia 2006, 26, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Penn, I.W.; Chuang, E.; Chuang, T.Y.; Lin, C.L.; Kao, C.H. Bidirectional association between migraine and fibromyalgia: Retrospective cohort analyses of two populations. BMJ Open 2019, 9, e026581. [Google Scholar] [CrossRef] [PubMed]
- Whealy, M.; Nanda, S.; Vincent, A.; Mandrekar, J.; Cutrer, F.M. Fibromyalgia in migraine: A retrospective cohort study. J. Headache Pain 2018, 19, 61. [Google Scholar] [CrossRef]
- Akdag Uzun, Z.; Kurt, S.; Karaer Unaldi, H. The relationship with restless legs syndrome, fibromyalgia, and depressive symptoms in migraine patients. Neurol. Sci. 2018, 39, 1409–1414. [Google Scholar] [CrossRef]
- Di Carlo, M.; Becciolini, A.; Lato, V.; Crotti, C.; Favalli, E.; Salaffi, F. The 12-item Psoriatic Arthritis Impact of Disease Questionnaire: Construct Validity, Reliability, and Interpretability in a Clinical Setting. J. Rheumatol. 2017, 44, 279–285. [Google Scholar] [CrossRef] [PubMed]
- Brikman, S.; Furer, V.; Wollman, J.; Borok, S.; Matz, H.; Polachek, A.; Elalouf, O.; Sharabi, A.; Kaufman, I.; Paran, D.; et al. The Effect of the Presence of Fibromyalgia on Common Clinical Disease Activity Indices in Patients with Psoriatic Arthritis: A Cross-sectional Study. J. Rheumatol. 2016, 43, 1749–1754. [Google Scholar] [CrossRef]
- Alvarez-Astorga, A.; García-Azorín, D.; Hernández, M.; de la Red, H.; Sotelo, E.; Uribe, F.; Guerrero, A.L. Pain catastrophising in a population of patients with migraine. Neurologia 2019. [Google Scholar] [CrossRef]
| Characteristic | All Patients N = 499 | RA N = 238 | SpA N = 188 | PsA N = 72 | p Value |
|---|---|---|---|---|---|
| Age, years [range] | 54.5 ± 14.4 [18–87] | 60.6 ± 12.3 [27–87] | 47.4 ± 14.1 [18–85] | 52.5 ± 13.0 [22–87] | <0.001 |
| Men, n (%) | 170 (34.1%) | 54 (22.7%) | 89 (47.3%) | 26 (36.1%) | <0.001 |
| Smokers, n (%) | 104 (23.2%) | 42 (17.6%) | 45 (23.9%) | 17 (23.6%) | 0.49 |
| Fibromyalgia, n (%) | 32 (6.4%) | 9 (3.7%) | 16 (8.5%) | 7 (9.7%) | 0.14 |
| Obesity, n (%) | 95 (19.0%) | 39 (16.4%) | 33 (17.6%) | 22 (30.6%) | 0.008 |
| Osteoarthritis, n (%) | 89 | 47 | 26 | 16 | 0.28 |
| Gougerot-Sjogren, n (%) | 10 (2.0%) | 9 (3.7%) | 0 (0.0%) | 1 (1.4%) | 0.049 |
| Depression, n (%) | 41 (8.2%) | 17 (7.1%) | 20 (10.6%) | 4 (5.6%) | 0.46 |
| Disease duration, years | 11.2 [4.9–20.0] | 14.0 [6.1–21.1] | 9.0 [4.5–18.2] | 9.5 [4.0–15.3] | 0.01 |
| Active disease, n (%) | 42/194 (21.6%) | 70/183 (38.3%) | 27/57 (47.4%) | ||
| DAS28 ESR score | 2.34 ± 1.23 | 2.39 ± 1.38 | |||
| BASDAI, mm | 33.6 ± 20.2 | 33.8 ± 20.5 | |||
| CRP, mg/L | 3.0 [1.3–6.0] | 3.0 [1.2–6.5] | 2.9 [1.2–4.7] | 3.0 [2.4–7.7] | 0.11 |
| HAQ score | 0.58 ± 0.60 | 0.64 ± 0.67 | 0.52 ± 0.53 | 0.52 ± 0.53 | 0.09 |
| HAD Anxiety score | 7.8 ± 4.0 | 7.7 ± 4.2 | 8.1 ± 3.7 | 7.8 ± 4.0 | 0.81 |
| PCS score | 15.5 ± 11.5 | 14.1 ± 11.5 | 16.8 ± 11.3 | 15.8 ± 11.3 | 0.22 |
| HAD Depression score | 5.3 ± 3.9 | 5.0 ± 3.6 | 5.7 ± 4.3 | 4.9 ± 3.5 | 0.94 |
| Treatments | |||||
| Pain treatment, n (%) | 112 (22.4%) | 50 (21.0%) | 38 (20.2%) | 24 (33.3%) | 0.11 |
| NSAID, n (%) | 108 (21.6%) | 30 (12.6%) | 61 (32.4%) | 17 (23.6%) | <0.001 |
| Corticosteroid, n (%) | 53 (10.6%) | 46 (19.3%) | 5 (2.7%) | 2 (2.8%) | <0.001 |
| Methotrexate, n (%) | 234 (46.9%) | 163 (68.4%) | 34 (18.1%) | 36 (50.0%) | <0.001 |
| Sulfasalazine, n (%) | 23 (4.6%) | 7 (2.9%) | 10 (5.3%) | 6 (8.3%) | 0.26 |
| Leflunomide, n (%) | 19 (3.8%) | 15 (6.3%) | 3 (1.6%) | 1 (1.4%) | 0.051 |
| Anti-TNF-alpha, n (%) | 241 (48.3%) | 77 (32.4%) | 130 (69.1%) | 33 (45.8%) | <0.001 |
| Hydroxychloroquine, n (%) | 59 (11.8%) | 57 (23.9%) | 1 (0.05%) | 0 (0.0%) | |
| Tocilizumab, n (%) | 23 (4.6%) | 23 (9.7%) | 0 (0.0%) | 0 (0.0%) | |
| Abatacept, n (%) | 7 (1.4%) | 7 (2.9%) | 0 (0.0%) | 0 (0.0%) | |
| Rituximab, n (%) | 288 (5.6%) | 27 (11.3%) | 0 (0.0%) | 0 (0.0%) | |
| Ustekinumab, n (%) | 7/499 (1.4%) | 0/238 (0.0%) | 5 (2.7%) | 2 (2.8%) | |
| Strict Migraine, n (%) | 64/484 (13.2%) | 23/203 (11.3%) | 26/186 (14.0%) | 15/71 (21.1%) | 0.12 |
| Strict + probable migraine, n (%) | 165/484 (34.0%) | 62/226 (27.4%) | 71/186 (38.2%) | 32/71 (45.1%) | 0.02 |
| Neuropathic pain, n (%) | 106/493 (21.5%) | 41/233 (17.6%) | 50/187 (26.7%) | 14/72 (19.4%) | 0.02 |
| Parameter | Patients with Migraine n = 165 | Patients without Migraine n = 324 | Univariate p-Value OR [95%CI] | Multivariable p-Value OR [95%CI] |
|---|---|---|---|---|
| Age, years [range] | 49.2 ± 12.8 [20–82] | 56.7 ± 14.7 [18–87] | p < 0.001 OR = 0.96 [0.95–0.97] | p = 0.002 OR = 0.97 [0.95–0.99] |
| Female, n (%) | 128/165 (77.6%) | 190/319 (59.6%) | p < 0.001 OR = 2.34 [1.54–3.64] | p < 0.001 OR = 3.65 [2.01–6.84] |
| Smokers, n (%) | 39 (26.7%) | 64 (22.2%) | p = 0.78 OR = 1.03 [0.81–1.31] | |
| VAS for disease activity, mm | 34.0 ± 25.7 | 25.4 ± 24.0 | p < 0.001 OR = 1.01 [1.00–1.02] | p = 0.44 OR = 1.00 [0.99–1.02] |
| CRP, mg/L | 3.0 [1.4–6.3] | 2.9 [1.2–6.0] | p = 0.90 OR = 1.0 [0.98–1.02] | |
| Disease duration, years | 12.7 [4.8–18.8] | 12.6 [5.0–20.1] | p = 0.08 OR = 0.99 [0.96–1.00] | p = 0.85 OR = 1.00 [0.98–1.03] |
| HAD Anxiety score | 9.5 ± 4.0 | 6.85 ± 3.6 | p < 0.001 OR = 1.20 [1.14–1.27] | p = 0.003 OR = 1.13 [1.04–1.23] |
| HAD Depression score | 6.4 ± 4.2 | 4.66 ± 3.6 | p < 0.001 OR = 1.12 [1.07–1.18] | p = 0.46 OR = 1.03 [0.95–1.12] |
| PCS score | 17.8 ± 11.4 | 13.9 ± 11.2 | p = 0.001 OR = 1.03 [1.01–1.05] | p = 0.95 OR = 1.00 [0.97–1.02] |
| Pain treatment *, n (%) | 46/165 (27.9%) | 60/319 (19%) | p = 0.02 OR = 1.67 [1.07–2.59] | p = 0.20 OR = 1.56 [0.79–3.06] |
| Anti-TNF-alpha treatment *, n (%) | 96/156 (58.2%) | 143/319 (44.8%) | p = 0.005 OR = 1.71 [1.17–2.51] | p = 0.017 OR = 1.90 [1.13–3.25] |
| Neuropathic pain, n (%) | 62/165 (37.6%) | 43/318 (13.5%) | p < 0.001 OR = 3.85 [2.46–6.06] | p = 0.005 OR = 2.49 [1.32–4.71] |
| Parameters | Patients with Migraine n = 62 | Patients without Migraine n = 164 | Univariate p Value OR [95%CI] | Multivariable p Value OR [95%CI] |
|---|---|---|---|---|
| Age, years [range] | 56.2 ± 11.0 [30–76] | 61.8 ± 12.5 [27–87] | p = 0.003 OR = 0.96 [0.94–0.99] | p = 0.03 OR = 0.96 [0.93–0.99] |
| Female | 54/62 (87.1%) | 121/164 (73.8%) | p = 0.001 OR = 2.4 [1.1–5.8] | p = 0.59 OR = 1.42 [0.43–5.67] |
| Smokers | 13/56 (23.2%) | 28/150 (18.7%) | p = 0.15 OR = 1.30 [0.91–1.84] | |
| DAS28 ESR score | 2.74 ± 1.19 | 2.24 ± 1.33 | p = 0.02 OR = 1.37 [1.05–1.80] | p = 0.08 OR = 1.35 [0.97–1.89] |
| CRP, mg/L | 3.0 [1.8–6.3] | 2.9 [1.0–6.6] | p = 0.42 OR = 1.02 [0.97–1.06] | |
| Disease duration, years | 12.4 [5.0–20.3] | 14.7 [7.0–21.7] | p = 0.26 OR = 0.99 [0.96–1.01] | |
| Erosive RA | 26/62 (41.9%) | 78/164 (47.5%) | p = 0.45 OR = 0.80 [0.44–1.43] | |
| RF and/or ACPA positive | 49/62 (79.0%) | 127/160 (77.4%) | p = 0.80 OR = 1.01 [0.55–2.30] | |
| HAD Anxiety score | 9.3 ± 4.6 | 6.9 ± 3.66 | p < 0.001 OR = 1.16 [1.08–1.25] | p = 0.83 OR = 0.99 [0.86–1.12] |
| HAD Depression score | 6.5 ± 4.2 | 4.4 ±3.27 | p < 0.001 OR = 1.16 [1.07–1.26] | p = 0.03 OR = 1.14 [1.01–1.30] |
| PCS score | 17.2 ± 12.0 | 12.5 ±10.9 | p = 0.02 OR = 1.04 [1.01–1.07] | p = 0.48 OR = 1.01 [0.98–1.05] |
| Parameter | Patients with Migraine n = 71 | Patients without Migraine n = 115 | Univariate p Value OR [95%CI] | Multivariable p Value OR [95%CI] |
|---|---|---|---|---|
| Age, years [range] | 44.8 ± 12.9 [20–82] | 48.8 ± 14.6 [18–85] | p = 0.06 OR= 0.98 [0.96–1.00] | p = 0.15 OR= 0.98 [0.96–1.01] |
| Female | 49/71(69.0%) | 49/115 (57.4%) | p < 0.001 OR= 3.0 [1.62–5.70] | p = 0.01 OR = 2.5 [1.3–5.2] |
| Smokers | 22/62 (35.5%) | 26/101 (25.7%) | p = 0.55 OR= 1.12 [0.76–1.66] | |
| BASDAI, mm | 41.5 ± 19.4 | 28.8 ± 19.4 | p < 0.001 OR = 1.03 [1.02–1.05] | p = 0.004 OR= 1.03 [1.01–1.05] |
| CRP, mg/L | 2.9 [1.0–4.3] | 2.9 [1.4–4.7] | p = 0.66 OR= 0.99 [0.96–1.02] | |
| Disease duration, years | 6.6 [4.7–15.4] | 9.9 [3.7–18.5] | p = 0.13 OR= 0.98 [0.95–1.00] | |
| HAD Anxiety score | 9.5 ± 3.6 | 7.1 ± 3.5 | p < 0.001 OR = 1.20 [1.10–1.31] | p = 0.004 OR = 1.19 [1.06–1.34] |
| HAD Depression score | 6.4 ± 4.4 | 5.2 ± 4.2 | p = 0.06 OR= 1.07 [0.99–1.14] | p = 0.23 OR= 0.94 [0.84–1.04] |
| PCS score | 18.4 ± 10.6 | 15.7 ± 11.8 | p = 0.15 OR= 1.02 [0.99–1.05] |
| Parameter | All Patients N = 165 | RA N = 62 | SpA N = 71 | PsA N = 32 | p Value |
|---|---|---|---|---|---|
| Age, years [range] | 49.2 ± 12.8 [20–82] | 56.2 ± 11.0 [30–76] | 44.8 ± 12.9 [20–82] | 45.5 ± 9.8 [22–63] | p < 0.001 |
| Men, n (%) | 37/165 (22.4%) | 8/62 (12.9%) | 22/71 (31.0%) | 7/32 (21.9%) | p = 0.04 |
| HIT-6 > 55, n (%) | 120/165 (72.7%) | 46/62 (74.2%) | 49/71 (69.0%) | 25/32 (78.1%) | p = 0.60 |
| Headaches ≥ 15 d/month, n (%) | 18/149 (12.1%) | 9/53 (17.0%) | 7/69 (10.1%) | 2/27 (7.4%) | p = 0.28 |
| Headaches 8–14 d/month, n (%) | 22/149 (14.8%) | 4/53 (7.5%) | 12/69 (17.4%) | 6/27 (22.2%) | |
| Headaches < 8 d/month, n (%) | 109/149 (73.2%) | 40/53 (75.5%) | 50/69 (72.5%) | 19/27 (70.4%) |
| Parameter | Patients with Neuropathic Pain n = 106 | Patients without Neuropathic Pain n = 392 | Univariate p Value OR [95%CI] | Multivariable p Value OR [95%CI] |
|---|---|---|---|---|
| Age, years [range] | 51.3 ± 13.8 [22–82] | 55.4 ± 14.5 [18–87] | p = 0.01 OR = 0.96 [0.95–0.98] | p = 0.26 OR = 1.00 [0.96–1.01] |
| Female | 77/106 (72.6%) | 252/392 (64.3%) | p = 0.11 OR = 1.48 [0.93–2.40] | |
| Smokers | 29/99 (29.3%) | 74/349 (21.2%) | p = 0.87 OR = 1.02 [0.78–1.33] | |
| VAS disease activity, mm | 39.4 ± 26.0 | 24.9 ± 23.6 | p < 0.001 OR = 1.02 [1.01–1.03] | p = 0.02 OR = 1.00 [1.00–1.03] |
| CRP, mg/L | 3.0 [1.3–5.7] | 3.0 [1.3–6.0] | p = 0.91 OR = 1.00 [0.97–1.02] | |
| Disease duration, years | 7.9 [4.5–17.9] | 12.6 [5.1–20.3] | p = 0.06 OR = 0.98 [0.96–1.00] | p = 0.06 OR = 1.01 [0.94–1.03] |
| HAQ | 0.86 ± 0.64 | 0.51 ± 0.57 | p < 0.001 OR = 2.44 [1.73–3.47] | p = 0.01 OR = 1.43 [1.18–3.50] |
| HAD Anxiety score | 9.4 ± 3.8 | 7.4 ± 3.9 | p < 0.001 OR = 1.13 [1.07–1.19] | p = 0.13 OR = 1.00 [0.98–1.17] |
| HAD Depression score | 6.9 ± 4.1 | 4.8 ± 3.7 | p < 0.001 OR = 1.14 [1.08–1.20] | p = 0.47 OR = 1.13 [0.94–1.13] |
| PCS score | 18.6 ± 10.9 | 14.6 ± 11.5 | p = 0.003 OR= 1.03 [1.01–1.05] | p = 0.71 OR = 1.00 [0.97–1.02] |
| NSAID Treatment * | 30/106 (28.3%) | 78/392 (20.0%) | p = 0.06 OR = 1.59 [0.96-2.58] | p = 0.13 OR = 0.97 [0.85-3.21] |
| Pain Treatment * | 35/106 (33.0%) | 77/392 (19.6%) | p = 0.004 OR = 2.01 [1.25-3.23] | p = 0.19 OR = 1.56 [0.79-3.09] |
| Sulfasalazine Treatment * | 9/106 (8.5%) | 14/392 (3.6%) | p = 0.04 OR = 2.51 [1.02–5.89] | p = 0.04 OR = 1.90 [1.05–12.7] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mathieu, S.; Couderc, M.; Pereira, B.; Dubost, J.-J.; Malochet-Guinamand, S.; Tournadre, A.; Soubrier, M.; Moisset, X. Prevalence of Migraine and Neuropathic Pain in Rheumatic Diseases. J. Clin. Med. 2020, 9, 1890. https://doi.org/10.3390/jcm9061890
Mathieu S, Couderc M, Pereira B, Dubost J-J, Malochet-Guinamand S, Tournadre A, Soubrier M, Moisset X. Prevalence of Migraine and Neuropathic Pain in Rheumatic Diseases. Journal of Clinical Medicine. 2020; 9(6):1890. https://doi.org/10.3390/jcm9061890
Chicago/Turabian StyleMathieu, Sylvain, Marion Couderc, Bruno Pereira, Jean-Jacques Dubost, Sandrine Malochet-Guinamand, Anne Tournadre, Martin Soubrier, and Xavier Moisset. 2020. "Prevalence of Migraine and Neuropathic Pain in Rheumatic Diseases" Journal of Clinical Medicine 9, no. 6: 1890. https://doi.org/10.3390/jcm9061890
APA StyleMathieu, S., Couderc, M., Pereira, B., Dubost, J.-J., Malochet-Guinamand, S., Tournadre, A., Soubrier, M., & Moisset, X. (2020). Prevalence of Migraine and Neuropathic Pain in Rheumatic Diseases. Journal of Clinical Medicine, 9(6), 1890. https://doi.org/10.3390/jcm9061890






