Decreased Cerebrospinal Fluid Orexin-A (Hypocretin-1) Concentrations in Patients after Generalized Convulsive Status Epilepticus
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Biochemical Analysis
2.3. Statistical Analysis
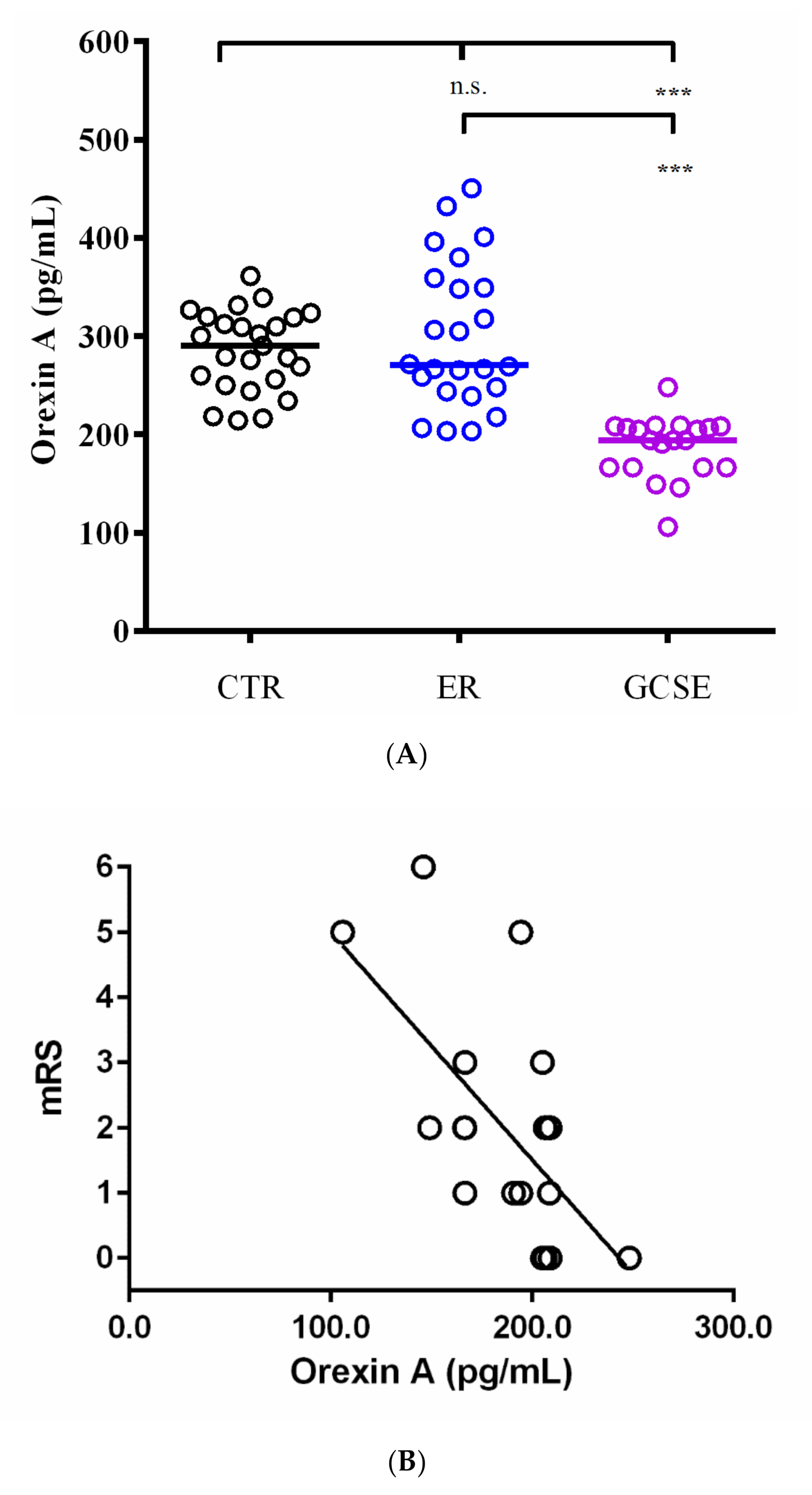
3. Results
3.1. Demographics and Clinical Characteristics
3.2. Biochemical and Clinical Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Betjemann, J.P.; Lowenstein, D.H. Status epilepticus in adults. Lancet Neurol. 2015, 14, 615–624. [Google Scholar] [CrossRef]
- Kornum, B.R.; Faraco, J.; Mignot, E. Narcolepsy with hypocretin/orexin deficiency, infections and autoimmunity of the brain. Curr. Opin. Neurobiol. 2011, 21, 897–903. [Google Scholar] [CrossRef] [PubMed]
- Ng, M.C. Orexin and Epilepsy: Potential Role of REM Sleep. Sleep 2017, 40, zsw061. [Google Scholar] [CrossRef] [PubMed]
- Kortunay, S.; Erken, H.A.; Erken, G.; Genç, O.; Sahiner, M.; Turgut, S.; Turgut, G. Orexins increase penicillin-induced epileptic activity. Peptides 2012, 34, 419–422. [Google Scholar] [CrossRef] [PubMed]
- Ni, L.Y.; Zhu, M.J.; Song, Y.; Liu, X.M.; Tang, J.Y. Pentylenetetrazol-induced seizures are exacerbated by sleep deprivation through orexin receptor-mediated hippocampal cell proliferation. Neurol. Sci. 2014, 35, 245–252. [Google Scholar] [CrossRef] [PubMed]
- Goudarzi, E.; Elahdadi-Salmani, M.; Lashkarbolouki, T.; Goudarzi, I. Hippocampal orexin receptors inactivation reduces PTZ induced seizures of male rats. Pharmacol. Biochem. Behav. 2015, 130, 77–83. [Google Scholar] [CrossRef]
- Socała, K.; Szuster-Ciesielska, A.; Wlaź, P. SB 334867, a selective orexin receptor type 1 antagonist, elevates seizure threshold in mice. Life Sci. 2016, 150, 81–88. [Google Scholar] [CrossRef]
- Asadi, S.; Roohbakhsh, A.; Shamsizadeh, A.; Fereidoni, M.; Kordijaz, E.; Moghimi, A. The effect of intracerebroventricular administration of orexin receptor type 2 antagonist on pentylenetetrazol-induced kindled seizures and anxiety in rats. BMC Neurosci. 2018, 19, 49. [Google Scholar] [CrossRef]
- Rejdak, K.; Papuć, E.; Grieb, P.; Stelmasiak, Z. Decreased cerebrospinal fluid hypocretin-1 (orexin A) in patients after repetitive generalized tonic-clonic seizures. Epilepsia 2009, 50, 1641–1644. [Google Scholar] [CrossRef]
- Trinka, E.; Cock, H.; Hesdorffer, D.; Rossetti, A.O.; Scheffer, I.E.; Shinnar, S.; Shorvon, S.; Lowenstein, D.H. A definition and classification of status epilepticus—Report of the ILAE Task Force on Classification of Status Epilepticus. Epilepsia 2015, 56, 1515–1523. [Google Scholar] [CrossRef]
- Jędrzejczak, J.; Mazurkiewicz-Bełdzińska, M.; Szmuda, M.; Majkowska-Zwolińska, B.; Steinborn, B.; Ryglewicz, D.; Owczuk, R.; Bartkowska-Śniatkowska, A.; Widera, E.; Rejdak, K.; et al. Convulsive status epilepticus management in adults and children: Report of the Working Group of the Polish Society of Epileptology. Neurol. Neurochir. Pol. 2018, 52, 419–426. [Google Scholar] [CrossRef] [PubMed]
- Bonita, R.; Beaglehole, R. Modification of Rankin Scale: Recovery of motor function after stroke. Stroke 1988, 19, 1497–1500. [Google Scholar] [CrossRef] [PubMed]
- Mignot, E.; Lammers, G.J.; Ripley, B.; Okun, M.; Nevsimalova, S.; Overeem, S.; Vankova, J.; Black, J.; Harsh, J.; Bassetti, C.; et al. The role of cerebrospinal fluid hypocretin measurement in the diagnosis of narcolepsy and other hypersomnias. Arch. Neurol. 2002, 59, 1553–1562. [Google Scholar] [CrossRef]
- Hagan, J.J.; Leslie, R.A.; Patel, S.; Evans, M.L.; Wattam, T.A.; Holmes, S.; Benham, C.D.; Taylor, S.G.; Routledge, C.; Hemmati, P.; et al. Orexin A activates locus coeruleus cell firing and increases arousal in the rat. Proc. Natl. Acad. Sci. USA 1999, 96, 10911–10926. [Google Scholar] [CrossRef] [PubMed]
- Ida, T.; Nakahara, K.; Katayama, T.; Murakami, N.; Nakazato, M. Effect of lateral cerebroventricular injection of the appetite-stimulating neuropeptide, orexin and neuropeptide Y, on the various behavioral activities of rats. Brain Res. 1999, 821, 526–529. [Google Scholar] [CrossRef]
- Selbach, O.; Doreulee, N.; Bohla, C.; Eriksson, K.S.; Sergeeva, O.A.; Poelchen, W.; Brown, R.E.; Haas, H.L. Orexins/hypocretins cause sharp wave- and theta-related synaptic plasticity in the hippocampus via glutamatergic, gabaergic, noradrenergic, and cholinergic signaling. Neuroscience 2004, 127, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Morales, A.; Bonnet, C.; Bourgoin, N.; Touvier, T.; Nadam, J.; Laglaine, A.; Navarro, F.; Moulin, C.; Georges, B.; Pequignot, J.M.; et al. Unexpected expression of orexin-B in basal conditions and increased levels in the adult rat hippocampus during pilocarpine-induced epileptogenesis. Brain Res. 2006, 1109, 164–175. [Google Scholar] [CrossRef]
- Kushikata, T.; Hirota, K.; Yoshida, H.; Kudo, M.; Lambert, D.G.; Smart, D.; Jerman, J.C.; Matsuki, A. Orexinergic neurons and barbiturate anesthesia. Neuroscience 2003, 121, 855–863. [Google Scholar] [CrossRef]
- He, Y.; Kudo, M.; Kudo, T.; Kushikata, T.; Li, E.; Hirota, K. The effects of benzodiazepines on orexinergic systems in rat cerebrocortical slices. Anesth. Analg. 2007, 104, 338–340. [Google Scholar] [CrossRef][Green Version]
- Ripley, B.; Overeem, S.; Fujiki, N.; Nevsimalova, S.; Uchino, M.; Yesavage, J.; Di Monte, D.; Dohi, K.; Melberg, A.; Lammers, G.J.; et al. CSF hypocretin/orexin levels in narcolepsy and other neurological conditions. Neurology 2001, 57, 2253–2258. [Google Scholar] [CrossRef]
- Rejdak, K.; Petzold, A.; Lin, L.; Smith, M.; Kitchen, N.; Thompson, E.J. Decreased CSF hypocretin-1 (orexin-A) after acute haemorrhagic brain injury. J. Neurol. Neurosurg. 2005, 76, 597–598. [Google Scholar] [CrossRef] [PubMed][Green Version]
| Characteristics | CTR | ER | GCSE | p-Value |
|---|---|---|---|---|
| n | 25 | 24 | 20 | NA |
| Age (median, range; years) | 43 (25–70) | 41 (26–73) | 46 (23–71) | n.s. |
| Gender (F/M) | 13–12 month | 14–10 month | 11–9 month | n.s. |
| Epilepsy diagnosis before admission (n, %) | 0 (0%) | 24 (100%) | 13 (65%) | NA |
| Duration since epilepsy diagnosis (median, range; years) | n/A | 10 (2–15) | 5 (0–14]) | NA |
| Etiology (n, %) | ||||
| -unknown | n/A | 20 (83%) | 6 (46%) | NA |
| -structural | n/A | 4 (17%) | 7 (54%) | |
| -other | n/A | 0 (0%) | 0 (0%) |
| Characteristics | GCSE Group |
|---|---|
| n | 20 |
| SE duration (median, range, hours) | 8 (1–72) |
| Time elapsed between CSF collection and SE cessation (days, median, range) | 3 (1–9) |
| Treatments for GCSE | |
| -benzodiazepines | 20 (100%) |
| -intravenous valproic acid | 13 (90%) |
| -intravenous phenytoin | 5 (25%) |
| -intravenous anesthetics | 5 (25%) |
| Outcome at 3-month follow-up | |
| -good outcome (0–2 mRS) | 15 (75%) |
| -poor outcome (3–5 mRS) | 4 (20%) |
| -death (6 mRS) | 1 (5%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Samzadeh, M.; Papuć, E.; Furtak-Niczyporuk, M.; Rejdak, K. Decreased Cerebrospinal Fluid Orexin-A (Hypocretin-1) Concentrations in Patients after Generalized Convulsive Status Epilepticus. J. Clin. Med. 2020, 9, 3354. https://doi.org/10.3390/jcm9103354
Samzadeh M, Papuć E, Furtak-Niczyporuk M, Rejdak K. Decreased Cerebrospinal Fluid Orexin-A (Hypocretin-1) Concentrations in Patients after Generalized Convulsive Status Epilepticus. Journal of Clinical Medicine. 2020; 9(10):3354. https://doi.org/10.3390/jcm9103354
Chicago/Turabian StyleSamzadeh, Mojdeh, Ewa Papuć, Marzena Furtak-Niczyporuk, and Konrad Rejdak. 2020. "Decreased Cerebrospinal Fluid Orexin-A (Hypocretin-1) Concentrations in Patients after Generalized Convulsive Status Epilepticus" Journal of Clinical Medicine 9, no. 10: 3354. https://doi.org/10.3390/jcm9103354
APA StyleSamzadeh, M., Papuć, E., Furtak-Niczyporuk, M., & Rejdak, K. (2020). Decreased Cerebrospinal Fluid Orexin-A (Hypocretin-1) Concentrations in Patients after Generalized Convulsive Status Epilepticus. Journal of Clinical Medicine, 9(10), 3354. https://doi.org/10.3390/jcm9103354






