Managed Care after Acute Myocardial Infarction (MC-AMI) Reduces Total Mortality in 12-Month Follow-Up—Results from a Poland’s National Health Fund Program of Comprehensive Post-MI Care—A Population-Wide Analysis
Abstract
1. Introduction
2. Materials and Methods
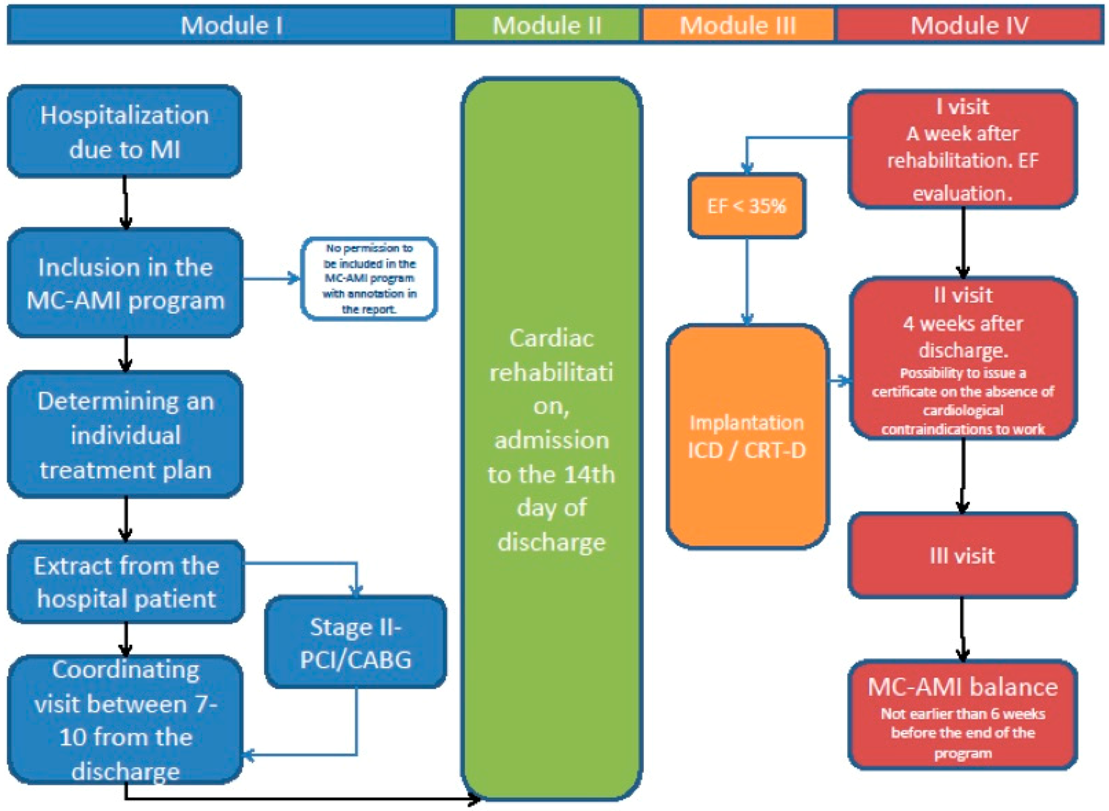
MC-AMI—Program Description and Definitions
3. Results
3.1. Primary End-Point
3.2. Components of MC-AMI
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Schmidt, M.; Jacobsen, J.B.; Lash, T.L.; Bøtker, H.E.; Sørensen, H.T. 25 years trends in first hospitalization for acute myocardial infarction, subsequent short and long term mortality, and the prognostic impact of sex and comorbidity: A Danish nationwide cohort study. BMJ 2012, 344, e356. [Google Scholar] [CrossRef] [PubMed]
- Smolina, K.; Wright, F.L.; Rayner, M.; Goldacre, M.J. Long-term survival and recurrence after acute myocardial infarction in England, 2004 to 2010. Circ. Cardiovasc. Qual. Outcomes 2012, 5, 532–540. [Google Scholar] [CrossRef] [PubMed]
- Freisinger, E.; Fuerstenberg, T.; Malyar, N.M.; Wellmann, J.; Keil, U.; Breithardt, G.; Reinecke, H. German nationwide data on current trends and management of acute myocardial infarction: Discrepancies between trials and real-life. Eur. Heart J. 2014, 35, 979–988. [Google Scholar] [CrossRef] [PubMed]
- Townsend, N.; Wilson, L.; Bhatnagar, P.; Wickramasinghe, K.; Rayner, M.; Nichols, M. Cardiovascular disease in Europe: Epidemiological update 2016. Eur. Heart J. 2016, 37, 3232–3245. [Google Scholar] [CrossRef] [PubMed]
- Gale, C.P.; Allan, V.; Cattle, B.A.; Hall, A.S.; West, R.M.; Timmis, A.; Gray, H.H.; Deanfield, J.E.; Fox, K.A.A.; Feltbower, R. Trends in hospital treatments, including revascularisation, following acute myocardial infarction, 2003–2010: A multilevel and relative survival analysis for the National Institute for Cardiovascular Outcomes Research (NICOR). Heart 2014, 100, 582–589. [Google Scholar] [CrossRef] [PubMed]
- Kotseva, K.; Wood, D.; De Bacquer, D.; De Backer, G.; Rydén, L.; Jennings, C.; Gyberg, V.; Amouyel, P.; Bruthans, J.; Conde, A.C.; et al. EUROASPIRE IV: A European Society of Cardiology survey on the lifestyle, risk factor and therapeutic management of coronary patients from 24 European countries. Eur. J. Prev. Cardiol. 2016, 23, 636–648. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.-T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation. Eur. Heart J. 2016, 37, 2315–2381. [Google Scholar] [PubMed]
- Généreux, P.; Campos, C.M.; Yadav, M.; Palmerini, T.; Caixeta, A.; Xu, K.; Francese, D.P.; Dangas, G.; Mehran, R.; Leon, M.B.; et al. Reasonable incomplete revascularisation after percutaneous coronary intervention: The SYNTAX Revascularisation Index. EuroIntervention 2015, 11, 634–642. [Google Scholar] [CrossRef] [PubMed]
- Rosner, G.F.; Kirtane, A.J.; Genereux, P.; Lansky, A.; Cristea, E.; Weisz, G.; Parise, H.; Fahy, M.; Mehran, R.; Stone, G.W.; et al. Impact of the presence and extent of incomplete angiographic revascularization after percutaneous coronary intervention in acute coronary syndromes: The Acute Catheterization and Urgent Intervention Triage Strategy (ACUITY) trial. Circulation 2012, 125, 2613–2620. [Google Scholar] [CrossRef] [PubMed]
- Pokorney, S.D.; Miller, A.L.; Chen, A.Y.; Thomas, L.; Fonarow, G.C.; De Lemos, J.A.; Al-Khatib, S.M.; Peterson, E.D.; Wang, T.Y. Implantable Cardioverter-Defibrillator Use Among Medicare Patients with Low Ejection Fraction After Acute Myocardial Infarction. JAMA 2015, 313, 2433–2440. [Google Scholar] [CrossRef] [PubMed]
- Narodowy Fundusz Zdrowia. Zarządzenie Nr 38/2017/DSOZ Prezesa Narodowego Funduszu Zdrowia Z Dnia 29 Maja 2017 R. W Sprawie Określenia Warunków Zawierania I Realizacji Umów W Rodzaju Leczenie Szpitalne-Świadczenia Kompleksowe. Available online: http://www.nfz.gov.pl/zarzadzenia-prezesa/zarzadzenia-prezesa-nfz/zarzadzenie-nr-382017dsoz,6578.html (accessed on 1 March 2019).
- Wita, K.; Kułach, A.; Wita, M.; Wybraniec, M.T.; Wilkosz, K.; Polak, M.; Matla, M.; Maciejewski, Łukasz; Fluder, J.; Kalańska-Łukasik, B.; et al. Managed Care after Acute Myocardial Infarction (KOS-zawał) reduces major adverse cardiovascular events by 45% in 3-month follow-up-single-center results of Poland’s National Health Fund program of comprehensive post-myocardial infarction care. Arch. Med. Sci. 2020, 16, 551–558. [Google Scholar] [CrossRef] [PubMed]
- Wita, K.; Kułach, A.; Wita, M.; Wybraniec, M.T.; Wilkosz, K.; Polak, M.; Matla, M.; Maciejewski, Łukasz; Fluder, J.; Kalańska-Łukasik, B.; et al. Managed Care after Acute Myocardial Infarction (MC-AMI)—A Poland’s nationwide program of comprehensive post-MI care-improves prognosis in 12-month follow-up. Preliminary experience from a single high-volume center. Int. J. Cardiol. 2019, 296, 8–14. [Google Scholar] [CrossRef] [PubMed]
- Vrints, C.J. Improving quality of care of acute myocardial infarction: More focus needed on long-term optimal medical treatment and secondary prevention. Rev. Esp. Cardiol. (Engl. Ed.) 2012, 65, 401–402. [Google Scholar] [CrossRef] [PubMed]
- Bettger, J.P.; Alexander, K.P.; Dolor, R.J.; Olson, D.M.; Kendrick, A.S.; Wing, L.; Coeytaux, R.R.; Graffagnino, C.; Duncan, P.W. Transitional care after hospitalization for acute stroke or myocardial infarction: A systematic review. Ann. Intern. Med. 2012, 157, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [PubMed]
- Anderson, L.; Thompson, D.R.; Oldridge, N.; Zwisler, A.-D.; Rees, K.; Martin, N.; Taylor, R. Exercise-based cardiac rehabilitation for coronary heart disease (Review). Cochrane Database Syst. Rev. 2016, 2016, CD001800. [Google Scholar] [CrossRef]
- Rauch, B.; Davos, C.H.; Doherty, P.; Saure, D.; Metzendorf, M.-I.; Salzwedel, A.; Völler, H.; Jensen, K.; Schmid, J.-P. The prognostic effect of cardiac rehabilitation in the era of acute revascularisation and statin therapy: A systematic review and meta-analysis of randomized and non-randomized studies—The Cardiac Rehabilitation Outcome Study (CROS). Eur. J. Prev. Cardiol. 2016, 23, 1914–1939. [Google Scholar] [CrossRef] [PubMed]
- Kabboul, N.; Tomlinson, G.; Francis, T.; Grace, S.L.; Chaves, G.; Rac, V.; Daou-Kabboul, T.; Bielecki, J.M.; Alter, D.A.; Krahn, M. Comparative liveness of the Core Components of Cardiac Rehabilitation on Mortality and Morbidity: A Systematic Review and Network Meta-Analysis. J. Clin. Med. 2018, 7, 514. [Google Scholar] [CrossRef] [PubMed]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [PubMed]
- Pokorney, S.D.; Miller, A.L.; Chen, A.Y.; Thomas, L.; Fonarow, G.C.; De Lemos, J.A.; Al-Khatib, S.M.; Velazquez, E.J.; Peterson, E.D.; Wang, T.Y. Reassessment of Cardiac Function and Implantable Cardioverter-Defibrillator Use Among Medicare Patients with Low Ejection Fraction After Myocardial Infarction. Circulation 2017, 135, 38–47. [Google Scholar] [CrossRef] [PubMed]

| Variable | Control Group Standard Care (n = 6946) | Study Group MC-AMI (n = 3898) | p | ||
|---|---|---|---|---|---|
| Age (years); mean ± SD | 69.8 ± 11.8 | 65.1 ± 10.6 | <0.001 | ||
| Female sex | 2784 | 40.1% | 1234 | 31.7% | <0.001 |
| STEMI presentation | 1950 | 28.1% | 1641 | 42.1% | <0.001 |
| Coroary angiography during MI hospitalization | 6010 | 86.5% | 3880 | 99.5% | <0.001 |
| PCI during MI hospitalization | 4394 | 63.3% | 3498 | 89.7% | <0.001 |
| Cardiac rehabilitation | 1613 | 23.2% | 2080 | 53.4% | <0.001 |
| Congestive Heart Failure | 1709 | 24.6% | 471 | 12.1% | <0.001 |
| Arterial hypertension | 4992 | 71.9% | 2665 | 68.4% | <0.001 |
| Diabetes mellitus | 2303 | 33.2% | 1134 | 29.1% | <0.001 |
| Atrial fibrillation | 896 | 12.9% | 293 | 7.5% | <0.001 |
| CKD | 448 | 6.5% | 167 | 4.3% | <0.001 |
| Malignancy | 1618 | 23.3% | 793 | 20.3% | 0.004 |
| Stroke | 419 | 6.0% | 140 | 3.6% | <0.001 |
| Scheduled PCI | 1095 | 15.8% | 591 | 15.2% | 0.422 |
| Scheduled CABG | 95 | 1.4% | 50 | 1.3% | 0.777 |
| Variable | Control Group Standard Care (n = 3551) | Study Group MC-AMI (n = 3551) | ||
|---|---|---|---|---|
| Age (years); mean ± SD | 66.1 ± 11.4 | 66.2 ± 10.1 | ||
| Female sex | 1179 | 33.2% | 1179 | 33.2% |
| STEMI presentation | 1384 | 39.0% | 1392 | 39.2% |
| Coroary angiography during MI hospitalization | 3541 | 99.7% | 3540 | 99.7% |
| PCI during MI hospitalization | 3124 | 88.0% | 3158 | 88.9% |
| Congestive Heart Failure | 428 | 12.1% | 466 | 13.1% |
| Arterial hypertension | 2433 | 68.5% | 2456 | 69.2% |
| Diabetes mellitus | 1060 | 29.9% | 1053 | 29.7% |
| Atrial fibrillation | 286 | 8.1% | 289 | 8.1% |
| CKD | 178 | 5.0% | 161 | 4.5% |
| Neoplasms | 751 | 21.2% | 747 | 21.0% |
| Stroke | 136 | 3.8% | 138 | 3.9% |
| History of PCI | 540 | 15.2% | 552 | 15.5% |
| History of CABG | 44 | 1.2% | 47 | 1.3% |
| Variable | Hazard Ratio (HR) | 95% CI Lower | 95% CI Upper | p Value |
|---|---|---|---|---|
| Age (per 10 y) | 1.47 | 1.37 | 1.57 | <0.001 |
| MC-AMI | 0.52 | 0.42 | 0.65 | <0.001 |
| STEMI (vs. NSTEMI) | 1.41 | 1.20 | 1.66 | <0.001 |
| Congestive Heart Failure | 2.08 | 1.78 | 2.42 | <0.001 |
| Diabetes | 1.52 | 1.31 | 1.76 | <0.001 |
| COPD | 1.32 | 1.08 | 1.62 | 0.007 |
| Malignancy | 1.33 | 1.14 | 1.55 | <0.001 |
| Stroke | 1.60 | 1.28 | 2.01 | <0.001 |
| Dialysis | 2.38 | 1.60 | 3.54 | <0.001 |
| Variable | MC-AMI n (n%) | Control Group n (n%) | p Value |
|---|---|---|---|
| Staged PCI (within index hospitalization) | 866 (22.2%) | 248 (7%) | p < 0.001 |
| Early CABG (index hospitalization or <6 weeks) | 259 (7.3%) | 76 (2.1%) | p < 0.001 |
| Cardiac rehabilitation—in hospital | 1921 (54.1%) | 971(27%) | p < 0.001 |
| Cardiac rehabilitation—outpatient | 1278 (36%) | 46 (1.3%) | p < 0.001 |
| ICD implantation | 116 (3.2%) | 32 (0.9%) | p < 0.001 |
| CRT implantation | 41 (1.1%) | 19 (0.5%) | p = 0.004 |
| MC-AMI 12month follow up completed | 2613 (73.6%) | n/a | – |
| Follow up: 2 or less visits completed | 923 | n/a | – |
| Follow up: 3 visits completed | 2060 (58%) | n/a | – |
| Follow up: 4 or more visits completed | 568 (16%) | n/a | – |
| Mean number of FU visits (mean. SD) | 2.72 ± 1.45 | 1.2 ± 1.1 | p < 0.001 |
| A: Multivariate Cox Regression—Entire Matched Cohort—Effect of Variables on 12-Month Mortality | ||||
| Variable | Hazard Ratio (HR) | 95% CI Lower | 95% CI Upper | p Value |
| Age (per 10 years) | 1.608 | 1.403 | 1.842 | 0.00000 |
| Congestive Heart Failure | 1.474 | 1.107 | 1.962 | 0.00794 |
| Diabetes | 1.499 | 1.167 | 1.926 | 0.00152 |
| Atrial Fibrillation | 1.519 | 1.094 | 2.109 | 0.01254 |
| COPD | 1.603 | 1.165 | 2.205 | 0.00374 |
| Dialysis | 4.289 | 2.101 | 8.756 | 0.00006 |
| ICD implantation | 2.009 | 1.256 | 3.213 | 0.00360 |
| CR—in hospital | 0.572 | 0.430 | 0.761 | 0.00013 |
| CR—outpatient | 0.262 | 0.167 | 0.409 | 0.00000 |
| B: Multivariate Cox Regression—12-Months Survivors (MC-AMI Completed)—Effect of Variables on 24-Months Mortality | ||||
| Variable | Hazard Ratio (HR) | 95% CI Lower | 95% CI Upper | p Value |
| Age (per 10 years) | 1.873 | 1.533 | 2.289 | 0.00000 |
| Congestive Heart Failure | 1.474 | 1.107 | 1.962 | 0.00794 |
| Atrial Fibrillation | 2.080 | 1.393 | 3.105 | 0.00034 |
| COPD | 1.779 | 1.121 | 2.824 | 0.01456 |
| CKD | 1.859 | 1.062 | 3.255 | 0.02996 |
| Dialysis | 3.554 | 1.179 | 10.719 | 0.02434 |
| CR | 0.343 | 0.180 | 0.652 | 0.00109 |
| MC-AMI FU completed | 0.416 | 0.291 | 0.594 | 0.00000 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wita, K.; Kułach, A.; Sikora, J.; Fluder, J.; Nowalany-Kozielska, E.; Milewski, K.; Pączek, P.; Sobocik, H.; Olender, J.; Szela, L.; et al. Managed Care after Acute Myocardial Infarction (MC-AMI) Reduces Total Mortality in 12-Month Follow-Up—Results from a Poland’s National Health Fund Program of Comprehensive Post-MI Care—A Population-Wide Analysis. J. Clin. Med. 2020, 9, 3178. https://doi.org/10.3390/jcm9103178
Wita K, Kułach A, Sikora J, Fluder J, Nowalany-Kozielska E, Milewski K, Pączek P, Sobocik H, Olender J, Szela L, et al. Managed Care after Acute Myocardial Infarction (MC-AMI) Reduces Total Mortality in 12-Month Follow-Up—Results from a Poland’s National Health Fund Program of Comprehensive Post-MI Care—A Population-Wide Analysis. Journal of Clinical Medicine. 2020; 9(10):3178. https://doi.org/10.3390/jcm9103178
Chicago/Turabian StyleWita, Krystian, Andrzej Kułach, Jacek Sikora, Joanna Fluder, Ewa Nowalany-Kozielska, Krzysztof Milewski, Piotr Pączek, Henryk Sobocik, Jacek Olender, Lucjan Szela, and et al. 2020. "Managed Care after Acute Myocardial Infarction (MC-AMI) Reduces Total Mortality in 12-Month Follow-Up—Results from a Poland’s National Health Fund Program of Comprehensive Post-MI Care—A Population-Wide Analysis" Journal of Clinical Medicine 9, no. 10: 3178. https://doi.org/10.3390/jcm9103178
APA StyleWita, K., Kułach, A., Sikora, J., Fluder, J., Nowalany-Kozielska, E., Milewski, K., Pączek, P., Sobocik, H., Olender, J., Szela, L., Kalarus, Z., Buszman, P., Jankowski, P., & Gąsior, M. (2020). Managed Care after Acute Myocardial Infarction (MC-AMI) Reduces Total Mortality in 12-Month Follow-Up—Results from a Poland’s National Health Fund Program of Comprehensive Post-MI Care—A Population-Wide Analysis. Journal of Clinical Medicine, 9(10), 3178. https://doi.org/10.3390/jcm9103178





