Associations of Health-Related Quality of Life, Fear of Falling and Objective Measures of Physical Function with Bone Health in Postmenopausal Women with Low Bone Mass
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
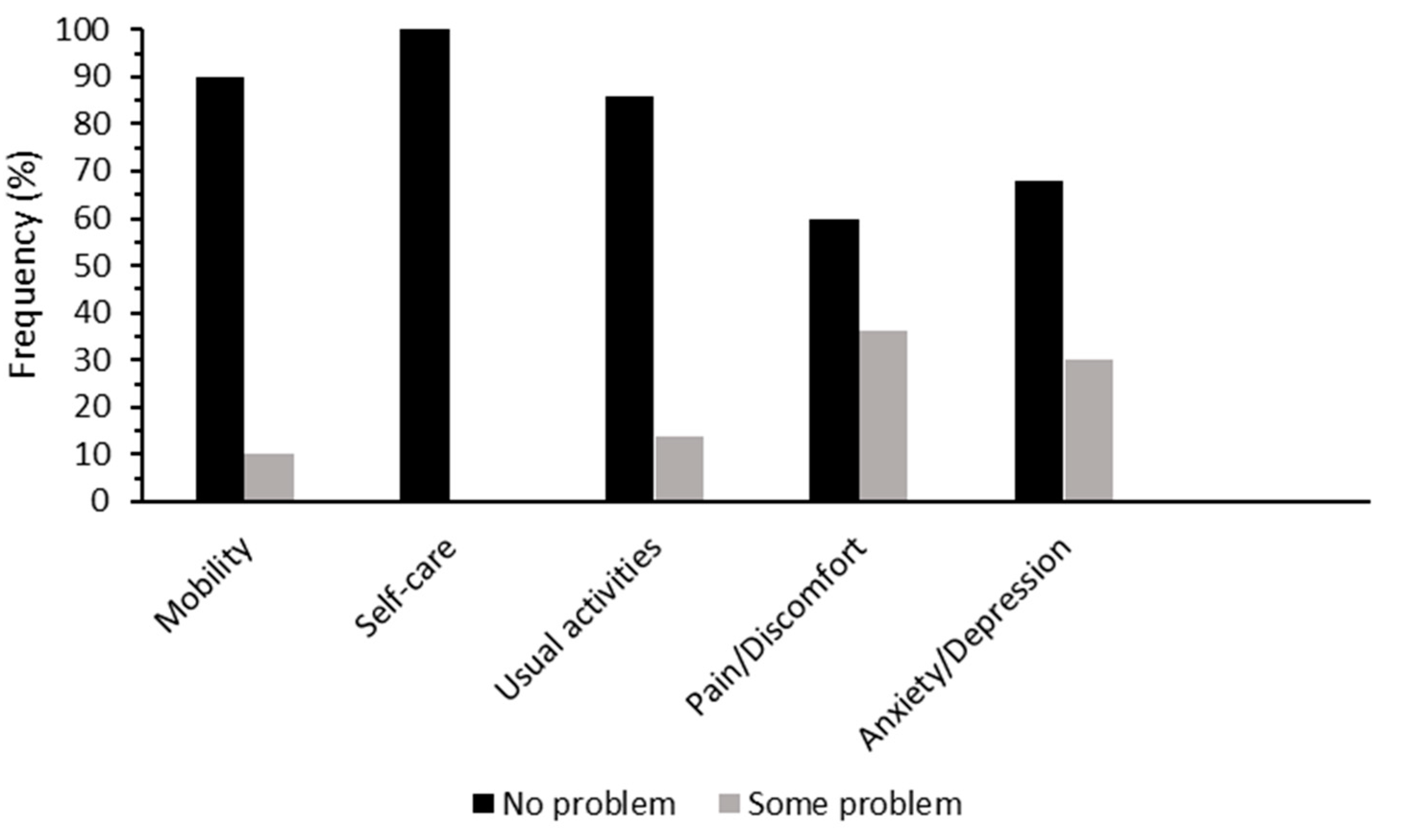
2.2. Questionnaires
2.3. Physical Function
2.4. Anthropometric, Bone and Blood Biochemistry Parameters
2.5. Accelerometer-Determined Physical Activity
2.6. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Ji, M.-X.; Yu, Q. Primary osteoporosis in postmenopausal women. Chronic Dis. Transl. Med. 2015, 1, 9. [Google Scholar] [PubMed]
- Tella, S.H.; Gallagher, J.C. Prevention and treatment of postmenopausal osteoporosis. J. Steroid Biochem. Mol. Boil. 2014, 142, 155–170. [Google Scholar] [CrossRef] [PubMed]
- Lips, P.; van Schoor, N.M. Quality of life in patients with osteoporosis. Osteoporos. Int. 2005, 16, 447–455. [Google Scholar] [CrossRef] [PubMed]
- Langdahl, B.L.; Ljunggren, Ö.; Benhamou, C.-L.; Marín, F.; Kapetanos, G.; Kocjan, T.; Lespessailles, E.; Napoli, N.; Nikolic, T.; Petto, H.; et al. Fracture Rate, Quality of Life and Back Pain in Patients with Osteoporosis Treated with Teriparatide: 24-Month Results from the Extended Forsteo Observational Study (ExFOS). Calcif. Tissue Int. 2016, 99, 259–271. [Google Scholar] [CrossRef] [PubMed]
- Mueller, D.; Gandjour, A. Cost-Effectiveness of Using Clinical Risk Factors with and without DXA for Osteoporosis Screening in Postmenopausal Women. Value Heal. 2009, 12, 1106–1117. [Google Scholar] [CrossRef] [PubMed]
- Demontiero, O.; Vidal, C.; Duque, G. Aging and bone loss: New insights for the clinician. Ther. Adv. Musculoskelet. Dis. 2012, 4, 61–76. [Google Scholar] [CrossRef]
- Pereira, C.L.N.; Vogelaere, P.; Baptista, F. Role of physical activity in the prevention of falls and their consequences in the elderly. Eur. Rev. Aging Phys. Act. 2008, 5, 51–58. [Google Scholar] [CrossRef]
- Berard, A.; Bravo, G.; Gauthier, P. Meta-analysis of the effectiveness of physical activity for the prevention of bone loss in postmenopausal women. Osteoporos. Int. 1997, 7, 331–337. [Google Scholar] [CrossRef]
- Sakazaki, T.; Koike, T.; Yanagimoto, Y.; Oshida, Y. Association between gait speed and bone strength in community-dwelling postmenopausal Japanese women. Environ. Heal. Prev. Med. 2012, 17, 394–400. [Google Scholar] [CrossRef]
- Beaudart, C.; Rolland, Y.; Cruz-Jentoft, A.J.; Bauer, J.M.; Sieber, C.; Cooper, C.; Al-Daghri, N.; Araujo de Carvalho, I.; Bautmans, I.; Bernabei, R.; et al. Assessment of Muscle Function and Physical Performance in Daily Clinical Practice: A position paper endorsed by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO). Calcif. Tissue Int. 2019, 105, 1–14. [Google Scholar] [CrossRef]
- Xu, X.; Ji, W.; Lv, X.-Q.; Zhu, Y.-C.; Zhao, J.-X.; Miao, L.-Z. Impact of physical activity on health-related quality of life in osteoporotic and osteopenic postmenopausal women: A systematic review. Int. J. Nurs. Sci. 2015, 2, 204–217. [Google Scholar] [CrossRef]
- McCaffrey, N.; Kaambwa, B.; Currow, D.C.; Ratcliffe, J. Health-related quality of life measured using the EQ-5D–5L: South Australian population norms. Heal. Qual. Life Outcomes 2016, 14, 133. [Google Scholar]
- Salaffi, F.; Cimmino, M.A.; Malavolta, N.; Carotti, M.; Di Matteo, L.; Scendoni, P.; Grassi, W. The burden of prevalent fractures on health-related quality of life in postmenopausal women with osteoporosis: The IMOF study. J. Rheumatol. 2007, 34, 34. [Google Scholar]
- Aleksic, J.; Zvekic-Svorcan, J.; Vujasinovic Stupar, N.; Jeremic, I.; Grgurevic, A. Cross-cultural validation of the Modified Falls Efficacy Scale in Serbian community-dwelling women at risk for osteoporotic fracture. Menopause 2018, 25, 444–450. [Google Scholar] [CrossRef] [PubMed]
- Hazzaa, N.; Naeem, F.; Eldin, H.G.; El Fattah, L.A. Validation of the Modified Falls Efficacy Scale-International (FES-I) in Egyptian Geriatric Population. Egypt. J. Hosp. Med. 2018, 71, 2294–2303. [Google Scholar]
- Pua, Y.-H.; Ong, P.-H.; Clark, R.A.; Matcher, D.B.; Lim, E.C.-W. Falls efficacy, postural balance, and risk for falls in older adults with falls-related emergency department visits: Prospective cohort study. BMC Geriatr. 2017, 17, 291. [Google Scholar] [CrossRef] [PubMed]
- Bean, J.F.; Kiely, D.K.; LaRose, S.; Alian, J.; Frontera, W.R. Is Stair Climb Power a Clinically Relevant Measure of Leg Power Impairments in At-Risk Older Adults? Arch. Phys. Med. Rehabil. 2007, 88, 604–609. [Google Scholar] [CrossRef]
- Freiberger, E.; De Vreede, P.; Schoene, D.; Rydwik, E.; Mueller, V.; Frändin, K.; Hopman-Rock, M. Performance-based physical function in older community-dwelling persons: A systematic review of instruments. Age Ageing 2012, 41, 712–721. [Google Scholar] [CrossRef]
- Guralnik, J.M.; Ferrucci, L.; Pieper, C.F.; Leveille, S.G.; Markides, K.S.; Ostir, G.V.; Studenski, S.; Berkman, L.F.; Wallace, R.B. Lower Extremity Function and Subsequent Disability: Consistency Across Studies, Predictive Models, and Value of Gait Speed Alone Compared with the Short Physical Performance Battery. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2000, 55, M221–M231. [Google Scholar]
- Kanis, J.A. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis: Synopsis of a WHO report. Osteoporos. Int. 1994, 4, 368–381. [Google Scholar] [CrossRef]
- Humbert, L.; Martelli, Y.; Fonolla, R.; Steghofer, M.; Di Gregorio, S.; Malouf, J.; Romera, J.; Barquero, L.M.D.R. 3D-DXA: Assessing the Femoral Shape, the Trabecular Macrostructure and the Cortex in 3D from DXA images. IEEE Trans. Med. Imaging 2017, 36, 27–39. [Google Scholar] [CrossRef] [PubMed]
- Bouxsein, M.L.; Boyd, S.K.; A Christiansen, B.; E Guldberg, R.; Jepsen, K.J.; Müller, R. Guidelines for assessment of bone microstructure in rodents using micro-computed tomography. J. Bone Miner. Res. 2010, 25, 1468–1486. [Google Scholar] [CrossRef] [PubMed]
- Cheung, A.M.; Adachi, J.D.; Hanley, D.A.; Kendler, D.L.; Davison, K.S.; Josse, R.; Brown, J.P.; Ste-Marie, L.-G.; Kremer, R.; Erlandson, M.C.; et al. High-Resolution Peripheral Quantitative Computed Tomography for the Assessment of Bone Strength and Structure: A Review by the Canadian Bone Strength Working Group. Curr. Osteoporos. Rep. 2013, 11, 136–146. [Google Scholar] [PubMed]
- Westbury, L.D.; Shere, C.; Edwards, M.H.; Cooper, C.; Dennison, E.M.; Ward, K.A. Cluster Analysis of Finite Element Analysis and Bone Microarchitectural Parameters Identifies Phenotypes with High Fracture Risk. Calcif. Tissue Int. 2019, 105, 252–262. [Google Scholar] [CrossRef] [PubMed]
- Boutroy, S.; Van Rietbergen, B.; Sornay-Rendu, E.; Munoz, F.; Bouxsein, M.L.; Delmas, P.D. Finite element analysis based on in vivo HR-pQCT images of the distal radius is associated with wrist fracture in postmenopausal women. J. Bone Miner. Res. 2008, 23, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Freedson, P.S.; Melanson, E.; Sirard, J. Calibration of the Computer Science and Applications, Inc. accelerometer. Med. Sci. Sports Exerc. 1998, 30, 777–781. [Google Scholar] [CrossRef] [PubMed]
- Menai, M.; Van Hees, V.T.; Elbaz, A.; Kivimaki, M.; Singh-Manoux, A.; Sabia, S. Accelerometer assessed moderate-to-vigorous physical activity and successful ageing: Results from the Whitehall II study. Sci. Rep. 2017, 7, 45772. [Google Scholar] [CrossRef]
- Miller, P.D. Management of severe osteoporosis. Expert Opin. Pharmacother. 2016, 17, 473–488. [Google Scholar] [CrossRef]
- Dhillon, V.; Hurst, N.; Hannan, J.; Nuki, G. Association of low general health status, measured prospectively by Euroqol EQ5D, with osteoporosis, independent of a history of prior fracture. Osteoporos. Int. 2005, 16, 483–489. [Google Scholar] [CrossRef]
- Jahelka, B.; Dorner, T.E.; Terkula, R.; Quittan, M.; Bröll, H.; Erlacher, L. Health-related quality of life in patients with osteopenia or osteoporosis with and without fractures in a geriatric rehabilitation department. Wien. Med. Wochenschr. 2009, 159, 235–240. [Google Scholar] [CrossRef]
- Park, H. The impact of osteoporosis on health-related quality of life in elderly women. Biomed. Res. 2018, 29, 3223–3227. [Google Scholar] [CrossRef]
- Halvarsson, A.; Franzen, E.; Stahle, A. Assessing the relative and absolute reliability of the Falls Efficacy Scale-International questionnaire in elderly individuals with increased fall risk and the questionnaire’s convergent validity in elderly women with osteoporosis. Osteoporos. Int. 2013, 24, 1853–1858. [Google Scholar] [CrossRef] [PubMed]
- Resnick, B.; Nahm, E.S.; Zhu, S.; Brown, C.; An, M.; Park, B.; Brown, J. The Impact of Osteoporosis, Falls, Fear of Falling, and Efficacy Expectations on Exercise Among Community-Dwelling Older Adults. Orthop. Nurs. 2014, 33, 277–286. [Google Scholar] [CrossRef] [PubMed]
- Taaffe, D.R.; Simonsick, E.M.; Visser, M.; Volpato, S.; Nevitt, M.C.; Cauley, J.A.; Tylavsky, F.A.; Harris, T.B. Lower extremity physical performance and hip bone mineral density in elderly black and white men and women: Cross-sectional associations in the Health ABC Study. J. Gerontol. Ser. A Boil. Sci. Med. Sci. 2003, 58, M934–M942. [Google Scholar] [CrossRef] [PubMed]
- Scott, D.; Johansson, J.; McMillan, L.B.; Ebeling, P.R.; Nordstrom, P.; Nordstrom, A. Associations of Sarcopenia and Its Components with Bone Structure and Incident Falls in Swedish Older Adults. Calcif. Tissue Int. 2019, 105, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Lindsey, C.; Brownbill, R.A.; Bohannon, R.A.; Ilich, J.Z. Association of Physical Performance Measures with Bone Mineral Density in Postmenopausal Women. Arch. Phys. Med. Rehabil. 2005, 86, 1102–1107. [Google Scholar] [CrossRef]
- Yu, R.; Leung, J.; Woo, J. Incremental Predictive Value of Sarcopenia for Incident Fracture in an Elderly Chinese Cohort: Results from the Osteoporotic Fractures in Men (MrOs) Study. J. Am. Med. Dir. Assoc. 2014, 15, 551–558. [Google Scholar] [CrossRef]
- Hong, A.R.; Kim, S.W. Effects of Resistance Exercise on Bone Health. Endocrinol. Metab. 2018, 33, 435–444. [Google Scholar] [CrossRef]
- Watson, S.L.; Weeks, B.K.; Weis, L.J.; Harding, A.T.; Horan, S.A.; Beck, B.R. High-Intensity Resistance and Impact Training Improves Bone Mineral Density and Physical Function in Postmenopausal Women with Osteopenia and Osteoporosis: The LIFTMOR Randomized Controlled Trial. J. Bone Miner. Res. 2018, 33, 211–220. [Google Scholar] [CrossRef]
- Chang, G.; Pakin, S.K.; Schweitzer, M.E.; Saha, P.K.; Regatte, R.R. Adaptations in Trabecular Bone Microarchitecture in Olympic Athletes Determined by 7T MRI. J. Magn. Reson. Imaging 2008, 27, 1089–1095. [Google Scholar] [CrossRef]
- Nikander, R.; Sievänen, H.; Heinonen, A.; Daly, R.M.; Uusi-Rasi, K.; Kannus, P. Targeted exercise against osteoporosis: A systematic review and meta-analysis for optimising bone strength throughout life. BMC Med. 2010, 8, 47. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.; Gibson, L. Modeling the mechanical behavior of vertebral trabecular bone: Effects of age-related changes in microstructure. Bone 1997, 21, 191–199. [Google Scholar] [CrossRef]
| Mean ± Standard Deviation or Percentage | |
|---|---|
| Age (years) | 64.4 ± 7.7 |
| Weight (kg) | 61.5 ± 8.5 |
| Height (cm) | 161.3 ± 6.5 |
| BMI (kg/m2) | 23.6 ± 3.0 |
| 25(OH)D (nmol/L) | 74.6 ± 25.1 |
| aBMD | |
| Total hip (g/cm2) Femoral neck (g/cm2) Lumbar spine (g/cm2) | 0.765 ± 0.081 0.636 ± 0.070 0.809 ± 0.112 |
| BMC | |
| Total hip (g) Femoral neck (g) Lumbar spine (g) | 26.582 ± 3.708 3.207 ± 0.388 43.585 ± 10.916 |
| Smoking status | |
| Current (%) Former (%) Never (%) | 0 22 78 |
| HRQoL and fear of falling | |
| EQ-5D score (out of 15) MFES score (out of 140) | 5 (5.0, 6.3) # 140 (134.8, 140) # |
| Physical activity | |
| Sedentary time physical activity (%) Light-intensity physical activity (%) Moderate-intensity physical activity (%) Vigorous-intensity physical activity (%) Very vigorous-intensity physical activity (%) | 73.3 ± 6.0 21.7 ± 4.7 4.8 ± 2.4 0.2 ± 0.4 0.004 ± 0.01 |
| Objective measures of physical function | |
| SPPB (out of 12) SCPT (W) | 12 (11, 12) # 277.2 (229.1, 335.5) |
| Self-reported comorbidities | |
| Hypertension (%) Hypercholesterolemia (%) Thrombosis (%) T2DM (%) Asthma (%) Bronchitis/emphysema (%) Any cancer (%) | 22 28 2 4 14 2 6 |
| EQ-5D | Mobility | Usual | Pain | Anxiety | MFES | |
|---|---|---|---|---|---|---|
| DXA bone parameters | ||||||
| Hip BMC (g) | 0.264 | 0.132 | 0.222 | 0.158 | 0.269 | −0.318 * |
| Hip aBMD (g/cm2) | 0.002 | −0.021 | 0.066 | −0.109 | 0.031 | −0.196 |
| Hip T-score | −0.008 | −0.036 | 0.060 | −0.103 | 0.036 | −0.173 |
| Spine BMC (g) | −0.056 | −0.081 | −0.034 | −0.096 | −0.044 | 0.041 |
| Spine aBMD (g/cm2) | −0.187 | −0.076 | −0.074 | −0.165 | −0.157 | 0.007 |
| Spine T-score | −0.149 | −0.057 | −0.062 | −0.155 | −0.128 | −0.015 |
| LS TBS | −0.033 | −0.039 | −0.056 | −0.045 | 0.103 | 0.062 |
| FN BMC (g) | 0.064 | 0.049 | 0.026 | 0.000 | 0.056 | 0.015 |
| FN aBMD (g/cm2) | −0.066 | −0.025 | −0.078 | −0.118 | −0.053 | 0.095 |
| FN T-score | −0.050 | −0.017 | −0.062 | −0.126 | −0.023 | 0.070 |
| DXA 3D bone parameters | ||||||
| Surface BMD (mg/cm3) | 0.084 | −0.043 | 0.037 | −0.045 | 0.036 | −0.157 |
| Trabecular vBMD (mg/cm3) | −0.259 | −0.076 | −0.049 | −0.342 * | −0.149 | −0.022 |
| Integral vBMD (mg/cm3) | −0.194 | −0.086 | −0.016 | −0.294 * | −0.149 | −0.078 |
| Cortical vBMD (mg/cm3) | −0.049 | −0.095 | 0.058 | −0.142 | −0.069 | −0.198 |
| Mean cortical thickness (mm) | 0.149 | −0.010 | 0.033 | 0.013 | 0.119 | −0.087 |
| HR-pQCT bone parameters at distal tibia | ||||||
| Trabecular area (mm2) | 0.080 | 0.173 | 0.054 | 0.099 | −0.072 | −0.163 |
| Trabecular thickness (mm) | 0.061 | 0.113 | 0.112 | −0.081 | 0.045 | 0.014 |
| Trabecular separation (mm) | 0.019 | 0.035 | −0.086 | −0.103 | 0.080 | −0.048 |
| Trabecular VMS (MPa) | −0.187 | −0.043 | −0.091 | −0.245 | −0.031 | 0.111 |
| Cortical Area (mm2) | −0.023 | −0.146 | −0.182 | −0.023 | −0.011 | 0.081 |
| Cortical vBMD (mg/cm3) | −0.139 | −0.312 * | −0.104 | −0.073 | −0.011 | 0.133 |
| Cortical periosteal perimeter (mm) | 0.022 | 0.148 | 0.110 | 0.042 | −0.180 | −0.142 |
| Cortical porosity (%) | −0.013 | 0.092 | −0.092 | −0.020 | −0.005 | 0.044 |
| Cortical VMS (MPa) | −0.263 | −0.248 | −0.198 | −0.261 | −0.041 | 0.187 |
| Estimated bone failure load (N) | 0.081 | 0.157 | 0.095 | 0.099 | −0.024 | −0.169 |
| Bone stiffness (N/mm) | −0.092 | −0.143 | −0.091 | −0.109 | 0.005 | 0.155 |
| Gait Speed (m/s) | Stair Climb Power (W) | Chair Stand Time (s) | SPPB | |
|---|---|---|---|---|
| DXA bone parameters | ||||
| Hip BMC (g) Hip aBMD (g/cm2) Hip T-score Spine BMC (g) Spine aBMD (g/cm2) Spine T-score LS TBS FN BMC (g) FN aBMD (g/cm2) FN T-score | 0.272 0.234 0.226 0.236 0.175 0.152 0.159 0.220 0.181 0.168 | 0.390 ** 0.249 0.296 * 0.395 ** 0.317 * 0.271 0.344 * 0.405 ** 0.328 * 0.347 * | −0.043 −0.172 −0.163 −0.191 −0.107 −0.116 −0.262 −0.007 −0.082 −0.089 | 0.106 0.211 0.190 0.026 −0.083 −0.062 0.299 * 0.092 0.002 0.032 |
| DXA 3D bone parameters | ||||
| Surface BMD (mg/cm3) Trabecular vBMD (mg/cm3) Integral vBMD (mg/cm3) Cortical vBMD (mg/cm3) Mean cortical thickness (mm) | 0.204 0.188 0.200 0.199 0.203 | 0.197 0.111 0.118 0.068 0.279 | −0.064 −0.271 −0.258 −0.136 −0.029 | 0.124 0.245 0.221 0.132 0.139 |
| HR-pQCT bone parameters at distal tibia | ||||
| Trabecular area (mm2) Trabecular thickness (mm) Trabecular separation (mm) Trabecular VMS (Mpa) Cortical Area (mm2) Cortical vBMD (mg/cm3) Cortical periosteal perimeter (mm) Cortical porosity (%) Cortical VMS (MPa) Estimated bone failure load (N) Bone stiffness (N/mm) | 0.151 −0.413 ** −0.196 −0.213 0.063 0.071 0.091 −0.018 0.118 −0.066 0.042 | 0.342 * −0.314 * −0.220 0.024 0.090 0.146 0.329 * −0.208 −0.036 −0.314 * −0.314 * | 0.153 0.097 0.058 −0.192 −0.341 * −0.186 0.116 −0.093 −0.298 * 0.217 −0.217 | −0.045 −0.109 0.119 0.018 0.087 0.229 −0.069 −0.151 0.331 * −0.106 0.079 |
| EQ-5D Score | MFES Score | Gait Speed (m/s) | Stair Climb Power (W) | Chair Stand Time (s) | SPPB | |
|---|---|---|---|---|---|---|
| DXA bone parameters | ||||||
| Hip BMC (g) | 0.218 (−0.072, 0.509) | −0.175 (−0.467, 0.117) | 0.266 (−0.030, 0.562) | 0.485 (0.175, 0.795) | −0.157 (−0.467, 0.153) | 0.016 (−0.344, 0.376) |
| Hip aBMD (g/cm2) | −0.012 (−0.327, 0.303) | 0.032 (−0.282, 0.346) | 0.265 (−0.050, 0.580) | 0.263 (−0.093, 0.618) | −0.271 (−0.592, 0.051) | 0.243 (−0.130, 0.616) |
| Hip T-score | −0.026 (−0.339, 0.288) | 0.038 (−0.274, 0.351) | 0.254 (−0.061, 0.569) | 0.239 (−0.112, 0.591) | −0.251 (−0.568, 0.066) | 0.212 (−0.161, 0.586) |
| Spine BMC (g) | −0.106 (−0.410, 0.198) | 0.119 (−0.184, 0.421) | 0.219 (−0.089, 0.527) | 0.288 (−0.055, 0.630) | −0.162 (−0.480, 0.156) | −0.107 (−0.475, 0.261) |
| Spine aBMD (g/cm2) | −0.263 (−0.566, 0.040) | 0.204 (−0.102, 0.510) | 0.145 (−0.177, 0.466) | 0.220 (−0.137, 0.576) | −0.136 (−0.464, 0.191) | −0.100 (−0.478, 0.277) |
| Spine T-score | −0.252 (−0.562, 0.058) | 0.211 (−0.101, 0.523) | 0.134 (−0.195, 0.463) | 0.224 (−0.135, 0.583) | −0.165 (−0.494, 0.164) | −0.063 (−0.450, 0.324) |
| LS TBS | −0.020 (−0.290, 0.249) | 0.098 (−0.169, 0.364) | −0.047 (−0.326, 0.231) | 0.034 (−0.278, 0.346) | −0.046 (−0.329, 0.238) | 0.052 (−0.274, 0.377) |
| FN BMC (g) | −0.018 (−0.322, 0.286) | 0.175 (−0.123, 0.473) | 0.294 (−0.006, 0.594) | 0.458 (0.136, 0.780) | −0.165 (−0.481, 0.151) | 0.268 (−0.090, 0.625) |
| FN aBMD (g/cm2) | −0.126 (−0.434, 0.182) | 0.250 (−0.050, 0.550) | 0.198 (−0.117, 0.513) | 0.353 (0.010, 0.696) | −0.205 (−0.526, 0.116) | 0.292 (−0.071, 0.656) |
| FN T-score | −0.121 (−0.431, 0.190) | 0.245 (−0.057, 0.547) | 0.188 (−0.131, 0.506) | 0.351 (0.011, 0.692) | −0.206 (−0.525, 0.113) | 0.306 (−0.059, 0.671) |
| DXA 3D bone parameters | ||||||
| Surface BMD (mg/cm3) | −0.007 (−0.328, 0.313) | 0.001 (−0.308, 0.309) | 0.211 (−0.102, 0.524) | 0.191 (−0.163, 0.544) | −0.122 (−0.445, 0.202) | 0.121 (−0.251, 0.492) |
| Trabecular vBMD (mg/cm3) | −0.246 (−0.561, 0.070) | 0.148 (−0.161, 0.457) | 0.145 (−0.176, 0.466) | 0.075 (−0.287, 0.437) | −0.252 (−0.573, 0.068) | 0.315 (−0.051, 0.680) |
| Integral vBMD (mg/cm3) | −0.200 (−0.520, 0.121) | 0.095 (−0.218, 0.408) | 0.151 (−0.171, 0.474) | 0.054 (−0.311, 0.419) | −0.235 (−0.559, 0.089) | 0.238 (−0.136, 0.611) |
| Cortical vBMD (mg/cm3) | −0.086 (−0.416, 0.243) | −0.053 (−0.375, 0.268) | 0.210 (−0.118, 0.538) | 0.068 (−0.301, 0.437) | −0.170 (−0.502, 0.162) | 0.072 (−0.318, 0.463) |
| Mean cortical thickness (mm) | 0.077 (−0.236, 0.389) | 0.041 (−0.264, 0.347) | 0.191 (−0.121, 0.502) | 0.243 (−0.100, 0.585) | −0.069 (−0.388, 0.249) | 0.153 (−0.215, 0.521) |
| HR-pQCT bone parameters at distal tibia | ||||||
| Trabecular area (mm2) | 0.161 (−0.150, 0.472) | −0.215 (−0.521, 0.092) | 0.180 (−0.141, 0.501) | 0.444 (0.106, 0.781) | 0.155 (−0.173, 0.484) | −0.044 (−0.425, 0.336) |
| Trabecular thickness (mm) | 0.076 (−0.249, 0.402) | −0.052 (−0.376, 0.273) | −0.439 (−0.745, −0.132) | −0.387 (−0.745, −0.029) | 0.089 (−0.254, 0.431) | 0.002 (−0.393, 0.396) |
| Trabecular separation (mm) | 0.311 (−0.002, 0.624) | −0.052 (−0.376, 0.273) | −0.115 (−0.452, 0.222) | −0.286 (−0.654, 0.082) | 0.002 (−0.342, 0.347) | 0.336 (−0.044, 0.717) |
| Trabecular VMS (MPa) | −0.221 (−0.539, 0.097) | 0.078 (−0.245, 0.401) | −0.322 (−0.643, −0.002) | −0.200 (−0.567, 0.166) | −0.175 (−0.509, 0.158) | 0.028 (−0.366, 0.421) |
| Cortical Area (mm2) | −0.081 (−0.400, 0.241) | 0.218 (−0.097, 0.534) | 0.043 (−0.290, 0.375) | 0.033 (−0.340, 0.405) | −0.279 (−0.606, 0.049) | −0.071 (−0.459, 0.317) |
| Cortical vBMD (mg/cm3) | −0.219 (−0.533, 0.094) | 0.339 (0.037, 0.641 | 0.051 (−0.281, 0.382) | 0.062 (−0.308, 0.433) | −0.168 (−0.501, 0.166) | 0.111 (−0.274, 0.497) |
| Cortical periosteal perimeter (mm) | 0.112 (−0.196, 0.419) | −0.212 (−0.514, 0.090) | 0.085 (−0.234, 0.405) | 0.447 (0.116, 0.777) | 0.081 (−0.244, 0.407) | −0.114 (−0.486, 0.259) |
| Cortical porosity (%) | 0.162 (−0.150, 0.475) | −0.192 (−0.502, 0.118) | −0.164 (−0.488, 0.160) | −0.257 (−0.616, 0.101) | −0.109 (−0.441, 0.223) | −0.208 (−0.585, 0.169) |
| Cortical VMS (MPa) | −0.237 (−0.537, 0.063) | 0.344 (0.055, 0.633) | −0.006 (−0.327, 0.315) | −0.188 (−0.537, 0.161) | −0.254 (−0.566, 0.058) | 0.411 (0.061, 0.760) |
| Estimated bone failure load (N) | 0.125 (−0.174, 424) | −0.074 (−0.374, 0.226) | 0.034 (−0.279, 0.347) | −0.147 (−0.490, 0.195) | 0.212 (−0.095, 0.519) | 0.025 (−0.341, 0.390) |
| Bone stiffness (N/mm) | −0.138 (−0.438, 0.163) | 0.067 (−0.235, 0.369) | −0.063 (−0.378, 0.251) | 0.123 (−0.223, 0.468) | −0.203 (−0.513, 0.106) | −0.061 (−0.428, 0.306) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gandham, A.; McMillan, L.B.; Ng, C.-A.; Humbert, L.; Bonham, M.P.; Zengin, A.; Ebeling, P.R.; Scott, D. Associations of Health-Related Quality of Life, Fear of Falling and Objective Measures of Physical Function with Bone Health in Postmenopausal Women with Low Bone Mass. J. Clin. Med. 2019, 8, 1370. https://doi.org/10.3390/jcm8091370
Gandham A, McMillan LB, Ng C-A, Humbert L, Bonham MP, Zengin A, Ebeling PR, Scott D. Associations of Health-Related Quality of Life, Fear of Falling and Objective Measures of Physical Function with Bone Health in Postmenopausal Women with Low Bone Mass. Journal of Clinical Medicine. 2019; 8(9):1370. https://doi.org/10.3390/jcm8091370
Chicago/Turabian StyleGandham, Anoohya, Lachlan B. McMillan, Carrie-Anne Ng, Ludovic Humbert, Maxine P. Bonham, Ayse Zengin, Peter R. Ebeling, and David Scott. 2019. "Associations of Health-Related Quality of Life, Fear of Falling and Objective Measures of Physical Function with Bone Health in Postmenopausal Women with Low Bone Mass" Journal of Clinical Medicine 8, no. 9: 1370. https://doi.org/10.3390/jcm8091370
APA StyleGandham, A., McMillan, L. B., Ng, C.-A., Humbert, L., Bonham, M. P., Zengin, A., Ebeling, P. R., & Scott, D. (2019). Associations of Health-Related Quality of Life, Fear of Falling and Objective Measures of Physical Function with Bone Health in Postmenopausal Women with Low Bone Mass. Journal of Clinical Medicine, 8(9), 1370. https://doi.org/10.3390/jcm8091370





