Role of Bronchoscopic Techniques in the Diagnosis of Thoracic Sarcoidosis
Abstract
1. Introduction
2. Standard Bronchoscopic Techniques
2.1. Endobronchial Biopsy (EBB)
2.2. Transbronchial Lung Biopsy (TBLB)
2.3. Conventional Transbronchial Needle Aspiration (cTBNA)
2.4. Bronchoalveolar Lavage Fluid (BALF)
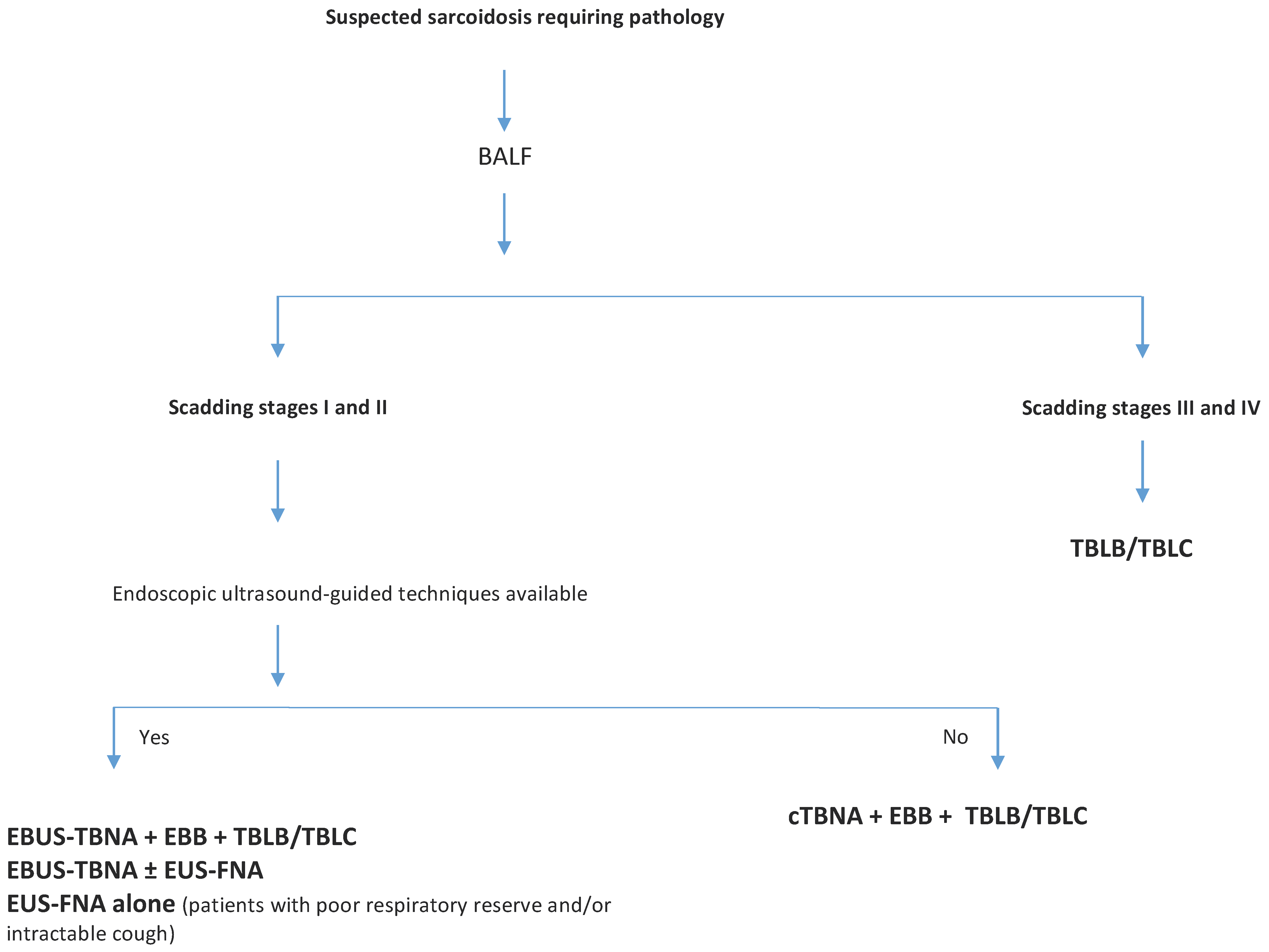
3. Recent Bronchoscopic Techniques
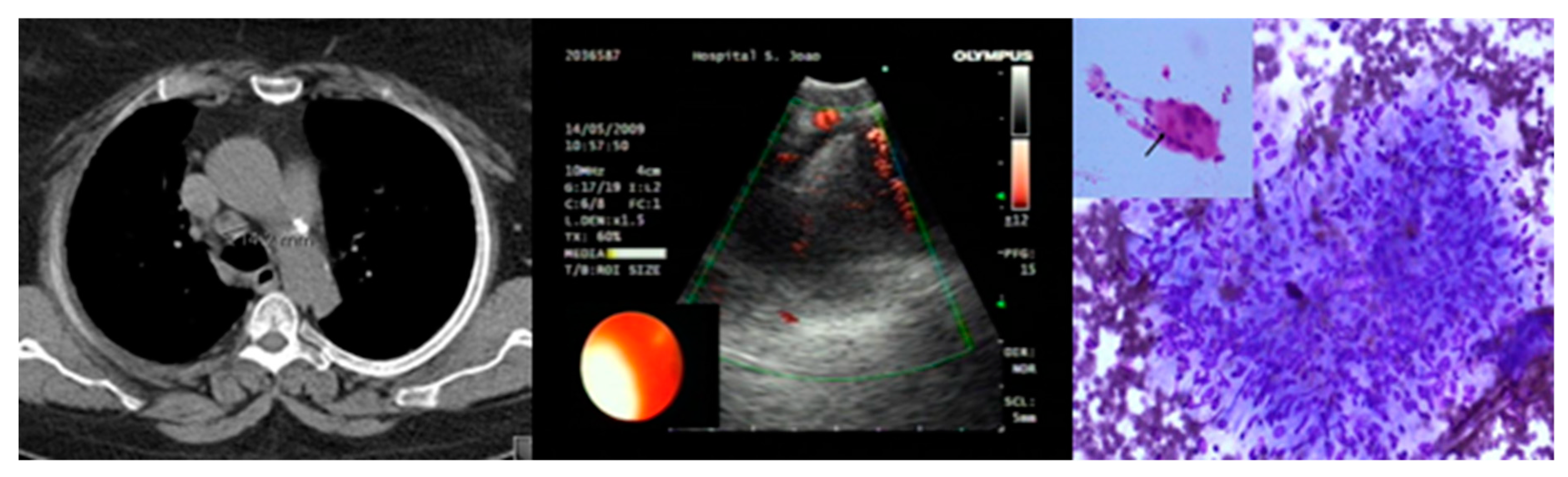
3.1. Endobronchial Ultrasound-Guided Transbronchial Needle Aspiration (EBUS-TBNA)
3.2. Endoscopic Ultrasound-Guided Fine Needle Aspiration (EUS-FNA)
3.3. Transesophageal Ultrasound-Guided Needle Aspiration with the Use of an Echo Bronchoscope (EUS-B-FNA)
3.4. Transbronchial Lung Cryobiopsy (TBLC)
4. A Key Emphasis to EBUS-TBNA and Standard Bronchoscopic Modalities
4.1. Complications of Endoscopic Ultrasound-Guided Techniques
4.2. Factors Affecting Diagnostic Accuracy of Endoscopic Ultrasound-Guided Techniques
4.2.1. Size of Needles
4.2.2. Rapid On-Site Evaluation (ROSE)
4.2.3. Size and Topography of Lymph Nodes
4.2.4. Endoscopist Experience
4.2.5. Number of Passes
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Hutchinson, J. Anomalous Diseases of Skin and Fingers: Case of Livid Papillary psoriasis? Illus. Clin. Surg. 1877, 1, 42. [Google Scholar]
- Valeyre, D.; Prasse, A.; Nunes, H.; Uzunhan, Y.; Brillet, P.Y.; Müller-Quernheim, J. Sarcoidosis. Lancet 2014, 383, 1155–1167. [Google Scholar] [CrossRef]
- Cardoso, A.V.; Mota, P.C.; Melo, N.; Guimarães, S.; Souto Moura, C.; Jesus, J.M.; Cunha, R.; Morais, A. Analysis of sarcoidosis in the Oporto region (Portugal). Revis. Port. Pneumol. 2017, 23, 251–258. [Google Scholar] [CrossRef]
- Baughman, R.P.; Culver, D.A.; Judson, M.A. A concise review of pulmonary sarcoidosis. Am. J. Respir. Crit. Care Med. 2011, 183, 573–581. [Google Scholar] [CrossRef]
- ATS/ERS/WASOG. Statement on sarcoidosis. Joint Statement of the American Thoracic Society (ATS), the European Respiratory Society (ERS) and the World Association of Sarcoidosis and Other Granulomatous Disorders (WASOG) adopted by the ATS Board of Directors and by the ER. Am. J. Respir. Crit. Care Med. 1999, 160, 736–755. [Google Scholar]
- Judson, M.A.; Thompson, B.W.; Rabin, D.L.; Steimel, J.; Knattereud, G.L.; Lackland, D.T.; Rose, C.; Rand, C.S.; Baughman, R.P.; Teirstein, A.S.; et al. The diagnostic pathway to sarcoidosis. Chest 2003, 123, 406–412. [Google Scholar] [CrossRef]
- Baughman, R.P.; Teirstein, A.S.; Judson, M.A.; Rossman, M.D.; Yeager, H., Jr.; Bresnitz, E.A.; Depalo, L.; Hunninghake, G.; Iannuzzi, M.C.; Johns, C.J.; et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am. J. Respir. Crit. Care Med. 2001, 164, 1885–1889. [Google Scholar] [CrossRef]
- Nagai, S.; Shigematsu, M.; Hamada, K.; Izumi, T. Clinical courses and prognoses of pulmonary sarcoidosis. Curr. Opin. Pulm. Med. 1999, 5, 293–298. [Google Scholar] [CrossRef]
- Scadding, J.G. Prognosis of intrathoracic sarcoidosis in England. A review of 136 cases after five years’ observation. Br. Med. J. 1961, 2, 1165–1172. [Google Scholar] [CrossRef]
- Israel-Biet, D.; Valeyre, D. Diagnosis of pulmonary sarcoidosis. Curr. Opin. Pulm. Med. 2013, 19, 510–515. [Google Scholar] [CrossRef]
- Mondoni, M.; Radovanovic, D.; Valenti, V.; Patella, V.; Santus, P. Bronchoscopy in sarcoidosis: Union is strength. Minerva Med. 2015, 63, 401–410. [Google Scholar]
- Culver, D.A. Diagnosing sarcoidosis. Curr. Opin. Pulm. Med. 2015, 21, 499–509. [Google Scholar] [CrossRef]
- Mota, P.C.; Morais, A.; Palmares, C.; Beltrão, M.; Melo, N.; Santos, A.C.; Delgado, L. Diagnostic value of CD103 expression in bronchoalveolar lymphocytes in sarcoidosis. Respir. Med. 2012, 106, 1014–1020. [Google Scholar] [CrossRef][Green Version]
- Poletti, V.; Casoni, G.L.; Gurioli, C.; Ryu, J.H.; Tomassetti, S. Lung cryobiopsies: A paradigm shift in diagnostic bronchoscopy? Respirology 2014, 19, 645–654. [Google Scholar] [CrossRef]
- Goyal, A.; Gupta, D.; Agarwal, R.; Bal, A.; Nijhawan, R.; Aggarwal, A.N. Value of different bronchoscopic sampling techniques in diagnosis of sarcoidosis: A prospective study of 151 patients. J. Bronchol. Interv. Pulmonol. 2014, 21, 220–226. [Google Scholar] [CrossRef]
- Benzaquen, S.; Aragaki-Nakahodo, A.A. Bronchoscopic modalities to diagnose sarcoidosis. Curr. Opin. Pulm. Med. 2017, 23, 433–438. [Google Scholar] [CrossRef]
- Oki, M.; Saka, H.; Kitagawa, C.; Kogure, Y.; Murata, N.; Ichihara, S.; Moritani, S. Prospective study of endobronchial ultrasound-guided transbronchial needle aspiration of lymph nodes versus transbronchial lung biopsy of lung tissue for diagnosis of sarcoidosis. J. Thorac. Cardiovasc. Surg. 2012, 143, 1324–1329. [Google Scholar] [CrossRef]
- Plit, M.; Pearson, R.; Havryk, A.; Da Costa, J.; Chang, C.; Glanville, A.R. Diagnostic utility of endobronchial ultrasound-guided transbronchial needle aspiration compared with transbronchial and endobronchial biopsy for suspected sarcoidosis. Intern. Med. J. 2012, 42, 434–438. [Google Scholar] [CrossRef]
- Agarwal, R.; Aggarwal, A.N.; Gupta, D. Efficacy and safety of conventional transbronchial needle aspiration in sarcoidosis: A systematic review and meta-analysis. Respir. Care 2013, 58, 683–693. [Google Scholar]
- Madan, K.; Dhungana, A.; Mohan, A.; Hadda, V.; Jain, D.; Arava, S.; Pandey, R.M.; Khilnani, G.C.; Guleria, R. Conventional Transbronchial Needle Aspiration Versus Endobronchial Ultrasound-guided Transbronchial Needle Aspiration, with or Without Rapid On-Site Evaluation, for the Diagnosis of Sarcoidosis: A Randomized Controlled Trial. J. Bronchol. Interv. Pulmonol. 2017, 24, 48–58. [Google Scholar] [CrossRef]
- Trisolini, R.; Agli, L.L.; Cancellieri, A.; Poletti, V.; Tinelli, C.; Baruzzi, G.; Patelli, M. The Value of Flexible Transbronchial Needle Aspiration in the Diagnosis of Stage I Sarcoidosis. Chest 2003, 124, 2126–2130. [Google Scholar] [CrossRef]
- Vilmann, P.; Krasnik, M.; Larsen, S.S.; Jacobsen, G.K.; Clementsen, P. Transesophageal endoscopic ultrasound-guided fine-needle aspiration (EUS-FNA) and endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA) biopsy: A combined approach in the evaluation of mediastinal lesions. Endoscopy 2005, 37, 833–839. [Google Scholar] [CrossRef]
- Bonifazi, M.; Tramacere, I.; Zuccatosta, L.; Mei, F.; Sediari, M.; Paonessa, M.C.; Gasparini, S. Conventional versus Ultrasound-Guided Transbronchial Needle Aspiration for the Diagnosis of Hilar/Mediastinal Lymph Adenopathies: A Randomized Controlled Trial. Respiration 2017, 94, 216–223. [Google Scholar] [CrossRef]
- Semenzato, G. ACCESS: A Case Control Etiologic Study of Sarcoidosis. Sarcoidosis Vasc. Diffus Lung Dis. 2005, 22, 83–86. [Google Scholar]
- Micames, C.G.; McCrory, D.C.; Pavey, D.A.; Jowell, P.S.; Gress, F.G. Endoscopic ultrasound-guided fine-needle aspiration for non-small cell lung cancer staging: A systematic review and metaanalysis. Chest 2007, 131, 539–548. [Google Scholar] [CrossRef]
- Li, K.; Jiang, S. A randomized controlled study of conventional TBNA versus EBUS-TBNA for diagnosis of suspected stage I and II sarcoidosis. Sarcoidosis Vasc. Diffus Lung Dis. 2014, 31, 211–218. [Google Scholar]
- Tremblay, A.; Stather, D.R.; MacEachern, P.; Khalil, M.; Field, S.K. A randomized controlled trial of standard vs endobronchial ultrasonography-guided transbronchial needle aspiration in patients with suspected sarcoidosis. Chest 2009, 136, 340–346. [Google Scholar] [CrossRef]
- Nakajima, T.; Yasufuku, K.; Kurosu, K.; Takiguchi, Y.; Fujiwara, T.; Chiyo, M.; Shibuya, K.; Hiroshima, K.; Nakatani, Y.; Yoshino, I. The role of EBUS-TBNA for the diagnosis of sarcoidosis - comparisons with other bronchoscopic diagnostic modalities. Respir. Med. 2009, 103, 1796–1800. [Google Scholar] [CrossRef]
- Eckardt, J.; Olsen, K.E.; Jørgensen, O.D. Minimally invasive diagnosis of sarcoidosis by EBUS when conventional diagnosis fail. Sarcoidosis Vasc. Diffus Lung Dis. 2010, 27, 43–48. [Google Scholar]
- Annema, J.T.; Veselic, M.; Rabe, K.F. Endoscopic ultrasound-guided fine-needle aspiration for the diagnosis of sarcoidosis. Eur. Respir. J. 2005, 25, 405–409. [Google Scholar] [CrossRef]
- Fritscher-Ravens, A.; Sriram, P.V.J.; Topalidis, T.; Hauber, H.P.; Meyer, A.; Soehendra, N.; Pforte, A. Diagnosing sarcoidosis using endosonography-guided fine-needle aspiration. Chest 2000, 118, 928–935. [Google Scholar] [CrossRef]
- Oki, M.; Saka, H.; Kitagawa, C.; Kogure, Y.; Murata, N.; Adachi, T.; Ichihara, S.; Moritani, S. Transesophageal bronchoscopic ultrasound-guided fine needle aspiration for diagnosis of sarcoidosis. Respiration 2013, 85, 137–143. [Google Scholar] [CrossRef]
- Tournoy, K.G.; Bolly, A.; Aerts, J.G.; Pierard, P.; De Pauw, R.; Leduc, D.; Leloup, A.; Pieters, T.; Slabbynck, H.; Janssens, A.; et al. The value of endoscopic ultrasound after bronchoscopy to diagnose thoracic sarcoidosis. Eur. Respir. J. 2010, 35, 1329–1335. [Google Scholar] [CrossRef]
- Aragaki-Nakahodo, A.A.; Baughman, R.P.; Shipley, R.T.; Benzaquen, S. The complimentary role of transbronchial lung cryobiopsy and endobronchial ultrasound fine needle aspiration in the diagnosis of sarcoidosis. Respir. Med. 2017, 131, 65–69. [Google Scholar] [CrossRef]
- Dziedzic, D.A.; Peryt, A.; Orlowski, T. The role of EBUS-TBNA and standard bronchoscopic modalities in the diagnosis of sarcoidosis. Clin. Respir. J. 2017, 11, 58–63. [Google Scholar] [CrossRef]
- Shorr, A.F.; Torrington, K.G.; Hnatiuk, O.W. Endobronchial involvement and airway hyperreactivity in patients with sarcoidosis. Chest 2001, 120, 881–886. [Google Scholar] [CrossRef]
- von Bartheld, M.B.; Dekkers, O.M.; Szlubowski, A.; Eberhardt, R.; Herth, F.J.; de Jong, Y.P.; van der Heijden, E.H.F.M.; Tournoy, K.G.; Claussen, M.; van den Blink, B.; et al. Endosonography vs conventional bronchoscopy for the diagnosis of sarcoidosis: The Granuloma randomized clinical trial. JAMA 2013, 309, 2457–2464. [Google Scholar] [CrossRef]
- Bonifazi, M.; Zuccatosta, L.; Trisolini, R.; Moja, L.; Gasparini, S. Transbronchial needle aspiration: A systematic review on predictors of a successful aspirate. Respiration 2013, 86, 123–134. [Google Scholar] [CrossRef]
- Holty, J.E.C.; Kuschner, W.G.; Gould, M.K. Accuracy of transbronchial needle aspiration for mediastinal staging of non-small cell lung cancer: A meta-analysis. Thorax 2005, 60, 949–955. [Google Scholar] [CrossRef]
- Khan, A.; Agarwal, R.; Aggarwal, A.N.; Gupta, N.; Bal, A.; Singh, N.; Gupta, D. Blind transbronchial needle aspiration without an on-site cytopathologist: Experience of 473 procedures. Natl. Med. J. India 2011, 24, 136. [Google Scholar]
- Bilaçeroğlu, S.; Perim, K.; Günel, O.; Cağirici, U.; Büyükşirin, M. Combining transbronchial aspiration with endobronchial and transbronchial biopsy in sarcoidosis. Monaldi Arch. Chest Dis. 1999, 54, 217–223. [Google Scholar]
- Trisolini, R.; Lazzari, L.A.; Cancellieri, A.; Poletti, V.; Candoli, P.; Paioli, D.; Alifano, M.; Tinelli, C.; Patelli, M. Transbronchial needle aspiration improves the diagnostic yield of bronchoscopy in sarcoidosis. Sarcoidosis Vasc. Diffus Lung Dis. 2004, 21, 147–151. [Google Scholar]
- Cameron, S.E.H.; Andrade, R.S.; Pambuccian, S.E. Endobronchial ultrasound-guided transbronchial needle aspiration cytology: A state of the art review. Cytopathology 2010, 21, 6–26. [Google Scholar] [CrossRef]
- Costabel, U.; Zaiss, A.; Guzman, J. Sensitivity and specifity of BAL findings in sarcoidosis. Sarcoidosis 1992, 9, 211–214. [Google Scholar]
- Winterbauer, R.H.; Lammert, J.; Selland, M.; Wu, R.; Corley, D.; Springmeyer, S.C. Bronchoalveolar lavage cell populations in the diagnosis of sarcoidosis. Chest 1993, 104, 352–361. [Google Scholar] [CrossRef][Green Version]
- Reichenberger, F.; Kleiber, B.; Baschiera, B.; Bubendorf, L.; Brutsche, M.; Dalquen, P.; Tamm, M. Bronchoalveolar lavage quality influences the T4/T8 ratio in sarcoidosis. Respir. Med. 2007, 101, 2025–2030. [Google Scholar] [CrossRef][Green Version]
- Thomeer, M.; Demedts, M. Predictive value of CD4/CD8 ratio in bronchoalveolar lavage in the diagnosis of sarcoidosis. Sarcoidosis Vasc. Diffus Lung Dis. 1997, 14, 36. [Google Scholar]
- Costabel, U. CD4/CD8 ratios in bronchoalveolar lavage fluid: Of value for diagnosing sarcoidosis? Eur. Respir. J. 1997, 10, 2699–2700. [Google Scholar] [CrossRef]
- Kantrow, S.P.; Meyer, K.C.; Kidd, P.; Raghu, G. The CD4/CD8 ratio in BAL fluid is highly variable in sarcoidosis. Eur. Respir. J. 1997, 10, 2716–2721. [Google Scholar] [CrossRef]
- Fuso, L.; Varone, F.; Magnini, D.; Calvello, M.; Lo Greco, E.; Richeldi, L. Ultrasonography of the Mediastinum: Techniques, Current Practice, and Future Directions. Respir. Care 2018, 63, 1421–1438. [Google Scholar] [CrossRef]
- Nakajima, T.; Yasufuku, K.; Yoshino, I. Current status and perspective of EBUS-TBNA. Gen. Thorac. Cardiovasc. Surg. 2013, 61, 390–396. [Google Scholar] [CrossRef]
- Agarwal, R.; Srinivasan, A.; Aggarwal, A.N.; Gupta, D. Efficacy and safety of convex probe EBUS-TBNA in sarcoidosis: A systematic review and meta-analysis. Respir. Med. 2012, 106, 883–892. [Google Scholar] [CrossRef]
- Fernandes, M.; Santos, V.; Martins, N.; Sucena, M.; Passos, M.; Marques, M.; Magalhães, A.; Bugalho, A. Endobronchial Ultrasound under Moderate Sedation versus General Anesthesia. J. Clin. Med. 2018, 7, 421. [Google Scholar] [CrossRef]
- Ribeiro, C.; Oliveira, A.; Neves, S.; Campainha, S.; Nogueira, C.; Torres, S.; Brito, M.C.C.; Almeida, J.; e Sá, J.M.M. Diagnosis of sarcoidosis in the Endobronchial Ultrasound-guided Transbronchial Needle Aspiration era. Rev. Port. Pneumol. 2014, 20, 237–241. [Google Scholar] [CrossRef]
- Toloza, E.M.; Harpole, L.; Detterbeck, F.; McCrory, D.C. Invasive staging of non-small cell lung cancer: A review of the current evidence. Chest 2003, 123, 157S–166S. [Google Scholar] [CrossRef]
- Neves, I.; Sucena, M.; Magalhães, A.; Fernandes, G. EBUS in pulmonary sarcoidosis: What to expect? Rev. Port. Pneumol. 2014, 20, 229–231. [Google Scholar] [CrossRef]
- Wang, Z.; Jiang, C. Endoscopic ultrasound in the diagnosis of mediastinal diseases. Open Med. 2015, 10, 560–565. [Google Scholar] [CrossRef]
- Trisolini, R.; Lazzari Agli, L.; Tinelli, C.; De Silvestri, A.; Scotti, V.; Patelli, M. Endobronchial ultrasound-guided transbronchial needle aspiration for diagnosis of sarcoidosis in clinically unselected study populations. Respirology 2015, 20, 226–234. [Google Scholar] [CrossRef]
- Von Bartheld, M.B.; Veselic-Charvat, M.; Rabe, K.F.; Annema, J.T. Endoscopic ultrasound-guided fine-needle aspiration for the diagnosis of sarcoidosis. Endoscopy 2010, 42, 213–217. [Google Scholar] [CrossRef]
- Hu, L.X.; Chen, R.X.; Huang, H.; Shao, C.; Wang, P.; Liu, Y.Z.; Xu, Z.J. Endobronchial ultrasound-guided transbronchial needle aspiration versus standard bronchoscopic modalities for diagnosis of sarcoidosis: A meta-analysis. Chin. Med. J. (Engl.) 2016, 129, 1607–1615. [Google Scholar] [CrossRef]
- Gnass, M.; Szlubowski, A.; Soja, J.; Kocoń, P.; Rudnicka, L.; Ćmiel, A.; Sładek, K.; Kuzdzal, J. Comparison of conventional and ultrasound-guided needle biopsy techniques in the diagnosis of sarcoidosis: A randomized trial. Pol. Arch. Med. Wewn. 2015, 125, 321–328. [Google Scholar] [CrossRef]
- Kocoń, P.; Szlubowski, A.; Kuzdzał, J.; Rudnicka-Sosin, L.; Ćmiel, A.; Soja, J.; Włodarczyk, J.R.; Talar, P.; Smȩder, T.; Gil, T.; et al. Endosonography-guided fine-needle aspiration in the diagnosis of sarcoidosis: A randomized study. Pol. Arch. Intern. Med. 2017, 127, 154–162. [Google Scholar]
- Dhooria, S.; Aggarwal, A.N.; Gupta, D.; Behera, D.; Agarwal, R. Utility and Safety of Endoscopic Ultrasound With Bronchoscope-Guided Fine-Needle Aspiration in Mediastinal Lymph Node Sampling: Systematic Review and Meta-Analysis. Respir. Care 2015, 60, 1040–1050. [Google Scholar] [CrossRef]
- Hwangbo, B.; Lee, H.S.; Lee, G.K.; Lim, K.Y.; Lee, S.H.; Kim, H.Y.; Lee, J.Y.; Zo, J.I. Transoesophageal needle aspiration using a convex probe ultrasonic bronchoscope. Respirology 2009, 14, 843–849. [Google Scholar] [CrossRef]
- Bugalho, A.; de Santis, M.; Szlubowski, A.; Rozman, A.; Eberhardt, R. Trans-esophageal endobronchial ultrasound-guided needle aspiration (EUS-B-NA): A road map for the chest physician. Pulmonology 2018, 24, 32–41. [Google Scholar] [CrossRef]
- Balli, T.; Krishna, G.; Moeller, P.; Hetzel, J.; Babiak, A.; Fritz, P.; Hetzel, M. Transbronchial Cryobiopsy: A New Tool for Lung Biopsies. Respiration 2009, 78, 203–208. [Google Scholar]
- Kropski, J.A.; Pritchett, J.M.; Mason, W.R.; Sivarajan, L.; Gleaves, L.A.; Johnson, J.E.; Lancaster, L.H.; Lawson, W.E.; Blackwell, T.S.; Steele, M.P.; et al. Bronchoscopic cryobiopsy for the diagnosis of diffuse parenchymal lung disease. PLoS ONE 2013, 8, e78674. [Google Scholar] [CrossRef]
- Casoni, G.L.; Tomassetti, S.; Cavazza, A.; Colby, T.V.; Dubini, A.; Ryu, J.H.; Carretta, E.; Tantalocco, P.; Piciucchi, S.; Ravaglia, C.; et al. Transbronchial lung cryobiopsy in the diagnosis of fibrotic interstitial lung diseases. PLoS ONE 2014, 9, e86716. [Google Scholar] [CrossRef]
- Almeida, L.M.; Lima, B.; Mota, P.C.; Melo, N.; Magalhães, A.; Pereira, J.M.; Moura, C.S.; Guimarães, S.; Morais, A. Learning curve for transbronchial lung cryobiopsy in diffuse lung disease. Pulmonology 2018, 24, 23–31. [Google Scholar] [CrossRef]
- Johannson, K.A.; Marcoux, V.S.; Ronksley, P.E.; Ryerson, C.J. Diagnostic yield and complications of transbronchial lung cryobiopsy for interstitial lung disease. A systematic review and metaanalysis. Ann. Am. Thorac. Soc. 2016, 13, 1828–1838. [Google Scholar]
- Hagmeyer, L.; Theegarten, D.; Wohlschläger, J.; Treml, M.; Matthes, S.; Priegnitz, C.; Randerath, W.J. The role of transbronchial cryobiopsy and surgical lung biopsy in the diagnostic algorithm of interstitial lung disease. Clin. Respir. J. 2016, 10, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Ravaglia, C.; Bonifazi, M.; Wells, A.U.; Tomassetti, S.; Gurioli, C.; Piciucchi, S.; Dubini, A.; Tantalocco, P.; Sanna, S.; Negri, E.; et al. Safety and diagnostic yield of transbronchial lung cryobiopsy in diffuse parenchymal lung diseases: A comparative study versus video-assisted thoracoscopic lung biopsy and a systematic review of the literature. Respiration 2016, 91, 215–227. [Google Scholar] [CrossRef]
- Dhooria, S.; Behera, D.; Aggarwal, A.N.; Sehgal, I.S.; Agarwal, R. Diagnostic Yield and Safety of Cryoprobe Transbronchial Lung Biopsy in Diffuse Parenchymal Lung Diseases: Systematic Review and Meta-Analysis. Respir. Care 2016, 61, 700–712. [Google Scholar] [CrossRef] [PubMed]
- Caldas Marçôa, A.R.; Linhas, R.; Apolinario, D.; Oliveira, A.; Nogueira, C.; Loureiro, A.; Almeida, J.; Costa, F.; Sanches, A.; Neves, S. Diagnostic yield of transbronchial lung cryobiopsy in interstitial lung diseases. Eur. Respir. J. 2017, 50, PA3023. [Google Scholar]
- Christophi, G.P.; Caza, T.; Curtiss, C.; Gumber, D.; Massa, P.T.; Landas, S.K. Gene expression profiles in granuloma tissue reveal novel diagnostic markers in sarcoidosis. Exp. Mol. Pathol. 2014, 96, 393–399. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Dadhwal, D.S.; Agarwal, R.; Gupta, N.; Bal, A.; Aggarwal, A.N. Endobronchial ultrasound-guided transbronchial needle aspiration vs conventional transbronchial needle aspiration in the diagnosis of sarcoidosis. Chest 2014, 146, 547–556. [Google Scholar] [CrossRef] [PubMed]
- Prasad, K.T.; Dhooria, S.; Sehgal, I.S.; Muthu, V.; Ram, B.; Gupta, N.; Aggarwal, A.N.; Agarwal, R. Endobronchial ultrasound-guided transbronchial needle aspiration in the economically disadvantaged: A retrospective analysis of 1582 individuals. Lung India 2018, 35, 483. [Google Scholar]
- Navani, N.; Booth, H.L.; Kocjan, G.; Falzon, M.; Capitanio, A.; Brown, J.M.; Porter, J.C.; Janes, S.M. Combination of endobronchial ultrasound-guided transbronchial needle aspiration with standard bronchoscopic techniques for the diagnosis of stage I and stage II pulmonary sarcoidosis. Respirology 2011, 16, 467–472. [Google Scholar] [CrossRef]
- Plit, M.L.; Havryk, A.P.; Hodgson, A.; James, D.; Field, A.; Carbone, S.; Glanville, A.R.; Bashirzadeh, F.; Chay, A.M.; Hundloe, J.; et al. Rapid cytological analysis of endobronchial ultrasound-guided aspirates in sarcoidosis. Eur. Respir. J. 2013, 42, 1302–1308. [Google Scholar] [CrossRef]
- Zhang, S.; Ma, W.X.; Jiang, S.J.; Li, Y.T.; Wang, Y.K. Diagnosis value of fiberoptic in sarcoidosis. Int. J. Respir. 2011, 31, 605–608. [Google Scholar]
- Hong, G.; Lee, K.J.; Jeon, K.; Koh, W.J.; Suh, G.Y.; Chung, M.P.; Kim, H.; Kwon, O.J.; Han, J.; Um, S.W. Usefulness of endobronchial ultrasound-guided transbronchial needle aspiration for diagnosis of sarcoidosis. Yonsei Med. J. 2013, 54, 1416–1421. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Von Bartheld, M.B.; Van Breda, A.; Annema, J.T. Complication rate of endosonography (endobronchial and endoscopic ultrasound): A systematic review. Respiration 2014, 87, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Bohle, W.; Zoller, W. Mediastinitis after EUS-FNA in a patient with sarcoidosis - case report with endosonographic features and review of the literature. Z. Gastroenterol. 2014, 52, 1171–1174. [Google Scholar] [CrossRef] [PubMed]
- Gimeno-García, A.Z.; Elwassief, A.; Paquin, S.C.; Gariépy, G.; Sahai, A.V. Randomized controlled trial comparing stylet-free endoscopic ultrasound-guided fine-needle aspiration with 22-G and 25-G needles. Dig. Endosc. 2014, 26, 467–473. [Google Scholar] [CrossRef] [PubMed]
- Varadarajulu, S.; Fraig, M.; Schmulewitz, N.; Roberts, S.; Wildi, S.; Hawes, R.H.; Hoffman, B.J.; Wallace, M.B. Comparison of EUS-guided 19-gauge Trucut needle biopsy with EUS-guided fine-needle aspiration. Endoscopy 2004, 36, 397–401. [Google Scholar] [CrossRef] [PubMed]
- Muthu, V.; Gupta, N.; Dhooria, S.; Sehgal, I.S.; Bal, A.; Aggarwal, A.N.; Behera, D.; Agarwal, R. A prospective, randomized, double-blind trial comparing the diagnostic yield of 21- and 22-gauge aspiration needles for performing endobronchial ultrasound-guided transbronchial needle aspiration in sarcoidosis: To the editor. Chest 2016, 149, 1111–1113. [Google Scholar] [CrossRef] [PubMed]
- Tyan, C.; Patel, P.; Czarnecka, K.; Gompelmann, D.; Eberhardt, R.; Fortin, M.; Maceachern, P.; Hergott, C.A.; Dumoulin, E.; Tremblay, A.; et al. Flexible 19-gauge endobronchial ultrasound-guided transbronchial needle aspiration needle: First experience. Respiration 2017, 94, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Choi, Y.R.; An, J.Y.; Kim, M.K.; Han, H.S.; Lee, K.H.; Kim, S.W.; Lee, K.M.; Choe, K.H. The diagnostic efficacy and safety of endobronchial ultrasound-guided transbronchial needle aspiration as an initial diagnostic tool. Korean J. Intern. Med. 2013, 28, 660–667. [Google Scholar] [CrossRef]
- Bonifazi, M.; Sediari, M.; Ferretti, M.; Poidomani, G.; Tramacere, I.; Mei, F.; Zuccatosta, L.; Gasparini, S. The role of the pulmonologist in rapid on-site cytologic evaluation of transbronchial needle aspiration: A prospective study. Chest 2014, 145, 60–65. [Google Scholar] [CrossRef]
- Burge, P.S.; Reynolds, J.; Trotter, S.; Burge, G.A.; Walters, G. Histologist’s original opinion compared with multidisciplinary team in determining diagnosis in interstitial lung disease. Thorax 2017, 72, 280–281. [Google Scholar] [CrossRef]
- Gianella, P.; Soccal, P.M.; Plojoux, J.; Frésard, I.; Pache, J.C.; Perneger, T.; Gex, G. Utility of rapid on-site cytologic evaluation during endobronchial ultrasound-guided transbronchial needle aspiration in malignant and nonmalignant disease. Acta Cytol. 2018, 62, 380–385. [Google Scholar] [CrossRef] [PubMed]
- Cardoso, A.V.; Neves, I.; Magalhães, A.; Sucena, M.; Barroca, H.; Fernandes, G. The value of rapid on-site evaluation during EBUS-TBNA. Rev. Port. Pneumol. 2015, 21, 253–258. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, I.S.; Dhooria, S.; Aggarwal, A.N.; Agarwal, R. Impact of Rapid On-Site Cytological Evaluation (ROSE) on the Diagnostic Yield of Transbronchial Needle Aspiration During Mediastinal Lymph Node Sampling: Systematic Review and Meta-Analysis. Chest 2018, 153, 929–938. [Google Scholar] [CrossRef] [PubMed]
- Abu-Hijleh, M.; El-Sameed, Y.; Eldridge, K.; Vadia, E.; Chiu, H.; Dreyfuss, Z.; Al Rabadi, L.S. Linear probe endobronchial ultrasound bronchoscopy with guided transbronchial needle aspiration (EBUS-TBNA) in the evaluation of mediastinal and hilar pathology: Introducing the procedure to a teaching institution. Lung 2013, 191, 109–115. [Google Scholar] [CrossRef] [PubMed]
- Cetinkaya, E.; Ozgül, M.A.; Tutar, N.; Ozgül, G.; Cam, E.; Bilaçeroglu, S. The diagnostic utility of real-time EBUS-TBNA for hilar and mediastinal lymph nodes in conventional TBNA negative patients. Ann. Thorac. Cardiovasc. Surg. 2014, 20, 106–112. [Google Scholar] [CrossRef] [PubMed]
- Folch, E.; Majid, A. Point: Are> 50 supervised procedures required to develop competency in performing endobronchial ultrasound-guided transbronchial needle aspiration for mediastinal staging? Yes. Chest 2013, 143, 888–891. [Google Scholar] [CrossRef] [PubMed]
- Kinsey, C.M.; Channick, C.L. Counterpoint: Are> 50 supervised procedures required to develop competency in performing endobronchial ultrasound-guided transbronchial needle aspiration for lung cancer staging? No. Chest 2013, 143, 891–893. [Google Scholar] [CrossRef] [PubMed]
- Stather, D.R.; Maceachern, P.; Rimmer, K.; Hergott, C.A.; Tremblay, A. Assessment and learning curve evaluation of endobronchial ultrasound skills following simulation and clinical training. Respirology 2011, 16, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Stather, D.R.; Mac Eachern, P.; Chee, A.; Dumoulin, E.; Tremblay, A. Evaluation of clinical endobronchial ultrasound skills following clinical versus simulation training. Respirology 2012, 17, 291–299. [Google Scholar] [CrossRef]
- Sehgal, I.S.; Dhooria, S.; Aggarwal, A.N.; Agarwal, R. Training and proficiency in endobronchial ultrasound-guided transbronchial needle aspiration: A systematic review. Respirology 2017, 22, 1547–1557. [Google Scholar] [CrossRef]
- Detterbeck, F.C.; Jantz, M.A.; Wallace, M.; Vansteenkiste, J.; Silvestri, G.A. Invasive mediastinal staging of lung cancer: ACCP evidence-based clinical practice guidelines. Chest 2007, 132, 202S–220S. [Google Scholar] [CrossRef] [PubMed]
- Urquiza, M.P.; Fernández-Esparrach, G.; Solé, M.; Colomo, L.; Castells, A.; Llach, J.; Mata, A.; Bordas, J.M.; Piqué, J.M.; Ginès, À. Endoscopic ultrasound-guided fine needle aspiration: Predictive factors of accurate diagnosis and cost-minimization analysis of on-site pathologist. Gastroenterol. Y Hepatol. 2007, 30, 319–324. [Google Scholar] [CrossRef]
| Techniques | Diagnostic Yield | References | |
|---|---|---|---|
| Standard | EBB | 20–61% | [15,16] |
| TBLB | 37–90% | [16,17,18] | |
| cTBNA | 6–90% | [16,19,20,21] | |
| Recent | EBUS-TBNA | 80–94% | [16,22,23,24,25,26,27,28,29] |
| EUS-FNA | 77–94% | [16,30,31,32,33] | |
| EUS-B-FNA | 86% (*) | [32] | |
| TBLC | 66.7% (*) | [34] |
| Study/Year | Scadding Stage | Number of Patients, n | EBUS-TBNA (%) | TBNA (%) | TBLB (%) | EBB (%) | TBLB + EBB (%) | EBUS-TBNA or EUS-FNA | EBUS-TBNA Group (%) | TBNA Group (%) | EUS-B-FNA | EBUS-TBNA + EUS-FNA |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| RCT | ||||||||||||
| Tremblay et al., 2009 * [27] | I or II | 50 | 83.3 | 60.9 | - | - | - | - | - | - | - | - |
| Bartheld et al., 2013 * [37] | I, II, III | 304 | - | - | - | 53.0 | 80.0 | - | - | - | - | |
| Gupta et al., 2014 * [77] | I or II | 117 | 74.5 | 48.4 | 69.6 | 36.3 | - | - | 92.7 | 85.5 | - | - |
| Li and Jiang, 2014 * [26] | I or II | 57 | 93.0 | 64.0 | 36.4 | 5.0 | - | - | - | 92.9 | - | - |
| Gnass et al., 2015 * [61] | I or II | 64 | 76.7 | 58.8 | - | - | - | - | - | - | 86.1 | - |
| Prospective | ||||||||||||
| Navani et al., 2011 * [78] | I or II | 27 | 85.0 | - | 29.6 | 11.1 | 33.3 | - | 92.6 | - | - | - |
| Oki et al., 2012 * [17] | I or II | 54 | 94.0 | - | 37.0 | - | - | - | - | - | - | - |
| Plit et al., 2013 * [79] | I or II | 49 | 91.8 | - | 67.3 | 28.6 | - | - | - | - | - | - |
| Goyal et al., 2014 * [15] | I, II, III, IV | 151 | 57.1 | 22.4 | 68.7 | 49.6 | 81.4 | - | 86.4 | 86.9 | - | - |
| Kocón et al., 2017 [62] | I or II | 100 | 61.9 | 44.0 | 42.0 | 12.0 | - | - | - | - | 74.55 | 80.0 |
| Retrospective | ||||||||||||
| Nakajima et al., 2009 * [28] | I or II | 35 | 91.4 | - | 40.0 | - | - | - | - | - | - | - |
| Zhang et al., 2011 * [80] | I, II, III | 50 | 86.7 | 82.5 | - | - | 66.7 | - | - | - | - | - |
| Plit et al., 2012 * [18] | I or II | 37 | 84.0 | - | 78.0 | 27.0 | - | - | 100.0 | - | - | - |
| Hong et al., 2013 * [81] | I or II | 31 | 90.0 | - | 35.0 | 6.0 | 39.0 | - | 94.0 | - | - | - |
| Dziedzic et al., 2015 * [35] | I or II | 653 | 84.0 | - | 43.9 | 29.7 | 54.0 | - | 89.0 | - | - | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pedro, C.; Melo, N.; Novais e Bastos, H.; Magalhães, A.; Fernandes, G.; Martins, N.; Morais, A.; Caetano Mota, P. Role of Bronchoscopic Techniques in the Diagnosis of Thoracic Sarcoidosis. J. Clin. Med. 2019, 8, 1327. https://doi.org/10.3390/jcm8091327
Pedro C, Melo N, Novais e Bastos H, Magalhães A, Fernandes G, Martins N, Morais A, Caetano Mota P. Role of Bronchoscopic Techniques in the Diagnosis of Thoracic Sarcoidosis. Journal of Clinical Medicine. 2019; 8(9):1327. https://doi.org/10.3390/jcm8091327
Chicago/Turabian StylePedro, Cecília, Natália Melo, Hélder Novais e Bastos, Adriana Magalhães, Gabriela Fernandes, Natália Martins, António Morais, and Patrícia Caetano Mota. 2019. "Role of Bronchoscopic Techniques in the Diagnosis of Thoracic Sarcoidosis" Journal of Clinical Medicine 8, no. 9: 1327. https://doi.org/10.3390/jcm8091327
APA StylePedro, C., Melo, N., Novais e Bastos, H., Magalhães, A., Fernandes, G., Martins, N., Morais, A., & Caetano Mota, P. (2019). Role of Bronchoscopic Techniques in the Diagnosis of Thoracic Sarcoidosis. Journal of Clinical Medicine, 8(9), 1327. https://doi.org/10.3390/jcm8091327






