Open Versus Robotic Cystectomy: A Propensity Score Matched Analysis Comparing Survival Outcomes
Abstract
1. Introduction
2. Experimental Section
2.1. Patients and Methods
2.2. Primary and Secondary End Points
2.3. Statistical Analyses
3. Results
3.1. Clinicopathologic Characteristics (Entire Cohort)
3.2. Clinicopathologic Characteristics (Adjusted Cohort)
3.3. Survival Analyses in the Entire Cohort (Unadjusted Cohort)
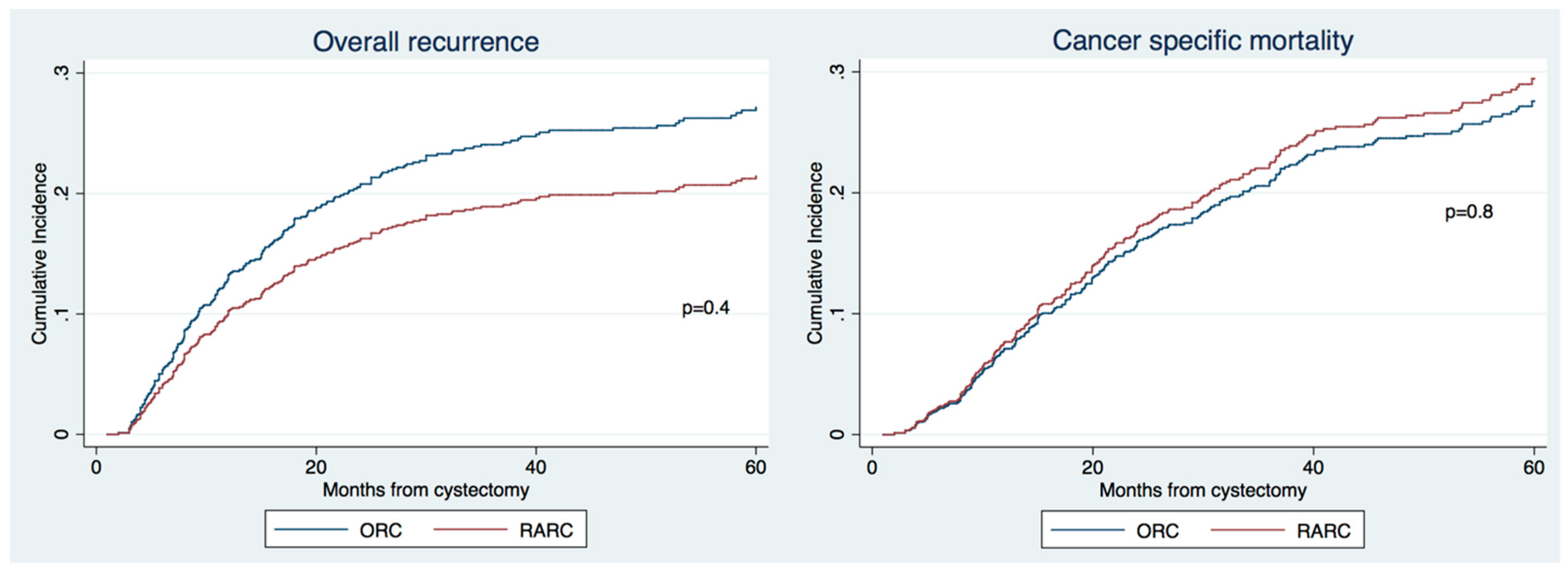
3.4. Survival Analyses after Propensity Matching (Adjusted Cohort)
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Siegel, R.L.; Miller, K.D.; Jemal, A. Cancer statistics, 2018. CA Cancer J. Clin. 2018, 68, 7–30. [Google Scholar] [CrossRef] [PubMed]
- Babjuk, M.; Böhle, A.; Burger, M.; Capoun, O.; Cohen, D.; Compérat, E.M.; Hernández, V.; Kaasinen, E.; Palou, J.; Rouprêt, M.; et al. EAU Guidelines on Non-Muscle-invasive Urothelial Carcinoma of the Bladder: Update 2016. Eur. Urol. 2016, 71, 447–461. [Google Scholar] [CrossRef] [PubMed]
- Moschini, M.; Simone, G.; Stenzl, A.; Gill, I.S.; Catto, J. Critical Review of Outcomes from Radical Cystectomy: Can Complications from Radical Cystectomy Be Reduced by Surgical Volume and Robotic Surgery? Eur. Urol. Focus 2016, 2, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Challacombe, B.J.; Bochner, B.H.; Dasgupta, P.; Gill, I.; Guru, K.; Herr, H.; Mottrie, A.; Pruthi, R.; Redorta, J.P.; Wiklund, P. The Role of Laparoscopic and Robotic Cystectomy in the Management of Muscle-Invasive Bladder Cancer with Special Emphasis on Cancer Control and Complications. Eur. Urol. 2011, 60, 767–775. [Google Scholar] [CrossRef] [PubMed]
- Yu, H.-Y.; Hevelone, N.D.; Lipsitz, S.R.; Kowalczyk, K.J.; Nguyen, P.L.; Choueiri, T.K.; Kibel, A.S.; Hu, J.C. Comparative Analysis of Outcomes and Costs Following Open Radical Cystectomy Versus Robot-Assisted Laparoscopic Radical Cystectomy: Results From the US Nationwide Inpatient Sample. Eur. Urol. 2012, 61, 1239–1244. [Google Scholar] [CrossRef] [PubMed]
- Styn, N.R.; Montgomery, J.S.; Wood, D.P.; Hafez, K.S.; Lee, C.T.; Tallman, C.; He, C.; Crossley, H.; Hollenbeck, B.K.; Weizer, A.Z. Matched comparison of robotic-assisted and open radical cystectomy. Urology 2012, 79, 1303–1309. [Google Scholar] [CrossRef]
- Ng, C.K.; Kauffman, E.C.; Lee, M.-M.; Otto, B.J.; Portnoff, A.; Ehrlich, J.R.; Schwartz, M.J.; Wang, G.J.; Scherr, D.S. A Comparison of Postoperative Complications in Open versus Robotic Cystectomy. Eur. Urol. 2010, 57, 274–282. [Google Scholar] [CrossRef]
- Hanna, N.; Leow, J.J.; Sun, M.; Friedlander, D.F.; Seisen, T.; Abdollah, F.; Lipsitz, S.R.; Menon, M.; Kibel, A.S.; Bellmunt, J.; et al. Comparative effectiveness of robot-assisted vs. open radical cystectomy. Urol. Oncol. Semin. Orig. Investig. 2018, 36, 88.e1–88.e9. [Google Scholar] [CrossRef]
- Hussein, A.A.; May, P.R.; Jing, Z.; Ahmed, Y.E.; Wijburg, C.J.; Canda, A.E.; Dasgupta, P.; Khan, M.S.; Menon, M.; Peabody, J.O.; et al. Outcomes of Intracorporeal Urinary Diversion after Robot-Assisted Radical Cystectomy: Results from the International Robotic Cystectomy Consortium. J. Urol. 2018, 199, 1302–1311. [Google Scholar] [CrossRef]
- Soria, F.; Moschini, M.; D’Andrea, D.; Abufaraj, M.; Foerster, B.; Mathiéu, R.; Gust, K.M.; Gontero, P.; Simone, G.; Meraney, A.; et al. Comparative Effectiveness in Perioperative Outcomes of Robotic versus Open Radical Cystectomy: Results from a Multicenter Contemporary Retrospective Cohort Study. Eur. Urol. Focus 2018. [Google Scholar] [CrossRef]
- Martin, A.D.; Nunez, R.N.; Pacelli, A.; Woods, M.E.; Davis, R.; Thomas, R.; Andrews, P.E.; Castle, E.P. Robot-assisted radical cystectomy: Intermediate survival results at a mean follow-up of 25 months. BJU Int. 2010, 105, 1706–1709. [Google Scholar] [CrossRef]
- Jonsson, M.N.; Adding, L.C.; Hosseini, A.; Schumacher, M.C.; Volz, D.; Nilsson, A.; Carlsson, S.; Wiklund, N.P. Robot-Assisted Radical Cystectomy with Intracorporeal Urinary Diversion in Patients with Transitional Cell Carcinoma of the Bladder. Eur. Urol. 2011, 60, 1066–1073. [Google Scholar] [CrossRef] [PubMed]
- Parekh, D.J.; Reis, I.M.; Castle, E.P.; Gonzalgo, M.L.; Woods, M.E.; Svatek, R.S.; Weizer, A.Z.; Konety, B.R.; Tollefson, M.; Krupski, T.L.; et al. Robot-assisted radical cystectomy versus open radical cystectomy in patients with bladder cancer (RAZOR): An open-label, randomised, phase 3, non-inferiority trial. Lancet 2018, 391, 2525–2536. [Google Scholar] [CrossRef]
- Novara, G.; Svatek, R.S.; Karakiewicz, P.I.; Skinner, E.; Ficarra, V.; Fradet, Y.; Lotan, Y.; Isbarn, H.; Capitanio, U.; Bastian, P.J.; et al. Soft Tissue Surgical Margin Status is a Powerful Predictor of Outcomes After Radical Cystectomy: A Multicenter Study of More Than 4400 Patients. J. Urol. 2010, 183, 2165–2170. [Google Scholar] [CrossRef] [PubMed]
- Xylinas, E.; Rink, M.; Novara, G.; Green, D.A.; Clozel, T.; Fritsche, H.M.; Guillonneau, B.; Lotan, Y.; Kassouf, W.; Tilki, D.; et al. Predictors of survival in patients with soft tissue surgical margin involvement at radical cystectomy. Ann. Surg. Oncol. 2013, 20, 1027–1034. [Google Scholar] [CrossRef] [PubMed]
- Mathieu, R.; Lucca, I.; Rouprêt, M.; Briganti, A.; Shariat, S.F. The prognostic role of lymphovascular invasion in urothelial carcinoma of the bladder. Nat. Rev. Urol. 2016, 13, 471–479. [Google Scholar] [CrossRef]
- Shariat, S.F.; Khoddami, S.M.; Saboorian, H.; Koeneman, K.S.; Sagalowsky, A.I.; Cadeddu, J.A.; McConnell, J.D.; Holmes, M.N.; Roehrborn, C.G. Lymphovascular Invasion is a Pathological Feature of Biologically Aggressive Disease in Patients Treated with Radical Prostatectomy. J. Urol. 2004, 171, 1122–1127. [Google Scholar] [CrossRef]
- Bochner, B.H.; Sjoberg, D.D.; Laudone, V.P. A Randomized Trial of Robot-Assisted Laparoscopic Radical Cystectomy. N. Engl. J. Med. 2014, 371, 389–390. [Google Scholar] [CrossRef]
- Parekh, D.J.; Messer, J.; Fitzgerald, J.; Ercole, B.; Svatek, R. Perioperative outcomes and oncologic efficacy from a pilot prospective randomized clinical trial of open versus robotic assisted radical cystectomy. J. Urol. 2013, 189, 474–479. [Google Scholar] [CrossRef]
- Nix, J.; Smith, A.; Kurpad, R.; Nielsen, M.E.; Wallen, E.M.; Pruthi, R.S. Prospective randomized controlled trial of robotic versus open radical cystectomy for bladder cancer: Perioperative and pathologic results. Eur. Urol. 2010, 57, 196–201. [Google Scholar] [CrossRef]
- Moschini, M.; Soria, F.; Mathieu, R.; Xylinas, E.; D’Andrea, D.; Tan, W.S.; Kelly, J.D.; Simone, G.; Tuderti, G.; Meraney, A.; et al. Propensity-score-matched comparison of soft tissue surgical margins status between open and robotic-assisted radical cystectomy. Urol. Oncol. Semin. Orig. Investig. 2019, 37, 179.e1–179.e7. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.P.; Awamlh, B.A.H.A.; Wu, X.; O’Malley, P.; Inoyatov, I.M.; Ayangbesan, A.; Faltas, B.M.; Christos, P.J.; Scherr, D.S. Recurrence Patterns After Open and Robot-assisted Radical Cystectomy for Bladder Cancer. Eur. Urol. 2015, 68, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Bochner, B.H.; Dalbagni, G.; Marzouk, K.H.; Sjoberg, D.D.; Lee, J.; Donat, S.M.; Coleman, J.A.; Vickers, A.; Herr, H.W.; Laudone, V.P. Randomized Trial Comparing Open Radical Cystectomy and Robot-assisted Laparoscopic Radical Cystectomy: Oncologic Outcomes. Eur. Urol. 2018, 74, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.S.; Gan, C.; Ahmed, K.; Ismail, A.F.; Watkins, J.; Summers, J.A.; Peacock, J.L.; Rimington, P.; Dasgupta, P. A Single-centre Early Phase Randomised Controlled Three-arm Trial of Open, Robotic, and Laparoscopic Radical Cystectomy (CORAL). Eur. Urol. 2016, 69, 613–621. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.C.; Chughtai, B.; O’Malley, P.; Halpern, J.A.; Mao, J.; Scherr, D.S.; Hershman, D.L.; Wright, J.D.; Sedrakyan, A. Perioperative Outcomes, Health Care Costs, and Survival After Robotic-assisted Versus Open Radical Cystectomy: A National Comparative Effectiveness Study. Eur. Urol. 2016, 70, 195–202. [Google Scholar] [CrossRef] [PubMed]
- Sathianathen, N.J.; Kalapara, A.; Frydenberg, M.; Lawrentschuk, N.; Weight, C.J.; Parekh, D.; Konety, B.R. Robotic Assisted Radical Cystectomy vs Open Radical Cystectomy: Systematic Review and Meta-Analysis. J. Urol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Necchi, A.; Pond, G.R.; Smaldone, M.C.; Pal, S.K.; Chan, K.; Wong, Y.-N.; Viterbo, R.; Sonpavde, G.; Harshman, L.C.; Crabb, S.; et al. Robot-assisted Versus Open Radical Cystectomy in Patients Receiving Perioperative Chemotherapy for Muscle-invasive Bladder Cancer: The Oncologist’s Perspective from a Multicentre Study. Eur. Urol. Focus 2018, 4, 937–945. [Google Scholar] [CrossRef]
- Pyun, J.H.; Kim, H.K.; Cho, S.; Kang, S.G.; Cheon, J.; Lee, J.G.; Kim, J.J.; Kang, S.H. Robot-Assisted Radical Cystectomy with Total Intracorporeal Urinary Diversion: Comparative Analysis with Extracorporeal Urinary Diversion. J. Laparoendosc. Adv. Surg. Tech. 2016, 26, 349–355. [Google Scholar] [CrossRef]
- Leow, J.J.; Reese, S.W.; Jiang, W.; Lipsitz, S.R.; Bellmunt, J.; Trinh, Q.-D.; Chung, B.I.; Kibel, A.S.; Chang, S.L. Propensity-Matched Comparison of Morbidity and Costs of Open and Robot-Assisted Radical Cystectomies: A Contemporary Population-Based Analysis in the United States. Eur. Urol. 2014, 66, 569–576. [Google Scholar] [CrossRef]
- Monn, M.F.; Cary, K.C.; Kaimakliotis, H.Z.; Flack, C.K.; Koch, M.O. National trends in the utilization of robotic-assisted radical cystectomy: An analysis using the Nationwide Inpatient Sample. Urol. Oncol. Semin. Orig. Investig. 2014, 32, 785–790. [Google Scholar] [CrossRef]

| Variables | Overall (n = 9757, 100%) | RARC (n = 767, 7.8%) | ORC (n = 8990, 92%) | p Value |
|---|---|---|---|---|
| Age, years | ||||
| Mean | 67 | 67 | 67 | 0.2 |
| Median (IQR) | 68 (60–74) | 68 (62–74) | 68 (60–74) | |
| Gender | ||||
| Male | 7775 (79%) | 612 (80%) | 7163 (80%) | 0.9 |
| Female | 1981 (20%) | 115 (20%) | 1827 (20%) | |
| Neoadjuvant chemotherapy | 520 (5.3%) | 198 (26%) | 322 (3.6%) | <0.001 |
| Pathological T stage | ||||
| pT0-pT1 | 2908 (31%) | 368 (48%) | 2540 (29%) | <0.001 |
| pT2 | 2239 (24%) | 93 (12%) | 2146 (25%) | |
| pT3-pT4 | 4248 (45%) | 305 (40%) | 3943 (46%) | |
| High grade | 8734 (94%) | 361 (76%) | 8373 (94%) | <0.001 |
| LNI | 2276 (24%) | 158 (22%) | 2118 (24%) | 0.001 |
| Nodes removed, number | ||||
| Mean | 20 | 21 | 20 | 0.001 |
| Median (IQR) | 16 (10–26) | 20 (13–28) | 16 (9–25) | |
| Positive surgical margins | 639 (6.7%) | 107 (10.0%) | 532 (6.3%) | <0.001 |
| LVI | 3007 (33%) | 25 (27%) | 2982 (34%) | 0.2 |
| Adjuvant chemotherapy | 1828 (19%) | 85 (13%) | 1743 (20.9%) | <0.001 |
| Variables | Overall (n = 1374, 100%) | RARC (n = 420, 33%) | ORC (n = 840, 67%) | p Value |
|---|---|---|---|---|
| Age, years | ||||
| Mean | 66 | 66 | 66 | 0.9 |
| Median (IQR) | 67 (59–73) | 67 (61–72) | 67 (51–72) | |
| Gender | ||||
| Male | 1003 (80%) | 365 (80%) | 728 (79%) | 0.9 |
| Female | 257 (20%) | 93 (20%) | 188 (21%) | |
| Neoadjuvant chemotherapy | 456 (33%) | 1162 (35%) | 294 (32%) | 0.2 |
| Pathological T stage | ||||
| pT0-pT1 | 535 (39%) | 189 (41%) | 346 (38%) | 0.4 |
| pT2 | 208 (15%) | 52 (11%) | 156 (17%) | |
| pT3-pT4 | 631 (46%) | 217 (47%) | 414 (52%) | |
| High grade | 1075 (78%) | 348 (76%) | 727 (79%) | 0.1 |
| Nodes removed, number | ||||
| Mean | 19 | 22 | 17 | 0.001 |
| Median (IQR) | 16 (10–25) | 19 (14–28) | 14 (8–24) | |
| LNI | 318 (23%) | 109 (24%) | 209 (23%) | 0.6 |
| Positive surgical margins | 115 (8.4%) | 52 (11%) | 63 (7.0%) | 0.006 |
| LVI | 302 (32%) | 23 (45%) | 282 (32%) | 0.04 |
| Adjuvant chemotherapy | 211 (16%) | 45 (12%) | 166 (18%) | 0.004 |
| Variables | Overall Recurrence | CSM | ||
|---|---|---|---|---|
| HR (CI 95%) | p Value | HR (CI 95%) | p Value | |
| Gender (male vs. female) | 1.07 (0.97–1.17) | 0.1 | 1.15 (1.04–1.27) | 0.005 |
| Age, years | 1.00 (0.99–1.00) | 0.5 | 1.00 (0.99–1.00) | 0.052 |
| RARC approach | 0.65 (0.34–1.26) | 0.2 | 1.00 (0.45–2.24) | 0.9 |
| pT stage | ||||
| pT0-pT1 | Ref | Ref | Ref | Ref |
| pT2 | 1.35 (1.18–1.55) | <0.001 | 1.49 (1.27–1.73) | <0.001 |
| pT3-4 | 2.10 (1.84–2.40) | <0.001 | 2.62 (2.27–3.03) | <0.001 |
| pN+ | 1.68 (1.51–1.86) | <0.001 | 2.09 (1.88–2.33) | <0.001 |
| Nodes removed | 0.99 (0.99–1.00) | 0.3 | 0.99 (0.99–1.00) | 0.04 |
| High grade vs. low | 2.53 (1.73–3.71) | <0.001 | 2.37 (1.56–3.60) | <0.001 |
| LVI | 1.44 (1.31–1.57) | <0.001 | 1.33 (1.21–1.46) | <0.001 |
| Positive surgical margins | 1.43 (1.25–1.65) | <0.001 | 1.64 (1.42–1.90) | <0.001 |
| Neoadjuvant chemotherapy | 1.69 (1.36–2.10) | <0.001 | 1.45 (1.15–1.85) | 0.002 |
| Adjuvant chemotherapy | 1.18 (1.06–1.31) | 0.001 | 0.89 (0.80–0.99) | 0.03 |
| Variables | Overall Recurrence | CSM | ||
|---|---|---|---|---|
| HR (CI 95%) | p Value | HR (CI 95%) | p Value | |
| Gender (male vs. female) | 1.09 (0.80–1.48) | 0.6 | 1.23 (0.91–1.67) | 0.1 |
| Age, years | 1.00 (0.99–1.01) | 0.5 | 1.01 (0.99–1.02) | 0.09 |
| RARC approach | 0.76 (0.39–1.47) | 0.4 | 1.34 (0.49–2.36) | 0.8 |
| pT stage | ||||
| pT0-1 | Ref | Ref | Ref | Ref |
| pT2 | 1.21 (0.77–1.90) | 0.3 | 1.34 (0.84–2.15) | 0.2 |
| pT3-4 | 1.57 (1.04–2.37) | 0.03 | 2.17 (1.40–3.35) | <0.001 |
| pN+ | 1.43 (1.05–1.94) | 0.02 | 2.33 (1.71–3.16) | <0.001 |
| Nodes removed | 0.99 (0.98–1.00) | 0.3 | 0.98 (0.97–0.99) | 0.01 |
| High grade vs. low | 3.20 (1.55–6.59) | 0.002 | 3.60 (1.62–7.98) | 0.002 |
| LVI | 1.85 (1.37–2.49) | <0.001 | 1.27 (0.96–1.70) | 0.09 |
| Positive surgical margins | 1.12 (0.74–1.69) | 0.5 | 1.30 (0.84–2.01) | 0.2 |
| Neoadjuvant chemotherapy | 1.96 (1.51–2.54) | <0.001 | 1.34 (1.02–1.76) | 0.03 |
| Adjuvant chemotherapy | 1.29 (0.94–1.77) | 0.1 | 0.77 (0.56–1.06) | 0.1 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Moschini, M.; Zamboni, S.; Soria, F.; Mathieu, R.; Xylinas, E.; Tan, W.S.; Kelly, J.D.; Simone, G.; Meraney, A.; Krishna, S.; et al. Open Versus Robotic Cystectomy: A Propensity Score Matched Analysis Comparing Survival Outcomes. J. Clin. Med. 2019, 8, 1192. https://doi.org/10.3390/jcm8081192
Moschini M, Zamboni S, Soria F, Mathieu R, Xylinas E, Tan WS, Kelly JD, Simone G, Meraney A, Krishna S, et al. Open Versus Robotic Cystectomy: A Propensity Score Matched Analysis Comparing Survival Outcomes. Journal of Clinical Medicine. 2019; 8(8):1192. https://doi.org/10.3390/jcm8081192
Chicago/Turabian StyleMoschini, Marco, Stefania Zamboni, Francesco Soria, Romain Mathieu, Evanguelos Xylinas, Wei Shen Tan, John D Kelly, Giuseppe Simone, Anoop Meraney, Suprita Krishna, and et al. 2019. "Open Versus Robotic Cystectomy: A Propensity Score Matched Analysis Comparing Survival Outcomes" Journal of Clinical Medicine 8, no. 8: 1192. https://doi.org/10.3390/jcm8081192
APA StyleMoschini, M., Zamboni, S., Soria, F., Mathieu, R., Xylinas, E., Tan, W. S., Kelly, J. D., Simone, G., Meraney, A., Krishna, S., Konety, B., Mattei, A., Baumeister, P., Mordasini, L., Montorsi, F., Briganti, A., Gallina, A., Stabile, A., Sanchez-Salas, R., ... Shariat, S. F. (2019). Open Versus Robotic Cystectomy: A Propensity Score Matched Analysis Comparing Survival Outcomes. Journal of Clinical Medicine, 8(8), 1192. https://doi.org/10.3390/jcm8081192







