Incidence and Impact of Acute Kidney Injury in Patients Receiving Extracorporeal Membrane Oxygenation: A Meta-Analysis
Abstract
1. Introduction
2. Methods
2.1. Information Sources and Search Strategy
2.2. Study Selection
2.3. Data Collection Process
2.4. Statistical Analysis
3. Results
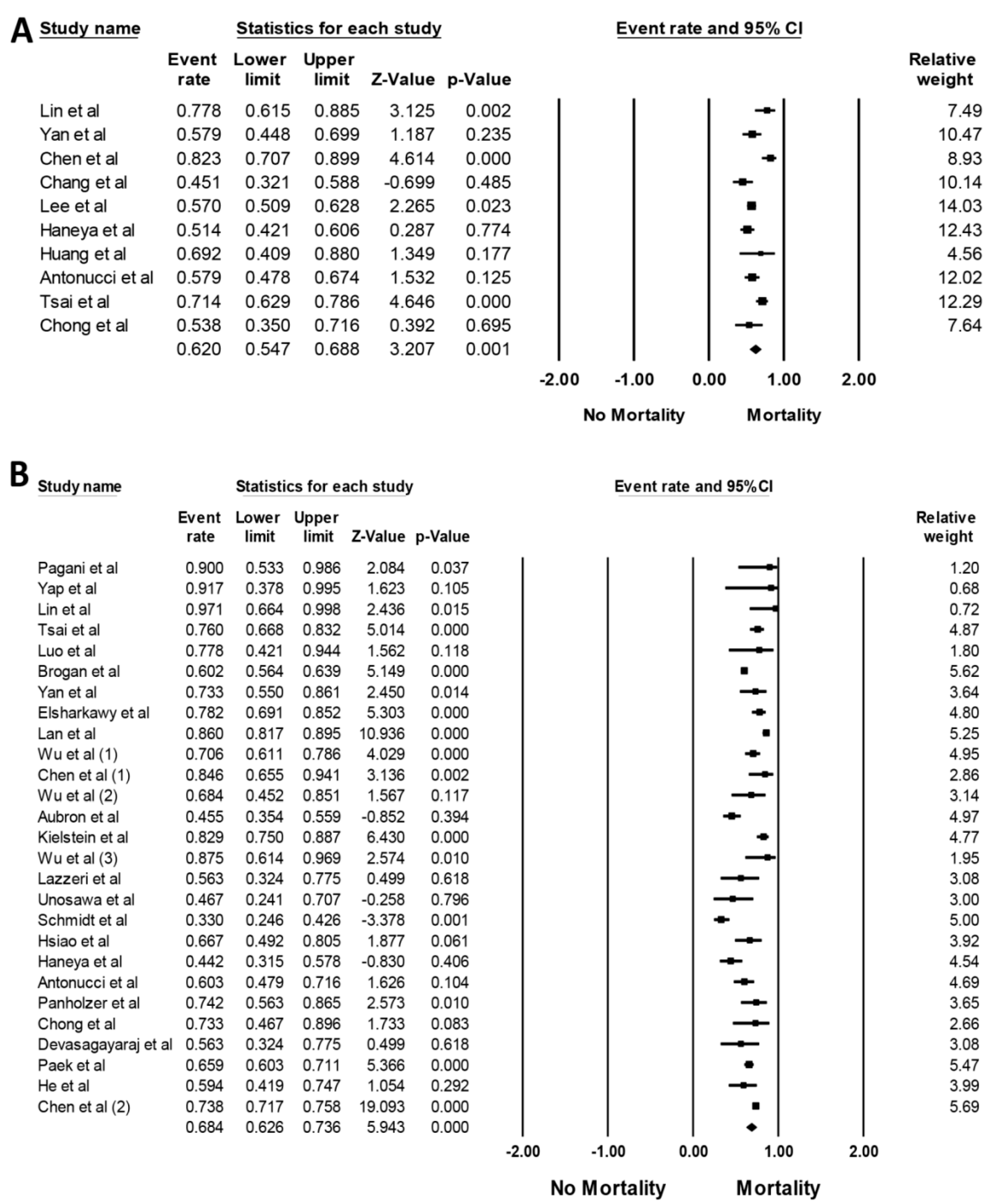
3.1. Incidence of AKI in Patients Requiring ECMO
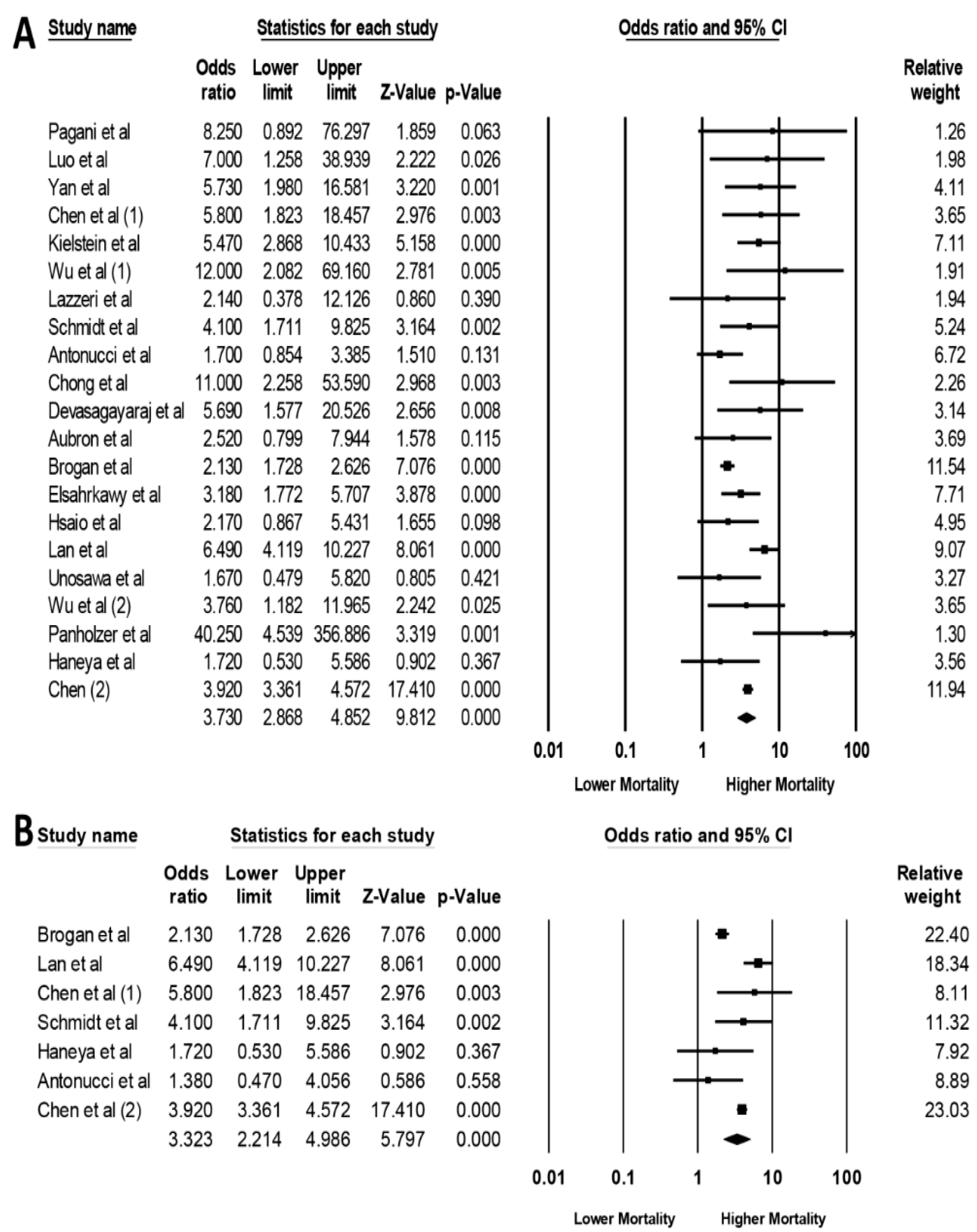
3.2. AKI associated Mortality in Patients Requiring ECMO
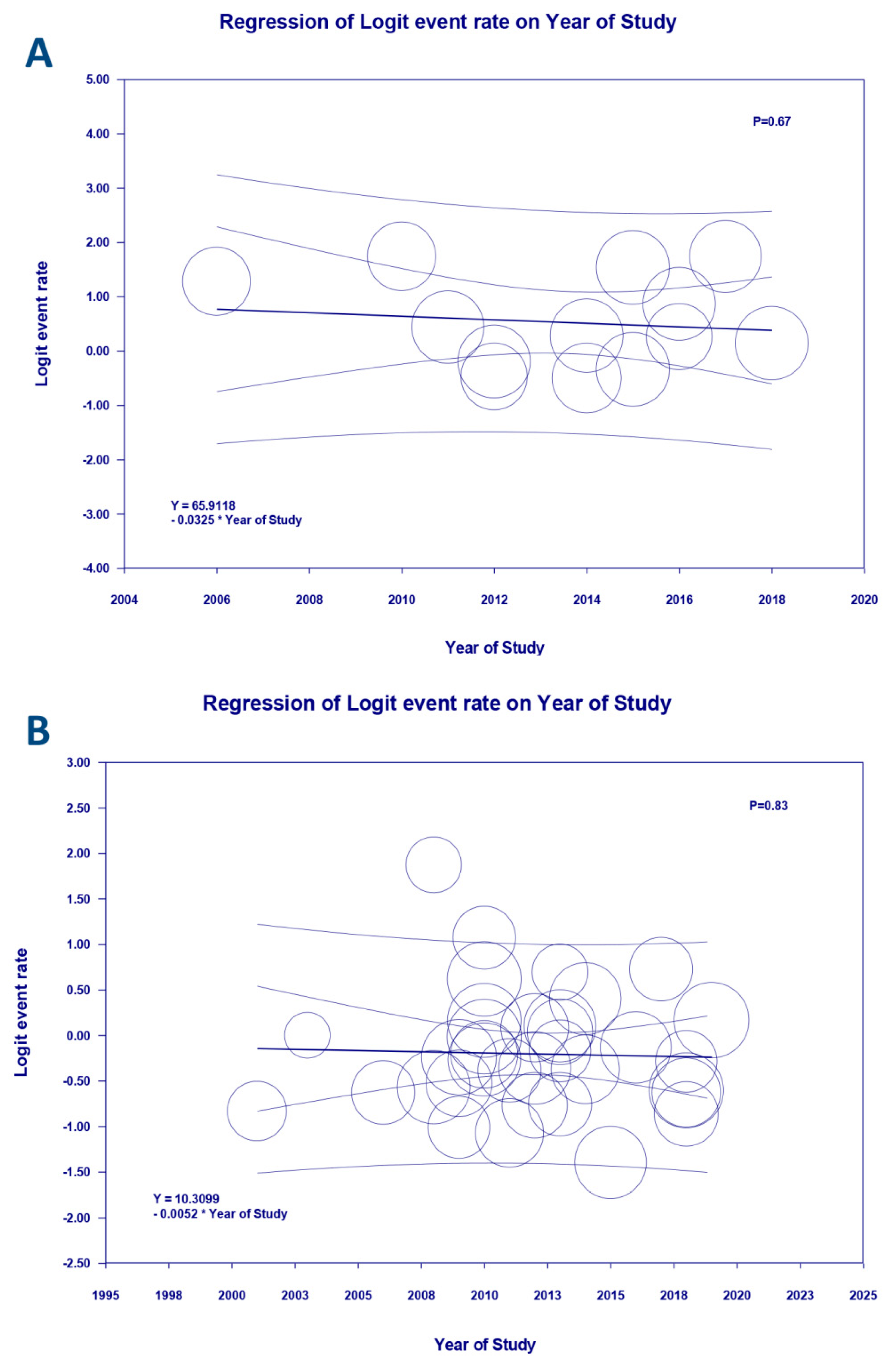
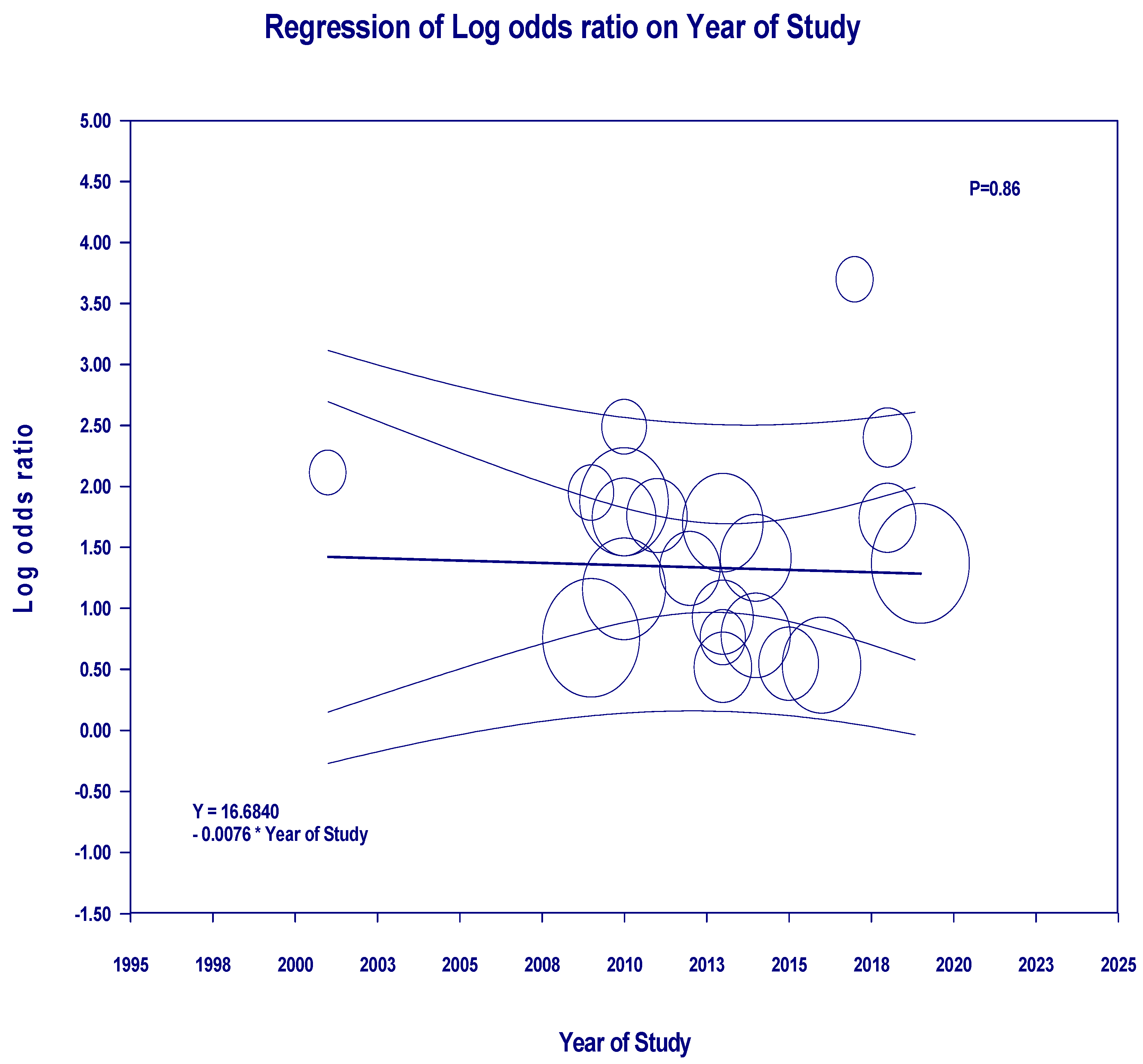
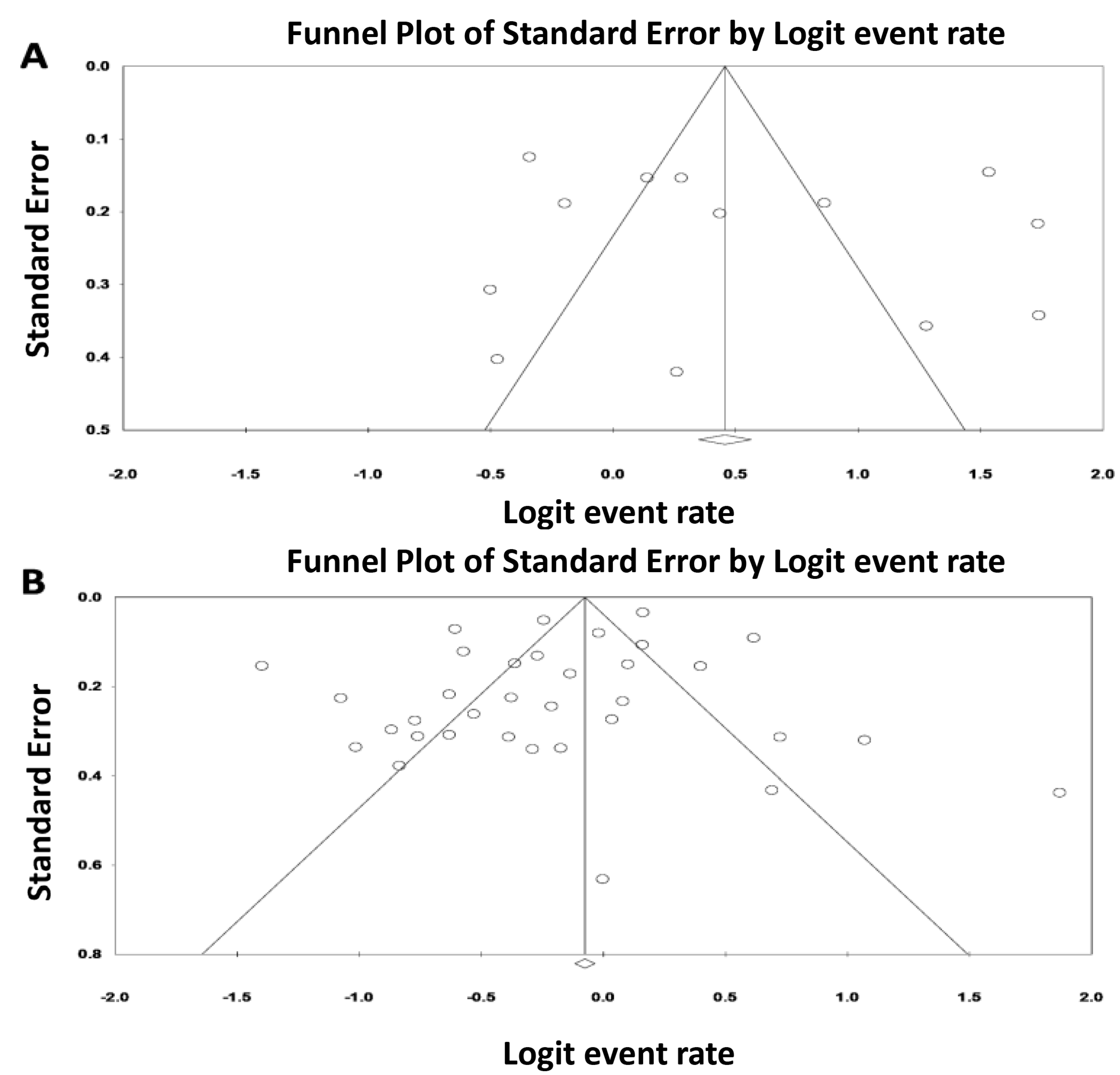
3.3. Evaluation for Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Conflicts of Interest
References
- Guru, P.K.; Singh, T.D.; Passe, M.; Kashani, K.B.; Schears, G.J.; Kashyap, R. Derivation and Validation of a Search Algorithm to Retrospectively Identify CRRT Initiation in the ECMO Patients. Appl. Clin. Inform. 2016, 7, 596–603. [Google Scholar] [CrossRef] [PubMed]
- Hill, J.D.; O’Brien, T.G.; Murray, J.J.; Dontigny, L.; Bramson, M.L.; Osborn, J.J.; Gerbode, F. Prolonged extracorporeal oxygenation for acute post-traumatic respiratory failure (shock-lung syndrome). Use of the Bramson membrane lung. N. Engl. J. Med. 1972, 286, 629–634. [Google Scholar] [CrossRef] [PubMed]
- Peek, G.J.; Mugford, M.; Tiruvoipati, R.; Wilson, A.; Allen, E.; Thalanany, M.M.; Hibbert, C.L.; Truesdale, A.; Clemens, F.; Cooper, N.; et al. Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): A multicentre randomised controlled trial. Lancet 2009, 374, 1351–1363. [Google Scholar] [CrossRef]
- Chen, Y.C.; Tsai, F.C.; Fang, J.T.; Yang, C.W. Acute kidney injury in adults receiving extracorporeal membrane oxygenation. J. Formos. Med. Assoc. 2014, 113, 778–785. [Google Scholar] [CrossRef] [PubMed]
- Thiagarajan, R.R.; Barbaro, R.P.; Rycus, P.T.; Mcmullan, D.M.; Conrad, S.A.; Fortenberry, J.D.; Paden, M.L. Extracorporeal Life Support Organization Registry International Report 2016. ASAIO J. 2017, 63, 60–67. [Google Scholar] [CrossRef] [PubMed]
- Paden, M.L.; Conrad, S.A.; Rycus, P.T.; Thiagarajan, R.R. Extracorporeal Life Support Organization Registry Report 2012. ASAIO J. 2013, 59, 202–210. [Google Scholar] [CrossRef]
- Schmidt, M.; Bailey, M.; Kelly, J.; Hodgson, C.; Cooper, D.J.; Scheinkestel, C.; Pellegrino, V.; Bellomo, R.; Pilcher, D. Impact of fluid balance on outcome of adult patients treated with extracorporeal membrane oxygenation. Intensive Care Med. 2014, 40, 1256–1266. [Google Scholar] [CrossRef]
- Hamdi, T.; Palmer, B.F. Review of Extracorporeal Membrane Oxygenation and Dialysis-Based Liver Support Devices for the Use of Nephrologists. Am. J. Nephrol. 2017, 46, 139–149. [Google Scholar] [CrossRef]
- Husain-Syed, F.; Ricci, Z.; Brodie, D.; Vincent, J.L.; Ranieri, V.M.; Slutsky, A.S.; Taccone, F.S.; Gattinoni, L.; Ronco, C. Extracorporeal organ support (ECOS) in critical illness and acute kidney injury: From native to artificial organ crosstalk. Intensive Care Med. 2018, 44, 1447–1459. [Google Scholar] [CrossRef]
- Bosarge, P.L.; Raff, L.A.; McGwin, G., Jr.; Carroll, S.L.; Bellot, S.C.; Diaz-Guzman, E.; Kerby, J.D. Early initiation of extracorporeal membrane oxygenation improves survival in adult trauma patients with severe adult respiratory distress syndrome. J. Trauma Acute Care Surg. 2016, 81, 236–243. [Google Scholar] [CrossRef]
- Combes, A.; Leprince, P.; Luyt, C.E.; Bonnet, N.; Trouillet, J.L.; Léger, P.; Pavie, A.; Chastre, J. Outcomes and long-term quality-of-life of patients supported by extracorporeal membrane oxygenation for refractory cardiogenic shock. Crit. Care Med. 2008, 36, 1404–1411. [Google Scholar] [CrossRef] [PubMed]
- Massetti, M.; Tasle, M.; Le Page, O.; Deredec, R.; Babatasi, G.; Buklas, D.; Thuaudet, S.; Charbonneau, P.; Hamon, M.; Grollier, G.; et al. Back from irreversibility: Extracorporeal life support for prolonged cardiac arrest. Ann. Thorac. Surg. 2005, 79, 178–183. [Google Scholar] [CrossRef] [PubMed]
- Shin, T.G.; Choi, J.H.; Jo, I.J.; Sim, M.S.; Song, H.G.; Jeong, Y.K.; Song, Y.B.; Hahn, J.Y.; Choi, S.H.; Gwon, H.C.; et al. Extracorporeal cardiopulmonary resuscitation in patients with inhospital cardiac arrest: A comparison with conventional cardiopulmonary resuscitation. Crit. Care Med. 2011, 39, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bednarczyk, J.M.; White, C.W.; Ducas, R.A.; Golian, M.; Nepomuceno, R.; Hiebert, B.; Bueddefeld, D.; Manji, R.A.; Singal, R.K.; Hussain, F.; et al. Resuscitative extracorporeal membrane oxygenation for in hospital cardiac arrest: A Canadian observational experience. Resuscitation 2014, 85, 1713–1719. [Google Scholar] [CrossRef] [PubMed]
- Pagani, F.D.; Aaronson, K.D.; Swaniker, F.; Bartlett, R.H. The use of extracorporeal life support in adult patients with primary cardiac failure as a bridge to implantable left ventricular assist device. Ann. Thorac. Surg. 2001, 71 (Suppl. 3), S77–S81. [Google Scholar] [CrossRef]
- Kagawa, E.; Dote, K.; Kato, M.; Sasaki, S.; Nakano, Y.; Kajikawa, M.; Higashi, A.; Itakura, K.; Sera, A.; Inoue, I.; et al. Should we emergently revascularize occluded coronaries for cardiac arrest?: Rapid-response extracorporeal membrane oxygenation and intra-arrest percutaneous coronary intervention. Circulation 2012, 126, 1605–1613. [Google Scholar] [CrossRef]
- Zangrillo, A.; Landoni, G.; Biondi-Zoccai, G.; Greco, M.; Greco, T.; Frati, G.; Patroniti, N.; Antonelli, M.; Pesenti, A.; Pappalardo, F. A meta-analysis of complications and mortality of extracorporeal membrane oxygenation. Crit. Care Resusc. 2013, 15, 172–178. [Google Scholar]
- Ostermann, M.; Connor, M.; Jr Kashani, K. Continuous renal replacement therapy during extracorporeal membrane oxygenation: Why, when and how? Curr. Opin. Crit. Care 2018, 24, 493–503. [Google Scholar] [CrossRef]
- Kagawa, E.; Inoue, I.; Kawagoe, T.; Ishihara, M.; Shimatani, Y.; Kurisu, S.; Nakama, Y.; Dai, K.; Takayuki, O.; Ikenaga, H.; et al. Assessment of outcomes and differences between in- and out-of-hospital cardiac arrest patients treated with cardiopulmonary resuscitation using extracorporeal life support. Resuscitation 2010, 81, 968–973. [Google Scholar] [CrossRef]
- Hei, F.; Lou, S.; Li, J.; Yu, K.; Liu, J.; Feng, Z.; Zhao, J.; Hu, S.; Xu, J.; Chang, Q.; et al. Five-year results of 121 consecutive patients treated with extracorporeal membrane oxygenation at Fu Wai Hospital. Artif. Organs 2011, 35, 572–578. [Google Scholar] [CrossRef]
- Tsai, T.Y.; Tsai, F.C.; Chang, C.H.; Jenq, C.C.; Hsu, H.H.; Chang, M.Y.; Tian, Y.C.; Hung, C.C.; Fang, J.T.; Yang, C.W.; et al. Prognosis of patients on extracorporeal membrane oxygenation plus continuous arteriovenous hemofiltration. Chang. Gung Med. J. 2011, 34, 636–643. [Google Scholar] [PubMed]
- Belle, L.; Mangin, L.; Bonnet, H.; Fol, S.; Santre, C.; Delavenat, L.; Savary, D.; Bougon, D.; Vialle, E.; Dompnier, A.; et al. Emergency extracorporeal membrane oxygenation in a hospital without on-site cardiac surgical facilities. EuroIntervention 2012, 8, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Slottosch, I.; Liakopoulos, O.; Kuhn, E.; Deppe, A.C.; Scherner, M.; Madershahian, N.; Choi, Y.H.; Wahlers, T. Outcomes after peripheral extracorporeal membrane oxygenation therapy for postcardiotomy cardiogenic shock: A single-center experience. J. Surg. Res. 2013, 181, e47–e55. [Google Scholar] [CrossRef] [PubMed]
- Seco, M.; Forrest, P.; Jackson, S.A.; Martinez, G.; Andvik, S.; Bannon, P.G.; Ng, M.; Fraser, J.F.; Wilson, M.K.; Vallely, M.P. Extracorporeal membrane oxygenation for very high-risk transcatheter aortic valve implantation. Heart Lung Circ. 2014, 23, 957–962. [Google Scholar] [CrossRef] [PubMed]
- Saxena, P.; Neal, J.; Joyce, L.D.; Greason, K.L.; Schaff, H.V.; Guru, P.; Shi, W.Y.; Burkhart, H.; Li, Z.; Oliver, W.C.; et al. Extracorporeal Membrane Oxygenation Support in Postcardiotomy Elderly Patients: The Mayo Clinic Experience. Ann. Thorac. Surg. 2015, 99, 2053–2060. [Google Scholar] [CrossRef] [PubMed]
- Thajudeen, B.; Kamel, M.; Arumugam, C.; Ali, S.A.; John, S.G.; Meister, E.E.; Mosier, J.M.; Raz, Y.; Madhrira, M.; Thompson, J.; et al. Outcome of patients on combined extracorporeal membrane oxygenation and continuous renal replacement therapy: A retrospective study. Int. J. Artif. Organs 2015, 38, 133–137. [Google Scholar] [CrossRef] [PubMed]
- Lyu, L.; Long, C.; Hei, F.; Ji, B.; Liu, J.; Yu, K.; Chen, L.; Yao, J.; Hu, Q.; Hu, J.; et al. Plasma Free Hemoglobin Is a Predictor of Acute Renal Failure During Adult Venous-Arterial Extracorporeal Membrane Oxygenation Support. J. Cardiothorac. Vasc. Anesth. 2016, 30, 891–895. [Google Scholar] [CrossRef]
- Martucci, G.; Panarello, G.; Occhipinti, G. Anticoagulation and Transfusions Management in Veno-Venous Extracorporeal Membrane Oxygenation for Acute Respiratory Distress Syndrome: Assessment of Factors Associated With Transfusion Requirements and Mortality. J. Intensive Care Med. 2017, 34, 630–639. [Google Scholar] [CrossRef]
- Yap, H.J.; Chen, Y.C.; Fang, J.T.; Huang, C.C. Combination of continuous renal replacement therapies (CRRT) and extracorporeal membrane oxygenation (ECMO) for advanced cardiac patients. Ren. Fail. 2003, 25, 183–193. [Google Scholar] [CrossRef]
- Lin, C.Y.; Chen, Y.C.; Tsai, F.C.; Tian, Y.C.; Jenq, C.C.; Fang, J.T.; Yang, C.W. RIFLE classification is predictive of short-term prognosis in critically ill patients with acute renal failure supported by extracorporeal membrane oxygenation. Nephrol. Dial. Transplant. 2006, 21, 2867–2873. [Google Scholar] [CrossRef]
- Tsai, C.W.; Lin, Y.F.; Wu, V.C.; Chu, T.S.; Chen, Y.M.; Hu, F.C.; Wu, K.D.; Ko, W.J. SAPS 3 at dialysis commencement is predictive of hospital mortality in patients supported by extracorporeal membrane oxygenation and acute dialysis. Eur. J. Cardiothorac. Surg. 2008, 34, 1158–1164. [Google Scholar] [CrossRef]
- Bakhtiary, F.; Keller, H.; Dogan, S.; Dzemali, O.; Oezaslan, F.; Meininger, D.; Ackermann, H.; Zwissler, B.; Kleine, P.; Moritz, A. Venoarterial extracorporeal membrane oxygenation for treatment of cardiogenic shock: Clinical experiences in 45 adult patients. J. Thorac. Cardiovasc. Surg. 2008, 135, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Luo, X.J.; Wang, W.; Hu, S.S.; Sun, H.S.; Gao, H.W.; Long, C.; Song, Y.H.; Xu, J.P. Extracorporeal membrane oxygenation for treatment of cardiac failure in adult patients. Interact. Cardiovasc. Thorac. Surg. 2009, 9, 296–300. [Google Scholar] [CrossRef] [PubMed]
- Brogan, T.V.; Thiagarajan, R.R.; Rycus, P.T.; Bartlett, R.H.; Bratton, S.L. Extracorporeal membrane oxygenation in adults with severe respiratory failure: A multi-center database. Intensive Care Med. 2009, 35, 2105–2114. [Google Scholar] [CrossRef]
- Wang, J.; Han, J.; Jia, Y.; Zeng, W.; Shi, J.; Hou, X.; Meng, X. Early and intermediate results of rescue extracorporeal membrane oxygenation in adult cardiogenic shock. Ann. Thorac. Surg. 2009, 88, 1897–1903. [Google Scholar] [CrossRef] [PubMed]
- Yan, X.; Jia, S.; Meng, X.; Dong, P.; Jia, M.; Wan, J.; Hou, X. Acute kidney injury in adult postcardiotomy patients with extracorporeal membrane oxygenation: Evaluation of the RIFLE classification and the Acute Kidney Injury Network criteria. Eur. J. Cardiothorac. Surg. 2010, 37, 334–338. [Google Scholar] [CrossRef]
- Elsharkawy, H.A.; Li, L.; Esa, W.A.; Sessler, D.I.; Bashour, C.A. Outcome in patients who require venoarterial extracorporeal membrane oxygenation support after cardiac surgery. J. Cardiothorac. Vasc. Anesth. 2010, 24, 946–951. [Google Scholar] [CrossRef]
- Hsu, P.S.; Chen, J.L.; Hong, G.J.; Tsai, Y.T.; Lin, C.Y.; Lee, C.Y.; Chen, Y.G.; Tsai, C.S. Extracorporeal membrane oxygenation for refractory cardiogenic shock after cardiac surgery: Predictors of early mortality and outcome from 51 adult patients. Eur. J. Cardiothorac. Surg. 2010, 37, 328–333. [Google Scholar] [CrossRef]
- Lan, C.; Tsai, P.R.; Chen, Y.S.; Ko, W.J. Prognostic factors for adult patients receiving extracorporeal membrane oxygenation as mechanical circulatory support—A 14-year experience at a medical center. Artif. Organs 2010, 34, E59–E64. [Google Scholar] [CrossRef]
- Rastan, A.J.; Dege, A.; Mohr, M.; Doll, N.; Falk, V.; Walther, T.; Mohr, F.W. Early and late outcomes of 517 consecutive adult patients treated with extracorporeal membrane oxygenation for refractory postcardiotomy cardiogenic shock. J. Thorac. Cardiovasc. Surg. 2010, 139, 302–311. [Google Scholar] [CrossRef]
- Wu, V.C.; Tsai, H.B.; Yeh, Y.C.; Huang, T.M.; Lin, Y.F.; Chou, N.K.; Chen, Y.S.; Han, Y.Y.; Chou, A.; Lin, Y.H.; et al. Patients supported by extracorporeal membrane oxygenation and acute dialysis: Acute physiology and chronic health evaluation score in predicting hospital mortality. Artif. Organs 2010, 34, 828–835. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.C.; Tsai, F.C.; Chang, C.H.; Lin, C.Y.; Jenq, C.C.; Juan, K.C.; Hsu, H.H.; Chang, M.Y.; Tian, Y.C.; Hung, C.C.; et al. Prognosis of patients on extracorporeal membrane oxygenation: The impact of acute kidney injury on mortality. Ann. Thorac. Surg. 2011, 91, 137–142. [Google Scholar] [CrossRef] [PubMed]
- Bermudez, C.A.; Rocha, R.V.; Toyoda, Y.; Zaldonis, D.; Sappington, P.L.; Mulukutla, S.; Marroquin, O.C.; Toma, C.; Bhama, J.K.; Kormos, R.L. Extracorporeal membrane oxygenation for advanced refractory shock in acute and chronic cardiomyopathy. Ann. Thorac. Surg. 2011, 92, 2125–2131. [Google Scholar] [CrossRef] [PubMed]
- Chang, W.W.; Tsai, F.C.; Tsai, T.Y.; Chang, C.H.; Jenq, C.C.; Chang, M.Y.; Tian, Y.C.; Hung, C.C.; Fang, J.T.; Yang, C.W.; et al. Predictors of mortality in patients successfully weaned from extracorporeal membrane oxygenation. PLoS ONE 2012, 7, e42687. [Google Scholar] [CrossRef] [PubMed]
- Kim, T.H.; Lim, C.; Park, I.; Kim, D.J.; Jung, Y.; Park, K.H. Prognosis in the patients with prolonged extracorporeal membrane oxygenation. Korea J. Thorac. Cardiovasc. Surg. 2012, 45, 236–241. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; Chung, C.H.; Won Lee, J.; Ho Jung, S.; Choo, S.J. Factors predicting early- and long-term survival in patients undergoing extracorporeal membrane oxygenation (ECMO). J. Card. Surg. 2012, 27, 255–263. [Google Scholar] [CrossRef] [PubMed]
- Loforte, A.; Montalto, A.; Ranocchi, F.; Della Monica, P.L.; Casali, G.; Lappa, A.; Menichetti, A.; Contento, C.; Musumeci, F. Peripheral extracorporeal membrane oxygenation system as salvage treatment of patients with refractory cardiogenic shock: Preliminary outcome evaluation. Artif. Organs 2012, 36, E53–E61. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.Y.; Lee, M.Y.; Lin, C.C.; Chang, Y.S.; Tsai, F.C.; Lin, P.J. Resuscitation of non-postcardiotomy cardiogenic shock or cardiac arrest with extracorporeal life support: The role of bridging to intervention. Resuscitation 2012, 83, 976–981. [Google Scholar] [CrossRef]
- Aubron, C.; Cheng, A.C.; Pilcher, D.; Leong, T.; Magrin, G.; Cooper, D.J.; Scheinkestel, C.; Pellegrino, V. Factors associated with outcomes of patients on extracorporeal membrane oxygenation support: A 5-year cohort study. Crit. Care 2013, 17, R73. [Google Scholar] [CrossRef]
- Kielstein, J.T.; Heiden, A.M.; Beutel, G.; Gottlieb, J.; Wiesner, O.; Hafer, C.; Hadem, J.; Reising, A.; Haverich, A.; Kühn, C.; et al. Renal function and survival in 200 patients undergoing ECMO therapy. Nephrol. Dial. Transplant. 2013, 28, 86–90. [Google Scholar] [CrossRef]
- Wu, M.Y.; Tseng, Y.H.; Chang, Y.S.; Tsai, F.C.; Lin, P.J. Using extracorporeal membrane oxygenation to rescue acute myocardial infarction with cardiopulmonary collapse: The impact of early coronary revascularization. Resuscitation 2013, 84, 940–945. [Google Scholar] [CrossRef] [PubMed]
- Lazzeri, C.; Bernardo, P.; Sori, A.; Innocenti, L.; Passantino, S.; Chiostri, M.; Gensini, G.F.; Valente, S. Renal replacement therapy in patients with refractory cardiac arrest undergoing extracorporeal membrane oxygenation. Resuscitation 2013, 84, e121–e122. [Google Scholar] [CrossRef] [PubMed]
- Unosawa, S.; Sezai, A.; Hata, M.; Nakata, K.; Yoshitake, I.; Wakui, S.; Kimura, H.; Takahashi, K.; Hata, H.; Shiono, M. Long-term outcomes of patients undergoing extracorporeal membrane oxygenation for refractory postcardiotomy cardiogenic shock. Surg. Today 2013, 43, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Xue, J.; Wang, L.; Chen, C.M.; Chen, J.Y.; Sun, Z.X. Acute kidney injury influences mortality in lung transplantation. Ren. Fail. 2014, 36, 541–545. [Google Scholar] [CrossRef] [PubMed]
- Hsiao, C.C.; Chang, C.H.; Fan, P.C.; Ho, H.T.; Jenq, C.C.; Kao, K.C.; Chiu, L.C.; Lee, S.Y.; Hsu, H.H.; Tian, Y.C.; et al. Prognosis of patients with acute respiratory distress syndrome on extracorporeal membrane oxygenation: The impact of urine output on mortality. Ann. Thorac. Surg. 2014, 97, 1939–1944. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.W.; Yu, M.Y.; Lee, H.; Ahn, S.Y.; Kim, S.; Chin, H.J.; Na, K.Y. Risk Factors for Acute Kidney Injury and In-Hospital Mortality in Patients Receiving Extracorporeal Membrane Oxygenation. PLoS ONE 2015, 10, e0140674. [Google Scholar] [CrossRef] [PubMed]
- Haneya, A.; Diez, C.; Philipp, A.; Bein, T.; Mueller, T.; Schmid, C.; Lubnow, M. Impact of Acute Kidney Injury on Outcome in Patients With Severe Acute Respiratory Failure Receiving Extracorporeal Membrane Oxygenation. Crit. Care Med. 2015, 43, 1898–1906. [Google Scholar] [CrossRef]
- Huang, L.; Li, T.; Xu, L.; Hu, X.M.; Duan, D.W.; Li, Z.B.; Gao, X.J.; Li, J.; Wu, P.; Liu, Y.W. Extracorporeal Membrane Oxygenation Outcomes in Acute Respiratory Distress Treatment: Case Study in a Chinese Referral Center. Med. Sci. Monit. 2017, 23, 741–750. [Google Scholar] [CrossRef][Green Version]
- Antonucci, E.; Lamanna, I.; Fagnoul, D.; Vincent, J.L.; De Backer, D.; Silvio Taccone, F. The Impact of Renal Failure and Renal Replacement Therapy on Outcome During Extracorporeal Membrane Oxygenation Therapy. Artif. Organs 2016, 40, 746–754. [Google Scholar] [CrossRef]
- Tsai, T.Y.; Chien, H.; Tsai, F.C.; Pan, H.C.; Yang, H.Y.; Lee, S.Y.; Hsu, H.H.; Fang, J.T.; Yang, C.W.; Chen, Y.C. Comparison of, R.I.F.L.E.; AKIN, and KDIGO classifications for assessing prognosis of patients on extracorporeal membrane oxygenation. J. Formos. Med. Assoc. 2017, 116, 844–851. [Google Scholar] [CrossRef]
- Panholzer, B.; Meckelburg, K.; Huenges, K.; Hoffmann, G.; von der Brelie, M.; Haake, N.; Pilarczyk, K.; Cremer, J.; Haneya, A. Extracorporeal membrane oxygenation for acute respiratory distress syndrome in adults: An analysis of differences between survivors and non-survivors. Perfusion 2017, 32, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Chong, S.Z.; Fang, C.Y.; Fang, H.Y.; Chen, H.C.; Chen, C.J.; Yang, C.H.; Hang, C.L.; Yip, H.K.; Wu, C.J.; Lee, W.C. Associations with the In-Hospital Survival Following Extracorporeal Membrane Oxygenation in Adult Acute Fulminant Myocarditis. J. Clin. Med. 2018, 7, 452. [Google Scholar] [CrossRef] [PubMed]
- Devasagayaraj, R.; Cavarocchi, N.C.; Hirose, H. Does acute kidney injury affect survival in adults with acute respiratory distress syndrome requiring extracorporeal membrane oxygenation? Perfusion 2018, 33, 375–382. [Google Scholar] [CrossRef] [PubMed]
- Liao, X.; Cheng, Z.; Wang, L.; Li, B. Analysis of the risk factors of acute kidney injury in patients receiving extracorporeal membrane oxygenation. Clin. Nephrol. 2018, 90, 270–275. [Google Scholar] [CrossRef] [PubMed]
- Paek, J.H.; Park, S.; Lee, A.; Park, S.; Chin, H.J.; Na, K.Y.; Lee, H.; Park, J.T.; Kim, S. Timing for initiation of sequential continuous renal replacement therapy in patients on extracorporeal membrane oxygenation. Kidney Res. Clin. Pract. 2018, 37, 239–247. [Google Scholar] [CrossRef]
- He, P.; Zhang, S.; Hu, B.; Wu, W. Retrospective study on the effects of the prognosis of patients treated with extracorporeal membrane oxygenation combined with continuous renal replacement therapy. Ann. Transl. Med. 2018, 6, 455. [Google Scholar] [CrossRef] [PubMed]
- Zhang, H.; Wu, J.; Zou, D.; Xiao, X.; Yan, H.; Li, X.C.; Chen, W. Ablation of interferon regulatory factor 4 in T cells induces “memory” of transplant tolerance that is irreversible by immune checkpoint blockade. Am. J. Transplant. 2019, 19, 884–893. [Google Scholar] [CrossRef]
- Kilburn, D.J.; Shekar, K.; Fraser, J.F. The Complex Relationship of Extracorporeal Membrane Oxygenation and Acute Kidney Injury: Causation or Association? BioMed Res. Int. 2016, 2016, 1094296. [Google Scholar] [CrossRef]
- Cheng, R.; Hachamovitch, R.; Kittleson, M.; Patel, J.; Arabia, F.; Moriguchi, J.; Esmailian, F.; Azarbal, B. Complications of extracorporeal membrane oxygenation for treatment of cardiogenic shock and cardiac arrest: A meta-analysis of 1,866 adult patients. Ann. Thorac.Surg. 2014, 97, 610–616. [Google Scholar] [CrossRef]
- Lin, C.Y.; Tsai, F.C.; Tian, Y.C.; Jenq, C.C.; Chen, Y.C.; Fang, J.T.; Yang, C.W. Evaluation of outcome scoring systems for patients on extracorporeal membrane oxygenation. Ann. Thorac. Surg. 2007, 84, 1256–1262. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff JAltman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Bellomo, R.; Ronco, C.; Kellum, J.A.; Mehta, R.L. Palevsky PAcute renal failure—Definition outcome measures animal, m.o.d.e.l.s., fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit. Care 2004, 8, R204–R212. [Google Scholar] [CrossRef] [PubMed]
- Mehta, R.L.; Kellum, J.A.; Shah, S.V.; Molitoris, B.A.; Ronco, C.; Warnock, D.G.; Levin, A. Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit. Care 2007, 11, R31. [Google Scholar] [CrossRef] [PubMed]
- Section 2: AKI Definition. Kidney Int. 2012, 2, 19–36. [CrossRef] [PubMed]
- DerSimonian, R.; Laird, N. Meta-analysis in clinical trials. Control. Clin. Trials 1986, 7, 177–188. [Google Scholar] [CrossRef]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [PubMed]
- Easterbrook, P.J.; Gopalan, R.; Berlin, J.A.; Matthews, D.R. Publication bias in clinical research. Lancet 1991, 337, 867–872. [Google Scholar] [CrossRef]
- McDonald, C.I.; Fraser, J.F.; Coombes, J.S.; Fung, Y.L. Oxidative stress during extracorporeal circulation. Eur. J. Cardiothorac. Surg. 2014, 46, 937–943. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, M.; Prachasilchai, W.; Burne-Taney, M.J.; Rabb, H.; Yokota-Ikeda, N. Ischemic acute tubular necrosis models and drug discovery: A focus on cellular inflammation. Drug Discov. Today 2006, 11, 364–370. [Google Scholar] [CrossRef] [PubMed]
- Yimin, H.; Wenkui, Y.; Jialiang, S.; Qiyi, C.; Juanhong, S.; Zhiliang, L.; Changsheng, H.; Ning, L.; Jieshou, L. Effects of continuous renal replacement therapy on renal inflammatory cytokines during extracorporeal membrane oxygenation in a porcine model. J. Cardiothorac. Surg. 2013, 8, 113. [Google Scholar] [CrossRef] [PubMed]
- McILwain, R.B.; Timpa, J.G.; Kurundkar, A.R.; Holt, D.W.; Kelly, D.R.; Hartman, Y.E.; Neel, M.L.; Karnatak, R.K.; Schelonka, R.L.; Anantharamaiah, G.M.; et al. Plasma concentrations of inflammatory cytokines rise rapidly during ECMO-related SIRS due to the release of preformed stores in the intestine. Lab. Investig. 2010, 90, 128–139. [Google Scholar] [CrossRef] [PubMed]
- Reed, R.C.; Rutledge, J.C. Laboratory and clinical predictors of thrombosis and hemorrhage in 29 pediatric extracorporeal membrane oxygenation nonsurvivors. Pediatr. Dev. Pathol. 2010, 13, 385–392. [Google Scholar] [CrossRef] [PubMed]
- Williams, D.C.; Turi, J.L.; Hornik, C.P.; Bonnadonna, D.K.; Williford, W.L.; Walczak, R.J.; Watt, K.M.; Cheifetz, I.M. Circuit oxygenator contributes to extracorporeal membrane oxygenation-induced hemolysis. ASAIO J. 2015, 61, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Askenazi, D.J.; Selewski, D.T.; Paden, M.L.; Cooper, D.S.; Bridges, B.C.; Zappitelli, M.; Fleming, G.M. Renal replacement therapy in critically ill patients receiving extracorporeal membrane oxygenation. Clin. J. Am. Soc. Nephrol. 2012, 7, 1328–1336. [Google Scholar] [CrossRef] [PubMed]
- Lubnow, M.; Philipp, A.; Foltan, M.; Enger, T.B.; Lunz, D.; Bein, T.; Haneya, A.; Schmid, C.; Riegger, G.; Müller, T.; et al. Technical complications during veno-venous extracorporeal membrane oxygenation and their relevance predicting a system-exchange—Retrospective analysis of 265 cases. PLoS ONE 2014, 9, e112316. [Google Scholar] [CrossRef] [PubMed]
- Murphy, D.A.; Hockings, L.E.; Andrews, R.K.; Aubron, C.; Gardiner, E.E.; Pellegrino, V.A.; Davis, A.K. Extracorporeal membrane oxygenation-hemostatic complications. Transfus. Med. Rev. 2015, 29, 90–101. [Google Scholar] [CrossRef]
- Lehle, K.; Philipp, A.; Zeman, F.; Lunz, D.; Lubnow, M.; Wendel, H.P.; Göbölös, L.; Schmid, C.; Müller, T. Technical-Induced Hemolysis in Patients with Respiratory Failure Supported with Veno-Venous ECMO—Prevalence and Risk Factors. PLoS ONE 2015, 10, e0143527. [Google Scholar] [CrossRef] [PubMed]
- Adademir, T.; Ak, K.; Aljodi, M.; Elçi, M.E.; Arsan, S.; Isbir, S. The effects of pulsatile cardiopulmonary bypass on acute kidney injury. Int. J. Artif. Organs 2012, 35, 511–519. [Google Scholar] [CrossRef]
- Abu-Omar, Y.; Ratnatunga, C. Cardiopulmonary bypass and renal injury. Perfusion 2006, 21, 209–213. [Google Scholar] [CrossRef]
- Santana-Santos, E.; Marcusso, M.E.; Rodrigues, A.O.; Queiroz, F.G.; Oliveira, L.B.; Rodrigues, A.R.; Palomo, J.D. Strategies for prevention of acute kidney injury in cardiac surgery: An integrative review. Revista Brasileira Terpia Intensiva 2014, 26, 183–192. [Google Scholar] [CrossRef]
- Thongprayoon, C.; Kaewput, W.; Thamcharoen, N.; Bathini, T.; Watthanasuntorn, K.; Lertjitbanjong, P.; Sharma, K.; Salim, S.A.; Ungprasert, P.; Wijarnpreecha, K.; et al. Incidence and Impact of Acute Kidney Injury after Liver Transplantation: A Meta-Analysis. J. Clin. Med. 2019, 8, 372. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Kaewput, W.; Thamcharoen, N.; Bathini, T.; Watthanasuntorn, K.; Salim, S.A.; Ungprasert, P.; Lertjitbanjong, P.; Aeddula, N.R.; Torres-Ortiz, A.; et al. Acute Kidney Injury in Patients Undergoing Total Hip Arthroplasty: A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 66. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Mao, M.A.; Harrison, A.M.; Erickson, S.B. Elevated admission serum calcium phosphate product as an independent risk factor for acute kidney injury in hospitalized patients. Hosp. Pract. (1995) 2019, 47, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Mao, M.A.; Sakhuja, A.; Kashani, K. U-shape association of serum albumin level and acute kidney injury risk in hospitalized patients. PLoS ONE 2018, 13, e0199153. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Mao, M.A.; Sakhuja, A.; Erickson, S.B. Admission calcium levels and risk of acute kidney injury in hospitalised patients. Int. J. Clin. Pract. 2018, 72, e13057. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Mao, M.A.; Sakhuja, A.; Erickson, S.B. Admission hyperphosphatemia increases the risk of acute kidney injury in hospitalized patients. J. Nephrol. 2018, 31, 241–247. [Google Scholar] [CrossRef] [PubMed]
- Razo-Vazquez, A.O.; Thornton, K. Extracorporeal Membrane Oxygenation-What the Nephrologist Needs to Know. Adv. Chronic Kidney Dis. 2016, 23, 146–151. [Google Scholar] [CrossRef]
- Pedersen, T.H.; Videm, V.; Svennevig, J.L.; Karlsen, H.; Østbakk, R.W.; Jensen, Ø.; Mollnes, T.E. Extracorporeal membrane oxygenation using a centrifugal pump and a servo regulator to prevent negative inlet pressure. Ann. Thorac. Surg. 1997, 63, 1333–1339. [Google Scholar] [CrossRef]
- Kress, D.C.; Cohen, D.J.; Swanson, D.K.; Hegge, J.O.; Young, J.W.; Watson, K.M.; Rasmussen, P.W.; Berkoff, H.A. Pump-induced hemolysis in a rabbit model of neonatal ECMO. ASAIO Trans. 1987, 33, 446–452. [Google Scholar]
- Lou, S.; MacLaren, G.; Best, D.; Delzoppo, C.; Butt, W. Hemolysis in pediatric patients receiving centrifugal-pump extracorporeal membrane oxygenation: Prevalence, risk factors, and outcomes. Crit. Care Med. 2014, 42, 1213–1220. [Google Scholar] [CrossRef]
- Toomasian, J.M.; Bartlett, R.H. Hemolysis and ECMO pumps in the 21st Century. Perfusion 2011, 26, 5–6. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Kittanamongkolchai, W.; Harrison, A.M.; Kashani, K. Prognostic Importance of Low Admission Serum Creatinine Concentration for Mortality in Hospitalized Patients. Am. J. Med. 2017, 130, 545–554. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Kashani, K. Serum creatinine level, a surrogate of muscle mass, predicts mortality in critically ill patients. J. Thorac. Dis. 2016, 8, E305–E311. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Cheungpasitporn, W.; Kittanamongkolchai, W.; Srivali, N.; Ungprasert, P.; Kashani, K. Optimum methodology for estimating baseline serum creatinine for the acute kidney injury classification. Nephrology (Carlton) 2015, 20, 881–886. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, V.S.; Ramirez, V.; Ichimura, T.; Bobadilla, N.A.; Bonventre, J.V. Urinary kidney injury molecule-1: A sensitive quantitative biomarker for early detection of kidney tubular injury. Am. J. Physiol. Renal Physiol. 2006, 290, F517–F529. [Google Scholar] [CrossRef]
- Mishra, J.; Ma, Q.; Prada, A.; Mitsnefes, M.; Zahedi, K.; Yang, J.; Barasch, J.; Devarajan, P. Identification of neutrophil gelatinase-associated lipocalin as a novel early urinary biomarker for ischemic renal injury. J. Am. Soc. Nephrol. 2003, 14, 2534–2543. [Google Scholar] [CrossRef]
- Hosohata, K.; Ando, H.; Fujimura, A. Urinary vanin-1 as a novel biomarker for early detection of drug-induced acute kidney injury. J. Pharmacol. Exp. Ther. 2012, 341, 656–662. [Google Scholar] [CrossRef]
- Kashani, K.; Cheungpasitporn, W.; Ronco, C. Biomarkers of acute kidney injury: The pathway from discovery to clinical adoption. Clin. Chem. Lab. Med. 2017, 55, 1074–1089. [Google Scholar] [CrossRef]


| Study | Year | Country | Patients | Number | AKI Definition | AKI Incidence | Mortality |
|---|---|---|---|---|---|---|---|
| Pagani et al. [15] | 2001 | USA | ECMO for cardiogenic shock or arrest | 33 | RRT | RRT 10/33 (30.3%) | Hospital mortality 9/10 (90%) |
| Yap et al. [29] | 2003 | Taiwan | ECMO for cardiogenic shock | 10 | RRT | RRT 5/10 (50%) | Mortality 5/5 (100%) |
| Lin et al. [30] | 2006 | Taiwan | ECMO | 46 | AKI; RIFLE criteria | AKI 36/46 (78.3%) CRRT 16/46 (34.8%) | AKI: Hospital mortality 28/36 (78%) CRRT: Hospital mortality 16/16 (100%) |
| Tsai et al. [31] | 2008 | Taiwan | ECMO | 288 | CRRT | CRRT 104/288 (36.1%) | Hospital mortality 79/104 (76%) |
| Bakhtiary et al. [32] | 2008 | Germany | VA-ECMO for refractory cardiogenic shock | 45 | CRRT | CRRT 39/45 (86.7%) | N/A |
| Luo et al. [33] | 2009 | China | VA-ECMO in severe heart failure | 45 | CRRT | CRRT 12/45 (26.6%) | Hospital mortality 7/9 (78%) |
| Brogan et al. [34] | 2009 | USA | ECMO in severe respiratory failure | 1473 | RRT | RRT 648/1473 (44%) | Hospital mortality RRT 390/648 (60%) |
| Wang et al. [35] | 2009 | China | VA ECMO for refractory cardiogenic shock after cardiac surgery | 62 | CRRT | CRRT 23/62 (37.0%) | N/A |
| Yan et al. [36] | 2010 | China | ECMO after cardiac surgery | 67 | AKI; RIFLE and AKIN criteria | RIFLE AKI 54/67 (80.6%) AKIN AKI 57/67 (85.1%) RRT 30/67 (44.8%) | Hospital mortality RIFLE AKI 32/54 (59%) AKIN AKI 33/57 (58%) RRT 22/30 (73%) |
| Elsharkawy et al. [37] | 2010 | USA | VA-ECMO after cardiac surgery | 233 | RRT | RRT 101/233 (43.3%) | Hospital mortality 79/101 (78%) |
| Hsu et al. [38] | 2010 | Taiwan | VA-ECMO for cardiogenic shock after cardiac surgery | 51 | CRRT | CRRT 38/51 (74.5%) | N/A |
| Lan et al. [39] | 2010 | Taiwan | ECMO | 607 | RRT | RRT 301/607 (49.6%) | Hospital mortality 259/301 (86%) |
| Rastan et al. [40] | 2010 | Germany | VA-ECMO for cardiogenic shock after cardiac surgery | 517 | RRT | RRT 336/517 (65.0%) | N/A |
| Wu et al. [41] | 2010 | Taiwan | ECMO | 346 | RRT | RRT 187/346 (54%) | RRT 72/102 (71%) |
| Chen et al. [42] | 2011 | Taiwan | ECMO | 102 | AKI; AKIN criteria | AKI 62/102 (60.8%) CRRT 26/102 (25.5%) | Hospital mortality AKI 51/62 (82%) CRRT 22/26 (85%) |
| Bermudez et al. [43] | 2011 | USA | ECMO for refractory cardiogenic shock; VA (88%) | 42 | RRT | RRT 17/42 (40.5%) | N/A |
| Chang et al. [44] | 2012 | Taiwan | Successfully weaned from ECMO | 113 | AKI; AKIN criteria at 48 h post-ECMO removal | AKI 51/113 (45.1%) | Hospital mortality AKI 23/51 (45%) |
| Kim et al. [45] | 2012 | Korea | ECMO; VA-ECMO (85%), VV-ECMO (15%) | 26 | AKI; AKIN criteria | AKI 10/26 (38.5%) | N/A |
| Lee et al. [46] | 2012 | Korea | ECMO; VA-ECMO (74%), VV-ECMO (26%) | 185 | CRRT | CRRT 76/185 (41.1%) | N/A |
| Loforte et al. [47] | 2012 | Italy | VA-ECMO | 73 | CRRT | CRRT 38/73 (52.1%) | N/A |
| Wu et al. [48] | 2012 | Taiwan | ECMO for non-post cardiotomy cardiogenic shock or cardiac arrest | 60 | RRT | RRT 19/60 (31.7%) | Hospital mortality 13/19 (68%) |
| Aubron et al. [49] | 2013 | Australia | ECMO; VA-ECMO (67%), VV-ECMO (33%) | 158 | RRT | VA-ECMO RRT 61/105 (58.1%) VV-ECMO RRT 27/53 (50.9%) | Hospital mortality VA-ECMO RRT 27/61 (44%) VV-ECMO RRT 13/27 (48%) |
| Kielstein et al. [50] | 2013 | Germany | ECMO; VA-ECMO (45%), VV-ECMO (55%) | 200 | RRT | RRT 117/200 (58.5%) RRT after ECMO 92/175 (52.6%) | 90-day mortality 97/117 (83%) |
| Wu et al. [51] | 2013 | Taiwan | ECMO for acute myocardial infarction-induced cardiac arrest | 35 | RRT | RRT 16/35 (45.7%) | Hospital mortality 14/16 (88%) |
| Lazzeri et al. [52] | 2013 | Italy | ECMO for refractory cardiac arrest | 25 | RRT | RRT 16/24 (66.7%) | Mortality 9/16 (56%) |
| Unosawa et al. [53] | 2013 | Japan | VA-ECMO for refractory cardiogenic shock after cardiac surgery | 47 | RRT | RRT 15/47 (31.9%) | Mortality on ECMO 7/15 (46.7%) |
| Xue et al. [54] | 2014 | China | ECMO in lung transplantation | 45 | AKI; AKIN criteria | AKI 17/45 (37.8%) | N/A |
| Schmidt et al. [7] | 2014 | Australia | ECMO for refractory cardiogenic shock or acute respiratory failure | 172 | AKI; RIFLE criteria | AKI at ECMO day 1 98/172 (57.0%) CRRT during ECMO 103/172 (59.9%) | 90-day mortality CRRT 34/103 (33%) |
| Hsiao et al. [55] | 2014 | Taiwan | ECMO for ARDS | 81 | CRRT | CRRT 33/81 (40.7%) | Hospital mortality CRRT 22/33 (67%) |
| Lee et al. [56] | 2015 | Korea | ECMO; VA-ECMO (71%), VV-ECMO (29%) | 322 | AKI; KDIGO criteria | AKI 265/322 (82.3%) | Hospital mortality 151/265 (57%) |
| Haneya [57] | 2015 | Germany | VV-ECMO for ARDS | 262 | AKI; KDIGO criteria | AKI 109/262 (41.6%) RRT during ECMO 52/262 (19.8%) | Mortality AKI 56/109 (51%) RRT during ECMO 23/52 (44%) |
| Huang et al. [58] | 2016 | China | ECMO for acute respiratory distress syndrome; VA-ECMO (17%), VV-ECMO (83%) | 23 | AKI; AKIN criteria | AKI 13/23 (56.5%) | Mortality 9/13 (69%) |
| Antonucci et al. [59] | 2016 | Belgium | ECMO; VA-ECMO (59%), VV-ECMO (41%) | 135 | AKI; AKIN criteria | AKI 95/135 (70.4%) CRRT 63/135 (46.7%) | ICU mortality AKI 55/95 (58%) CRRT 38/63 (60%) |
| Tsai et al. [60] | 2017 | Taiwan | ECMO | 167 | AKI; RIFLE, AKIN and KDIGO on ECMO day 1 | RIFLE AKI 126/167 (75.4%) AKIN AKI 141/167 (84.4%) KDIGO AKI 142/167 (85.0%) | Hospital mortality RIFLE AKI 85/126 (67%) AKIN AKI 90/126 (71%) RIFLE AKI 90/126 (71%) |
| Panholzer et al. [61] | 2017 | Germany | VV-ECMO for ARDS | 46 | RRT | RRT 31/46 (67.4%) | Mortality RRT 23/31 (74%) |
| Chong et al. [62] | 2018 | Taiwan | VA-ECMO for acute fulminant myocarditis and cardiogenic shock | 35 | AKI; not specified | AKI 26/35 (74.3%) RRT 15/35 (42.9%) | Hospital mortality AKI 14/26 (54%) RRT 11/15 (73%) |
| Devasagayaraj et al. [63] | 2018 | USA | VV-ECMO for ARDS | 54 | CRRT | CRRT 16/54 (29.6%) | Hospital mortality 9/16 (56%) |
| Liao et al. [64] | 2018 | China | ECMO; VA-ECMO (93%), VV-ECMO (7%) | 170 | AKI; KDIGO criteria | AKI 91/170 (53.5%) | N/A |
| Paek et al. [65] | 2018 | Korea | ECMO | 538 | CRRT | CRRT 296/838 (35.3%) | 30-day mortality 195/296 (66%) |
| He et al. [66] | 2018 | China | ECMO | 92 | CRRT | CRRT 32/92 (34.8%) | Hospital mortality 19/32 (59%) |
| Chen et al. [67] | 2019 | Taiwan | ECMO | 3251 | RRT | RRT 1759/3251 (54.1%) | Hospital mortality 1298/1759 (74%) |
| Study. | Year | Number | Outcomes | Confounder Adjustment |
|---|---|---|---|---|
| Pagani et al. [15] | 2001 | 33 | Hospital mortality 8.25 (0.89–76.12) | None |
| Lin et al. [30] | 2006 | 46 | Hospital mortality AKI: 14.0 (2.46–79.55) CRRT: 16/16 vs. 14/30 | None |
| Luo et al. [33] | 2009 | 45 | Hospital mortality CRRT: 7.0 (1.26–38.99) | None |
| Brogan et al. [34] | 2009 | 1473 | Hospital mortality Renal insufficiency/failure: 2.13 (1.69–2.72) RRT: 2.13 (1.73–2.63) | Age, duration of mechanical ventilation, weight, pre-ECMO pH, race, diagnosis, ECMO mode, post-ECMO complication |
| Elsharkawy et al. [37] | 2010 | 233 | Hospital mortality RRT: 3.18 (1.77–5.70) | None |
| Yan et al. [36] | 2010 | 67 | Hospital mortality RIFLE AKI: 8.0 (1.61–39.68) AKIN AKI: 12.38 (1.47–104.33) CRRT: 5.73 (1.98–16.58) | None |
| Lan et al. [39] | 2010 | 607 | Hospital mortality RRT: 6.49 (4.12–10.23) | Age, stroke, pre-ECMO infection, hypoglycemia, alkalosis |
| Chen et al. [67] | 2011 | 102 | Hospital mortality AKI: 4.32 (1.65–11.30) CRRT: 5.80 (1.82–18.43) | Age, GCS |
| Chang et al. [44] | 2012 | 113 | Hospital mortality AKI: 2.1 (1.48–3.00) | None |
| Wu et al. [48] | 2012 | 60 | Hospital mortality RRT: 3.76 (1.18–11.95) | None |
| Kielstein et al. [50] | 2013 | 200 | 90-day mortality RRT: 5.47(2.87–10.44) | None |
| Aubron et al. [49] | 2013 | 158 | VA ECMO RRT: 2.12 (0.92–4.88) VV ECMO RRT: 2.52 (0.80–7.95) | None |
| Wu et al. [51] | 2013 | 35 | Hospital mortality RRT: 12 (2.08–69.09) | None |
| Slottosch et al. [23] | 2013 | 77 | 30-day mortality Renal failure: 2.20 (0.78–6.12) | None |
| Unosawa et al. [53] | 2013 | 47 | Mortality during ECMO RRT: 1.67 (0.48–5.83) | None |
| Lazzeri et al. [52] | 2013 | 25 | Mortality RRT: 2.14 (0.38–12.20) | None |
| Hsiao et al. [55] | 2014 | 81 | Hospital mortality CRRT: 2.17 (0.87–5.45) | None |
| Schmidt et al. [7] | 2014 | 172 | Hospital mortality CRRT at ECMO day 1–3: 4.1 (1.71–9.82) 90-day mortality CRRT at ECMO day 1–3: 3.17 (1.32–7.61) | APACHE, fluid balance, major bleeding, propensity score |
| Lee et al. [56] | 2015 | 322 | Hospital mortality AKI: 3.71 (1.96–7.02) | None |
| Haneya et al. [57] | 2015 | 262 | Mortality AKI: 2.18 (1.31–3.61) RRT during ECMO: 1.72 (0.53–5.59) | Age, SOFA score, minute volume, pH, lactate, RRT prior to ECMO, RBC, and FFP transfusion |
| Huang et al. [58] | 2016 | 23 | Mortality AKI: 20.25 (1.88–218.39) | None |
| Lyu et al. [27] | 2016 | 84 | Mortality ARF: 23.90 (7.00–81.60) | None |
| Antonucci et al. [59] | 2016 | 135 | ICU mortality AKI: 1.86 (0.88–3.93) CRRT: 1.70 (0.85–3.37) | None |
| Tsai et al. [60] | 2017 | 167 | Hospital mortality RIFLE AKI: 8.55 (3.63–20.16) AKIN AKI: 13.53 (3.87–47.28) KDIGO AKI: 12.69 (3.62–44.46) | None |
| Panholzer et al. [61] | 2017 | 46 | Mortality RRT: 40.25 (4.54–356.93) | None |
| Martucci et al. [28] | 2017 | 82 | Mortality on ECMO AKI stage 3: 4.55 (1.37–15.17) | None |
| Chong et al. [62] | 2018 | 35 | Hospital mortality AKI: 9.33 (1.02–85.70) RRT: 11.0 (2.26–53.64) | None |
| Devasagayaraj et al. [63] | 2018 | 54 | Hospital mortality RRT: 5.69 (1.58–20.56) | None |
| Chen et al. [67] | 2019 | 3,251 | Hospital mortality RRT: 3.92 (3.36–4.57) | Age, sex, ECMO indication, comorbid conditions, hospital level, study year |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thongprayoon, C.; Cheungpasitporn, W.; Lertjitbanjong, P.; Aeddula, N.R.; Bathini, T.; Watthanasuntorn, K.; Srivali, N.; Mao, M.A.; Kashani, K. Incidence and Impact of Acute Kidney Injury in Patients Receiving Extracorporeal Membrane Oxygenation: A Meta-Analysis. J. Clin. Med. 2019, 8, 981. https://doi.org/10.3390/jcm8070981
Thongprayoon C, Cheungpasitporn W, Lertjitbanjong P, Aeddula NR, Bathini T, Watthanasuntorn K, Srivali N, Mao MA, Kashani K. Incidence and Impact of Acute Kidney Injury in Patients Receiving Extracorporeal Membrane Oxygenation: A Meta-Analysis. Journal of Clinical Medicine. 2019; 8(7):981. https://doi.org/10.3390/jcm8070981
Chicago/Turabian StyleThongprayoon, Charat, Wisit Cheungpasitporn, Ploypin Lertjitbanjong, Narothama Reddy Aeddula, Tarun Bathini, Kanramon Watthanasuntorn, Narat Srivali, Michael A. Mao, and Kianoush Kashani. 2019. "Incidence and Impact of Acute Kidney Injury in Patients Receiving Extracorporeal Membrane Oxygenation: A Meta-Analysis" Journal of Clinical Medicine 8, no. 7: 981. https://doi.org/10.3390/jcm8070981
APA StyleThongprayoon, C., Cheungpasitporn, W., Lertjitbanjong, P., Aeddula, N. R., Bathini, T., Watthanasuntorn, K., Srivali, N., Mao, M. A., & Kashani, K. (2019). Incidence and Impact of Acute Kidney Injury in Patients Receiving Extracorporeal Membrane Oxygenation: A Meta-Analysis. Journal of Clinical Medicine, 8(7), 981. https://doi.org/10.3390/jcm8070981






