Impaired Skeletal Muscle Kynurenine Metabolism in Patients with Chronic Obstructive Pulmonary Disease
Abstract
1. Introduction
2. Experimental Section
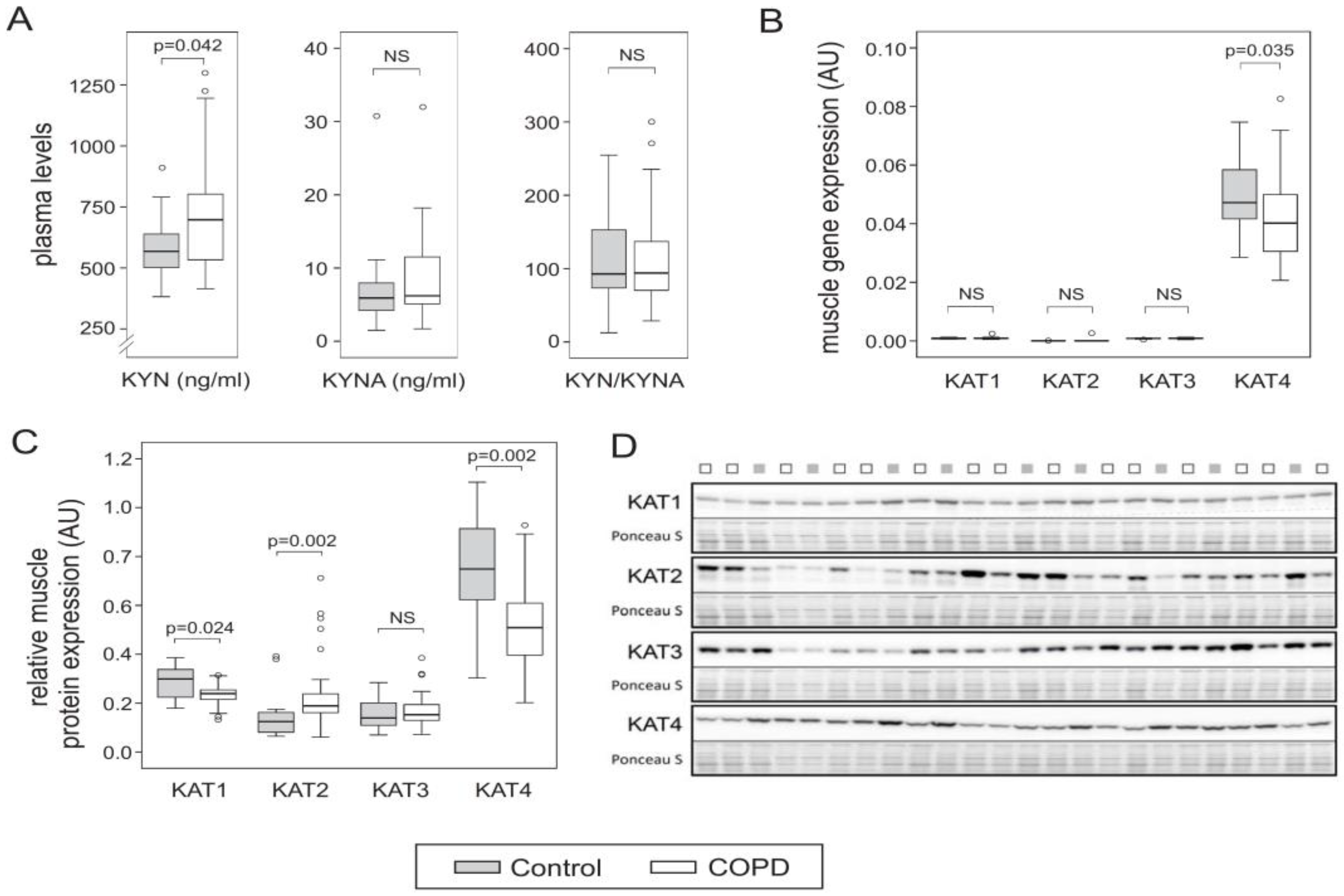
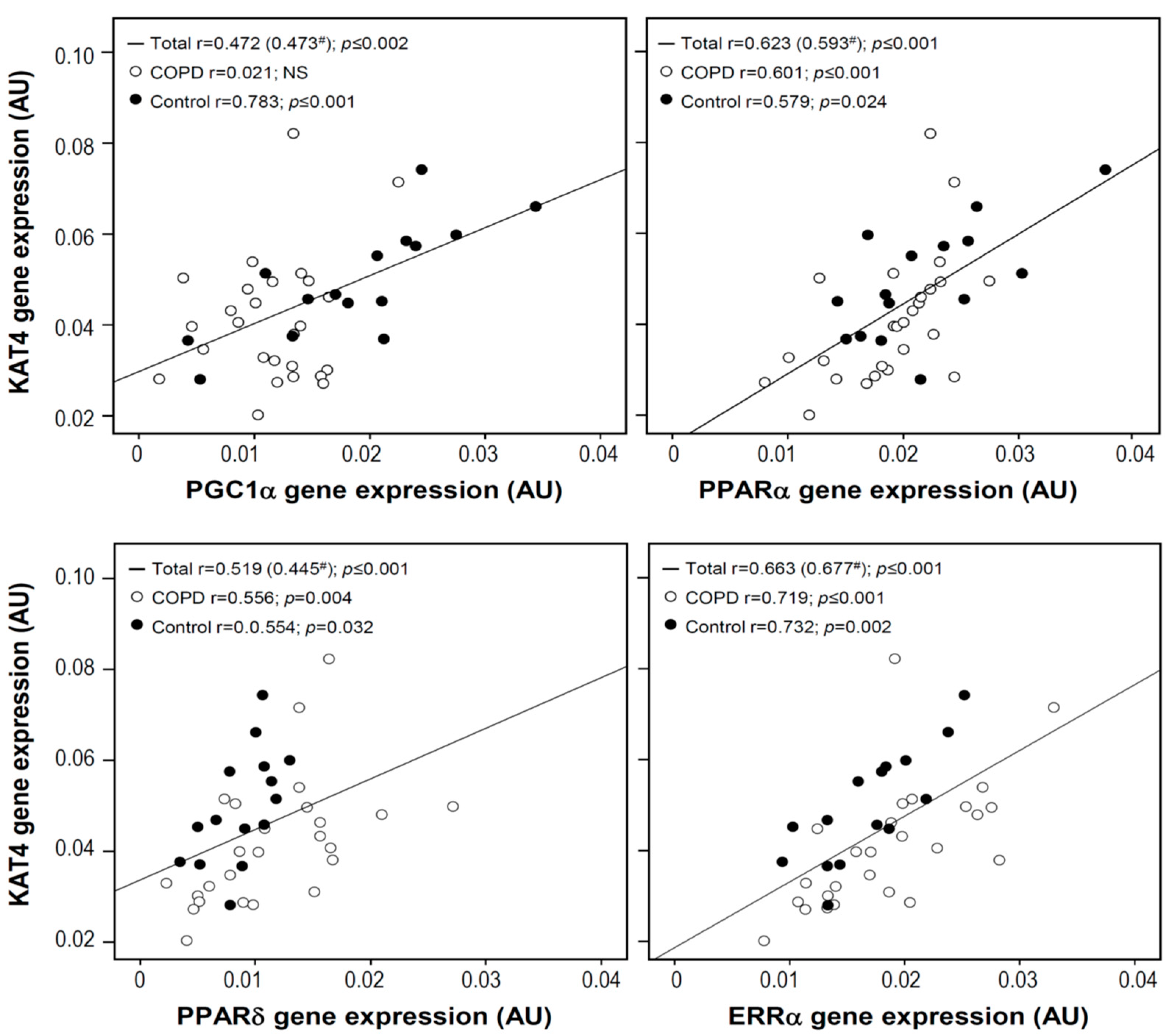
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Vanfleteren, L.; Spruit, M.A.; Wouters, E.F.M.; Franssen, F.M.E. Management of chronic obstructive pulmonary disease beyond the lungs. Lancet Respir. Med. 2016, 4, 911–924. [Google Scholar] [CrossRef]
- Barnes, P.J.; Celli, B.R. Systemic manifestations and comorbidities of COPD. Eur. Respir. J. 2009, 33, 1165–1185. [Google Scholar] [CrossRef]
- Maltais, F.; Decramer, M.; Casaburi, R.; Barreiro, E.; Burelle, Y.; Debigare, R.; Dekhuijzen, P.N.; Franssen, F.; Gayan-Ramirez, G.; Gea, J.; et al. An official American Thoracic Society/European Respiratory Society statement: Update on limb muscle dysfunction in chronic obstructive pulmonary disease. Am. J. Respir. Crit. Care Med. 2014, 189, e15–e62. [Google Scholar] [CrossRef] [PubMed]
- Van Beers, M.; Janssen, D.J.A.; Gosker, H.R.; Schols, A. Cognitive impairment in chronic obstructive pulmonary disease: Disease burden, determinants and possible future interventions. Expert Rev. Respir. Med. 2018, 12, 1061–1074. [Google Scholar] [CrossRef] [PubMed]
- Wilson, I. Depression in the patient with COPD. Int. J. Chron. Obstruct. Pulmon. Dis. 2006, 1, 61–64. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hegerl, U.; Mergl, R. Depression and suicidality in COPD: Understandable reaction or independent disorders? Eur. Respir. J. 2014, 44, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Remels, A.H.; Schrauwen, P.; Broekhuizen, R.; Willems, J.; Kersten, S.; Gosker, H.R.; Schols, A.M. Peroxisome proliferator-activated receptor expression is reduced in skeletal muscle in COPD. Eur. Respir. J. 2007, 30, 245–252. [Google Scholar] [CrossRef]
- Remels, A.H.; Gosker, H.R.; van der Velden, J.; Langen, R.C.; Schols, A.M. Systemic inflammation and skeletal muscle dysfunction in chronic obstructive pulmonary disease: State of the art and novel insights in regulation of muscle plasticity. Clin. Chest. Med. 2007, 28, 537–552. [Google Scholar] [CrossRef]
- Van den Borst, B.; Slot, I.G.; Hellwig, V.A.; Vosse, B.A.; Kelders, M.C.; Barreiro, E.; Schols, A.M.; Gosker, H.R. Loss of quadriceps muscle oxidative phenotype and decreased endurance in patients with mild-to-moderate COPD. J. Appl. Physiol. 2013, 114, 1319–1328. [Google Scholar] [CrossRef]
- Remels, A.H.; Gosker, H.R.; Schrauwen, P.; Hommelberg, P.P.; Sliwinski, P.; Polkey, M.; Galdiz, J.; Wouters, E.F.; Langen, R.C.; Schols, A.M. TNF-alpha impairs regulation of muscle oxidative phenotype: Implications for cachexia? FASEB J. 2010, 24, 5052–5062. [Google Scholar] [CrossRef]
- Pelgrim, C.E.; Peterson, J.D.; Gosker, H.R.; Schols, A.; van Helvoort, A.; Garssen, J.; Folkerts, G.; Kraneveld, A.D. Psychological co-morbidities in COPD: Targeting systemic inflammation, a benefit for both? Eur. J. Pharmacol. 2019, 842, 99–110. [Google Scholar] [CrossRef] [PubMed]
- Zinellu, A.; Fois, A.G.; Zinellu, E.; Sotgiu, E.; Sotgia, S.; Arru, D.; Mangoni, A.A.; Carru, C.; Pirina, P. Increased kynurenine plasma concentrations and kynurenine-tryptophan ratio in mild-to-moderate chronic obstructive pulmonary disease patients. Biomark. Med. 2018, 12, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Cervenka, I.; Agudelo, L.Z.; Ruas, J.L. Kynurenines: Tryptophan’s metabolites in exercise, inflammation, and mental health. Science 2017, 357. [Google Scholar] [CrossRef] [PubMed]
- Solvang, S.H.; Nordrehaug, J.E.; Tell, G.S.; Nygard, O.; McCann, A.; Ueland, P.M.; Midttun, O.; Meyer, K.; Vedeler, C.A.; Aarsland, D.; et al. The kynurenine pathway and cognitive performance in community-dwelling older adults. The Hordaland Health Study. Brain Behav. Immun. 2019, 75, 155–162. [Google Scholar] [CrossRef] [PubMed]
- Moon, H.Y.; van Praag, H. Muscle over mind. Cell Metab. 2014, 20, 560–562. [Google Scholar] [CrossRef] [PubMed]
- Agudelo, L.Z.; Femenia, T.; Orhan, F.; Porsmyr-Palmertz, M.; Goiny, M.; Martinez-Redondo, V.; Correia, J.C.; Izadi, M.; Bhat, M.; Schuppe-Koistinen, I.; et al. Skeletal muscle PGC-1alpha1 modulates kynurenine metabolism and mediates resilience to stress-induced depression. Cell 2014, 159, 33–45. [Google Scholar] [CrossRef] [PubMed]
- Clarke, G.; Fitzgerald, P.; Cryan, J.F.; Cassidy, E.M.; Quigley, E.M.; Dinan, T.G. Tryptophan degradation in irritable bowel syndrome: Evidence of indoleamine 2,3-dioxygenase activation in a male cohort. BMC Gastroenterol. 2009, 9, 6. [Google Scholar] [CrossRef] [PubMed]
- Liu, J.J.; Movassat, J.; Portha, B. Emerging role for kynurenines in metabolic pathologies. Curr. Opin. Clin. Nutr. Metab. Care 2019, 22, 82–90. [Google Scholar] [CrossRef] [PubMed]
- Schlittler, M.; Goiny, M.; Agudelo, L.Z.; Venckunas, T.; Brazaitis, M.; Skurvydas, A.; Kamandulis, S.; Ruas, J.L.; Erhardt, S.; Westerblad, H.; et al. Endurance exercise increases skeletal muscle kynurenine aminotransferases and plasma kynurenic acid in humans. Am. J. Physiol. Cell Physiol. 2016, 310, C836–C840. [Google Scholar] [CrossRef] [PubMed]
- Herrstedt, A.; Bay, M.L.; Simonsen, C.; Sundberg, A.; Egeland, C.; Thorsen-Streit, S.; Djurhuus, S.S.; Magne Ueland, P.; Midttun, O.; Pedersen, B.K.; et al. Exercise-mediated improvement of depression in patients with gastro-esophageal junction cancer is linked to kynurenine metabolism. Acta. Oncol. 2019, in press. [Google Scholar] [CrossRef] [PubMed]
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Hill, K.; Holland, A.E.; Lareau, S.C.; Man, W.D.; et al. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2013, 188, e13–e64. [Google Scholar] [CrossRef] [PubMed]
- Gordon, C.S.; Waller, J.W.; Cook, R.M.; Cavalera, S.L.; Lim, W.T.; Osadnik, C.R. Effect of pulmonary rehabilitation on symptoms of anxiety and depression in chronic obstructive pulmonary disease: A systematic review and meta-analysis. Chest. in press. [CrossRef]
- Desveaux, L.; Harrison, S.L.; Gagnon, J.F.; Goldstein, R.S.; Brooks, D.; Pepin, V. Effects of exercise training on cognition in chronic obstructive pulmonary disease: A systematic review. Respir. Med. 2018, 139, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Schols, A. Nutrition as a metabolic modulator in COPD. Chest 2013, 144, 1340–1345. [Google Scholar] [CrossRef] [PubMed]
- Wirthgen, E.; Hoeflich, A.; Rebl, A.; Gunther, J. Kynurenic Acid: The Janus-Faced Role of an Immunomodulatory Tryptophan Metabolite and Its Link to Pathological Conditions. Front. Immunol. 2017, 8, 1957. [Google Scholar] [CrossRef] [PubMed]
| Controls (n = 15) | COPD (n = 29) | ||
|---|---|---|---|
| Demographics | |||
| Age, years | 65 (6) | 65 (6) | NS |
| Sex, % men | 60 | 55 | NS |
| BMI, kg/m2 | 24.9 (3.3) | 25.5 (3.6) | NS |
| Pulmonary function | |||
| FEV1, % pred | 113 (15) | 58 (16) | p ≤ 0.001 |
| FVC, % pred | 120 (17) | 104 (22) | p = 0.016 |
| FEV1/FVC, % | 74 (5) | 45 (11) | p ≤ 0.001 |
| DLCO, % pred | 95 (19) | 53 (18) | p ≤ 0.001 |
| Muscle Biopsy | |||
| PGC1α gene expression (AU) | 0.019 (0.008) | 0.011 (0.005) | p ≤ 0.001 |
| ETC complex IV protein expression (AU) | 5.11 (3.51) | 2.71 (1.97) | p = 0.024 |
| ETC complex V protein expression (AU) | 0.83 (0.50) | 0.57 (0.33) | p = 0.047 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gosker, H.R.; Clarke, G.; de Theije, C.C.; Cryan, J.F.; Schols, A.M.W.J. Impaired Skeletal Muscle Kynurenine Metabolism in Patients with Chronic Obstructive Pulmonary Disease. J. Clin. Med. 2019, 8, 915. https://doi.org/10.3390/jcm8070915
Gosker HR, Clarke G, de Theije CC, Cryan JF, Schols AMWJ. Impaired Skeletal Muscle Kynurenine Metabolism in Patients with Chronic Obstructive Pulmonary Disease. Journal of Clinical Medicine. 2019; 8(7):915. https://doi.org/10.3390/jcm8070915
Chicago/Turabian StyleGosker, Harry R., Gerard Clarke, Chiel C. de Theije, John F. Cryan, and Annemie M. W. J. Schols. 2019. "Impaired Skeletal Muscle Kynurenine Metabolism in Patients with Chronic Obstructive Pulmonary Disease" Journal of Clinical Medicine 8, no. 7: 915. https://doi.org/10.3390/jcm8070915
APA StyleGosker, H. R., Clarke, G., de Theije, C. C., Cryan, J. F., & Schols, A. M. W. J. (2019). Impaired Skeletal Muscle Kynurenine Metabolism in Patients with Chronic Obstructive Pulmonary Disease. Journal of Clinical Medicine, 8(7), 915. https://doi.org/10.3390/jcm8070915





