The Value of Oxygenation Saturation Index in Predicting the Outcomes of Patients with Acute Respiratory Distress Syndrome
Abstract
1. Introduction
2. Patients and Methods
2.1. Patients and Hospital Setting
2.2. Variables Measurements
2.3. Definitions
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Conflicts of Interest
References
- Phua, J.; Badia, J.R.; Adhikari, N.K.; Friedrich, J.O.; Fowler, R.A.; Singh, J.M.; Scales, D.C.; Stather, D.R.; Li, A.; Jones, A.; et al. Has mortality from acute respiratory distress syndrome decreased over time? A systematic review. Am. J. Respir. Crit. Care Med. 2009, 179, 220–227. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Blanco, J.; Añón, J.M.; Santos-Bouza, A.; Blanch, L.; Ambrós, A.; Gandía, F.; Carriedo, D.; Mosteiro, F.; Basaldúa, S.; et al. The ALIEN study: Incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation. Intensive Care Med. 2011, 37, 1932–1941. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Sulemanji, D.; Kacmarek, R.M. The acute respiratory distress syndrome: Incidence and mortality, has it changed? Curr. Opin. Crit. Care 2014, 20, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Bernard, G.R.; Artigas, A.; Brigham, K.L.; Carlet, J.; Falke, K.; Hudson, L.; Lamy, M.; Legall, J.R.; Morris, A.; Spragg, R. The American-European consensus conference on ARDS. Definitions, mechanisms, relevant outcomes, and clinical trial coordination. Am. J. Respir. Crit. Care Med. 1994, 149, 818–824. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S.; Antonelli, M.; Anzueto, A.; et al. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [PubMed]
- Cooke, C.R.; Kahn, J.M.; Caldwell, E.; Okamoto, V.N.; Heckbert, S.R.; Hudson, L.D.; Rubenfeld, G.D. Predictors of hospital mortality in a population-based cohort of patients with acute lung injury. Crit. Care Med. 2008, 36, 1412–1420. [Google Scholar] [CrossRef] [PubMed]
- Villar, J.; Pérez-Méndez, L.; Basaldúa, S.; Blanco, J.; Aguilar, G.; Toral, D.; Zavala, E.; Romera, M.A.; González-Díaz, G.; Nogal, F.D.; et al. A risk tertiles model for predicting mortality in patients with acute respiratory distress syndrome: Age, plateau pressure, and P(aO(2))/F(IO(2)) at ARDS onset can predict mortality. Respir. Care 2011, 56, 420–428. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.C.; Sung, M.I.; Ho, C.H.; Liu, H.H.; Chen, C.M.; Chiang, S.R.; Chao, C.M.; Liu, W.L.; Hsing, S.C.; Cheng, K.C. The prognostic value of N-terminal proB-type natriuretic peptide in patients with acute respiratory distress syndrome. Sci. Rep. 2017, 7, 44784. [Google Scholar] [CrossRef] [PubMed]
- Lai, C.C.; Sung, M.I.; Liu, H.H.; Chen, C.M.; Chiang, S.R.; Liu, W.L.; Chao, C.M.; Ho, C.H.; Weng, S.F.; Hsing, S.C.; et al. The ratio of partial pressure arterial oxygen and fraction of inspired oxygen 1 day after acute respiratory distress syndrome onset can predict the outcomes of involving patients. Medicine 2016, 95, e3333. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.M.; Duggal, A.; Hou, P.C.; Tidswell, M.; Khan, A.; Exline, M.; Park, P.K.; Schoenfeld, D.A.; Liu, M.; Grissom, C.K.; et al. Nonlinear imputation of PaO2/FIO2 from SpO2/FIO2 among mechanically ventilated patients in the ICU: A prospective, observational study. Crit. Care Med. 2017, 45, 1317–1324. [Google Scholar] [CrossRef] [PubMed]
- Brown, S.M.; Grissom, C.K.; Moss, M.; Rice, T.W.; Schoenfeld, D.; Hou, P.C.; Thompson, B.T.; Brower, R.G.; NIH/NHLBI PETAL Network Collaborators. Nonlinear imputation of PaO2/FiO2 from SpO2/FiO2 among patients with acute respiratory distress syndrome. Chest 2016, 150, 307–313. [Google Scholar] [CrossRef] [PubMed]
- DesPrez, K.; McNeil, J.B.; Wang, C.; Bastarache, J.A.; Shaver, C.M.; Ware, L.B. Oxygenation saturation index predicts clinical outcomes in ARDS. Chest 2017, 152, 1151–1158. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Janz, D.R.; Shaver, C.M.; Bernard, G.R.; Bastarache, J.A.; Ware, L.B. Clinical characteristics and outcomes are similar in ARDS diagnosed by oxygen saturation/FiO2 ratio compared with PaO2/FiO2 ratio. Chest 2015, 148, 1477–1483. [Google Scholar] [CrossRef] [PubMed]
- Barbas, C.S.; Isola, A.M.; Caser, E.B. What is the future of acute respiratory distress syndrome after the Berlin definition? Curr. Opin. Crit. Care 2014, 20, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Hernu, R.; Wallet, F.; Thiollière, F.; Martin, O.; Richard, J.C.; Schmitt, Z.; Wallon, G.; Delannoy, B.; Rimmelé, T.; Démaret, C.; et al. An attempt to validate the modification of the American-European consensus definition of acute lung injury/acute respiratory distress syndrome by the Berlin definition in a university hospital. Intensive Care Med. 2013, 39, 2161–2170. [Google Scholar] [CrossRef] [PubMed]
| Variables | No (%) of Patients (n = 101) | No (%) of Survivors (n = 43) | No (%) of Mortalities (n = 58) | p Value * |
|---|---|---|---|---|
| Age (years) | 69.2 ± 13.5 | 66.7 ± 14.4 | 71.0 ± 12.7 | 0.12 |
| Gender | ||||
| Male | 63 (62.4) | 25 (58.1) | 38 (65.5) | 0.45 |
| Female | 38 (37.6) | 18 (41.9) | 20 (34.5) | |
| APACHE II scores | 27.9 ± 10.4 | 23.0 ± 9.1 | 31.6 ± 9.8 | <0.001 |
| Extra-pulmonary ARDS | 8 (7.9) | 3 (7.0) | 5 (8.6) | 0.76 |
| Cause of ARDS | ||||
| Pneumonia | 94 (94.1) | 40 (93.0) | 54 (93.1) | 0.29 |
| Sepsis | 5 (5.0) | 1 (2.3) | 4 (6.9) | |
| Major trauma | 1 (1.0) | 1 (2.3) | 0 (0) | |
| Acute pancreatitis | 1 (1.0) | 1 (2.3) | 0 (0) | |
| Shock | 81 (80.2) | 32 (74.4) | 49 (84.5) | 0.21 |
| Underlying disease | ||||
| Chronic lung disease | 5 (5.0) | 1 (2.3) | 4 (6.9) | 0.30 |
| Chronic kidney disease | 21 (20.8) | 10 (23.3) | 11 (19.0) | 0.60 |
| Congestive heart failure | 8 (7.9) | 2 (4.7) | 6 (10.3) | 0.30 |
| Liver cirrhosis | 11 (10.9) | 5 (11.6) | 6 (10.3) | 0.84 |
| Diabetes mellitus | 33 (32.7) | 15 (34.9) | 18 (31.0) | 0.68 |
| Malignancy | 42 (41.6) | 15 (34.9) | 27 (46.6) | 0.24 |
| Ventilator setting | ||||
| PEEP | 10 (10–12) | 10 (10–12) | 10 (10–12) | 0.47 |
| Vt | 450 (410–549) | 476 (420–557) | 450 (400–534) | 0.13 |
| Laboratory findings | ||||
| Hemoglobin | 9.9 (8.8–11.4) | 9.9 (9.7–17.2) | 9.9 (9.2–10.9) | 0.96 |
| Total-bilirubin | 1.0 (0.5–2.0) | 0.8 (0.5–1.6) | 1.1 (0.6–2.4) | 0.16 |
| pH | 7.35 (7.28–7.41) | 7.35 (7.28–7.41) | 7.34 (7.28–7.42) | 0.98 |
| HCO3− | 20.3 (16.9–24.1) | 20.3 (17.0–22.5) | 20.0 (16.4–26.1) | 0.91 |
| Lowest PaO2 | 72.0 (64.2–83.1) | 72.2 (64.3–83.2) | 71.7 (63.4–83.4) | 0.71 |
| Lowest SpO2 | 90.0 (85.5–92.5) | 92.0 (90.0–94.0) | 88.0 (80.8–91.3) | <0.001 |
| Lowest PaO2/FiO2 ratio | 108.8 (91.7–138.3) | 114.0 (100.9–145.6) | 106.0 (88.7–130.0) | 0.08 |
| Lowest SpO2/FiO2 ratio | 145.0 (116.3–186.0) | 148.3 (130.7–190.0) | 139.3 (102.1–163.5) | 0.046 |
| Highest mean airway pressure | 21.0 (19.5–23.0) | 21.0 (18.0–22.0) | 21.5 (20.0–24.0) | 0.012 |
| Oxygenation index | 19.0 (15.0–23.5) | 15.9 (13.7–22.1) | 20.5 (16.0–26.6) | 0.008 |
| Oxygenation saturation index | 15.0 (11.3–18.2) | 13.6 (9.7–17.2) | 16.0 (12.9–21.4) | 0.008 |
| Outcome | ||||
| MV duration | 12.0 (5–21.8) | 15.5 (8.8–32.5) | 8.0 (3.4–19.0) | 0.002 |
| ICU LOS | 13.0 (4.3–25.8) | 19.0 (10.8–38) | 7.0 (2.8–18.0) | <0.001 |
| Hospital LOS | 18.0 (4.3–33.3) | 32.5 (19.5–48.5) | 7.0 (2.8–18.0) | <0.001 |
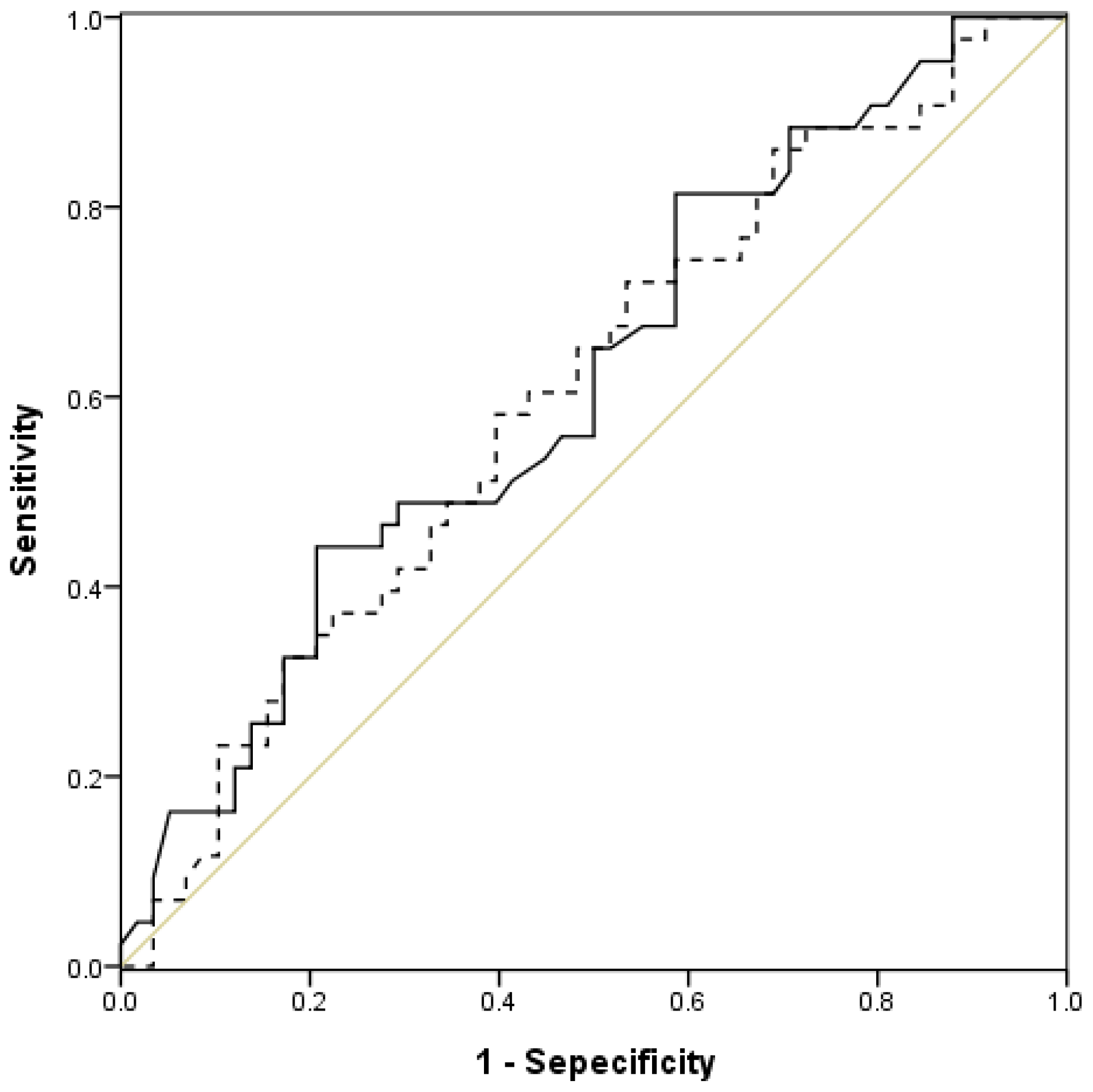
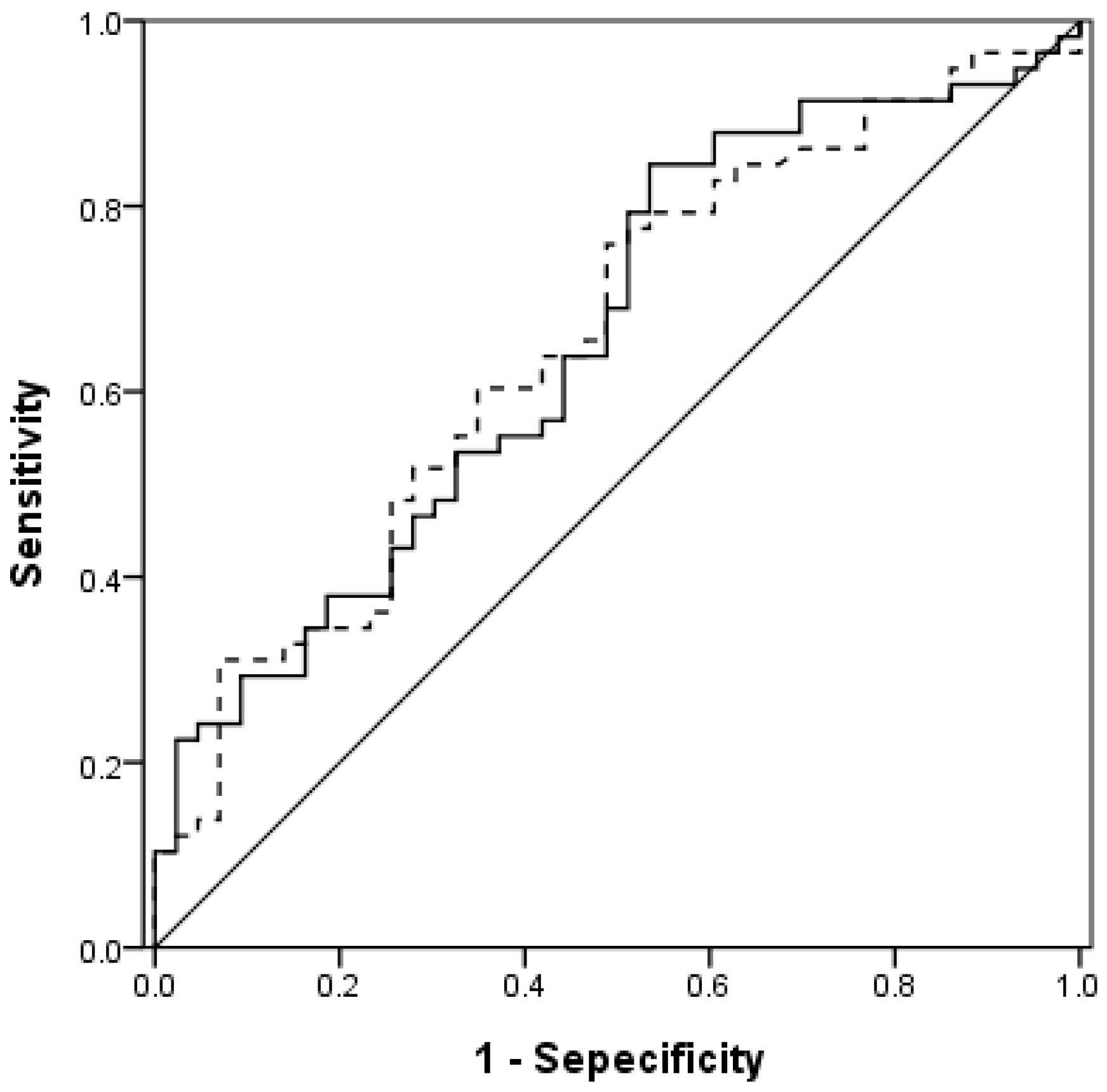
| Measure | Area under the ROC Curve | 95% CI | p Value |
|---|---|---|---|
| Lowest PaO2/FiO2 ratio | 0.603 | 0.492–0.714 | 0.08 |
| Lowest SpO2/FiO2 ratio | 0.616 | 0.506–0.726 | 0.046 |
| Oxygenation index | 0.654 | 0.547–0.761 | 0.008 |
| Oxygen saturation index | 0.656 | 0.548–0.763 | 0.008 |
| Variable | OR | 95% CI | p Value |
|---|---|---|---|
| Lowest PaO2/FiO2 ratio | |||
| ≤100 | 1 | ||
| >100 | 0.794 | 0.25–2.52 | 0.7 |
| Lowest SpO2/FiO2 ratio | |||
| ≤142 | 1 | ||
| >142 | 0.36 | 0.09–1.35 | 0.13 |
| Oxygenation index | |||
| <16 | 1 | ||
| ≥16 | 2.92 | 0.98–8.68 | 0.054 |
| Oxygenation saturation index | |||
| <12 | 1 | ||
| ≥12 | 5.22 | 1.31–20.76 | 0.019 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, W.-L.; Lin, W.-T.; Kung, S.-C.; Lai, C.-C.; Chao, C.-M. The Value of Oxygenation Saturation Index in Predicting the Outcomes of Patients with Acute Respiratory Distress Syndrome. J. Clin. Med. 2018, 7, 205. https://doi.org/10.3390/jcm7080205
Chen W-L, Lin W-T, Kung S-C, Lai C-C, Chao C-M. The Value of Oxygenation Saturation Index in Predicting the Outcomes of Patients with Acute Respiratory Distress Syndrome. Journal of Clinical Medicine. 2018; 7(8):205. https://doi.org/10.3390/jcm7080205
Chicago/Turabian StyleChen, Wan-Ling, Wei-Ting Lin, Shu-Chen Kung, Chih-Cheng Lai, and Chien-Ming Chao. 2018. "The Value of Oxygenation Saturation Index in Predicting the Outcomes of Patients with Acute Respiratory Distress Syndrome" Journal of Clinical Medicine 7, no. 8: 205. https://doi.org/10.3390/jcm7080205
APA StyleChen, W.-L., Lin, W.-T., Kung, S.-C., Lai, C.-C., & Chao, C.-M. (2018). The Value of Oxygenation Saturation Index in Predicting the Outcomes of Patients with Acute Respiratory Distress Syndrome. Journal of Clinical Medicine, 7(8), 205. https://doi.org/10.3390/jcm7080205





