Can Photoplethysmography Replace Arterial Blood Pressure in the Assessment of Blood Pressure?
Abstract
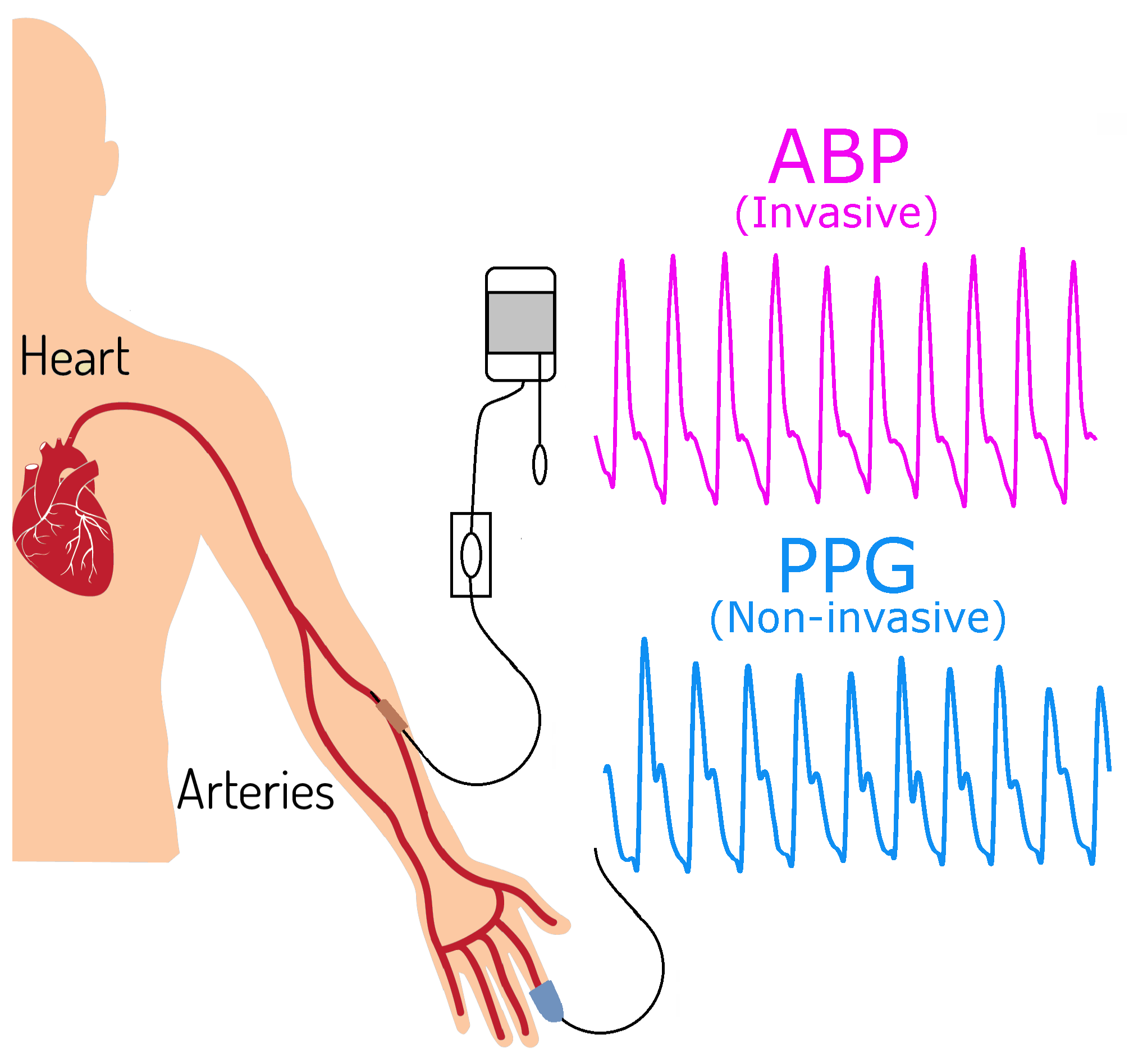
1. Introduction
2. Methods
2.1. Hypotheses
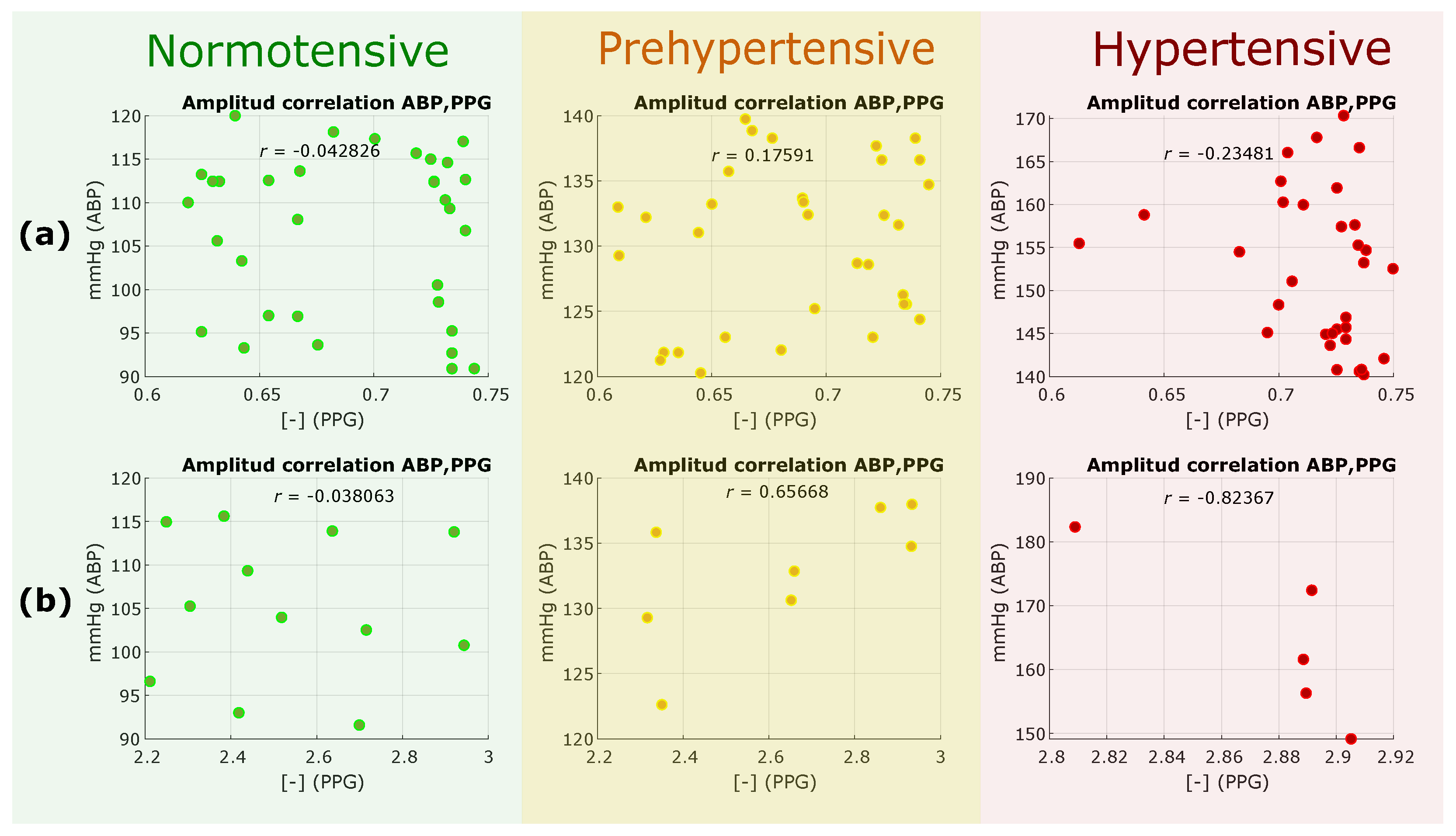
- H1: If the PPG amplitude (Linear time domain analysis) is correlated with the ABP amplitude, then the PPG amplitude can replace ABP for measuring BP.
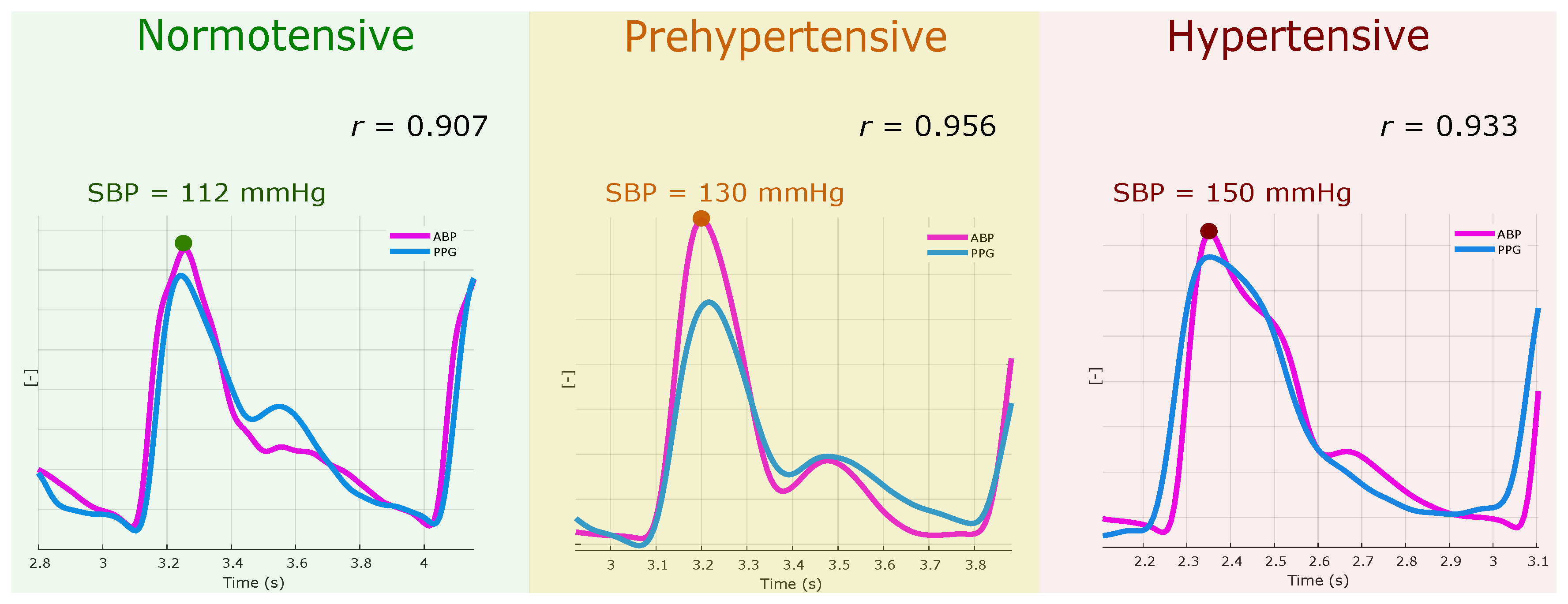
- H2: If the PPG morphology (Linear time domain analysis) is correlated with the ABP morphology, then the PPG waveform morphology holds valuable information that can be used for evaluating BP.
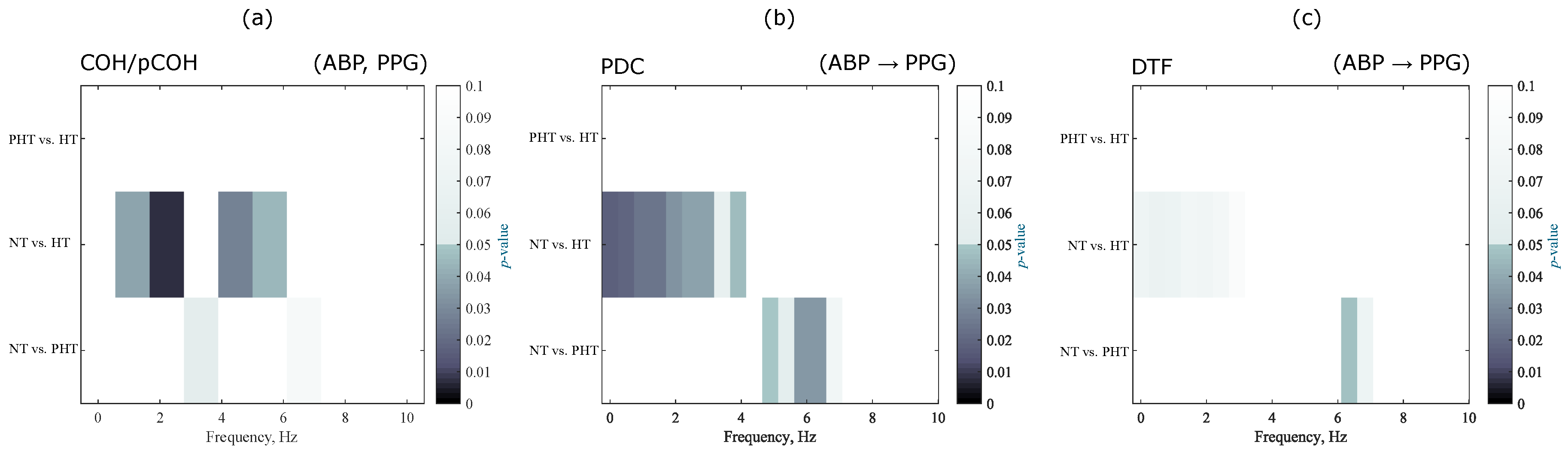
- H3: If the PPG waveform and the ABP have mutual information and coherence (Nonlinear dependency analysis), then the PPG waveform morphology holds valuable information that can be used for evaluating BP.
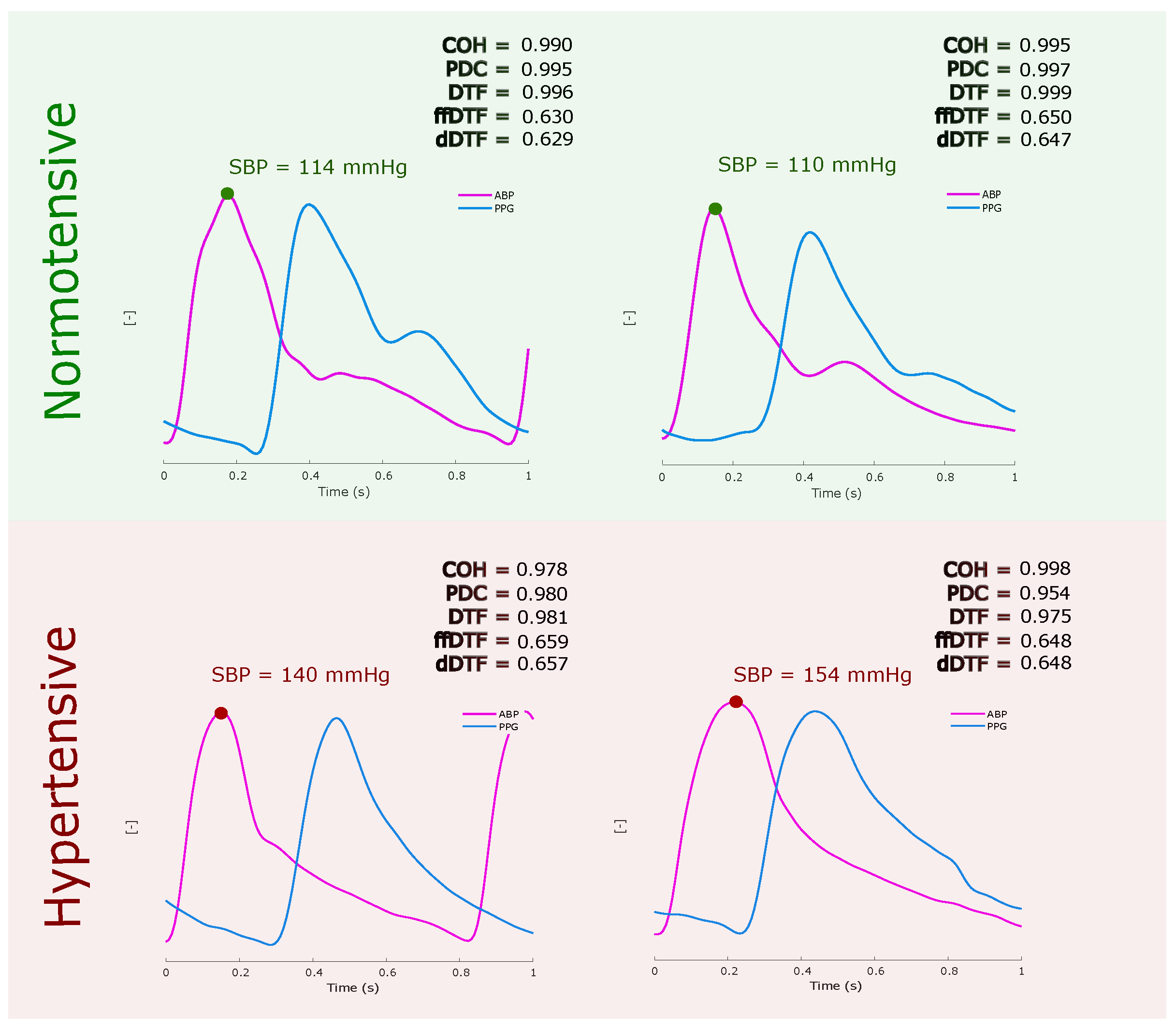
2.2. In-Phase Analysis
2.3. Out-Phase Analysis
2.4. Statistical Analysis
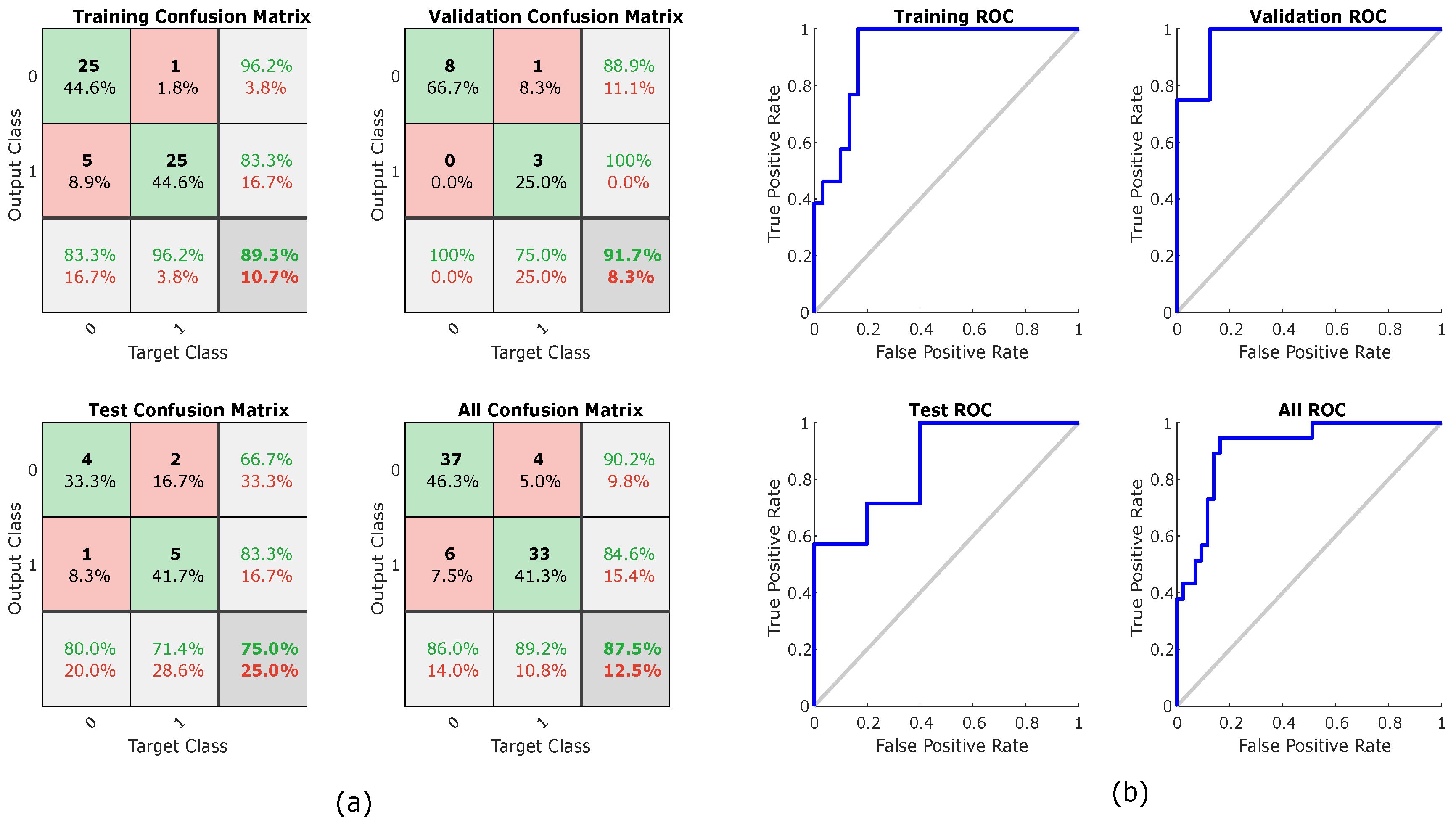
2.5. Classification Analysis
3. Results and Discussion
4. Limitation of Study and Future Work
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gabb, G.M.; Mangoni, A.A.; Anderson, C.S.; Cowley, D.; Dowden, J.S.; Golledge, J.; Hankey, G.J.; Howes, F.S.; Leckie, L.; Perkovic, V.; et al. Guideline for the diagnosis and management of hypertension in adults—2016. Mortality 2016, 205, 85–89. [Google Scholar]
- Kumar, V.; Abbas, A.; Fausto, N.; Aster, J. Robbins and Cotran Pathologic Basis of Disease, Professional; Elsevier: Amsterdam, The Netherlands, 2009. [Google Scholar]
- Allen, J. Photoplethysmography and its application in clinical physiological measurement. Physiol. Meas. 2007, 28, R1. [Google Scholar] [CrossRef]
- Xing, X.; Sun, M. Optical blood pressure estimation with photoplethysmography and FFT-based neural networks. Biomed. Opt. Express 2016, 7, 3007–3020. [Google Scholar]
- Nitzan, M.; Slotki, I.; Shavit, L. More accurate systolic blood pressure measurement is required for improved hypertension management: A perspective. Med. Devices 2017, 10, 157–163. [Google Scholar]
- Njoum, H.; Kyriacou, P.A. Photoplethysmography for the assessment of haemorheology. Sci. Rep. 2017, 7, 1406. [Google Scholar] [CrossRef]
- Sharkey, E.J.; Di Maria, C.; Klinge, A.; Murray, A.; Zheng, D.; O’Sullivan, J.; Allen, J. Innovative multi-site photoplethysmography measurement and analysis demonstrating increased arterial stiffness in paediatric heart transplant recipients. Physiol. Meas. 2018, 39. [Google Scholar] [CrossRef]
- Hsu, P.-C.; Wu, H.-T.; Sun, C.-K. Assessment of subtle changes in diabetes-associated arteriosclerosis using photoplethysmographic pulse wave from index finger. J. Med. Syst. 2018, 42, 43. [Google Scholar] [CrossRef]
- Rajala, S.; Lindholm, H.; Taipalus, T. Comparison of photoplethysmogram measured from wrist and finger and the effect of measurement location on pulse arrival time. Physiol. Meas. 2018, 39. [Google Scholar] [CrossRef]
- Elgendi, M.; Liang, Y.; Ward, R. Toward generating more diagnostic features from photoplethysmogram waveforms. Diseases 2018, 6, 20. [Google Scholar]
- Euliano, T.Y.; Michalopoulos, K.; Singh, S.; Gregg, A.R.; Del Rio, M.; Vasilopoulos, T.; Johnson, A.M.; Onkala, A.; Darmanjian, S.; Euliano, N.R.; et al. Photoplethysmography and heart rate variability for the diagnosis of preeclampsia. Anest. Anal. 2018, 126, 913–919. [Google Scholar]
- Lan, K.C.; Raknim, P.; Kao, W.F.; Huang, J.H. Toward Hypertension Prediction Based on PPG-Derived HRV Signals: A Feasibility Study. J. Med. Syst. 2018, 42, 103. [Google Scholar]
- Shariati, N.H.; Zahedi, E.; Jajai, H.M. Classification of vascular function in upper limb using bilateral photoplethysmographic signals. Physiol. Meas. 2008, 29, 365–374. [Google Scholar]
- Liang, Y.; Chen, Z.; Ward, R.; Elgendi, M. Hypertension assessment via ECG and PPG signals: An evaluation using MIMIC database. Diagnostics 2018, 8, 65. [Google Scholar] [CrossRef]
- Picone, D.S.; Schultz, M.G.; Otahal, P.; Aakhus, S.; Al-Jumaily, A.M.; Black, J.A.; Bos, W.J.; Chambers, J.B.; Chen, C.H.; Cheng, H.M.; et al. Accuracy of cuff-measured blood pressure: Systematic reviews and meta-analyses. J. Am. Coll. Cardiol. 2017, 70, 572–586. [Google Scholar]
- Johnson, A.E.; Pollard, T.J.; Shen, L.; Lehman, L.H.; Feng, M.; Ghassemi, M.; Moody, B.; Szolovits, P.; Anthony Celi, L.; Mark, R.G. MIMIC-III, a freely accessible critical care database. Sci. Data 2016, 3, 160035. [Google Scholar] [CrossRef]
- Blinowska, K.J. Review of the methods of determination of directed connectivity from multichannel data. Med. Biol. Eng. Comput. 2011, 49, 521–529. [Google Scholar]
- Takalo, R.; Hytti, H.; Ihalainen, H. Tutorial on univariate autoregressive spectral analysis. J. Clin. Monit. Comput. 2005, 19, 401–410. [Google Scholar]
- Baccalá, L.A.; Sameshima, K. Partial directed coherence: a new concept in neural structure determination. Biol. Cybern. 2001, 84, 463–474. [Google Scholar]
- Kaminski, M.J.; Blinowska, K.J. A new method of the description of the information flow in the brain structures. Biol. Cybern. 1991, 65, 203–210. [Google Scholar]
- Clifford, G.D.; Scott, D.J.; Villarroel, M. User Guide and Documentation for the MIMIC II Database, Version 2.6. Available online: https://mimic.mit.edu/archive/mimic-ii-guide.pdf (accessed on 8 February 2012).
- Hsiu, H.; Hsu, C.-L.; Wu, T.-L. A preliminary study on the correlation of frequency components between finger PPG and radial arterial BP waveforms. In Proceedings of the International Conference on Biomedical and Pharmaceutical Engineering, Singapore, 2–4 December 2009; pp. 1–4. [Google Scholar]
- Choi, A.; Shin, H. Photoplethysmography sampling frequency: Pilot assessment of how low can we go to analyze pulse rate variability with reliability? Physiol. Meas. 2017, 38, 2252. [Google Scholar]
- Shaw, L.; Routray, A. Topographical assessment of neurocortical connectivity by using directed transfer function and partial directed coherence during meditation. Cogn. Process. 2018, 1–10. [Google Scholar] [CrossRef]
- Sezen, C.; Didier, G.; Olivier, R. Time, frequency, and time—varying granger—causality measures in neuroscience. Stat. Med. 2018, 37, 1910–1931. [Google Scholar]
- Aguilar, G.M.M.; Gutiérrez, D. Using cortico-muscular and cortico-cardiac coherence to study the role of the brain in the development of muscular fatigue. Biomed. Signal Process. Control 2018. In press. [Google Scholar]
- Orini, M.; Citi, L.; Barbieri, R. Bivariate point process modeling and joint non-stationary analysis of pulse transit time and heart period. Conf. Proc. IEEE Eng. Med. Biol. Soc. 2012, 2012, 2831–2834. [Google Scholar]
- Forouzanfar, M.; Ahmad, S.; Batkin, I.; Dajani, H.R.; Groza, V.Z.; Bolic, M. Coefficient-free blood pressure estimation based on pulse transit time-cuff pressure dependence. IEEE Trans. Biomed. Eng. 2013, 60, 1814–1824. [Google Scholar] [CrossRef] [PubMed]
- Wang, R.; Jia, W.; Mao, Z.-H.; Sclabassi, R.J.; Sun, M. Cuff-free blood pressure estimation using pulse transit time and heart rate. Int. Conf. Signal Process. Proc. 2014, 2014, 115–118. [Google Scholar]
- Zhang, Q.; Chen, X.; Fang, Z.; Xue, Y.; Zhan, Q.; Yang, T.; Xia, S. Cuff-less blood pressure measurement using pulse arrival time and a kalman filter. J. Micromech. Microeng. 2017, 27, 024002. [Google Scholar] [CrossRef]
- Pflugradt, M.; Geissdoerfer, K.; Goernig, M.; Orglmeister, R. A fast multimodal ectopic beat detection method applied for blood pressure estimation based on pulse wave velocity measurements in wearable sensors. Sensors 2017, 17, 158. [Google Scholar]
- Feng, J.; Huang, Z.; Zhou, C.; Ye, X. Study of continuous blood pressure estimation based on pulse transit time, heart rate and photoplethysmography-derived hemodynamic covariates. Aust. Phys. Eng. Sci. Med. 2018, 41, 403–413. [Google Scholar]
- Gesche, H.; Grosskurth, D.; Küchler, G.; Patzak, A. Continuous blood pressure measurement by using the pulse transit time: comparison to a cuff-based method. Eur. J. Appl. Physiol. 2012, 112, 309–315. [Google Scholar]
- McCarthy, B.; Vaughan, C.; O’flynn, B.; Mathewson, A.; Mathúna, C.Ó. An examination of calibration intervals required for accurately tracking blood pressure using pulse transit time algorithms. J. Hum. Hypertens. 2013, 27, 744. [Google Scholar]
- Plante, T.B.; Urrea, B.; MacFarlane, Z.T.; Blumenthal, R.S.; Miller, E.R.; Appel, L.J.; Martin, S.S. Validation of the instant blood pressure smartphone app. JAMA Int. Med. 2016, 176, 700–702. [Google Scholar]
- Raichle, C.J.; Eckstein, J.; Lapaire, O.; Leonardi, L.; Brasier, N.; Vischer, A.S.; Burkard, T. Performance of a blood pressure smartphone app in pregnant women: The iparr trial (iphone app compared with standard rr measurement. Hypertension 2018, 71, 1164–1169. [Google Scholar]
| Normotensive | Prehypertensive | Hypertensive | |||
|---|---|---|---|---|---|
| Subject ID | r | Subject ID | r | Subject ID | r |
| ’11727_2’ | 0.9073 | ’12531_2’ | 0.8385 | ’10464_2’ | 0.9327 |
| ’12174_2’ | 0.9142 | ’13600_2’ | 0.916 | ’11187_2’ | 0.906 |
| ’17848_2’ | 0.9676 | ’15218_2’ | 0.9797 | ’1501_2’ | 0.9023 |
| ’19700_2’ | 0.951 | ’15716_2’ | 0.9286 | ’15902_2’ | 0.9696 |
| ’2104_2’ | 0.9459 | ’16129_2’ | 0.9557 | ’18642_2’ | 0.9448 |
| ’2513_2’ | 0.9201 | ’18970_2’ | 0.9025 | ’19578_2’ | 0.9492 |
| ’27436_2’ | 0.9806 | ’21730_2’ | 0.7777 | ’20726_2’ | 0.9109 |
| ’27648_2’ | 0.9689 | ’26897_2’ | 0.9317 | ’22335_2’ | 0.947 |
| ’27833_2’ | 0.9354 | ’27241_2’ | 0.9359 | ’23201_2’ | 0.9558 |
| ’27887_2’ | 0.802 | ’27337_2’ | 0.9384 | ’2458_2’ | 0.9744 |
| ’28077_2’ | 0.9362 | ’27434_2’ | 0.8639 | ’27446_2’ | 0.7908 |
| ’28187_2’ | 0.9633 | ’27845_2’ | 0.9413 | ’28499_2’ | 0.9787 |
| ’28813_2’ | 0.9802 | ’28758_2’ | 0.8939 | ’28510_2’ | 0.921 |
| ’28910_2’ | 0.9699 | ’28882_2’ | 0.9833 | ’28775_2’ | 0.8816 |
| ’29102_2’ | 0.9178 | ’44088_2’ | 0.8657 | ’29127_2’ | 0.978 |
| ’29120_2’ | 0.9382 | ’44104_2’ | 0.9413 | ’44118_2’ | 0.9415 |
| ’3039_2’ | 0.9481 | ’44201_2’ | 0.9773 | ’44171_2’ | 0.9377 |
| ’44223_2’ | 0.9533 | ’44233_2’ | 0.9592 | ’44173_2’ | 0.969 |
| ’44409_2’ | 0.9441 | ’44458_2’ | 0.8442 | ’44347_2’ | 0.8966 |
| ’44422_2’ | 0.9672 | ’44496_2’ | 0.9571 | ’44572_2’ | 0.93 |
| ’44432_2’ | 0.956 | ’44590_2’ | 0.9745 | ’44615_2’ | 0.8795 |
| ’44526_2’ | 0.8325 | ’44623_2’ | 0.945 | ’44616_2’ | 0.9505 |
| ’44598_2’ | 0.9419 | ’44640_2’ | 0.9663 | ’44626_2’ | 0.9526 |
| ’44601_2’ | 0.9499 | ’44647_2’ | 0.9771 | ’44704_2’ | 0.9689 |
| ’44629_2’ | 0.9757 | ’44902_2’ | 0.9434 | ’44839_2’ | 0.9742 |
| ’44671_2’ | 0.9612 | ’45181_2’ | 0.8832 | ’44981_2’ | 0.9583 |
| ’44758_2’ | 0.9754 | ’45384_2’ | 0.9142 | ’45098_2’ | 0.9663 |
| ’44763_2’ | 0.9261 | ’45426_2’ | 0.8659 | ’45140_2’ | 0.9561 |
| ’44783_2’ | 0.9333 | ’45533_2’ | 0.9798 | ’45212_2’ | 0.9223 |
| ’44810_2’ | 0.8872 | ’45572_2’ | 0.8721 | ’45227_2’ | 0.8929 |
| ’45049_2’ | 0.9529 | ’45636_2’ | 0.9239 | ’45550_2’ | 0.9355 |
| ’45186_2’ | 0.9373 | ’45641_2’ | 0.9278 | ’45627_2’ | 0.902 |
| ’45311_2’ | 0.9615 | ’46138_2’ | 0.9157 | ’46216_2’ | 0.8924 |
| ’45343_2’ | 0.9688 | ’46297_2’ | 0.8783 | ’46303_2’ | 0.9499 |
| ’45353_2’ | 0.8794 | ’46416_2’ | 0.7969 | ’801_2’ | 0.9454 |
| ’45487_2’ | 0.9774 | ’4679_2’ | 0.849 | ’8141_2’ | 0.9484 |
| ’45556_2’ | 0.9586 | ’6581_2’ | 0.9256 | ’8318_2’ | 0.871 |
| ’45645_2’ | 0.9703 | ’6692_2’ | 0.9332 | ||
| ’46122_2’ | 0.981 | ’7614_2’ | 0.908 | ||
| ’46230_2’ | 0.9661 | ’9124_2’ | 0.9677 | ||
| ’46424_2’ | 0.9086 | ||||
| ’5937_2’ | 0.9206 | ||||
| ’946_2’ | 0.9474 | ||||
| Average | 0.9414 | 0.917 | 0.932 | ||
| Time Domain | NT vs. PHT | NT vs. HT | PHT vs. HT | p-Value (K–W Test) NT vs. PHT vs. HT |
| -value (Wilcoxon Test) | ||||
| r | 0.4466 | 0.4552 | 0.9600 | 0.6726 |
| Frequency domain | -value (Wilcoxon Test) | -value (K–W test) NT vs. PHT vs. HT | ||
| COH & pCOH | 0.2355 | 0.0069 | 0.1630 | 0.0281 |
| PPG → ABP | -value (Wilcoxon Test) | -value (K–W test) NT vs. PHT vs. HT | ||
| PDC | 0.6258 | 0.1861 | 0.4536 | 0.4248 |
| DTF | 0.5324 | 0.2061 | 0.4475 | 0.4219 |
| ffDTF | 0.2527 | 0.2928 | 0.9715 | 0.4352 |
| dDTF | 0.2681 | 0.2973 | 0.9552 | 0.4506 |
| ABP → PPG | -value (Wilcoxon Test) | -value (K–W test) NT vs. PHT vs. HT | ||
| PDC | 0.0264 | 0.0102 | 0.7250 | 0.0188 |
| DTF | 0.1788 | 0.0479 | 0.5995 | 0.1304 |
| ffDTF | 0.0762 | 0.0022 | 0.1128 | 0.0064 |
| dDTF | 0.0718 | 0.0020 | 0.1249 | 0.0061 |
| # | Classifier | COH | PDC | DTF | ffDTF | dDTF | All Features |
|---|---|---|---|---|---|---|---|
| 1.1 | Linear | 66.3% | 51.3% | 53.8% | 65.0% | 62.5% | 70.0% |
| 1.2 | Diaglinear | 66.3% | 51.3% | 53.8% | 65.0% | 62.5% | 70.0% |
| 1.3 | Quadratic | 60.0% | 52.5% | 50.0% | 62.5% | 62.5% | 58.8% |
| 1.4 | Diagquadratic | 60.0% | 52.5% | 50.0% | 62.5% | 62.5% | 65.0% |
| 1.5 | Mahalanobis | 70.0% | 52.5% | 48.8% | 61.3% | 61.3% | 65.0% |
| 1.6 | SVM | 66.3% | 55.0% | 53.7% | 56.2% | 56.2% | 67.5% |
| 1.7 | KNN | 63.8% | 45.0% | 56.2% | 47.5% | 47.5% | 71.3% |
| 1.8 | Tree | 71.3% | 57.5% | 65.0% | 52.5% | 57.5% | 60.0% |
| 1.9 | Naive Bayes | 62.5% | 52.5% | 50.0% | 62.5% | 62.5% | 65.0% |
| 1.10 | Ecoc | 53.7% | 53.7% | 53.7% | 53.7% | 53.7% | 60.0% |
| 1.11 | Esemble | 63.8% | 51.2% | 50.0% | 53.7% | 56.2% | 62.5% |
| 1.12 | Two-layer feed forward Neural Network | 77.5% | 66.3% | 63.7% | 78.8% | 67.5% | 87.5% |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez, G.; Howard, N.; Abbott, D.; Lim, K.; Ward, R.; Elgendi, M. Can Photoplethysmography Replace Arterial Blood Pressure in the Assessment of Blood Pressure? J. Clin. Med. 2018, 7, 316. https://doi.org/10.3390/jcm7100316
Martínez G, Howard N, Abbott D, Lim K, Ward R, Elgendi M. Can Photoplethysmography Replace Arterial Blood Pressure in the Assessment of Blood Pressure? Journal of Clinical Medicine. 2018; 7(10):316. https://doi.org/10.3390/jcm7100316
Chicago/Turabian StyleMartínez, Gloria, Newton Howard, Derek Abbott, Kenneth Lim, Rabab Ward, and Mohamed Elgendi. 2018. "Can Photoplethysmography Replace Arterial Blood Pressure in the Assessment of Blood Pressure?" Journal of Clinical Medicine 7, no. 10: 316. https://doi.org/10.3390/jcm7100316
APA StyleMartínez, G., Howard, N., Abbott, D., Lim, K., Ward, R., & Elgendi, M. (2018). Can Photoplethysmography Replace Arterial Blood Pressure in the Assessment of Blood Pressure? Journal of Clinical Medicine, 7(10), 316. https://doi.org/10.3390/jcm7100316







