Serum Urokinase-Type Plasminogen Activator Receptor Does Not Outperform C-Reactive Protein and Procalcitonin as an Early Marker of Severity of Acute Pancreatitis
Abstract
:1. Introduction
2. Materials and Methods
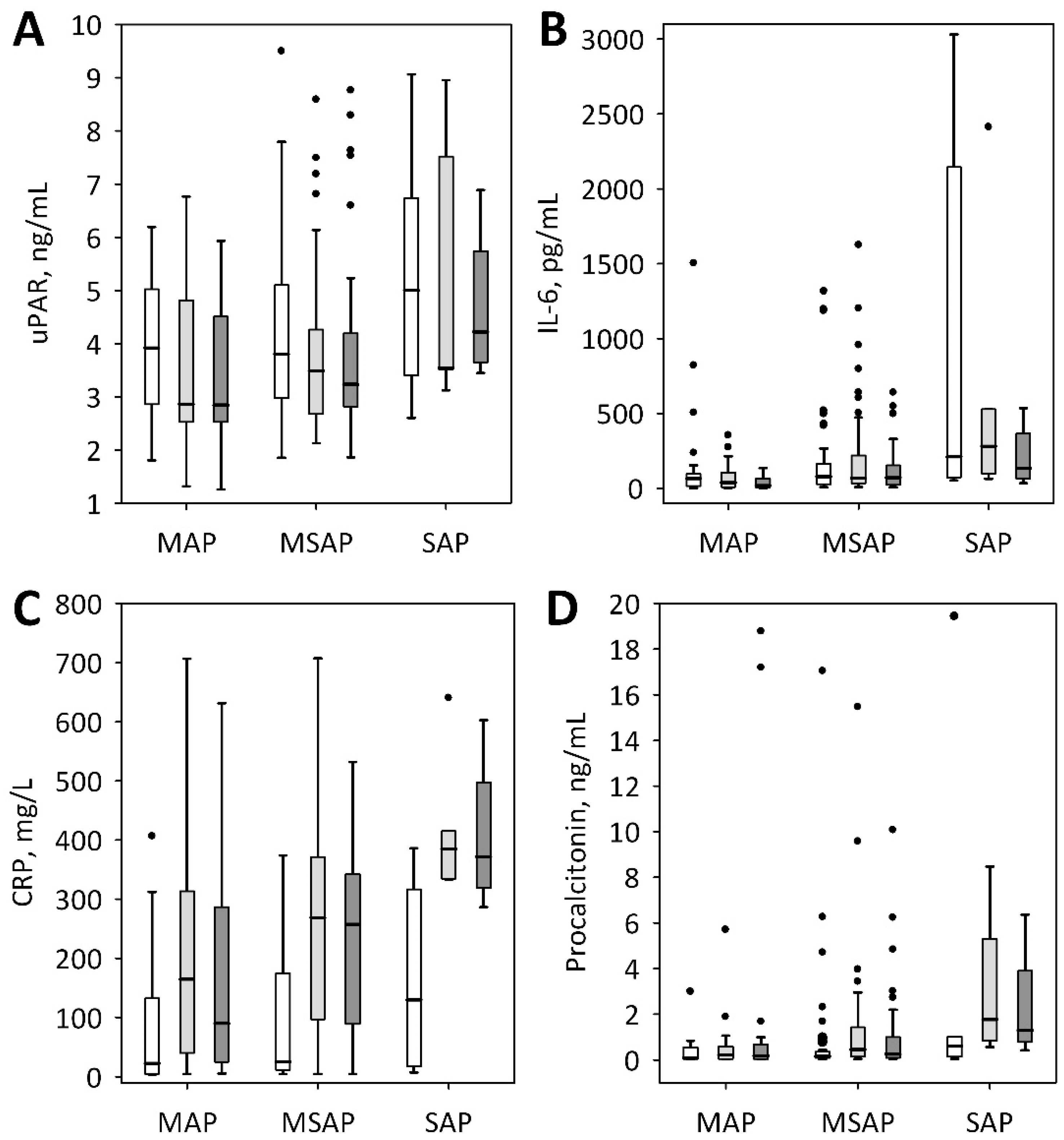
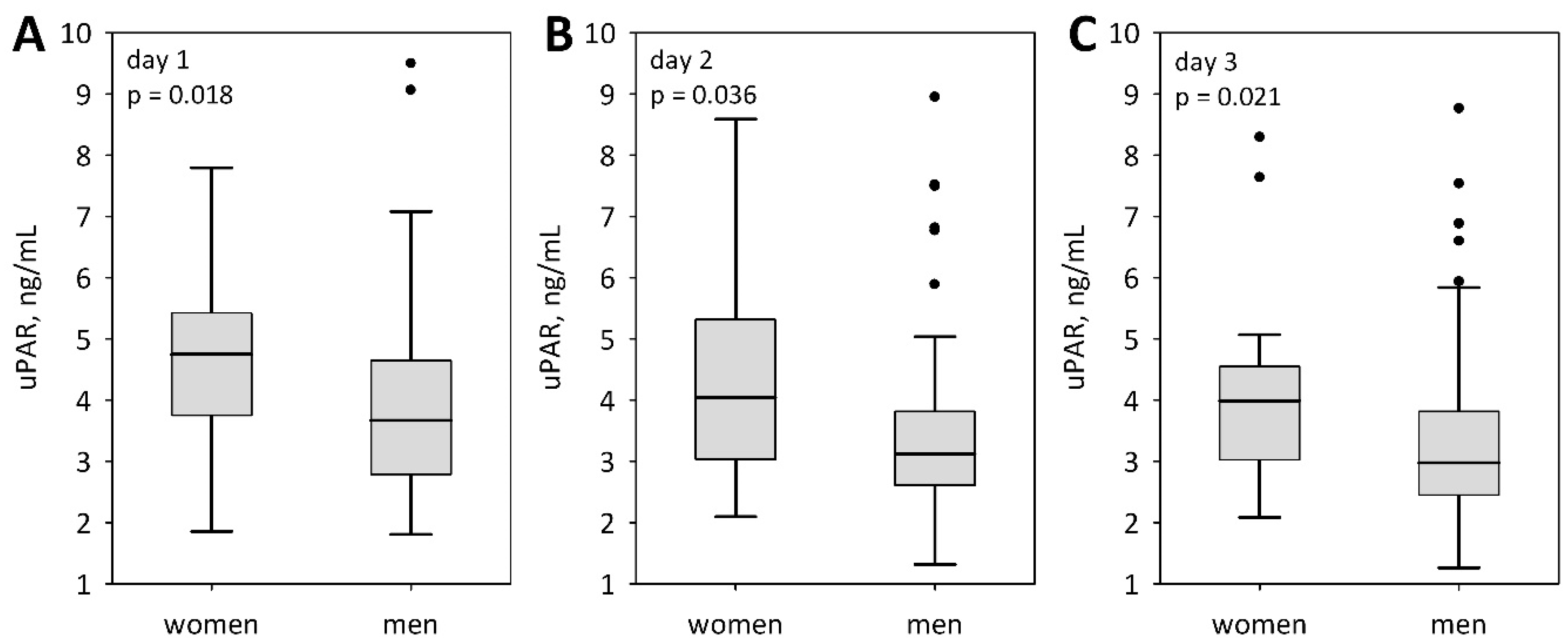
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Laboratory Marker | AUC (95% CI); p-Value * for Prediction of | ||
|---|---|---|---|
| SAP | Organ Failure (MMSS ≥2 Points) | ICU Transfer or Death | |
| IL-6 | 0.753 (0.590–0.917); p = 0.002 | 0.767 (0.578–0.956); p = 0.006 | 0.781 (0.610–0.953); p = 0.001 |
| CRP | 0.647 (0.412–0.882); p = 0.2 | 0.592 (0.373–0.810); p = 0.4 | 0.675 (0.425–0.925); p = 0.2 |
| Procalcitonin | 0.669 (0.378–0.961); p = 0.3 | 0.870 (0.729–1.000); p < 0.001 | 0.844 (0.627–1.000); p = 0.002 |
| D-dimer | 0.605 (0.377–0.901); p = 0.4 | 0.674 (0.485–0.863); p = 0.07 | 0.746 (0.582–0.909); p = 0.003 |
| sFlt-1 | 0.770 (0.546–0.993); p = 0.018 | 0.921 (0.825–1.000); p < 0.001 | 0.758 (0.495–1.000); p = 0.054 |
References
- Baron, T. Managing severe acute pancreatitis. Clevel. Clin. J. Med. 2013, 80, 354–359. [Google Scholar] [CrossRef] [PubMed]
- Párniczky, A.; Kui, B.; Szentesi, A.; Balázs, A.; Szűcs, Á.; Mosztbacher, D.; Czimmer, J.; Sarlós, P.; Bajor, J.; Gódi, S.; et al. Prospective, multicentre, nationwide clinical data from 600 cases of acute pancreatitis. PLoS ONE 2016, 11, e0165309. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.U.; Banks, P. Clinical management of patients with acute pancreatitis. Gastroenterology 2013, 144, 1272–1281. [Google Scholar] [CrossRef] [PubMed]
- Tenner, S.; Baillie, J.; Dewitt, J.; Vege, S.S. American College of Gastroenterology guideline: Management of acute pancreatitis. Am. J. Gastroenterol. 2013, 108, 1400–1415. [Google Scholar] [CrossRef] [PubMed]
- Wereszczyńska-Siemiątkowska, U.; Siemiątkowki, A. Mediators of inflammatory and coagulation processes in acute pancreatitis—Selected issues. Postępy Nauk Med. 2011, 3, 222–231. [Google Scholar]
- Banks, P.A.; Bollen, T.L.; Dervenis, C.; Gooszen, H.G.; Johnson, C.D.; Sarr, M.G.; Tsiotos, G.C.; Vege, S.S. Classification of acute pancreatitis—2012: Revision of the Atlanta classification and definitions by international consensus. Gut 2013, 62, 102–111. [Google Scholar] [CrossRef] [PubMed]
- Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology 2013, 13, e1–e15. [Google Scholar] [CrossRef] [PubMed]
- Swaroop, S.S.; Whitcomb, D.C.; Grover, S. Predicting the Severity of Acute Pancreatitis. UpToDate. Available online: http://www.uptodate.com (accessed on 12 April 2018).
- Naskalski, J.W.; Kusnierz-Cabala, B.; Panek, J.; Kedra, B. Poly-C specific ribonuclease activity correlates with increased concentrations of IL-6, IL-8 and sTNFR55/TNFR75 in plasma of patients with acute pancreatitis. J. Physiol. Pharmacol. 2003, 54, 439–448. [Google Scholar] [PubMed]
- Gurda-Duda, A.; Kusnierz-Cabala, B.; Nowak, W.; Naskalski, J.W.; Kulig, J. Assessment of prognostic value of certain acute phase proteins and procalcitonin in the prognosis of acute pancreatitis. Pancreas 2008, 37, 449–453. [Google Scholar] [CrossRef] [PubMed]
- Kuśnierz-Cabala, B.; Nowak, E.; Sporek, M.; Kowalik, A.; Kuźniewski, M.; Enguita, F.J.; Stępień, E. Serum levels of unique miR-551-5p and endothelial-specific miR-126a-5p allow discrimination of patients in the early phase of acute pancreatitis. Pancreatology 2015, 15, 344–351. [Google Scholar] [CrossRef] [PubMed]
- Spitzer, A.L.; Barcia, A.M.; Schell, M.T.; Barber, A.; Norman, J.; Grendell, J.; Harris, H.W. Applying Ockham’s Razor to pancreatitis prognostication. Ann. Surg. 2006, 243, 380–388. [Google Scholar] [CrossRef] [PubMed]
- Huang, H.L.; Nie, X.; Cai, B.; He, Y.; Miao, Q.; Song, H.L.; Luo, T.X.; Gao, B.X.; Wang, L.L.; Li, G.X. Procalcitonin levels predicts acute kidney injury and prognosis in acute pancreatitis: A prospective study. PLoS ONE 2013, 8, e82250. [Google Scholar] [CrossRef] [PubMed]
- Dumnicka, P.; Maduzia, D.; Ceranowicz, P.; Olszanecki, R.; Drożdż, R.; Kuśnierz-Cabala, B. The interplay between inflammation, coagulation and endothelial injury in the early phase of acute pancreatitis: Clinical implications. Int. J. Mol. Sci. 2017, 18, 354. [Google Scholar] [CrossRef] [PubMed]
- Dumnicka, P.; Sporek, M.; Mazur-Laskowska, M.; Ceranowicz, P.; Kuźniewski, M.; Drożdż, R.; Ambroży, T.; Olszanecki, R.; Kuśnierz-Cabala, B. Serum soluble Fms-like tyrosine kinase 1 (sFlt-1) predicts the severity of acute pancreatitis. Int. J. Mol. Sci. 2017, 17, 2038. [Google Scholar] [CrossRef] [PubMed]
- Dumnicka, P.; Kuśnierz-Cabala, B.; Sporek, M.; Mazur-Laskowska, M.; Gil, K.; Kuźniewski, M.; Ceranowicz, P.; Warzecha, Z.; Dembiński, A.; Bonior, J.; et al. Serum concentrations of Angiopoietin-2 and soluble fms-like tyrosine kinase (sFlt-1) are associated with coagulopathy among patients with acute pancreatitis. Int. J. Mol. Sci. 2017, 18, 753. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.; Long, D.; Yu, L.; Yang, J.H.; Zhang, Y.C.; Geng, F. Urokinase-type plasminogen activator receptor as a predictor of poor outcome in patients with systemic inflammatory response syndrome. World J. Emerg. Med. 2013, 4, 190–195. [Google Scholar] [CrossRef] [PubMed]
- Iba, T.; Gando, S.; Murata, A.; Kushimoto, S.; Saitoh, D.; Eguchi, Y.; Ohtomo, Y.; Okamoto, K.; Koseki, K.; Mayumi, T.; et al. Predicting the severity of Systemic Inflammatory Response Syndrome (SIRS)–associated coagulopathy with hemostatic molecular markers and vascular endothelial injury markers. J. Trauma 2007, 63, 1093–1098. [Google Scholar] [CrossRef] [PubMed]
- Friess, H.; Duarte, R.; Kleeff, J.; Fukuda, A.; Tang, W.H.; Graber, H.; Schilling, M.; Zimmermann, A.; Korc, M.; Büchler, M.W. The plasminogen activator/plasmin system is up-regulated after acute necrotizing pancreatitis in human beings. Surgery 1998, 124, 79–86. [Google Scholar] [CrossRef]
- Koch, A.; Voigt, S.; Kruschinski, C.; Sanson, E.; Duckers, H.; Horn, A.; Yagmur, E.; Zimmermann, H.; Trautwein, C.; Tacke, F. Circulating soluble urokinase plasminogen activator receptor is stably elevated during the first week of treatment in the intensive care unit and predicts mortality in critically ill patients. Crit. Care 2011, 15, R63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Backes, Y.; Sluijs, K.F.; Mackie, D.P.; Tacke, F.; Koch, A.; Teuhunen, J.J.; Schultz, M.J. Usefulness of suPAR as a biological marker in patients with systemic inflammation or infection: A systemic review. Intensive Care Med. 2012, 38, 1418–1428. [Google Scholar] [CrossRef] [PubMed]
- Donadello, K.; Scalletta, S.; Covajes, C.; Vincent, J.L. suPAR as a prognostic biomarker in sepsis. BMC Med. 2012, 10, 2. [Google Scholar] [CrossRef] [PubMed]
- Thunø, M.; Macho, B.; Eugen-Olsen, J. suPAR: The molecular crystal ball. Dis. Mark. 2009, 27, 157–172. [Google Scholar] [CrossRef]
- Yu, L.; Long, D.; Wu, X.L.; Yang, J.H.; Yang, Y.C.; Feng, G. Prognostic significance of urokinase-type plasminogen activator and its receptor in patients with systemic inflammatory response syndrome. World J. Emerg. Med. 2011, 2, 185–189. [Google Scholar] [CrossRef] [PubMed]
- Seppala, U.; Huttunen, R.; Tarkka, M.; Aittoniemi, J.; Koskinen, J.; Leino, A.; Vahlberg, T.; Rintala, E.M. Soluble urokinase–type plasminogen activator in patients with suspected infection in the emergency room: A prospective cohort study. J. Intern. Med. 2012, 272, 247–256. [Google Scholar] [CrossRef] [PubMed]
- Lipinski, M.; Rydzewska-Rosołowska, A.; Rydzewski, A.; Cicha, M. Rydzewska G: Soluble urokinase-type activator receptor (suPAR) patients with acute pancreatitis (AP)–Progress in prediction of AP severity. Pancreatology 2017, 17, 24–29. [Google Scholar] [CrossRef] [PubMed]
- Kellum, J.A.; Lameire, N.; Aspelin, P.; Barsoum, R.S.; Burdmann, E.A.; Goldstein, S.L.; Herzog, C.A.; Joannidis, M.; Kribben, A.; Levey, A.S.; et al. Kidney Disease: Improving Global Outcomes (KDIGO) Acute Kidney Injury Work Group. KDIGO clinical practice guideline for acute kidney injury. Kidney Int. Suppl. 2012, 2, 1–138. [Google Scholar]
- ARDS Definition Task Force; Ranieri, V.M.; Rubenfeld, G.D.; Thompson, B.T.; Ferguson, N.D.; Caldwell, E.; Fan, E.; Camporota, L.; Slutsky, A.S. Acute respiratory distress syndrome: The Berlin Definition. JAMA 2012, 307, 2526–2533. [Google Scholar] [PubMed]
- Kofoed, K.; Eugen-Olsen, J.; Petersen, J.; Larsen, K.; Anderson, O. Predicting mortality in patients with systemic inflammatory response syndrome: An evaluation of two prognostic models, two soluble receptors, and a macrophage migration inhibitory factor. Eur. J. Clin. Microbiol. Infect. Dis. 2008, 27, 375–383. [Google Scholar] [CrossRef] [PubMed]
- Raggam, R.B.; Wagner, J.; Prüller, F.; Grisold, A.; Leitner, E.; Zollner-Schwetz, I.; Valentin, T.; Krause, R.; Hoenigl, M. Soluble urokinase plasminogen activator receptor predicts mortality in patients with systemic inflammatory response syndrome. J. Intern. Med. 2014, 276, 651–658. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Botha, S.; Fourie, C.M.; Schutte, R.; Eugen-Olsen, J.; Schutte, A.E. Soluble urokinase plasminogen activator receptor as a prognostic marker of all-cause and cardiovascular mortality in black population. Int. J. Cardiol. 2015, 184, 631–636. [Google Scholar] [CrossRef] [PubMed]
- Koller, L.; Stojkovic, S.; Richter, B.; Sulzgruber, P.; Potolidis, C.; Liebhart, F.; Mörtl, D.; Berger, R.; Goliasch, G.; Wojta, J.; et al. Soluble urokinase-type plasminogen activator receptor improves risk prediction in patients with chronic heart failure. JACC Heart Fail. 2017, 5, 268–277. [Google Scholar] [CrossRef] [PubMed]
- Lyngbæk, S.; Andersson, C.; Marott, J.L.; Møller, D.V.; Christiansen, M.; Iversen, K.K.; Clemmensen, P.; Eugen-Olsen, J.; Hansen, P.R.; Jeppesen, J.L. Soluble urokinase plasminogen activator receptor for risk prediction in patients admitted with acute chest pain. Clin. Chem. 2013, 59, 1621–1629. [Google Scholar] [CrossRef] [PubMed]
- Geboers, D.; de Beer, F.; Tuip-de Boer, A.; van der Poll, T.; Horn, J.; Cremer, O.; Bonten, M.J.; Ong, D.S.; Schultz, M.J.; Bos, L.D. Plasma suPAR as a prognostic biological marker for ICU mortality in ARDS patients. Int. Care Med. 2015, 41, 1281–1290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Giamarellos-Bourboulis, E.J.; Norrby-Teglund, A.; Mylona, V.; Savva, A.; Tsangaris, I.; Dimopoulou, I.; Mouktaroudi, M.; Raftogiannis, M.; Georgitsi, M.; Linnér, A.; et al. Risk assessment in sepsis: A new prognostication rule by APACHE II score and serum soluble urokinase plasminogen activator receptor. Crit. Care 2012, 16, R149. [Google Scholar] [CrossRef] [PubMed]
- Nikkola, A.; Aittoniemi, J.; Huttunen, R.; Rajala, L.; Nordback, I.; Sand, J.; Laukkarinen, J. Plasma level of soluble urokinase-type plasminogen activator receptor predicts the severity of acute alcohol pancreatitis. Pancreas 2017, 46, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, H.W.; Koch, A.; Seidler, S.; Trautwein, C.; Tacke, F. Circulating soluble urokinase plasminogen activator is elevated in patients with chronic liver disease, discriminates stage and aetiology of cirrhosis and predicts prognosis. Liver Int. 2011, 32, 500–509. [Google Scholar] [CrossRef] [PubMed]
- Wei, C.; Trachtman, H.; Li, J.; Dong, C.; Friedman, A.L.; Gassman, J.J.; McMahan, J.L.; Radeva, M.; Heil, K.M.; Trautmann, A.; et al. Circulating suPAR in two cohorts of primary FSGS. J. Am. Soc. Nephrol. 2012, 23, 2051–2059. [Google Scholar] [CrossRef] [PubMed]
- Lyngbæk, S.; Marott, J.L.; Møller, D.V.; Christiansen, M.; Iversen, K.K.; Clemmensen, P.M.; Eugen-Olsen, J.; Jeppesen, J.L.; Hansen, P.R. Usefulness of soluble urokinase plasminogen activator receptor to predict repeat myocardial infarction and mortality in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous intervention. Am. J. Cardiol. 2012, 110, 1756–1763. [Google Scholar] [CrossRef] [PubMed]

| Characteristic | MAP (n = 29) | MSAP (n = 58) | SAP (n = 8) | p-Value |
|---|---|---|---|---|
| Male sex, n (%) | 17 (59) | 41 (71) | 7 (88) | 0.2 |
| Mean age (SD), years | 43 (16) | 50 (16) | 51 (20) | 0.1 |
| Pre-existing comorbidities, n (%) | 10 (34) | 27 (47) | 5 (62) | 0.3 |
| Cardiac diseases, n (%) | 5 (17) | 20 (34) | 5 (62) | |
| Diabetes, n (%) | 0 | 6 (10) | 2 (25) | |
| Dyslipidemia, n (%) | 1 (3) | 2 (3) | 0 | |
| Chronic kidney disease, n (%) | 0 | 2 (3) | 0 | |
| Liver disease, n (%) | 1 (3) | 2 (3) | 0 | |
| Other comorbidities, n (%) | 3 (10) | 0 | 0 | |
| Etiology | 0.1 | |||
| Biliary, n (%) | 9 (31) | 17 (29) | 1 (12) | |
| Alcoholic, n (%) | 12 (41) | 11 (19) | 6 (75) | |
| Hipertriglyceridemia, n (%) | 1 (3) | 4 (7) | 0 | |
| Other/idiopathic, n (%) | 7 (24) | 26 (45) | 1 (12) | |
| Median Ranson score (Q1; Q3), points | 2 (1; 3) | 3 (3; 4) | 6 (4; 7) | <0.001 a,b,c |
| Median duration of hospital stay(Q1; Q3), days | 10 (7; 12) | 14 (10; 16) | 26 (13; 41) | 0.001 a,c |
| SIRS in first 24 h, n (%) | 18 (62) | 49 (84) | 7 (88) | 0.047 c |
| Early/late mortality, n (%) | 0 | 0/2 (3) | 1 (12)/1 (12) | 0.006 a,b |
| Therapeutic ERCP, n (%) | 0 | 3 (5) | 2 (25) | 0.020 a,b |
| Surgery, n (%) | 0 | 3 (5) | 4 (50) | <0.001 a,b |
| Enteral feeding via nasojejunal tube, n (%) | 0 | 4 (7) | 6 (75) | <0.001 a,b |
| Parenteral feeding, n (%) | 0 | 1 (2) | 2 (25) | 0.001 a,b |
| Transfer to ICU, n (%) | 0 | 2 (3) | 5 (62) | <0.001 a,b |
| Variable | MAP (n = 29) | MSAP (n = 58) | SAP (n = 8) | p-Value |
|---|---|---|---|---|
| Hematocrit, % | 42 (5) | 43 (6) | 46 (7) | 0.4 |
| Albumin, g/L | 38 (7) | 35 (6) | 36 (8) | 0.6 |
| Total calcium, mmol/L | 2.13 (0.23) | 2.15 (0.19) | 1.92 (0.48) | 0.5 |
| Glucose, mmol/L | 6.44 (5.61; 7.67) | 8.17 (6.78; 9.33) | 7.92 (7.22; 10.64) | 0.002 a,c |
| Urea, mmol/L | 3.67 (2.83; 6.00) | 4.67 (3.50; 6.00) | 6.67 (5.00; 13.00) | 0.015 a |
| Creatinine, µmol/L | 65.4 (59.2; 80.4) | 69.8 (60.1; 87.5) | 92.4 (75.6; 171.1) | 0.033 a |
| Bilirubin, µmol/L | 23.4 (13.5; 38.5) | 27.2 (13.8; 53.3) | 29.1 (16.2; 36.9) | 0.7 |
| AST, U/L | 59 (33; 209) | 116 (55; 202) | 122 (87; 166) | 0.3 |
| ALT, U/L | 62 (43; 174) | 133 (54; 299) | 85 (49; 158) | 0.3 |
| LDH, U/L | 553 (488; 810) | 636 (507; 850) | 1013 (737; 1294) | 0.1 |
| WBC, ×103/µL | 12.4 (9.5; 15.2) | 13.1 (10.4; 16.2) | 17.1 (10.3; 23.3) | 0.4 |
| Platelet count, ×103/µL | 199 (176; 231) | 218 (165; 279) | 227 (162; 292) | 0.8 |
| CRP, mg/L | 22.7 (5.3; 132.4) | 25.4 (11.9; 174.7) | 129.6 (17.4; 316.7) | 0.4 |
| D-dimer, mg/L | 1.49 (0.85; 2.19) | 1.90 (1.00; 3.41) | 2.76 (1.20; 3.39) | 0.2 |
| Procalcitonin, ng/mL | 0.10 (0.05; 0.55) | 0.17 (0.10; 0.36) | 0.61 (0.14; 1.03) | 0.1 |
| uPAR, ng/mL | 3.92 (2.86; 5.02) | 3.81 (2.98; 5.10) | 5.00 (3.41; 6.74) | 0.4 |
| Interleukin 6, pg/mL | 64.7 (14.8; 95.7) | 78.9 (27.8; 163.0) | 210.7 (73.1; 21.5) | 0.037 a |
| sFlt-1, pg/mL | 129 (119; 169) | 140 (112; 154) | 191 (155; 536) | 0.1 |
| Dependent Variable | uPAR on Admission, per 1 ng/mL | Maximum uPAR, per 1 ng/mL |
|---|---|---|
| SAP (2012 Atlanta) | 1.41 (0.92–2.17); p = 0.1 | 1.49 (0.94–2.37); p = 0.08 |
| MSAP plus SAP (2012 Atlanta) | 1.16 (0.84–1.60); p = 0.4 | 1.16 (0.86–1.58); p = 0.3 |
| Persistent (≥48 h) SIRS | 0.92 (0.69–1.22); p = 0.5 | 0.90 (0.69–1.18); p = 0.4 |
| Ranson ≥ 3 points at 48 h | 1.39 (1.01–1.89); p = 0.038 | 1.28 (0.96–1.71); p = 0.08 |
| Organ failure (MMSS ≥ 2 points) | 2.14 (1.33–3.46); p = 0.002 | 2.06 (1.30–3.26); p = 0.002 |
| Cardiovascular failure | 2.33 (1.34–4.08); p = 0.002 | 2.41 (1.29–4.50); p = 0.005 |
| ARDS | 1.01 (0.59–1.72); p = 0.9 | 1.19 (0.73–1.94); p = 0.5 |
| AKI | 1.78 (1.11–2.84); p = 0.015 | 1.77 (1.10–2.85); p = 0.017 |
| ICU transfer | 2.06 (1.24–3.43); p = 0.005 | 2.35 (1.27–4.35); p = 0.005 |
| Death | 1.82 (1.06–3.12); p = 0.027 | 2.25 (1.15–4.37); p = 0.015 |
| Dependent Variable | AUC (95% CI) | p * | Cut-Off Value, ng/mL | Sensitivity, % | Specificity, % |
|---|---|---|---|---|---|
| SAP | 0.641 (0.417–0.864) | 0.2 | 5.004 | 57 | 75 |
| Organ failure (MMSS ≥2 points) | 0.761 (0.565–0.958) | 0.009 | 6.736 | 56 | 97 |
| ICU transfer or death | 0.759 (0.536–0.983) | 0.023 | 6.021 | 57 | 92 |
| Variable | Day 1 | Day 2 | Day 3 | |||
|---|---|---|---|---|---|---|
| R | p | R | p | R | p | |
| Hematocrit | −0.11 | 0.3 | −0.31 | 0.006 | −0.27 | 0.022 |
| Albumin | −0.32 | 0.014 | −0.54 | <0.001 | −0.44 | <0.001 |
| Urea | 0.16 | 0.2 | 0.10 | 0.4 | −0.04 | 0.8 |
| Creatinine | 0.18 | 0.1 | 0.05 | 0.7 | −0.05 | 0.7 |
| Bilirubin | 0.34 | 0.003 | 0.39 | <0.001 | 0.41 | <0.001 |
| AST | 0.49 | <0.001 | 0.53 | <0.001 | 0.39 | 0.001 |
| ALT | 0.37 | 0.001 | 0.37 | 0.001 | 0.30 | 0.009 |
| LDH | 0.46 | <0.001 | 0.28 | 0.026 | 0.52 | <0.001 |
| WBC | −0.03 | 0.8 | −0.03 | 0.8 | 0.19 | 0.09 |
| CRP | 0.19 | 0.1 | 0.29 | 0.012 | 0.42 | <0.001 |
| D-dimer | 0.26 | 0.030 | 0.19 | 0.09 | 0.30 | 0.010 |
| Procalcitonin | 0.57 | <0.001 | 0.54 | <0.001 | 0.61 | <0.001 |
| Interleukin 6 | 0.25 | 0.027 | 0.35 | 0.002 | 0.54 | <0.001 |
| sFlt-1 | 0.48 | <0.001 | 0.02 | 0.9 | - | - |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kolber, W.; Kuśnierz-Cabala, B.; Dumnicka, P.; Maraj, M.; Mazur-Laskowska, M.; Pędziwiatr, M.; Ceranowicz, P. Serum Urokinase-Type Plasminogen Activator Receptor Does Not Outperform C-Reactive Protein and Procalcitonin as an Early Marker of Severity of Acute Pancreatitis. J. Clin. Med. 2018, 7, 305. https://doi.org/10.3390/jcm7100305
Kolber W, Kuśnierz-Cabala B, Dumnicka P, Maraj M, Mazur-Laskowska M, Pędziwiatr M, Ceranowicz P. Serum Urokinase-Type Plasminogen Activator Receptor Does Not Outperform C-Reactive Protein and Procalcitonin as an Early Marker of Severity of Acute Pancreatitis. Journal of Clinical Medicine. 2018; 7(10):305. https://doi.org/10.3390/jcm7100305
Chicago/Turabian StyleKolber, Witold, Beata Kuśnierz-Cabala, Paulina Dumnicka, Małgorzata Maraj, Małgorzata Mazur-Laskowska, Michał Pędziwiatr, and Piotr Ceranowicz. 2018. "Serum Urokinase-Type Plasminogen Activator Receptor Does Not Outperform C-Reactive Protein and Procalcitonin as an Early Marker of Severity of Acute Pancreatitis" Journal of Clinical Medicine 7, no. 10: 305. https://doi.org/10.3390/jcm7100305
APA StyleKolber, W., Kuśnierz-Cabala, B., Dumnicka, P., Maraj, M., Mazur-Laskowska, M., Pędziwiatr, M., & Ceranowicz, P. (2018). Serum Urokinase-Type Plasminogen Activator Receptor Does Not Outperform C-Reactive Protein and Procalcitonin as an Early Marker of Severity of Acute Pancreatitis. Journal of Clinical Medicine, 7(10), 305. https://doi.org/10.3390/jcm7100305








