Sleeve Gastrectomy Leads to Immediate, Significant Intraoperative Increase in Lower Esophageal Distensibility and Opening Area
Abstract
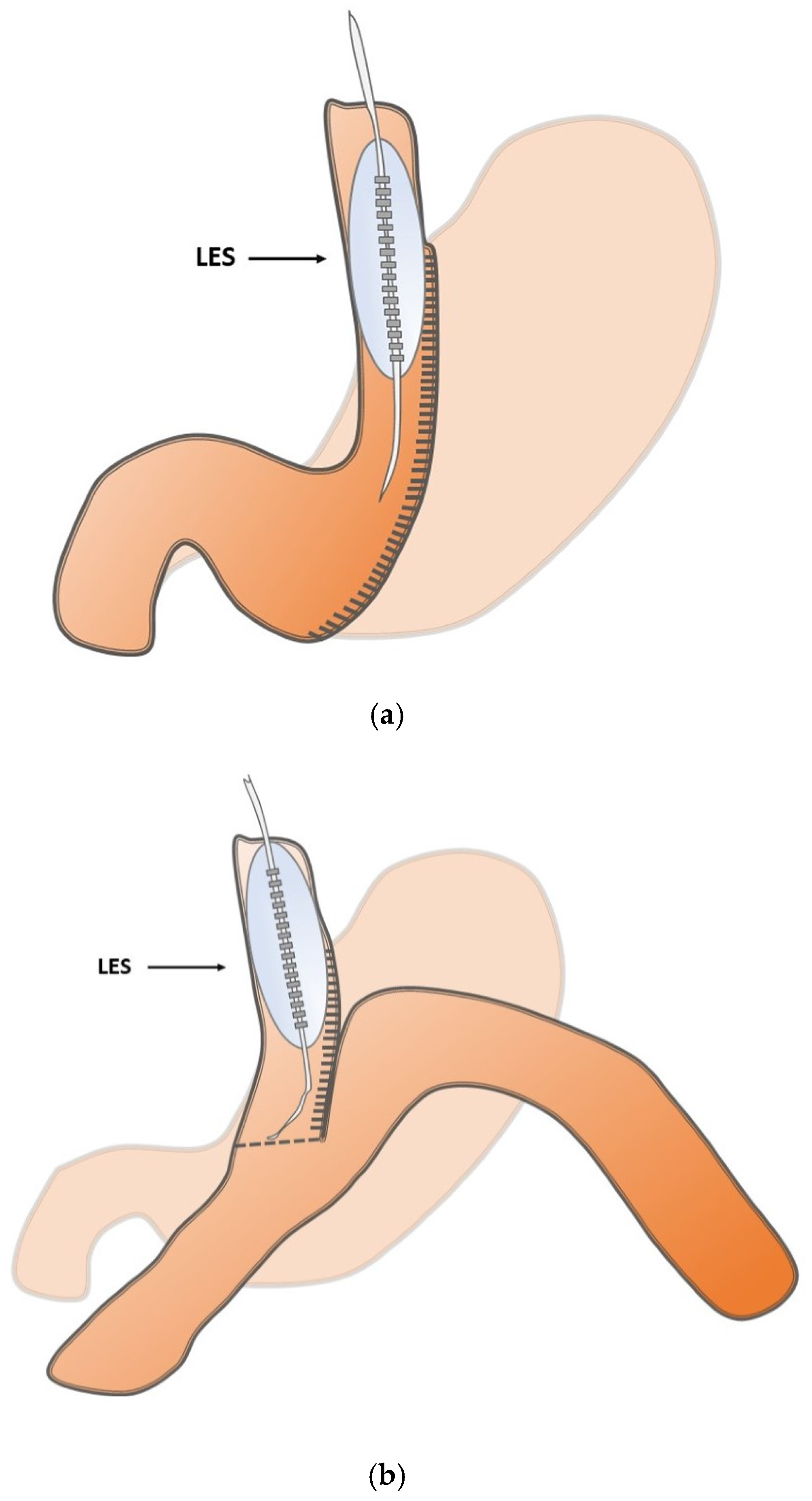
1. Introduction
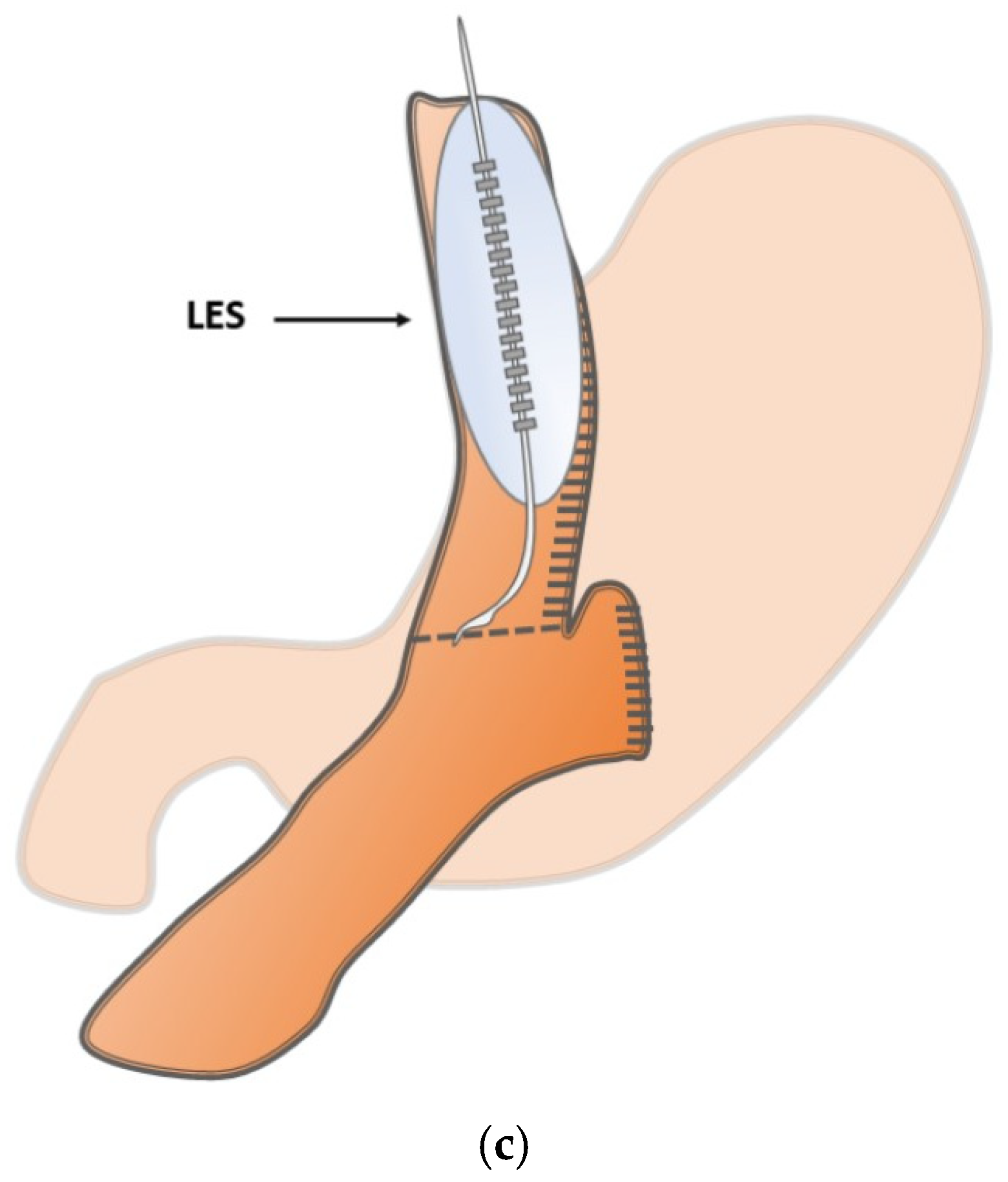
2. Materials and Methods
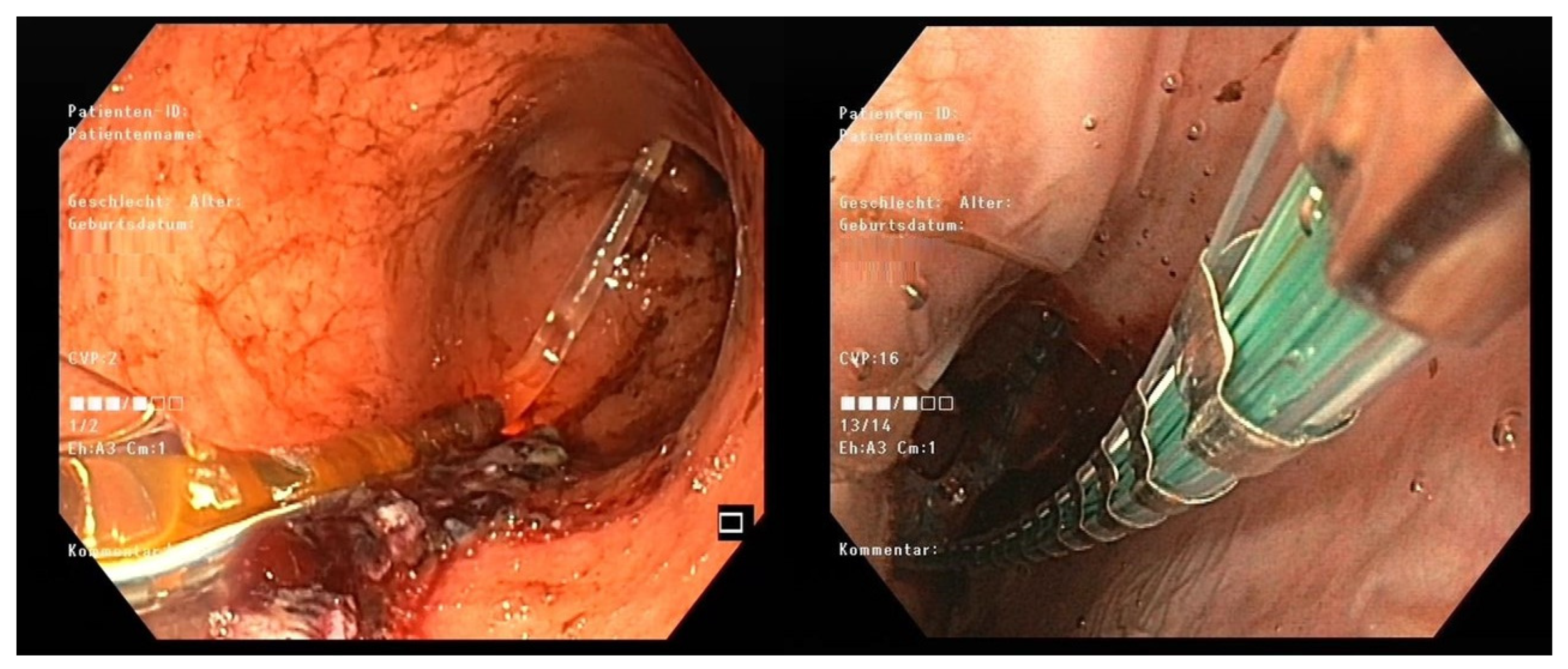
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ASA | American Society of Anesthesiologists |
| BMI | Body mass index |
| CSA | Cross-sectional area |
| DI | Distensibility index |
| Dmin | Minimal diameter |
| GB | Gastric bypass |
| IBP | Intra-balloon pressure |
| LES | Lower esophageal sphincter |
| MBS | Metabolic baria |
| OAGB | One-anastomosis gastric bypass |
| RYGB | Roux-en-Y gastric bypass |
| SG | Sleeve gastrectomy |
| UGIT | Upper gastrointestinal tract |
References
- Bredenoord, A.J.; Pandolfino, J.E.; Smout, A.J. Gastro-oesophageal reflux disease. Lancet 2013, 381, 1933–1942. [Google Scholar] [CrossRef]
- Yamasaki, T.; Hemond, C.; Eisa, M.; Ganocy, S.; Fass, R. The Changing Epidemiology of Gastroesophageal Reflux Disease: Are Patients Getting Younger? J. Neurogastroenterol. Motil. 2018, 24, 559–569. [Google Scholar] [CrossRef]
- O’Neill, O.M.; Johnston, B.T.; Coleman, H.G. Achalasia: A review of clinical diagnosis, epidemiology, treatment and outcomes. World J. Gastroenterol. 2013, 19, 5806–5812. [Google Scholar] [CrossRef] [PubMed]
- Muir, A.; Falk, G.W. Eosinophilic Esophagitis: A Review. JAMA 2021, 326, 1310–1318. [Google Scholar] [CrossRef]
- Emerenziani, S.; Guarino, M.P.L.; Trillo Asensio, L.M.; Altomare, A.; Ribolsi, M.; Balestrieri, P.; Cicala, M. Role of Overweight and Obesity in Gastrointestinal Disease. Nutrients 2019, 12, 111. [Google Scholar] [CrossRef]
- Iannelli, A.; Treacy, P.; Sebastianelli, L.; Martini, F.; Schiavo, L. Perioperative complications of sleeve gastrectomy: Review of the literature. J. Minim. Access Surg. 2019, 15, 1–7. [Google Scholar]
- Aleman, R.; Lo Menzo, E.; Szomstein, S.; Rosenthal, R.J. Efficiency and risks of one-anastomosis gastric bypass. Ann. Transl. Med. 2020, 8, S7. [Google Scholar] [CrossRef]
- Jedamzik, J.; Bichler, C.; Felsenreich, D.M.; Gensthaler, L.; Eichelter, J.; Nixdorf, L.; Krebs, M.; Langer, F.B.; Prager, G. Conversion from one-anastomosis gastric bypass to Roux-en-Y gastric bypass: When and why-a single-center experience of all consecutive OAGB procedures. Surg. Obes. Relat. Dis. 2022, 18, 225–232. [Google Scholar] [CrossRef]
- Cucchi, S.G.; Pories, W.J.; MacDonald, K.G.; Morgan, E.J. Gastrogastric fistulas. A complication of divided gastric bypass surgery. Ann. Surg. 1995, 221, 387–391. [Google Scholar] [CrossRef] [PubMed]
- Ramos, A.C.; Marchesini, J.C.; de Souza Bastos, E.L.; Ramos, M.G.; de Souza, M.D.G.; Campos, J.M.; Ferraz, A.B. The Role of Gastrojejunostomy Size on Gastric Bypass Weight Loss. Obes. Surg. 2017, 27, 2317–2323. [Google Scholar] [CrossRef] [PubMed]
- Pandolfino, J.E.; de Ruigh, A.; Nicodème, F.; Xiao, Y.; Boris, L.; Kahrilas, P.J. Distensibility of the esophagogastric junction assessed with the functional lumen imaging probe (FLIP™) in achalasia patients. Neurogastroenterol. Motil. 2013, 25, 496–501. [Google Scholar] [CrossRef]
- Carlson, D.A. Functional lumen imaging probe: The FLIP side of esophageal disease. Curr. Opin. Gastroenterol. 2016, 32, 310–318. [Google Scholar] [CrossRef]
- Desprez, C.; Roman, S.; Leroi, A.M.; Gourcerol, G. The use of impedance planimetry (Endoscopic Functional Lumen Imaging Probe, EndoFLIP®) in the gastrointestinal tract: A systematic review. Neurogastroenterol. Motil. 2020, 32, e13980. [Google Scholar] [CrossRef]
- Carlson, D.A.; Kou, W.; Lin, Z.; Hinchcliff, M.; Thakrar, A.; Falmagne, S.; Prescott, J.; Dorian, E.; Kahrilas, P.J.; Pandolfino, J.E. Normal Values of Esophageal Distensibility and Distension-Induced Contractility Measured by Functional Luminal Imaging Probe Panometry. Clin. Gastroenterol. Hepatol. 2019, 17, 674–681. [Google Scholar] [CrossRef] [PubMed]
- Bredenoord, A.J.; Rancati, F.; Lin Haiying, L.; Schwartz, N.; Argov, M. Normative values for esophageal functional lumen imaging probe measurements: A meta-analysis. Neurogastroenterol. Motil. 2022, 34, e14419. [Google Scholar] [CrossRef] [PubMed]
- Su, B.; Attaar, M.; Wong, H.; Callahan, Z.M.; Kuchta, K.; Stearns, S.; Linn, J.G.; Denham, W.; Haggerty, S.P.; Ujiki, M.B. Using a standardized intra-operative endoflip protocol during fundoplication to identify factors that affect distensibility. Surg. Endosc. 2021, 35, 5717–5723. [Google Scholar] [CrossRef] [PubMed]
- Ahuja, N.K.; Agnihotri, A.; Lynch, K.L.; Hoo-Fatt, D.; Onyimba, F.; McKnight, M.; Okeke, F.C.; Garcia, P.; Dhalla, S.; Stein, E.; et al. Esophageal distensibility measurement: Impact on clinical management and procedure length. Dis. Esophagus 2017, 30, 1–8. [Google Scholar] [CrossRef]
- Haq, Z.; Itani, M.I.; Zhang, L.; Dinary, F.; Farha, J.; Abbarh, S.; Akshintala, V.; Koller, K.; Jovani, M.; Hedjoudje, A.; et al. The Utility of EndoFLIP for Measuring Gastrojejunal Anastomosis Diameter and Distensibility in Patients Experiencing Weight Regain Post Roux-en-Y Gastric Bypass. Obes. Surg. 2021, 31, 3353–3359. [Google Scholar] [CrossRef]
- Yu, J.X.; Evans, G.; Volk, S.; Watts, L.; Schulman, A.R. Endoscopic severity of gastric sleeve stenosis can be quantified using impedance planimetry. Surg. Endosc. 2023, 37, 5969–5974. [Google Scholar] [CrossRef]
- Razzak, F.A.; Kerbage, A.; Brunaldi, V.O.; Mrad, R.; Mahmoud, T.; Gala, K.; Vargas, E.J.; Storm, A.; Ghanem, O.; Abu Dayyeh, B. Correlation Between Gastrojejunal Anastomosis Diameter, Distensibility Index, and Weight Regain After Roux-en-Y Gastric Bypass. Obes. Surg. 2023, 33, 4042–4048. [Google Scholar] [CrossRef]
- Su, B.; Novak, S.; Callahan, Z.M.; Kuchta, K.; Carbray, J.; Ujiki, M.B. Using impedance planimetry (EndoFLIP™) in the operating room to assess gastroesophageal junction distensibility and predict patient outcomes following fundoplication. Surg. Endosc. 2020, 34, 1761–1768. [Google Scholar] [CrossRef]
- Reynolds, J.L.; Zehetner, J.; Shiraga, S.; Lipham, J.C.; Katkhouda, N. Intraoperative assessment of the effects of laparoscopic sleeve gastrectomy on the distensibility of the lower esophageal sphincter using impedance planimetry. Surg. Endosc. 2016, 30, 4904–4909. [Google Scholar] [CrossRef]
- Magyar, C.T.J.; Borbély, Y.; Wiest, R.; Stirnimann, G.; Candinas, D.; Lenglinger, J.; Nett, P.C.; Kröll, D. Gastroesophageal Junction and Pylorus Distensibility Before and After Sleeve Gastrectomy-pilot Study with EndoFlipTM. Obes. Surg. 2023, 33, 2255–2260. [Google Scholar] [CrossRef] [PubMed]
- Pavone, G.; Tartaglia, N.; Porfido, A.; Panzera, P.; Pacilli, M.; Ambrosi, A. The new onset of GERD after sleeve gastrectomy: A systematic review. Ann. Med. Surg. 2022, 77, 103584. [Google Scholar] [CrossRef] [PubMed]
- Genco, A.; Soricelli, E.; Casella, G.; Maselli, R.; Castagneto-Gissey, L.; Di Lorenzo, N.; Basso, N. Gastroesophageal reflux disease and Barrett’s esophagus after laparoscopic sleeve gastrectomy: A possible, underestimated long-term complication. Surg. Obes. Relat. Dis. 2017, 13, 568–574. [Google Scholar] [CrossRef]
- Huynh, D.; Mazer, L.; Tung, R.; Cunneen, S.; Shouhed, D.; Burch, M. Conversion of laparoscopic sleeve gastrectomy to Roux-en-Y gastric bypass: Patterns predicting persistent symptoms after revision. Surg. Obes. Relat. Dis. 2021, 17, 1681–16881. [Google Scholar] [CrossRef] [PubMed]
| Patient Demographics | |
|---|---|
| Patients (n) | 40 |
| Female | 31 |
| Male | 9 |
| Age (years) | 40 (23–65) |
| BMI (kg/m2) | 45.2 (35–68) |
| ASA classification | 3 (2–3) |
| Comorbidities | |
| Diabetes mellitus | 7 (18) |
| Obstructive sleep apnea | 12 (30) |
| Bronchial asthma | 3 (7.5) |
| NAFLD | 2 (5) |
| Procedure n (%) | |
| Sleeve gastrectomy | 17 (42) |
| OAGB | 15 (38) |
| RYGB | 8 (20) |
| Hospital stay after surgery (days) | 5 (4–16) |
| EndoFLIPTM-related adverse events n (%) | 0 (0) |
| LES Measurements | Before | After | 95% CI | p-Value |
|---|---|---|---|---|
| Dmin | 12.0 (±1.2) | 13.9 (±2.8) | −3.6 to −0.2 | 0.028 |
| DI | 2.1 (±0.5) | 2.9 (±1.3) | −1.6 to −0.14 | 0.023 |
| IBP | 56.3 (±7.6) | 55.6 (±12.1) | −8.0 to 9.4 | 0.863 |
| CSA | 109.6 (±28.1) | 157.8 (±56.0) | −84.2 to −12.3 | 0.011 |
| LES Measurements | Before | After | 95% CI | p-Value |
|---|---|---|---|---|
| Dmin | 14.1 (±3.6) | 15.4 (±2.6) | −4.5 to 1.9 | 0.389 |
| DI | 4.0 (±2.0) | 4.0 (±2.0) | −1.8 to 1.8 | 0.988 |
| IBP | 46.7 (±12.6) | 51.0 (±12.2) | −15.6 to 7.0 | 0.425 |
| CSA | 166.8 (±73.3) | 191.4 (±65.4) | −89.8 to 40.5 | 0.422 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
de Cillia, M.; Mittermair, C.; Hoi, H.; Grünbart, M.; Weiss, H. Sleeve Gastrectomy Leads to Immediate, Significant Intraoperative Increase in Lower Esophageal Distensibility and Opening Area. J. Clin. Med. 2026, 15, 701. https://doi.org/10.3390/jcm15020701
de Cillia M, Mittermair C, Hoi H, Grünbart M, Weiss H. Sleeve Gastrectomy Leads to Immediate, Significant Intraoperative Increase in Lower Esophageal Distensibility and Opening Area. Journal of Clinical Medicine. 2026; 15(2):701. https://doi.org/10.3390/jcm15020701
Chicago/Turabian Stylede Cillia, Michael, Christof Mittermair, Hannes Hoi, Martin Grünbart, and Helmut Weiss. 2026. "Sleeve Gastrectomy Leads to Immediate, Significant Intraoperative Increase in Lower Esophageal Distensibility and Opening Area" Journal of Clinical Medicine 15, no. 2: 701. https://doi.org/10.3390/jcm15020701
APA Stylede Cillia, M., Mittermair, C., Hoi, H., Grünbart, M., & Weiss, H. (2026). Sleeve Gastrectomy Leads to Immediate, Significant Intraoperative Increase in Lower Esophageal Distensibility and Opening Area. Journal of Clinical Medicine, 15(2), 701. https://doi.org/10.3390/jcm15020701






