Effect of Surgeon Service Volume on Survival of Liver Transplant Patients: A Nationwide Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Sources and Study Populations
2.2. Definition of Relevant Variables
2.3. Statistical Analysis
3. Results
4. Discussion
5. Limitation
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CCI | Charlson Comorbidity Index |
| MELD | Model for End-Stage Liver Disease |
References
- Taiwanese Ministry of Health and Welfare. Statistics on the Cause of Death of Taiwanese People 2017; Taiwanese Ministry of Health and Welfare: Taipei City, Taiwan, 2017.
- Finkenstedt, A.; Nachbaur, K.; Zoller, H. Acute-on-chronic liver failure: Excellent outcomes after liver transplantation but high mortality on the wait list. Liver Transplant. 2013, 19, 879–886. [Google Scholar] [CrossRef] [PubMed]
- Rattanasiri, S.; McDaniel, D.O.; McEvoy, M. The association between cytokine gene polymorphisms and graft rejection in liver transplantation: A systematic review and meta-analysis. Transpl. Immunol. 2013, 28, 62–70. [Google Scholar] [CrossRef] [PubMed]
- Sannananja, B.; Seyal, A.R.; Baheti, A.D. Tricky Findings in Liver Transplant Imaging: A Review of Pitfalls with Solutions. Curr. Probl. Diagn. Radiol. 2017, 47, 179–188. [Google Scholar] [CrossRef] [PubMed]
- National Health Insurance Administration. The National Health Insurance Administration Has Released Four Postoperative Survival Indicators for Organ Transplant Patients. Available online: https://www.nhi.gov.tw/ch/cp-7585-27ad4-3255-1.html (accessed on 26 December 2025).
- Levitsky, J.; Cohen, S.M. The liver transplant recipient: What you need to know for long-term care. J. Fam. Pract. 2006, 55, 136–144. [Google Scholar]
- Wu, L.M.; Xu, X.; Zheng, S.S. Hepatitis B virus reinfection after liver transplantation: Related risk factors and perspective. Hepatobiliary Pancreat. Dis. Int. 2005, 4, 502–508. [Google Scholar]
- Pol, B.; Campan, P.; Hardwigsen, J. Morbidity of major hepatic resections: A 100-case prospective study. Eur. J. Surg. 1999, 165, 446–453. [Google Scholar]
- Hillner, B.E.; Smith, T.J.; Desch, C.E. Hospital and physician volume or specialization and outcomes in cancer treatment: Importance in quality of cancer care. J. Clin. Oncol. 2000, 18, 2327–2340. [Google Scholar] [CrossRef]
- Adams, D.F.; Fraser, D.B.; Abrams, H.L. The Complications of Coronary Arteriography. Circulation 1973, 48, 609–618. [Google Scholar] [CrossRef]
- Xirasagar, S.; Lien, Y.C.; Lin, H.C. Procedure volume of gastric cancer resections versus 5-year survival. Eur. J. Surg. Oncol. 2008, 34, 23–29. [Google Scholar] [CrossRef]
- Archampong, D.; Borowski, D.; Wille-Jørgensen, P. Workload and surgeon’s specialty for outcome after colorectal cancer surgery. Cochrane Libr. 2012, 14, CD005391. [Google Scholar]
- Smith, M.D.; Patterson, E.; Wahed, A.S. Relationship between surgeon volume and adverse outcomes after RYGB in Longitudinal Assessment of Bariatric Surgery (LABS) study. Surg. Obes. Relat. Dis. 2010, 6, 118–125. [Google Scholar] [CrossRef]
- Amato, L.; Colais, P.; Davoli, M. Volume and health outcomes: Evidence from systematic reviews and from evaluation of Italian hospital data. Epidemiol. Prev. 2013, 37, 1–100. [Google Scholar] [PubMed]
- Luft, H.S. Hospital Volume, Physician Volume, and Patient Outcome: Assessing the Evidence; Health Administration Press: Chicago, IL, USA, 1990. [Google Scholar]
- Waldman, J.D.; Yourstone, S.A.; Smith, H.L. Learning curves in health care. Health Care Manag. Rev. 2003, 28, 41–54. [Google Scholar] [CrossRef] [PubMed]
- Adam, R.; Cailliez, V.; Majno, P. Normalised intrinsic mortality risk in liver transplantation: European Liver Transplant Registry study. Lancet 2000, 356, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Axelrod, D.A.; Guidinger, M.K.; McCullough, K.P. Association of center volume with outcome after liver and kidney transplantation. Am. J. Transplant. 2004, 4, 920–927. [Google Scholar] [CrossRef]
- Busuttil, R.W.; Lake, J.R. Role of tacrolimus in the evolution of liver transplantation. Transplantation 2004, 77, 44–51. [Google Scholar] [CrossRef]
- Lorenzo, M.; Herrero, J.I.; Quiroga, J. De novo neoplasia after liver transplantation: An analysis of risk factors and influence on survival. Liver Transplant. 2005, 11, 89–97. [Google Scholar]
- Hong, Z.; Wu, J.; Smart, G. Survival analysis of liver transplant patients in Canada 1997–2002. Transplant. Proc. 2006, 38, 2951–2956. [Google Scholar] [CrossRef]
- Desai, S.; Hong, J.C.; Saab, S. Cardiovascular risk factors following orthotopic liver transplantation: Predisposing factors, incidence and management. Liver Int. 2010, 30, 948–957. [Google Scholar] [CrossRef]
- Ozhathil, D.K.; Li, Y.F.; Smith, J.K. Impact of center volume on outcomes of increased-risk liver transplants. Liver Transplant. 2011, 17, 1191–1199. [Google Scholar] [CrossRef]
- Magnetta, M.J.; Xing, M.; Zhang, D. The effect of bridging locoregional therapy and Sociodemographics on survival in hepatocellular carcinoma patients undergoing orthotopic liver transplantation: A united network for organ sharing population study. J. Vasc. Interv. Radiol. 2016, 27, 1822–1828. [Google Scholar] [CrossRef]
- Kwon, J.H.; Yoon, Y.I.; Song, G.W. Living Donor Liver Transplantation for Patients Older Than Age 70 Years: A Single-Center Experience. Am. J. Transplant. 2017, 17, 2890–2900. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Wang, X.; Huang, R. Prognostic value of marital status on stage at diagnosis in hepatocellular carcinoma. Sci. Rep. 2017, 7, 41695. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Pu, L.; Gao, W. Influence of marital status on the survival of adults with extrahepatic/intrahepatic cholangiocarcinoma. Oncotarget 2017, 8, 28959. [Google Scholar] [CrossRef] [PubMed]
- Ramos, P.A.; Hervás, M.D.; García, C.A. Outcomes in patients with diabetes 10 years after liver transplantation. J. Diabetes 2017, 9, 1033–1039. [Google Scholar] [CrossRef]
- Burroughs, A.K.; Sabin, C.A.; Rolles, K. 3-month and 12-month mortality after first liver transplant in adults in Europe: Predictive models for outcome. Lancet 2006, 367, 225–232. [Google Scholar] [CrossRef]
- VanWagner, L.B.; Ning, H.; Whitsett, M. A point-based prediction model for cardiovascular risk in orthotopic liver transplantation: The Carolt score. Hepatology 2017, 66, 1968–1979. [Google Scholar] [CrossRef]
- Gallagher, T.K.; Thomas, K.A.; Ladner, D.P. Incidence and Risk Factors of Intracranial Hemorrhage in Liver Transplant Recipients. Transplantation 2018, 102, 448–453. [Google Scholar] [CrossRef]
- Deyo, R.A.; Cherkin, D.C.; Ciol, M.A. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J. Clin. Epidemiol. 1992, 45, 613–619. [Google Scholar] [CrossRef]
- Liu, C.Y.; Hung, Y.T.; Chuang, Y.L. Incorporating Development Stratification of Taiwan Townships into Sampling Design of Large Scale Health Interview Survey. J. Health Manag. 2006, 4, 1–22. [Google Scholar]
- Scarborough, J.E.; Pietrobon, R.; Tuttle-Newhall, J.E. Relationship between provider volume and outcomes for orthotopic liver transplantation. J. Gastrointest. Surg. 2008, 12, 1527–1533. [Google Scholar] [CrossRef] [PubMed]
- Weng, S.F.; Chu, C.C.; Chien, C.C. Renal transplantation: Relationship between hospital/surgeon volume and postoperative severe sepsis/graft-failure. A nationwide population-based study. Int. J. Med. Sci. 2014, 11, 918. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.; Dhar, V.K.; Wima, K. The center volume–outcome effect in pancreas transplantation: A national analysis. J. Surg. Res. 2017, 213, 25–31. [Google Scholar] [CrossRef] [PubMed]
- de Boer, J.D.; Putter, H.; Blok, J.J.; Alwayn, I.P.J.; van Hoek, B.; Braat, A.E. Predictive Capacity of Risk Models in Liver Transplantation. Transpl. Direct 2019, 5, e457. [Google Scholar] [CrossRef]
- Kang, C.; Ryu, H.G. Impact of institutional case volume of solid organ transplantation on patient outcomes and implications for healthcare policy in Korea. Korean J. Transpl. 2023, 37, 1–10. [Google Scholar] [CrossRef]
- Palaniyappan, N.; Peach, E.; Pearce, F.; Dhaliwal, A.; Campos-Varela, I.; Cant, M.R.; Dopazo, C.; Trotter, J.; Divani-Patel, S.; Hatta, A.A.; et al. Long-term outcomes (beyond 5 years) of liver transplant recipients—A transatlantic multicenter study. Liver Transplant. 2024, 30, 170–181. [Google Scholar] [CrossRef]
- Huang, J.W.; Kung, Y.T.; Chang, W.T. Risk Factors Analysis for New-Onset Diabetes Mellitus after Liver Transplantation—A National Population Based Study in Taiwan. Med. J. South Taiwan 2016, 12, 29–37. [Google Scholar]
- Petrowsky, H.; Rana, A.; Kaldas, F.M. Liver transplantation in highest acuity recipients: Identifying factors to avoid futility. Ann. Surg. 2014, 259, 1186–1194. [Google Scholar] [CrossRef]
- Pischke, S.; Lege, M.C.; von Wulffen, M. Factors associated with long-term survival after liver transplantation: A retrospective cohort study. World J. Hepatol. 2017, 9, 427. [Google Scholar] [CrossRef]
| Variable | N | % |
|---|---|---|
| Total | 3233 | 100 |
| 1-year survival after surgery | ||
| Dead | 459 | 14.20 |
| Alive | 2774 | 85.80 |
| Surgeon’s relative service volume (cases) | ||
| Low (≤31) | 811 | 25.09 |
| Medium (32–306) | 1611 | 49.82 |
| High (≥307) | 811 | 25.09 |
| Surgeon’s cumulative service volume (cases) | ||
| ≤20 | 619 | 19.15 |
| 21–40 | 320 | 9.90 |
| 41–60 | 249 | 7.70 |
| 61–80 | 193 | 5.97 |
| 81–100 | 123 | 3.80 |
| 101–120 | 124 | 3.84 |
| 121–140 | 119 | 3.68 |
| 141–160 | 118 | 3.65 |
| 161–180 | 125 | 3.87 |
| 181–200 | 105 | 3.25 |
| 201–230 | 104 | 3.22 |
| 231–260 | 88 | 2.72 |
| 261–300 | 117 | 3.62 |
| 301–400 | 297 | 9.19 |
| 401–500 | 210 | 6.50 |
| ≥501 | 322 | 9.96 |
| Patient sex | ||
| Male | 2299 | 71.11 |
| Female | 934 | 28.89 |
| Patient age (years) | ||
| <20 | 250 | 7.73 |
| 20–34 | 132 | 4.08 |
| 35–44 | 360 | 11.14 |
| 55–64 | 1181 | 36.53 |
| ≥65 | 185 | 5.72 |
| Monthly salary (USD) | ||
| <564 | 601 | 18.59 |
| 564–744 | 1151 | 35.60 |
| 745–940 | 298 | 9.22 |
| 941–1186 | 324 | 10.02 |
| 1187–1496 | 488 | 15.09 |
| ≥1497 | 371 | 11.48 |
| Charlson Comorbidity Index | ||
| 0 | 701 | 21.68 |
| 1–2 | 1391 | 43.03 |
| ≥3 | 1141 | 35.29 |
| Urbanization of residence area | ||
| Level 1 | 824 | 25.49 |
| Level 2 | 1020 | 31.55 |
| Level 3 | 568 | 17.57 |
| Level 4 | 498 | 15.40 |
| Level 5 | 65 | 2.01 |
| Level 6 | 118 | 3.65 |
| Level 7 | 140 | 4.33 |
| Whether the surgeon changed the practice hospital | ||
| Yes | 8 | 0.25 |
| No | 3225 | 99.75 |
| Hospital accreditation level | ||
| Medical center | 3139 | 97.09 |
| Regional hospital | 94 | 2.91 |
| Hospital ownership | ||
| Public hospital | 1027 | 31.77 |
| Non-public hospital | 2206 | 68.23 |
| Year of transplantation | ||
| 2005 | 177 | 5.47 |
| 2006 | 210 | 6.50 |
| 2007 | 254 | 7.86 |
| 2008 | 325 | 10.05 |
| 2009 | 347 | 10.73 |
| 2010 | 429 | 13.27 |
| 2011 | 503 | 15.56 |
| 2012 | 512 | 15.84 |
| 2013 | 476 | 14.72 |
| Year after surgery | Alive (N) | Survival rate (%) |
| First year | 2774 | 85.80 |
| Second year | 2660 | 82.25 |
| Third year | 2595 | 80.27 |
| Fourth year | 2555 | 79.03 |
| Fifth year | 2527 | 78.16 |
| Variable | Survival, N | Survival (%) | p-Value |
|---|---|---|---|
| Total | 2774 | 85.80 | |
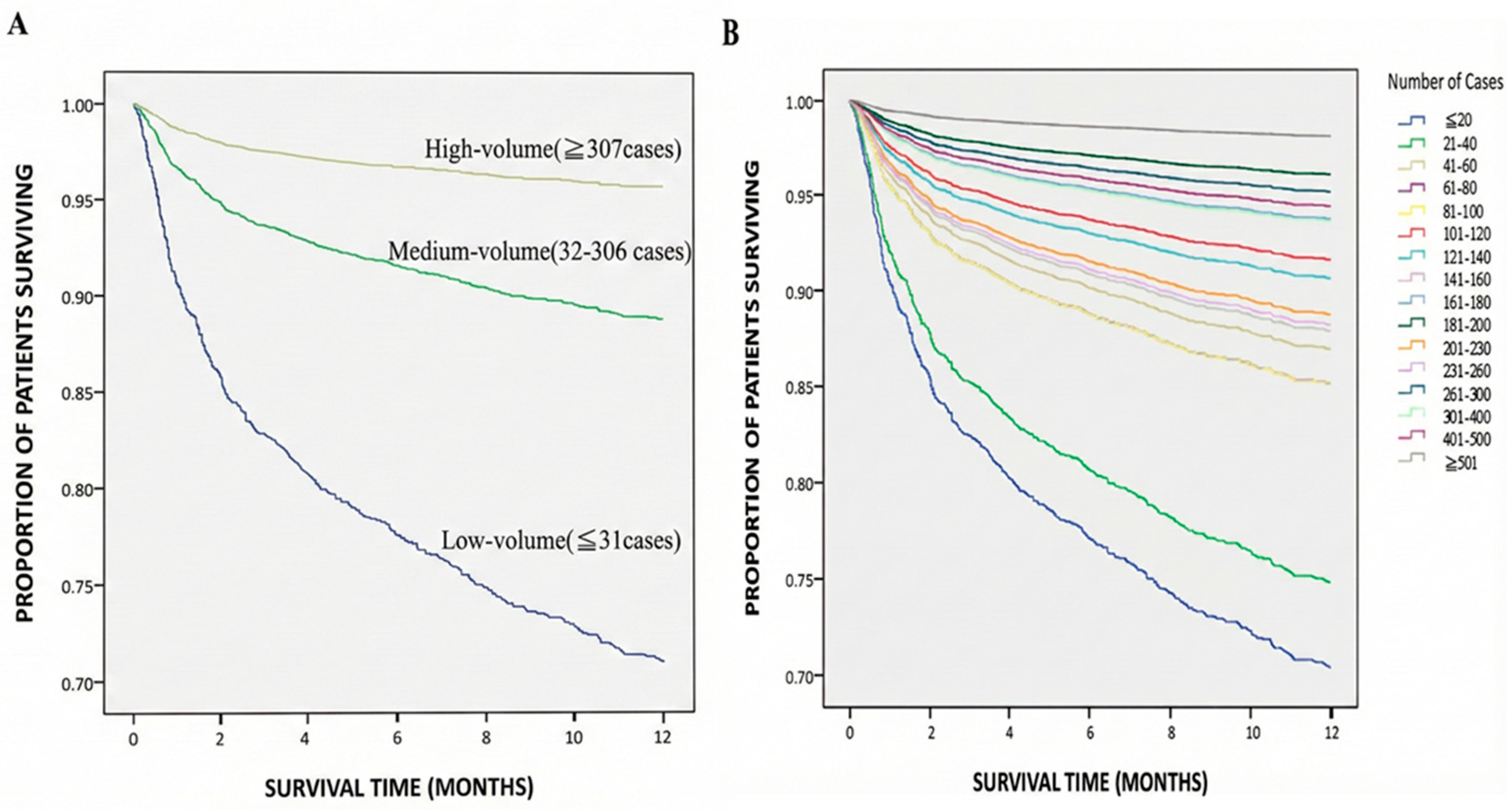
| Surgeon’s relative service volume (cases) | <0.001 | ||
| Low (≤31) | 579 | 71.39 | |
| Medium (32–306) | 1422 | 88.27 | |
| High (≥307) | 773 | 95.31 | |
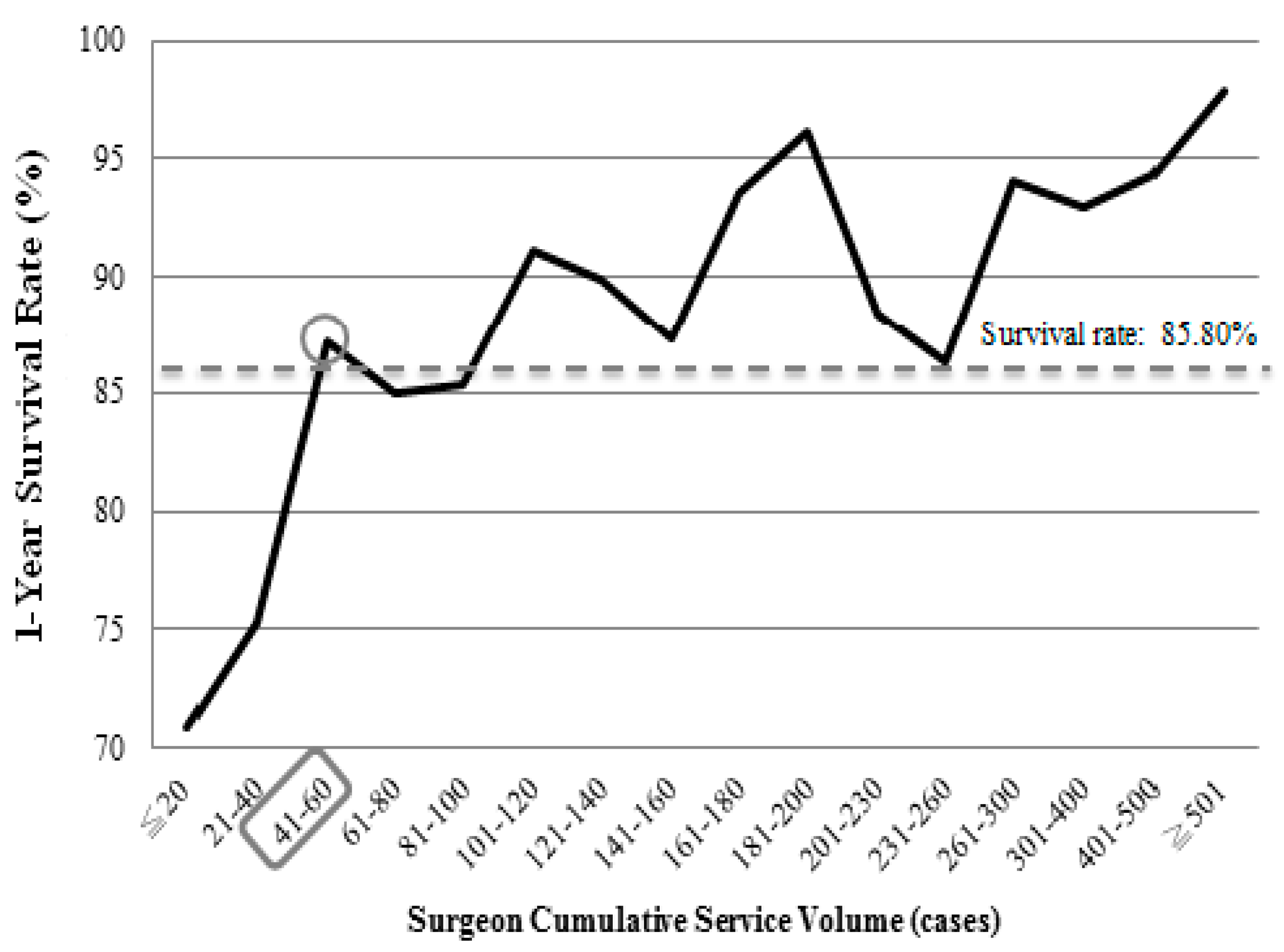
| Surgeon’s cumulative service volume (cases) | <0.001 | ||
| ≤20 | 439 | 70.92 | |
| 21–40 | 241 | 75.31 | |
| 41–60 | 217 | 87.15 | |
| 61–80 | 164 | 84.97 | |
| 81–100 | 105 | 85.37 | |
| 101–120 | 113 | 91.13 | |
| 121–140 | 107 | 89.92 | |
| 141–160 | 103 | 87.29 | |
| 161–180 | 117 | 93.60 | |
| 181–200 | 101 | 96.19 | |
| 201–230 | 92 | 88.46 | |
| 231–260 | 76 | 86.36 | |
| 261–300 | 110 | 94.02 | |
| 301–400 | 276 | 92.93 | |
| 401–500 | 198 | 94.29 | |
| ≥501 | 315 | 97.83 | |
| Patient sex | 0.823 | ||
| Male | 1974 | 85.86 | |
| Female | 800 | 85.65 | |
| Patient age | 0.350 | ||
| <20 | 216 | 86.40 | |
| 20–34 | 114 | 86.36 | |
| 35–44 | 315 | 87.50 | |
| 45–54 | 980 | 87.11 | |
| 55–64 | 995 | 84.25 | |
| ≥65 | 154 | 83.24 | |
| Monthly salary (USD) | 0.148 | ||
| <564 | 499 | 83.03 | |
| 564–744 | 983 | 85.40 | |
| 745–940 | 255 | 85.57 | |
| 941–1186 | 283 | 87.35 | |
| 1187–1496 | 430 | 88.11 | |
| ≥1497 | 324 | 87.33 | |
| Charlson Comorbidity Index | 0.001 | ||
| 0 | 621 | 88.59 | |
| 1–2 | 1208 | 86.84 | |
| ≥3 | 945 | 82.82 | |
| Urbanization of residence area | 0.522 | ||
| Level 1 | 697 | 84.59 | |
| Level 2 | 888 | 87.06 | |
| Level 3 | 493 | 86.80 | |
| Level 4 | 426 | 85.54 | |
| Level 5 | 53 | 81.54 | |
| Level 6 | 101 | 85.59 | |
| Level 7 | 116 | 82.86 | |
| Whether the surgeon changed the practice hospital | 0.053 | ||
| Yes | 5 | 62.50 | |
| No | 2769 | 85.86 | |
| Hospital accreditation level | 0.044 | ||
| Medical center | 2700 | 86.01 | |
| Regional hospital | 74 | 78.72 | |
| Hospital ownership | 0.026 | ||
| Public hospital | 862 | 83.93 | |
| Non-public hospital | 1912 | 86.67 | |
| Year of transplantation | <0.001 | ||
| 2005 | 144 | 81.36 | |
| 2006 | 163 | 77.62 | |
| 2007 | 202 | 79.53 | |
| 2008 | 277 | 85.23 | |
| 2009 | 305 | 87.90 | |
| 2010 | 372 | 86.71 | |
| 2011 | 434 | 86.28 | |
| 2012 | 447 | 87.30 | |
| 2013 | 430 | 90.34 |
| Variable | Adjusted Model 1 | Adjusted Model 2 | ||||||
|---|---|---|---|---|---|---|---|---|
| HR | 95%C.I. | p-Value | HR | 95%C.I. | p-Value | |||
| Surgeon’s relative service volume (cases) | ||||||||
| Low (≤31) | 1.00 | |||||||
| Medium (32–306) | 0.35 | 0.28 | 0.43 | <0.001 | ||||
| High (≥307) | 0.13 | 0.09 | 0.19 | <0.001 | ||||
| Surgeon’s cumulative service volume (cases) | ||||||||
| ≤20 | 1.00 | |||||||
| 21–40 | 0.83 | 0.63 | 1.09 | 0.179 | ||||
| 41–60 | 0.40 | 0.27 | 0.59 | <0.001 | ||||
| 61–80 | 0.46 | 0.31 | 0.69 | <0.001 | ||||
| 81–100 | 0.46 | 0.28 | 0.75 | 0.002 | ||||
| 101–120 | 0.25 | 0.14 | 0.47 | <0.001 | ||||
| 121–140 | 0.28 | 0.15 | 0.51 | <0.001 | ||||
| 141–160 | 0.37 | 0.21 | 0.63 | <0.001 | ||||
| 161–180 | 0.18 | 0.09 | 0.38 | <0.001 | ||||
| 181–200 | 0.12 | 0.04 | 0.31 | <0.001 | ||||
| 201–230 | 0.34 | 0.19 | 0.62 | <0.001 | ||||
| 231–260 | 0.36 | 0.20 | 0.65 | 0.001 | ||||
| 261–300 | 0.14 | 0.07 | 0.31 | <0.001 | ||||
| 301–400 | 0.19 | 0.12 | 0.30 | <0.001 | ||||
| 401–500 | 0.16 | 0.09 | 0.31 | <0.001 | ||||
| ≥501 | 0.06 | 0.03 | 0.12 | <0.001 | ||||
| Patient sex | ||||||||
| Male | 1.00 | 1.00 | ||||||
| Female | 0.95 | 0.77 | 1.17 | 0.639 | 0.98 | 0.79 | 1.21 | 0.848 |
| Patient age | ||||||||
| <20 | 1.00 | 1.00 | ||||||
| 20–34 | 0.88 | 0.49 | 1.59 | 0.680 | 0.83 | 0.46 | 1.49 | 0.526 |
| 35–44 | 0.81 | 0.50 | 1.32 | 0.399 | 0.75 | 0.46 | 1.21 | 0.239 |
| 45–54 | 0.90 | 0.59 | 1.37 | 0.609 | 0.84 | 0.55 | 1.29 | 0.427 |
| 55–64 | 1.12 | 0.74 | 1.70 | 0.593 | 1.05 | 0.69 | 1.59 | 0.835 |
| ≥65 | 1.23 | 0.72 | 2.09 | 0.451 | 1.13 | 0.66 | 1.93 | 0.653 |
| Monthly salary (USD) | ||||||||
| <564 | 1.00 | 1.00 | ||||||
| 564–744 | 0.89 | 0.70 | 1.15 | 0.385 | 0.92 | 0.71 | 1.18 | 0.505 |
| 745–940 | 0.84 | 0.59 | 1.21 | 0.349 | 0.85 | 0.59 | 1.23 | 0.391 |
| 941–1186 | 0.77 | 0.53 | 1.11 | 0.160 | 0.77 | 0.53 | 1.11 | 0.165 |
| 1187–1496 | 0.77 | 0.55 | 1.07 | 0.121 | 0.80 | 0.57 | 1.11 | 0.183 |
| ≥1497 | 0.82 | 0.58 | 1.16 | 0.264 | 0.87 | 0.61 | 1.23 | 0.420 |
| Charlson Comorbidity Index | ||||||||
| 0 | 1.00 | 1.00 | ||||||
| 1–2 | 1.21 | 0.90 | 1.62 | 0.204 | 1.21 | 0.90 | 1.63 | 0.201 |
| ≥3 | 1.52 | 1.13 | 2.05 | 0.006 | 1.54 | 1.14 | 2.08 | 0.005 |
| Urbanization of residence area | ||||||||
| Level 1 | 1.00 | 1.00 | ||||||
| Level 2 | 0.92 | 0.72 | 1.18 | 0.506 | 0.91 | 0.71 | 1.17 | 0.456 |
| Level 3 | 0.87 | 0.65 | 1.16 | 0.337 | 0.87 | 0.65 | 1.16 | 0.336 |
| Level 4 | 0.94 | 0.70 | 1.27 | 0.703 | 0.94 | 0.69 | 1.26 | 0.657 |
| Level 5 | 1.27 | 0.70 | 2.33 | 0.431 | 1.28 | 0.70 | 2.34 | 0.427 |
| Level 6 | 0.73 | 0.44 | 1.24 | 0.244 | 0.76 | 0.45 | 1.28 | 0.303 |
| Level 7 | 1.21 | 0.77 | 1.89 | 0.402 | 1.16 | 0.74 | 1.82 | 0.510 |
| Whether the surgeon changed the practice hospital | ||||||||
| Yes | 1.00 | 1.00 | ||||||
| No | 0.75 | 0.23 | 2.41 | 0.627 | 0.77 | 0.24 | 2.50 | 0.668 |
| Hospital accreditation level | ||||||||
| Medical center | 1.00 | 1.00 | ||||||
| Regional hospital | 0.64 | 0.40 | 1.03 | 0.064 | 0.62 | 0.39 | 1.00 | 0.051 |
| Hospital ownership | ||||||||
| Public hospital | 1.00 | 1.00 | ||||||
| Non-public hospital | 1.09 | 0.88 | 1.34 | 0.443 | 1.18 | 0.95 | 1.46 | 0.133 |
| Year of transplantation | ||||||||
| 2005 | 1.00 | 1.00 | ||||||
| 2006 | 1.16 | 0.74 | 1.82 | 0.516 | 1.12 | 0.71 | 1.76 | 0.637 |
| 2007 | 1.20 | 0.78 | 1.87 | 0.410 | 1.24 | 0.80 | 1.94 | 0.343 |
| 2008 | 0.89 | 0.57 | 1.40 | 0.617 | 0.90 | 0.57 | 1.41 | 0.637 |
| 2009 | 0.77 | 0.48 | 1.21 | 0.257 | 0.73 | 0.46 | 1.16 | 0.183 |
| 2010 | 0.97 | 0.62 | 1.50 | 0.876 | 0.97 | 0.62 | 1.51 | 0.885 |
| 2011 | 0.98 | 0.64 | 1.50 | 0.938 | 1.03 | 0.67 | 1.58 | 0.897 |
| 2012 | 1.11 | 0.72 | 1.71 | 0.637 | 1.07 | 0.68 | 1.66 | 0.781 |
| 2013 | 0.88 | 0.56 | 1.40 | 0.592 | 0.89 | 0.56 | 1.43 | 0.635 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Chiang, L.-Y.; Wang, T.-W.; Kung, P.-T.; Tsai, W.-C. Effect of Surgeon Service Volume on Survival of Liver Transplant Patients: A Nationwide Cohort Study. J. Clin. Med. 2026, 15, 321. https://doi.org/10.3390/jcm15010321
Chiang L-Y, Wang T-W, Kung P-T, Tsai W-C. Effect of Surgeon Service Volume on Survival of Liver Transplant Patients: A Nationwide Cohort Study. Journal of Clinical Medicine. 2026; 15(1):321. https://doi.org/10.3390/jcm15010321
Chicago/Turabian StyleChiang, Liang-Yu, Tzu-Wei Wang, Pei-Tseng Kung, and Wen-Chen Tsai. 2026. "Effect of Surgeon Service Volume on Survival of Liver Transplant Patients: A Nationwide Cohort Study" Journal of Clinical Medicine 15, no. 1: 321. https://doi.org/10.3390/jcm15010321
APA StyleChiang, L.-Y., Wang, T.-W., Kung, P.-T., & Tsai, W.-C. (2026). Effect of Surgeon Service Volume on Survival of Liver Transplant Patients: A Nationwide Cohort Study. Journal of Clinical Medicine, 15(1), 321. https://doi.org/10.3390/jcm15010321






