Association Between Lipid-Lowering Therapy and Differences in the Distribution of LDL-C, apoB and non-HDL-C
Abstract
1. Introduction
2. Materials and Methods
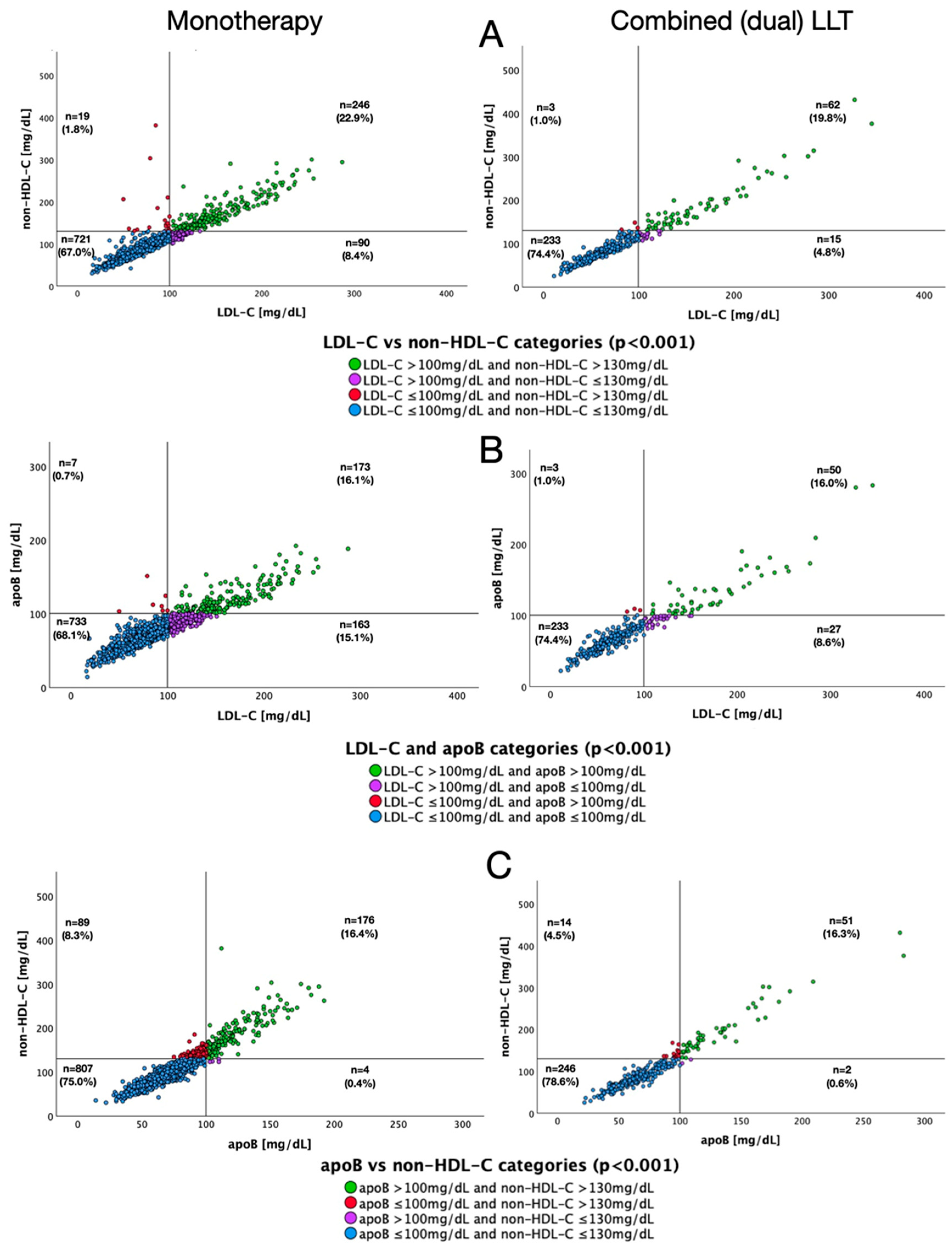
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| LDL-C | low-density lipoprotein cholesterol |
| non-HDL-C | non-high-density lipoprotein cholesterol |
| apoB | Apolipoprotein B |
| LLT | lipid-lowering therapy |
| ASCVD | atherosclerotic cardiovascular disease |
| TG | triglyceride |
| DM | diabetes mellitus |
| VLDL | very-low-density lipoprotein |
| IDL | intermediate-density lipoprotein |
| Lp(a) | Lipoprotein (a) |
| JLS | Jurasz Lipid Study |
| BMI | body mass index |
| SCORE2 | Systematic Coronary Risk Evaluation 2 |
| SCORE2-OP | Systematic Coronary Risk Estimation 2-Older Persons |
| CV | cardiovascular |
| IQR | interquartile range |
| MESA | The Multi-Ethnic Study of Atherosclerosis |
References
- Burden of Cardiovascular Diseases Writing Group. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019: Update From the GBD 2019 Study. J. Am. Coll. Cardiol. 2020, 76, 2982–3021, Erratum in J. Am. Coll. Cardiol. 2021, 77, 1958–1959. https://doi.org/10.1016/j.jacc.2021.02.039. [CrossRef]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk: The Task Force for the management of dyslipidaemias of the European Society of Cardiology (ESC) and European Atherosclerosis Society (EAS). Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [PubMed]
- Prassl, R.; Laggner, P. Lipoprotein Structure and Dynamics: Low Density Lipoprotein Viewed as a Highly Dynamic and Flexible Nanoparticle. In Lipoproteins—Role in Health and Diseases; Frank, S., Kostnern, G., Eds.; InTech: London, UK, 2012. [Google Scholar] [CrossRef]
- Glavinovic, T.; Thanassoulis, G.; de Graaf, J.; Couture, P.; Hegele, R.A.; Sniderman, A.D. Physiological Bases for the Superiority of Apolipoprotein B Over Low-Density Lipoprotein Cholesterol and Non-High-Density Lipoprotein Cholesterol as a Marker of Cardiovascular Risk. J. Am. Heart Assoc. 2022, 11, e025858. [Google Scholar] [CrossRef] [PubMed]
- Banach, M.; Burchardt, P.; Chlebus, K.; Dobrowolski, P.; Dudek, D.; Dyrbuś, K.; Gąsior, M.; Jankowski, P.; Jóźwiak, J.; Kłosiewicz-Latoszek, L.; et al. PTL/KLRWP/PTK/PTDL/PTD/PTNT Guidelines diagnosis and treatment of lipid disorders in Poland 2021 (Wytyczne PTL/KLRWP/PTK/PTDL/PTD/PTNT diagnostyki i leczenia zaburzeń lipidowych w Polsce 2021). Nadciśnienie Tętnicze Praktyce 2021, 7, 113–122. [Google Scholar]
- Ratajczak, J.; Kubica, A.; Michalski, P.; Pietrzykowski, Ł.; Białczyk, A.; Kosobucka-Ozdoba, A.; Bergmann, K.; Buczkowski, K.; Krintus, M.; Jankowski, P.; et al. Determinants of Lipid Parameters in Patients without Diagnosed Cardiovascular Disease—Results of the Polish Arm of the EUROASPIRE V Survey. J. Clin. Med. 2023, 12, 2738. [Google Scholar] [CrossRef] [PubMed]
- Ratajczak, J.; Kubica, A.; Pietrzykowski, Ł.; Michalski, P.; Kosobucka-Ozdoba, A.; Buczkowski, K.; Krintus, M.; Jankowski, P.; Kubica, J. Lipoprotein (a) and the Occurrence of Lipid Disorders and Other Cardiovascular Risk Factors in Patients without Diagnosed Cardiovascular Disease. J. Clin. Med. 2024, 13, 4649. [Google Scholar] [CrossRef] [PubMed]
- Ziółkowski, M.; Ratajczak, J.; Obońska, K.; Adamski, P.; Banach, M.; Chlebus, K.; Grymuza, M.; Grzelakowska, K.; Jankowski, P.; Konarski, J.; et al. Lipid profile and the variables associated with control of selected lipid parameters in patients of a large multi-specialist hospital in Poland - the Jurasz Lipid Study (JLS). Lipids Health Dis. 2025, 24, 300. [Google Scholar] [CrossRef] [PubMed]
- Visseren, F.L.J.; Mach, F.; Smulders, Y.M.; Carballo, D.; Koskinas, K.C.; Bäck, M.; Benetos, A.; Biffi, A.; Boavida, J.M.; Capodanno, D.; et al. 2021 ESC Guidelines on cardiovascular disease prevention in clinical practice. Eur. Heart J. 2021, 42, 3227–3337. [Google Scholar] [CrossRef] [PubMed]
- Solnica, B.; Sniderman, A.D.; Wyszomirski, A.; Rutkowski, M.; Chlebus, K.; Bandosz, P.; Pencina, M.J.; Zdrojewski, T. Concordance/discordance between serum apolipoprotein B, low density lipoprotein cholesterol and non-high density lipoprotein cholesterol in NATPOL 2011 participants—An epidemiological perspective. Int. J. Cardiol. 2023, 390, 131150. [Google Scholar] [CrossRef] [PubMed]
- Zdrojewski, T.; Solnica, B.; Cybulska, B.; Bandosz, P.; Rutkowski, M.; Stokwiszewski, J.; Gaciong, Z.; Banach, M.; Wojtyniak, B.; Pencina, M.; et al. Prevalence of lipid abnormalities in Poland. The NATPOL 2011 survey. Kardiol. Pol. 2016, 74, 213–223. [Google Scholar] [CrossRef] [PubMed]
- Cao, J.; Nomura, S.O.; Steffen, B.T.; Guan, W.; Remaley, A.T.; Karger, A.B.; Ouyang, P.; Michos, E.D.; Tsai, M.Y. Apolipoprotein B discordance with low-density lipoprotein cholesterol and non-high-density lipoprotein cholesterol in relation to coronary artery calcification in the Multi-Ethnic Study of Atherosclerosis (MESA). J. Clin. Lipidol. 2020, 14, 109–121.e5. [Google Scholar] [CrossRef] [PubMed]
- Kim, C.W.; Hong, S.; Chang, Y.; Lee, J.A.; Shin, H.; Ryu, S. Discordance Between Apolipoprotein B and Low-Density Lipoprotein Cholesterol and Progression of Coronary Artery Calcification in Middle Age. Circ. J. 2021, 85, 900–907. [Google Scholar] [CrossRef] [PubMed]
- Johannesen, C.D.L.; Mortensen, M.B.; Langsted, A.; Nordestgaard, B.G. Apolipoprotein B and Non-HDL Cholesterol Better Reflect Residual Risk Than LDL Cholesterol in Statin-Treated Patients. J. Am. Coll. Cardiol. 2021, 77, 1439–1450. [Google Scholar] [CrossRef] [PubMed]
- Wong, N.D.; Chuang, J.; Zhao, Y.; Rosenblit, P.D. Residual dyslipidemia according to low-density lipoprotein cholesterol, non-high-density lipoprotein cholesterol, and apolipoprotein B among statin-treated US adults: National Health and Nutrition Examination Survey 2009–2010. J. Clin. Lipidol. 2015, 9, 525–532. [Google Scholar] [CrossRef] [PubMed]
- Boekholdt, S.M.; Arsenault, B.J.; Mora, S.; Pedersen, T.R.; LaRosa, J.C.; Nestel, P.J.; Simes, R.J.; Durrington, P.; Hitman, G.A.; Welch, K.M.; et al. Association of LDL cholesterol, non-HDL cholesterol, and apolipoprotein B levels with risk of cardiovascular events among patients treated with statins: A meta-analysis. JAMA 2012, 307, 1302–1309. [Google Scholar] [CrossRef] [PubMed]




| Comorbidities | ICD-10 and ICD-9 |
|---|---|
| Acute coronary syndromes | I20; I21; I22; I24 |
| Chronic coronary syndromes | I25 |
| CABG/PCI | Z95.1; Z95.5; 36.091; 36.11–16 |
| Aortic stenosis and mitral valve diseases | I34; I35.0; I35.2 |
| Stroke | I61; I62; I63; I64; I69 |
| Other atherosclerotic diseases | I65; I66.; I70; 39.501 |
| Atrial fibrillation | I48 |
| Arterial hypertension | I10; I12; I13 |
| Diabetes mellitus type 1 | E10 |
| Diabetes mellitus type 2 | E11 |
| Acute/chronic pancreatitis | K85; K86.1 |
| Aortic aneurysm | I71 |
| Analyzed Parameter | All Patients (n = 5 048) | Without LLT (n = 3 656) | LLT (n = 1 392) | p-Value | |
|---|---|---|---|---|---|
| Age, median (IQR), [y] | 64 (45–74) | 59 (37–72) | 70 (62–77) | <0.001 | |
| Male gender, n (%) | 2599 (51.5) | 1800 (49.2) | 799 (57.4) | <0.001 | |
| BMI, median (IQR), [kg/m2] | 26.6 (23.0–30.6) * | 26.1 (22.5–30.4) | 27.5 (24.3–31.4) | <0.001 | |
| History of ACS, n (%) | 874 (17.3) | 386 (10.6) | 488 (35.1) | <0.001 | |
| History of CCS, n (%) | 1246 (24.7) | 622 (17.0) | 624 (44.8) | <0.001 | |
| History of PCI/CABG, n (%) | 817 (16.2) | 375 (10.3) | 442 (31.8) | <0.001 | |
| DM, n (%) | 975 (19.3) | 495 (13.5) | 480 (34.5) | <0.001 | |
| Arterial hypertension, n (%) | 1988 (39.4) | 1098 (30.0) | 890 (63.9) | <0.001 | |
| SBP, median (IQR), [mmHg] | 134 (120–150) * | 131 (118.5–150) | 139 (122–156) | <0.001 | |
| DBP, median (IQR), [mmHg] | 80 (70–88) * | 80 (70–88) | 79 (70–88) | 0.304 | |
| eGFR, median (IQR), [ml/min] | 85.1 (61–101.8) * | 89.5 (68.2–108) | 70 (47.1–88) | <0.001 | |
| Stroke, n (%) | 872 (17.3) | 470 (12.9) | 402 (28.9) | <0.001 | |
| Peripheral and carotid artery disease, n (%) | 729 (14.4) | 362 (9.9) | 367 (26.4) | <0.001 | |
| Aortic aneurysm, n (%) | 126 (2.5) | 66 (1.8) | 60 (4.3) | <0.001 | |
| Aortic stenosis, n (%) | 402 (8.0) | 223 (6.1) | 179 (12.9) | <0.001 | |
| Mitral valve disease, n (%) | 730 (14.5) | 369 (10.1) | 361 (25.9) | <0.001 | |
| Atrial fibrillation, n (%) | 1159 (23.0) | 639 (17.5) | 520 (37.4) | <0.001 | |
| History of pancreatitis, n (%) | 63 (1.2) | 49 (1.3) | 14 (1.0) | 0.339 | |
| Smoker, n (%) | 692 (13.7) | 462 (12.6) | 230 (16.5) | <0.001 | |
| TC, median (IQR), [mg/dL] | 159 (131–196) | 167 (137–202) | 143 (116–176) | <0.001 | |
| LDL-C, median (IQR), [mg/dL] | 96 (69–130) | 103 (76–136) | 78 (57–109) | <0.001 | |
| Non-HDL-C, median (IQR), [mg/dL] | 112 (88–146) | 117.5 (93–152) | 97 (76–127) | <0.001 | |
| apoB, median (IQR), [mg/dL] | 78 (63–99) | 81 (66–101) | 72 (57–90) | <0.001 | |
| HDL-C, median (IQR), [mg/dL] | 45 (36–55) | 46 (37–56) | 42 (33–52) | <0.001 | |
| TG, median (IQR), [mg/dL] | 97 (69–137) | 96 (68–134) | 101 (73.3–141.8) | <0.001 | |
| Lp(a), median (IQR), [mg/dL] | 11 (5–29) | 10 (5–26) | 14 (6–40) | <0.001 | |
| SCORE2/SCORE2-OP categories, n (%) | Low-to-moderate | 212 (16.8) * | 189 (18.5) | 23 (9.4) | <0.001 |
| High | 406 (32.1) * | 353 (34.6) | 53 (21.7) | ||
| Very high | 646 (51.1) * | 478 (46.9) | 168 (68.9) | ||
| Lipid-Lowering Therapy | N (%) |
|---|---|
| Single LLT | 1076 (77.3) |
| 1054 (75.7) |
| 689 (49.5) |
| HD (40–80 mg) | 210 (15.1) |
| LD (<40 mg) | 416 (29.9) |
| No info | 63 (4.5) |
| 353 (25.4) |
| HD (20–40 mg) | 186 (13.4) |
| LD (<20 mg) | 117 (8.4) |
| No info | 50 (3.6) |
| 11 (0.8) |
| 20–40 mg | 10 (0.7) |
| No info | 1 (0.1) |
| 1 (0.1) |
| 17 (1.2) |
| 5 (0.4) |
| Combined-Dual LLT | 313 (22.5) |
| 308 (22.1) |
| Atorvastatin/Rosuvastatin HD | 206 (14.8) |
| Other | 59 (4.2) |
| No info | 43 (3.1) |
| 4 (0.3) |
| Atorvastatin/Rosuvastatin HD | 2 (0.1) |
| Other | 2 (0.1) |
| No info | 0 (0.0) |
| 1 (0.1) |
| Combined-Triple LLT | |
| 3 (0.2) |
| Atorvastatin/Rosuvastatin HD | 3 |
| Total, n (%) | Without LLT, n (%) | With LLT, n (%) | OR [95% CI] | Mono-Therapy, n (%) | Combined Therapy, n (%) | OR [95% CI] | |
|---|---|---|---|---|---|---|---|
| Discordant apoB/LDL-C | 1193 (23.6) | 993 (27.2) | 200 (14.4) | 0.45 [0.38–0.53] | 170 (15.8) | 30 (9.5) | 0.56 [0.37–0.84] |
| Discordant apoB/non-HDL-C | 637 (12.6) | 527 (14.4) | 110 (7.9) | 0.51 [0.41–0.63] | 109 (10.1) | 19 (6.0) | 0.57 [0.34–0.94] |
| Discordant LDL-C/non-HDL-C | 660 (13.0) | 532 (14.6) | 128 (9.2) | 0.60 [0.49–0.73] | 92 (8.6) | 17 (5.4) | 0.60 [0.35–1.02] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Ziółkowski, M.; Obońska, K.; Ratajczak, J.; Adamski, P.; Banach, M.; Chlebus, K.; Grzelakowska, K.; Jankowski, P.; Krintus, M.; Kryś, J.; et al. Association Between Lipid-Lowering Therapy and Differences in the Distribution of LDL-C, apoB and non-HDL-C. J. Clin. Med. 2026, 15, 26. https://doi.org/10.3390/jcm15010026
Ziółkowski M, Obońska K, Ratajczak J, Adamski P, Banach M, Chlebus K, Grzelakowska K, Jankowski P, Krintus M, Kryś J, et al. Association Between Lipid-Lowering Therapy and Differences in the Distribution of LDL-C, apoB and non-HDL-C. Journal of Clinical Medicine. 2026; 15(1):26. https://doi.org/10.3390/jcm15010026
Chicago/Turabian StyleZiółkowski, Marcin, Karolina Obońska, Jakub Ratajczak, Piotr Adamski, Maciej Banach, Krzysztof Chlebus, Klaudyna Grzelakowska, Piotr Jankowski, Magdalena Krintus, Jacek Kryś, and et al. 2026. "Association Between Lipid-Lowering Therapy and Differences in the Distribution of LDL-C, apoB and non-HDL-C" Journal of Clinical Medicine 15, no. 1: 26. https://doi.org/10.3390/jcm15010026
APA StyleZiółkowski, M., Obońska, K., Ratajczak, J., Adamski, P., Banach, M., Chlebus, K., Grzelakowska, K., Jankowski, P., Krintus, M., Kryś, J., Laskowska, E., Mrzywka, N., Niezgoda, P., Ostrowska, M., Podhajski, P., Skonieczny, G., Sosnowska, B., Szarpak, Ł., Topolska, M., ... Kubica, J. (2026). Association Between Lipid-Lowering Therapy and Differences in the Distribution of LDL-C, apoB and non-HDL-C. Journal of Clinical Medicine, 15(1), 26. https://doi.org/10.3390/jcm15010026








