Headless Screw Fixation Is Associated with Reduced Hardware Removal After Tibial Tubercle Osteotomy: A Retrospective Cohort Study
Abstract
1. Introduction
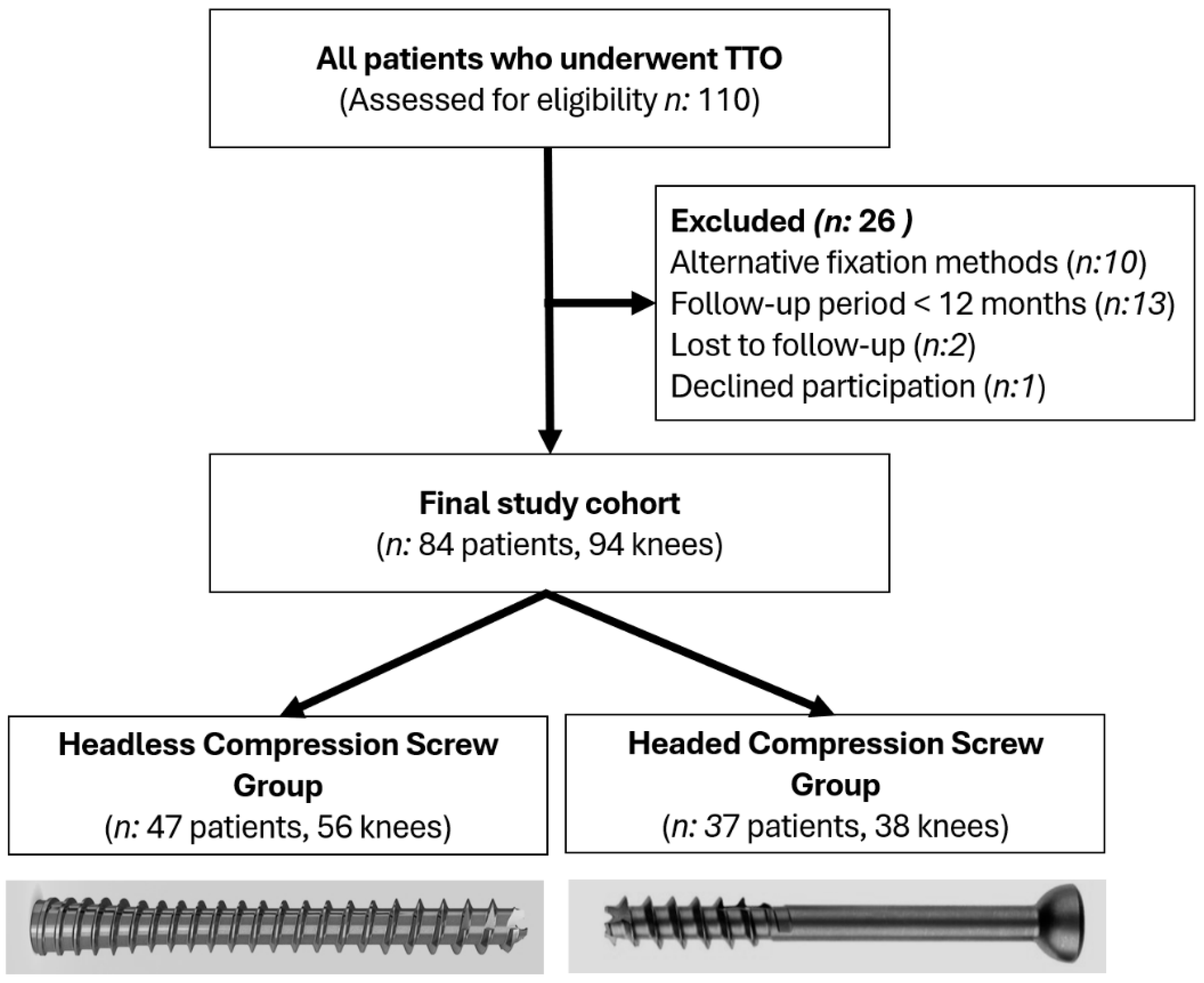
2. Materials and Methods
2.1. Patients and Study Design
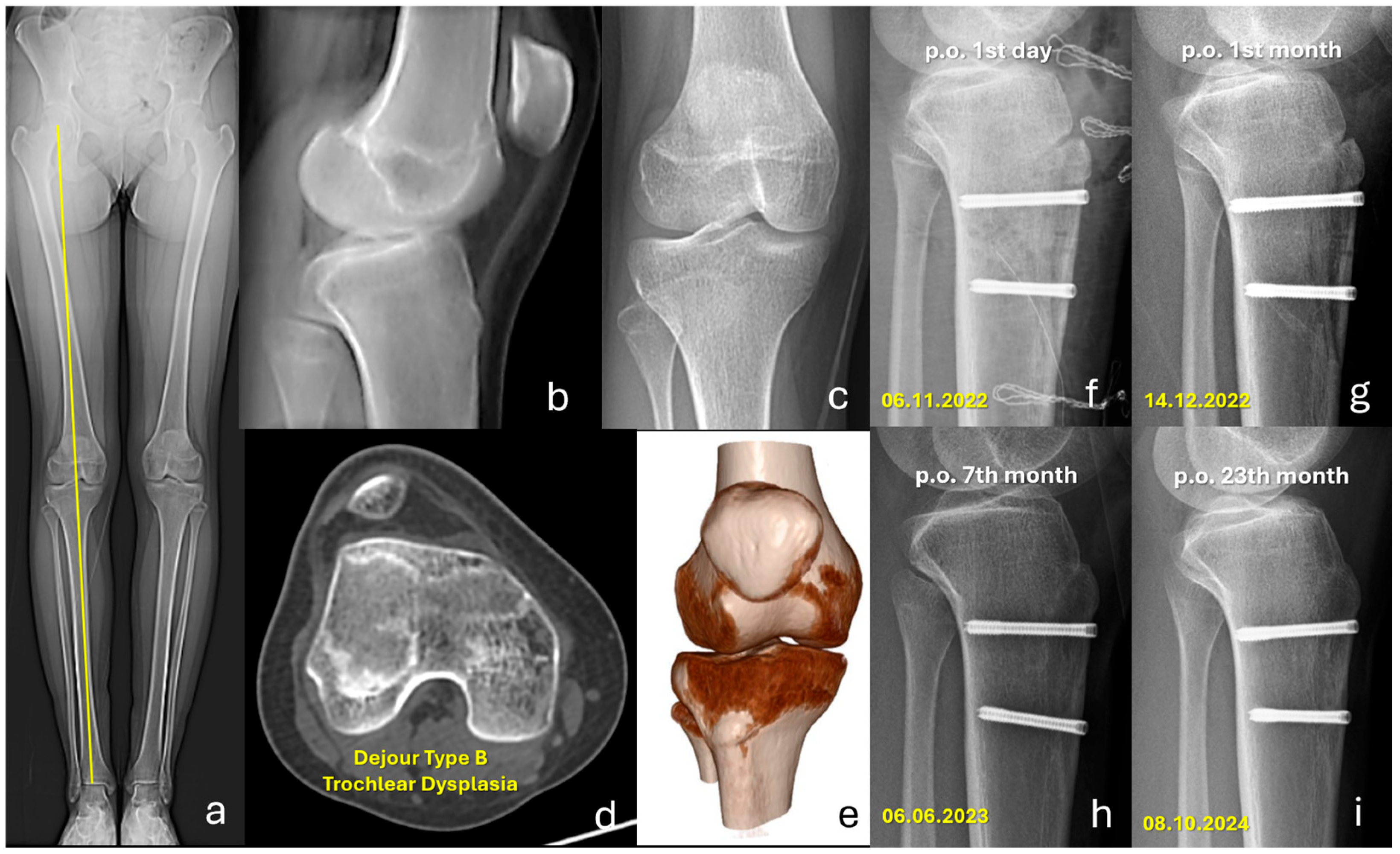
2.2. Surgical Technique and Implants
2.3. Postoperative Follow-Up
2.4. Radiological Assessments and Data Collection
2.5. Functional Outcome Assessments
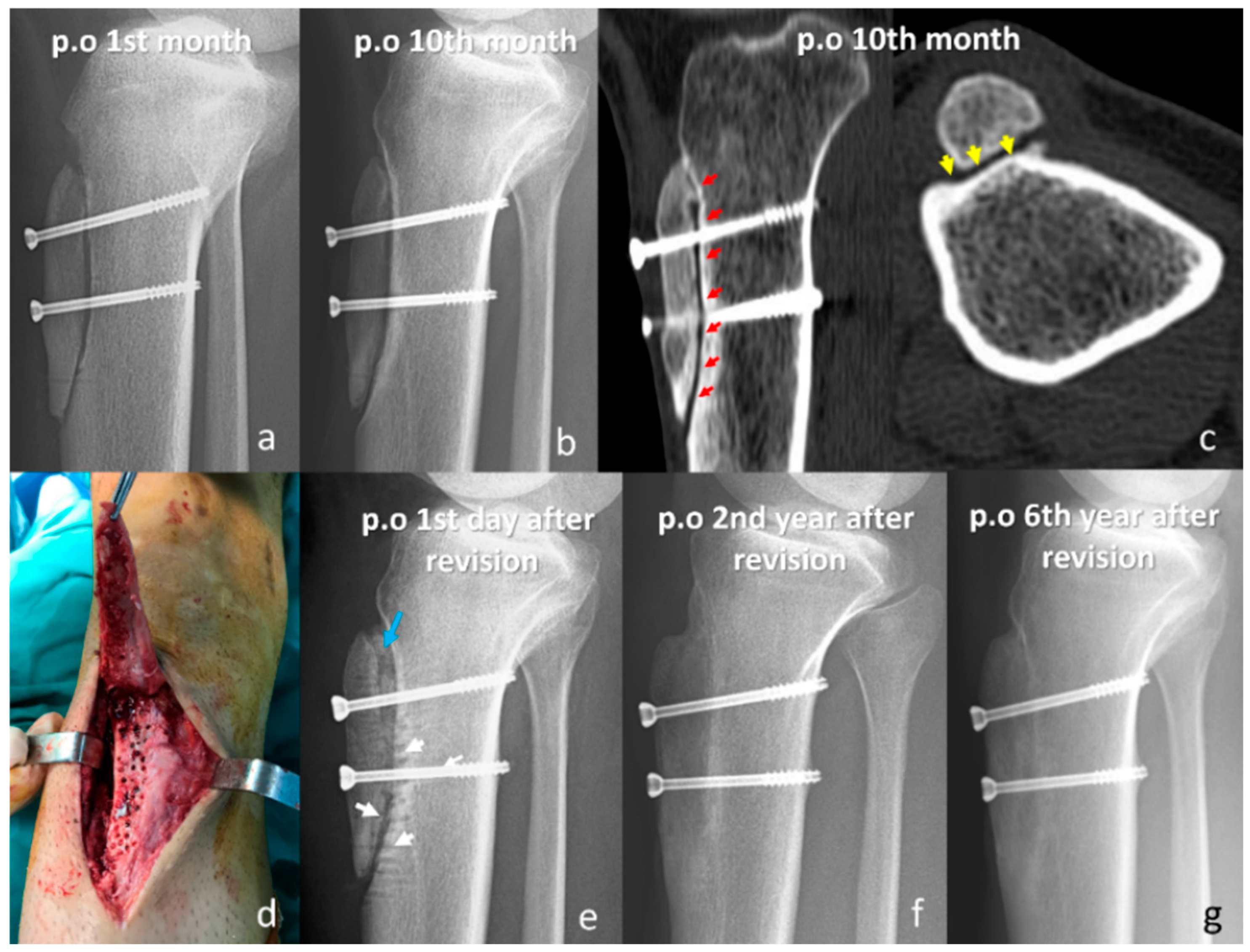
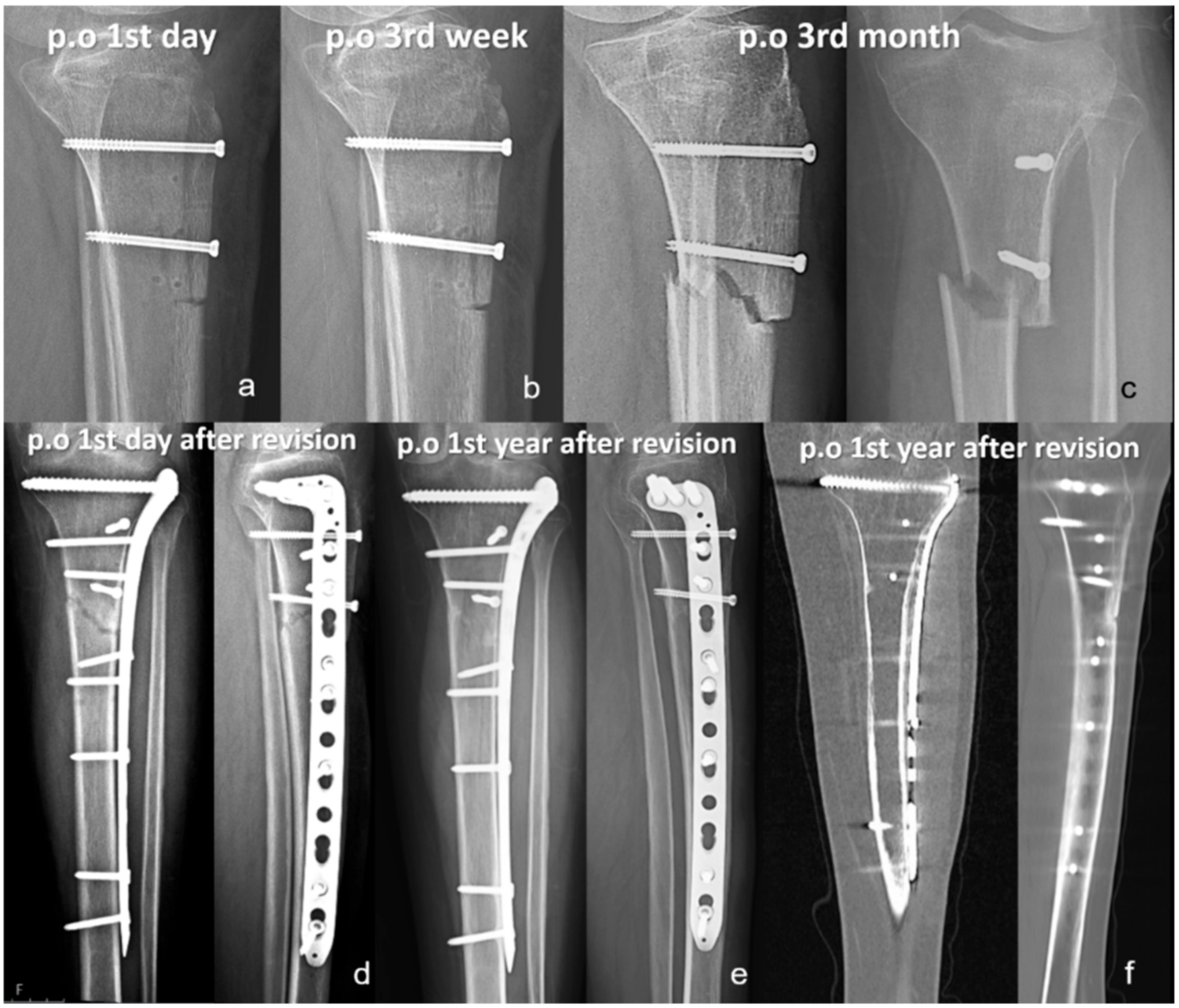
2.6. Assessment of Complications
2.7. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| TTO | Tibial Tubercle Osteotomy |
| PFI | Patellofemoral Instability |
| MPFL | Medial Patellofemoral Ligament |
| MPFLR | Medial Patellofemoral Ligament Reconstruction |
| TT-TG | Tibial Tuberosity-Trochlear Groove |
| ROM | Range of Motion |
| MRI | Magnetic Resonance Imaging |
| CT | Computed Tomography |
| MAD | Mechanical Axis Deviation |
| ASA | American Society of Anesthesiologists |
| VAS | Visual Analog Scale |
References
- Gravesen, K.S.; Kallemose, T.; Blønd, L.; Troelsen, A.; Barfod, K.W. High incidence of acute and recurrent patellar dislocations: A retrospective nationwide epidemiological study involving 24.154 primary dislocations. Knee Surg. Sports Traumatol. Arthrosc. 2018, 26, 1204–1209. [Google Scholar] [CrossRef] [PubMed]
- Huntington, L.S.; Webster, K.E.; Devitt, B.M.; Scanlon, J.P.; Feller, J.A. Factors Associated With an Increased Risk of Recurrence After a First-Time Patellar Dislocation: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2020, 48, 2552–2562. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.Y.; Ding, H.Y.; Li, E.M.; Zheng, L.; Bai, Z.W.; Shi, H.; Fan, F.J.; Guo, D. Incidence of second-time lateral patellar dislocation is associated with anatomic factors, age and injury patterns of medial patellofemoral ligament in first-time lateral patellar dislocation: A prospective magnetic resonance imaging study with 5-year follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 197–205. [Google Scholar] [CrossRef] [PubMed]
- Danielsen, O.; Poulsen, T.A.; Eysturoy, N.H.; Mortensen, E.S.; Hölmich, P.; Barfod, K.W. Trochlea dysplasia, increased TT-TG distance and patella alta are risk factors for developing first-time and recurrent patella dislocation: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2023, 31, 3806–3846. [Google Scholar] [CrossRef] [PubMed]
- Desio, S.M.; Burks, R.T.; Bachus, K.N. Soft tissue restraints to lateral patellar translation in the human knee. Am. J. Sports Med. 1998, 26, 59–65. [Google Scholar] [CrossRef]
- Kluczynski, M.A.; Miranda, L.; Marzo, J.M. Prevalence and Site of Medial Patellofemoral Ligament Injuries in Patients With Acute Lateral Patellar Dislocations: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2020, 8, 2325967120967338. [Google Scholar] [CrossRef]
- Blønd, L.; Askenberger, M.; Stephen, J.; Akmeşe, R.; Balcarek, P.; El Attal, R.; Chouliaras, V.; Ferrua, P.; Monart, J.M.; Pagenstert, G.; et al. Management of first-time patellar dislocation: The ESSKA 2024 formal consensus-Part 1. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 1925–1932. [Google Scholar] [CrossRef]
- Balcarek, P.; Blønd, L.; Beaufils, P.; Askenberger, M.; Stephen, J.M.; Akmeşe, R.; El Attal, R.; Chouliaras, V.; Ferrua, P.; Minguell Monart, J.; et al. Management of first-time patellar dislocation: The ESSKA 2024 formal consensus-Part 2. Knee Surg. Sports Traumatol. Arthrosc. 2025, 33, 4197–4206. [Google Scholar] [CrossRef]
- Dejour, D.H.; Mesnard, G.; Giovannetti de Sanctis, E. Updated treatment guidelines for patellar instability: “un menu à la carte”. J. Exp. Orthop. 2021, 8, 109. [Google Scholar] [CrossRef]
- Stokes, D.J.; Elrick, B.P.; Carpenter, M.L.; Raji, Y.; McQuivey, K.S.; Sherman, S.L.; Frank, R.M. Tibial Tubercle Osteotomy: Indications, Outcomes, and Complications. Curr. Rev. Musculoskelet. Med. 2024, 17, 484–495. [Google Scholar] [CrossRef]
- Meng, X.; Ji, Z.; Wu, P.; Fang, H.; Zhao, P.; Ding, Y.; Wang, Z. Combining tibial tubercle osteotomy with medial patellofemoral ligament reconstruction often yields better outcomes in treating patellofemoral instability: A systematic review and meta-analysis of case-control studies. J. Orthop. Surg. Res. 2024, 19, 695. [Google Scholar] [CrossRef] [PubMed]
- Knapik, D.M.; Kunze, K.N.; Azua, E.; Vadhera, A.; Yanke, A.B.; Chahla, J. Radiographic and Clinical Outcomes After Tibial Tubercle Osteotomy for the Treatment of Patella Alta: A Systematic Review and Meta-analysis. Am. J. Sports Med. 2022, 50, 2042–2051. [Google Scholar] [CrossRef] [PubMed]
- Saltzman, B.M.; Rao, A.; Erickson, B.J.; Cvetanovich, G.L.; Levy, D.; Bach, B.R., Jr.; Cole, B.J. A Systematic Review of 21 Tibial Tubercle Osteotomy Studies and More Than 1000 Knees: Indications, Clinical Outcomes, Complications, and Reoperations. Am. J. Orthop. 2017, 46, E396–E407. [Google Scholar] [PubMed]
- Payne, J.; Rimmke, N.; Schmitt, L.C.; Flanigan, D.C.; Magnussen, R.A. The Incidence of Complications of Tibial Tubercle Osteotomy: A Systematic Review. Arthroscopy 2015, 31, 1819–1825. [Google Scholar] [CrossRef]
- Lundeen, A.; Macalena, J.; Agel, J.; Arendt, E. High incidence of complication following tibial tubercle surgery. J. ISAKOS 2023, 8, 81–85. [Google Scholar] [CrossRef]
- Pesante, B.D.; Ward, B.A.; Stacey, S.C.; Parry, J.A. A Retrospective Comparison of Headless Versus Standard Interlocking Screw Fixation of Tibia Intramedullary Nails. J. Am. Acad. Orthop. Surg. 2025, 33, 145–149. [Google Scholar] [CrossRef]
- Bulut, T.; Gursoy, M.; Ertem, H. Fully threaded headless compression screw versus partially threaded cancellous lag screw in medial malleolus fractures: Clinical and radiological outcomes. Eur. J. Trauma Emerg. Surg. 2021, 47, 179–185. [Google Scholar] [CrossRef]
- Lehane, K.; Wolfe, I.; Buseck, A.; Moore, M.R.; Chen, L.; Strauss, E.J.; Jazrawi, L.M.; Golant, A. Predictors of Increased Complication Rate Following Tibial Tubercle Osteotomy (TTO). Knee 2025, 53, 93–102. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann. Intern. Med. 2007, 147, 573–577, Erratum in Ann. Intern. Med. 2008, 148, 168. [Google Scholar] [CrossRef]
- Dejour, D.; Reynaud, P.; Lecoultre, B. Douleurs et instabilitè rotulienne: Essai de classification. Med. Hyg. 1998, 56, 1466–1471. [Google Scholar]
- Caton, J. Méthode de mesure de la hauteur de la rotule [Method of measuring the height of the patella]. Acta Orthop. Belg. 1989, 55, 385–386. [Google Scholar]
- Kujala, U.M.; Jaakkola, L.H.; Koskinen, S.K.; Taimela, S.; Hurme, M.; Nelimarkka, O. Scoring of patellofemoral disorders. Arthroscopy 1993, 9, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Kuru, T.; Dereli, E.E.; Yaliman, A. Validity of the Turkish version of the Kujala patellofemoral score in patellofemoral pain syndrome. Acta Orthop. Traumatol. Turc. 2010, 44, 152–156. [Google Scholar] [CrossRef] [PubMed]
- Tegner, Y.; Lysholm, J. Rating systems in the evaluation of knee ligament injuries. Clin. Orthop. Relat. Res. 1985, 198, 43–49. [Google Scholar] [CrossRef]
- Celik, D.; Coşkunsu, D.; Kiliçoğlu, O. Translation and cultural adaptation of the Turkish Lysholm knee scale: Ease of use, validity, and reliability. Clin. Orthop. Relat. Res. 2013, 471, 2602–2610. [Google Scholar] [CrossRef]
- Quinn, J.V.; Drzewiecki, A.E.; Stiell, I.G.; Elmslie, T.J. Appearance scales to measure cosmetic outcomes of healed lacerations. Am. J. Emerg. Med. 1995, 13, 229–231. [Google Scholar] [CrossRef]
- Davis, M.; Meta, F.; Dancy, M.E.; Scott, P.A.; Pan, X.; Tagliero, A.J.; Krych, A.J.; Hevesi, M.; Okoroha, K.R. Pain and Hardware Removal After Tibial Tubercle Osteotomy: Incidence, Associated Factors, and Outcomes. Orthop. J. Sports Med. 2025, 13, 23259671251324481. [Google Scholar] [CrossRef]
- Johnson, A.A.; Wolfe, E.L.; Mintz, D.N.; Demehri, S.; Shubin Stein, B.E.; Cosgarea, A.J. Complications After Tibial Tuberosity Osteotomy: Association With Screw Size and Concomitant Distalization. Orthop. J. Sports Med. 2018, 6, 2325967118803614. [Google Scholar] [CrossRef]
- Assari, S.; Darvish, K.; Ilyas, A.M. Biomechanical analysis of second-generation headless compression screws. Injury 2012, 43, 1159–1165. [Google Scholar] [CrossRef]
- Wheeler, D.L.; McLoughlin, S.W. Biomechanical assessment of compression screws. Clin. Orthop. Relat. Res. 1998, 350, 237–245. [Google Scholar] [CrossRef]
| Variables | Headless Screws (# of Knees: 56) | Headed Screws (# of Knees: 38) | p-Value |
|---|---|---|---|
| Age (years ± SD) | 20.4 ± 6.7 | 22.3 ± 10.2 | 0.537 1 |
| Sex (n, %) | 0.348 2 | ||
| Male | 13 (23.2%) | 11 (28.9%) | |
| Female | 43 (76.8%) | 27 (71.1%) | |
| Side | 0.480 2 | ||
| Right | 25 (44.6%) | 18 (47.4%) | |
| Left | 31 (55.4%) | 20 (52.6%) | |
| Weight (kg ± SD) | 65.2 ± 12.6 | 66.4 ± 12.7 | 0.656 1 |
| Height (cm ± SD) | 165.2 ± 8.6 | 164.6 ± 9.6 | 0.648 3 |
| BMI (kg/m2 ± SD) | 23.9 ± 4.4 | 24.6 ± 5.1 | 0.473 3 |
| Acute vs. Recurrent (n, %) | 0.331 2 | ||
| Acute | 17 (30.4%) | 14 (36.8%) | |
| Recurrent | 39 (69.6%) | 24 (63.2%) | |
| Tobacco users (n, %) | 10 (17.9%) | 8 (21.1%) | 0.448 2 |
| Diabetes Mellitus (n, %) | 1 (1.8%) | 0 (0%) | 0.596 2 |
| ASA Score | 0.662 2 | ||
| ASA I | 41 (73.2%) | 27 (71.1%) | |
| ASA II | 14 (25.0%) | 11 (28.9%) | |
| ASA III | 1 (1.8%) | 0 (0%) | |
| TT-TG Distance (mm ± SD) | 20.6 ± 3.5 | 19.9 ± 3.9 | 0.355 3 |
| Dejour Classification (n, %) | 0.103 3 | ||
| Type A | 15 (26.8%) | 5 (13.2%) | |
| Type B | 17 (30.4%) | 15 (39.5%) | |
| Type C | 15 (26.8%) | 6 (15.8%) | |
| Type D | 9 (16.1%) | 12 (31.6%) | |
| Caton–Deschamps Index | 1.16 ± 0.17 | 1.11 ± 0.16 | 0.190 3 |
| Patella Alta (n, %) | 21 (37.5%) | 12 (31.6%) | 0.357 2 |
| Patellar Tilt (° ± SD) | 31.3 ± 10.9 | 31.7 ± 10.6 | 0.860 3 |
| Limb Alignment (n, %) | 0.351 2 | ||
| Normal | 35 (62.55) | 21 (55.3%) | |
| Varus | 9 (16.1%) | 4 (10.5%) | |
| Valgus | 12 (21.4%) | 13 (34.2%) | |
| Prior Surgery (n, %) | 4 (7.1%) | 4 (10.5%) | 0.414 2 |
| Variables | Headless Screws (# of Knees: 56) | Headed Screws (# of Knees: 38) | p-Value |
|---|---|---|---|
| Length of Osteotomy (cm ± SD) | 7.9 ± 0.8 | 7.5 ± 1.5 | 0.067 1 |
| Osteotomy Shape (n, %) | 0.001 2 | ||
| Greenstick | 43 (76.8%) | 17 (44.7%) | |
| Slopped | 13 (23.2%) | 4 (10.5%) | |
| Blunt | 0 (0%) | 17 (44.7%) | |
| Number of Screws (n, %) | 0.001 2 | ||
| Two-screw fixation | 20 (35.7%) | 31 (81.6%) | |
| Three-screw fixation | 36 (64.3%) | 7 (18.4%) | |
| Screw Size ** (n, %) | 0.011 2 | ||
| 3.5 mm | - | 7 (8.5%) | |
| 4.5 mm | 148 (100%) | 76 (91.5%) | |
| Concomitant interventions (n, %) | |||
| MPFLR | 55 (98.2%) | 31 (73.7%) | 0.007 2 |
| Lateral Lengthening | 5 (8.9%) | 14 (36.8%) | 0.001 2 |
| Patellar OCF Removal | 3 (5.4%) | 2 (5.3%) | 0.679 2 |
| Patellar OCF Fixation | 1 (1.8%) | 2 (5.3%) | 0.357 2 |
| Distalization | 1 (1.8%) | 3 (7.9%) | 0.300 2 |
| MPFL Graft Option * (n, %) | 0.564 2 | ||
| Gracilis | 54 (98.2%) | 27 (96.4%) | |
| AHPLT | 1 (1.8%) | 1 (3.6%) | |
| Double vs. Single Bundle MPFLR * | 0.548 2 | ||
| Single | 48 (87.3%) | 25 (89.3%) | |
| Double | 7 (12.7%) | 3 (10.7%) | |
| Duration of Operation (min ± SD) | 95.8 ± 11.6 | 106.8 ± 15.9 | 0.001 1 |
| Anesthesia type | 0.520 2 | ||
| Spinal | 49 (87.5%) | 34 (89.5%) | |
| General | 7 (12.5%) | 4 (10.5%) | |
| LOS (days ± SD) | 1.4 ± 0.7 | 2.1 ± 0.8 | 0.001 1 |
| Variables | Headless Screws (# of Knees: 56) | Headed Screws (# of Knees: 38) | p-Value |
|---|---|---|---|
| Clinical Follow-up (months ± SD) | 21.8 ± 6.7 | 62.1 ± 30.3 | 0.001 1 |
| Radiological Follow-up (months ± SD) | 19.6 ± 5.9 | 45.8 ± 24.5 | 0.001 1 |
| Preop Kujala Score (points ± SD) | 55.4 ± 19.7 | 49.3 ± 20.0 | 0.176 1 |
| Postop Kujala Score (points ± SD) | 94.0 ± 7.6 | 92.6 ± 8.7 | 0.650 1 |
| p-value * | 0.001 2 | 0.001 2 | |
| Preop Lysholm Knee Score (points ± SD) | 58.2 ± 15.8 | 53.8 ± 16.9 | 0.228 1 |
| Postop Lysholm Knee Score (points ± SD) | 94.4 ± 5.6 | 94.6 ± 6.2 | 0.782 1 |
| p-value * | 0.001 2 | 0.001 2 | |
| Preop Tegner Activity Scale (points ± SD) | 5.9 ± 1.8 | 6.1 ± 1.7 | 0.697 1 |
| Postop Tegner Activity Scale (points ± SD) | 5.4 ± 1.5 | 5.0 ± 1.2 | 0.260 1 |
| p-value * | 0.016 2 | 0.001 2 | |
| Postop Tegner Activity Scale | 0.454 3 | ||
| Remained unchanged | 35 (62.5%) | 19 (50.0%) | |
| Decreased | 18 (32.1%) | 17 (44.7%) | |
| Increased | 3 (5.4%) | 2 (5.3%) | |
| Knee ROM Deficit (n, %) | NA | ||
| Flexion | 0 (0%) | 0 (0%) | |
| Extension | 0 (0%) | 0 (0%) | |
| Manual Muscle Strength Deficit (n, %) | 0 (0%) | 0 (0%) | NA |
| Thigh Atrophy | 0 (0%) | 0 (0%) | NA |
| J-Sign at Final Follow-up (n, %) | 0.449 | ||
| None | 45 (80.4%) | 33 (86.8%) | |
| Mild | 9 (16.1%) | 5 (13.2%) | |
| Moderate | 2 (3.6%) | 0 (0%) | |
| Severe | 0 (0%) | 0 (0%) | |
| Positive Apprehension Test (n, %) | 0.212 3 | ||
| Mild | 6 (10.7%) | 3 (7.9%) | |
| Moderate | 2 (3.6%) | 5 (13.2%) | |
| Positive Giving way (n, %) | 0 (0%) | 1 (2.6%) | 0.404 3 |
| Positive Patellar Grinding Test (n, %) | 0 (0%) | 0 (0%) | NA |
| Overall Satisfaction (points ± SD) | 9.2 ± 1.1 | 9.0 ± 2.3 | 0.262 1 |
| Cosmetic Satisfaction (points ± SD) | 7.6 ± 2.3 | 7.5 ± 2.5 | 0.925 1 |
| Variables | Headless Screws (# of Knees: 56) | Headed Screws (# of Knees: 38) | p-Value |
|---|---|---|---|
| Non-Union (n, %) | 0 (0%) | 1 (2.6%) | 0.404 1 |
| Fracture (n, %) | 0 (0%) | 1 (2.6%) | 0.404 1 |
| Recurrent Instability (n, %) | 2 (3.6%) | 2 (5.3%) | 0.534 1 |
| Superficial Infection (n, %) | 2 (3.6%) | 1 (2.6%) | 0.799 1 |
| Deep Infection (n, %) | 0 (0%) | 0 (0%) | NA |
| Pulmonary Embolism (n, %) | 0 (0%) | 1 (2.6%) | 0.404 1 |
| Hypoesthesia (n, %) | 27 (48.2%) | 13 (34.2%) | 0.127 1 |
| Arthrofibrosis (n, %) | 0 (0%) | 1 (2.6%) | 0.404 1 |
| Hypertrophic Scar/Keloid (n, %) | 0 (0%) | 0 (0%) | NA |
| Painful Implant Removal (n, %) | 0 (0%) | 5 (13.2%) | 0.009 1 |
| Reoperation excluding implant removal (n, %) | 2 (3.6%) | 5 (13.2%) | 0.092 1 |
| Reoperation for any reason (n, %) | 2 (3.6%) | 10 (26.3%) | 0.002 1 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Uslu, O.; Kose, O. Headless Screw Fixation Is Associated with Reduced Hardware Removal After Tibial Tubercle Osteotomy: A Retrospective Cohort Study. J. Clin. Med. 2026, 15, 235. https://doi.org/10.3390/jcm15010235
Uslu O, Kose O. Headless Screw Fixation Is Associated with Reduced Hardware Removal After Tibial Tubercle Osteotomy: A Retrospective Cohort Study. Journal of Clinical Medicine. 2026; 15(1):235. https://doi.org/10.3390/jcm15010235
Chicago/Turabian StyleUslu, Oguzhan, and Ozkan Kose. 2026. "Headless Screw Fixation Is Associated with Reduced Hardware Removal After Tibial Tubercle Osteotomy: A Retrospective Cohort Study" Journal of Clinical Medicine 15, no. 1: 235. https://doi.org/10.3390/jcm15010235
APA StyleUslu, O., & Kose, O. (2026). Headless Screw Fixation Is Associated with Reduced Hardware Removal After Tibial Tubercle Osteotomy: A Retrospective Cohort Study. Journal of Clinical Medicine, 15(1), 235. https://doi.org/10.3390/jcm15010235






