Toward Equitable Kidney Care: Insights from the Survey Among Polish Doctors on the Women’s Health in Chronic Kidney Disease Management
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. General Part of the Survey for All Specialists
3.1.1. Demographical Data and Patients’ Profile
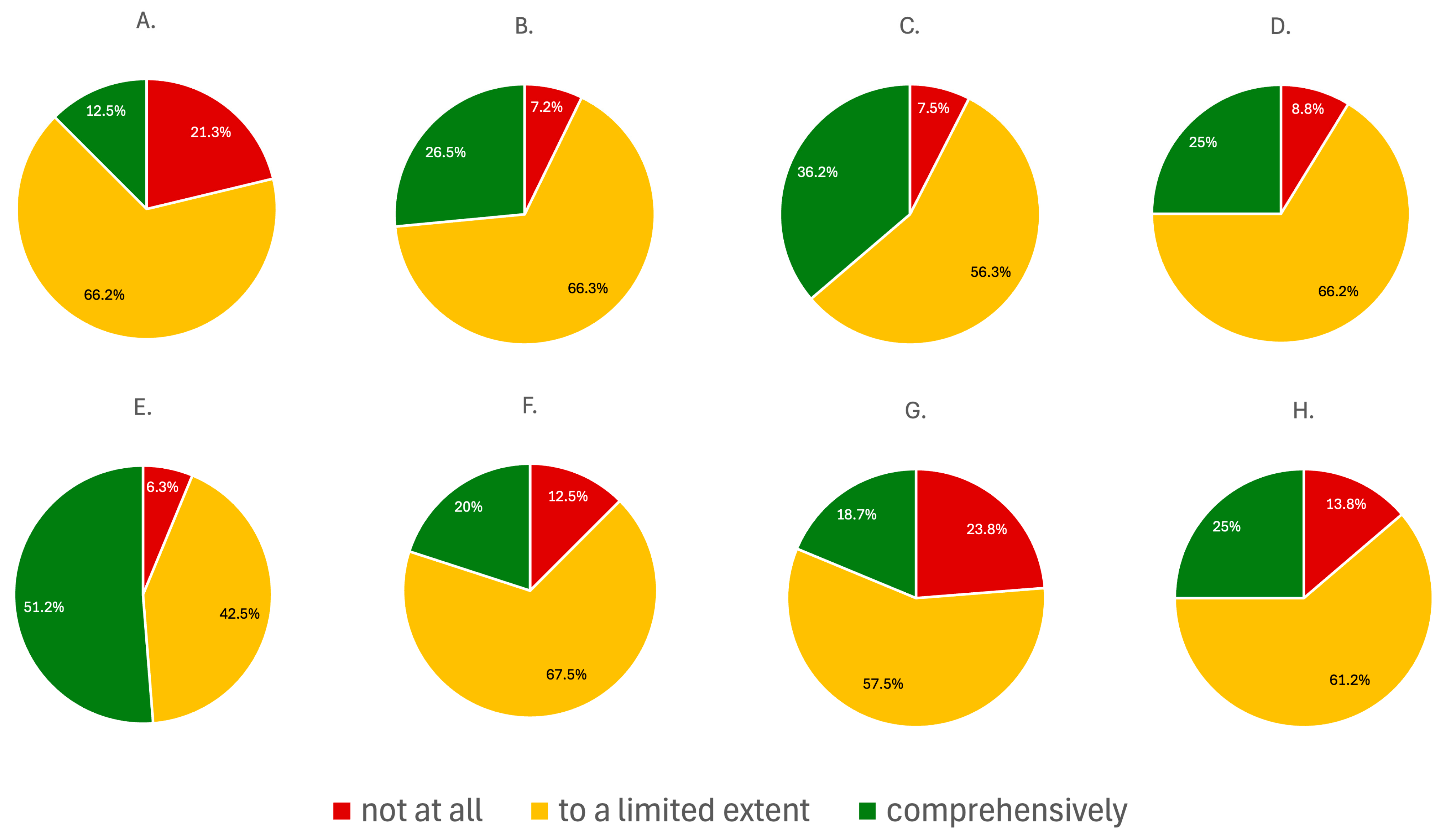
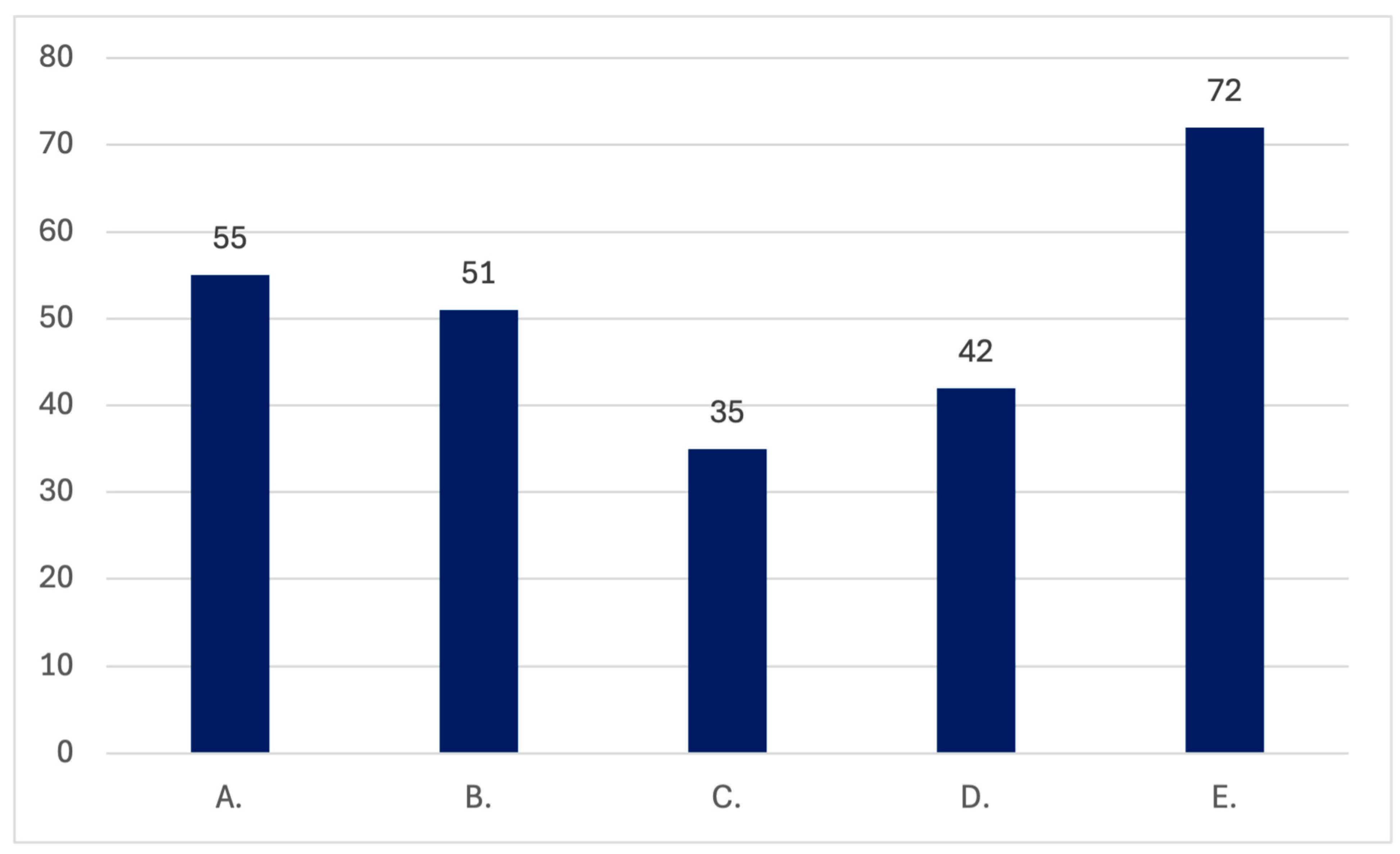
3.1.2. Level of the Clinical Experience in the Management of Patients with CKD Across Various Specialties
3.1.3. Women’s Health-Related Issues in Medical History
3.1.4. Survey Insights on Angiotensin-Converting Enzyme Inhibitors or Angiotensin II Receptor Blockers ACE-I/ARBs Use
3.2. Responses to Nephrologist-Specific Questions
3.2.1. The Assessment of Focus on Women’s Health-Related Issues During Residency Training
3.2.2. Level of the Clinical Experience in the Management of Women’s Health
3.2.3. The Assessment of the Opinions on the Need to Implement More Women’s Health-Related Issues into the Nephrology Care in Poland
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| ACE-I/ARBs | angiotensin-converting enzyme inhibitors or angiotensin II receptor blockers |
| ART | assisted reproductive technologies |
| CKD | chronic kidney disease |
| eGFR | estimated glomerular filtration rate |
| EULAR | European Alliance of Associations for Rheumatology |
| GnRHa | gonadotropin-releasing hormone agonists |
| HELIUS | Healthy Life in an Urban Setting |
| KDIGO | Kidney Disease: Improving Global Outcomes |
| MMG | mammography |
| NCD | noncommunicable disease |
| OTC | ovarian tissue cryopreservation |
| uACR | urinary albumin-to-creatinine ratio |
| USA | the United States of America |
| USG | ultrasound |
| WHO | World Health Organisation |
References
- Bikbov, B.; Purcell, C.A.; Levey, A.S.; Smith, M.; Abdoli, A.; Abebe, M.; Adebayo, O.M.; Afarideh, M.; Agarwal, S.K.; Agudelo-Botero, M.; et al. Global, Regional, and National Burden of Chronic Kidney Disease, 1990–2017: A Systematic Analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef]
- Reducing the Burden of Noncommunicable Diseases Through Promotion of Kidney Health and Strengthening Prevention and Control of Kidney Disease. Available online: https://apps.who.int/gb/ebwha/pdf_files/EB156/B156_CONF6-en.pdf (accessed on 1 September 2025).
- Francis, A.; Harhay, M.N.; Ong, A.C.M.; Tummalapalli, S.L.; Ortiz, A.; Fogo, A.B.; Fliser, D.; Roy-Chaudhury, P.; Fontana, M.; Nangaku, M.; et al. Chronic Kidney Disease and the Global Public Health Agenda: An International Consensus. Nat. Rev. Nephrol. 2024, 20, 473–485. [Google Scholar] [CrossRef] [PubMed]
- Lou-Meda, R.; Pérez, J.B. Reducing the Burden of Chronic Kidney Disease in the World. Lancet 2025, 405, 1810. [Google Scholar] [CrossRef]
- Deng, L.; Guo, S.; Liu, Y.; Zhou, Y.; Liu, Y.; Zheng, X.; Yu, X.; Shuai, P. Global, Regional, and National Burden of Chronic Kidney Disease and Its Underlying Etiologies from 1990 to 2021: A Systematic Analysis for the Global Burden of Disease Study 2021. BMC Public Health 2025, 25, 636. [Google Scholar] [CrossRef]
- Carrero, J.J.; Hecking, M.; Chesnaye, N.C.; Jager, K.J. Sex and Gender Disparities in the Epidemiology and Outcomes of Chronic Kidney Disease. Nat. Rev. Nephrol. 2018, 14, 151–164. [Google Scholar] [CrossRef]
- Vosters, T.G.; Kingma, F.M.; Stel, V.S.; Jager, K.J.; van Ittersum, F.J.; van den Born, B.-J.H.; Vogt, L.; van Valkengoed, I.G.M. The Association and Contribution of Gender-Related Characteristics to Prevalent Chronic Kidney Disease in Women and Men in a Multi-Ethnic Population—The HELIUS Study. BMC Public Health 2025, 25, 853. [Google Scholar] [CrossRef]
- Tong, A.; Evangelidis, N.; Kurnikowski, A.; Lewandowski, M.; Bretschneider, P.; Oberbauer, R.; Baumgart, A.; Scholes-Robertson, N.; Stamm, T.; Carrero, J.J.; et al. Nephrologists’ Perspectives on Gender Disparities in CKD and Dialysis. Kidney Int. Rep. 2022, 7, 424–435. [Google Scholar] [CrossRef] [PubMed]
- Prejbisz, A.; Dobrowolski, P.; Doroszko, A.; Olszanecka, A.; Tycińska, A.; Tykarski, A.; Adamczak, M.; Begier-Krasińska, B.; Chrostowska, M.; Dzida, G.; et al. Guidelines for the Management of Hypertension in Poland 2024—The Position of the Polish Society of Hypertension/Polish Cardiac Society Experts. Arter. Hypertens. 2024, 28, 91–146. [Google Scholar] [CrossRef]
- Piccoli, G.B.; Ahmed, S.B.; Fakhouri, F.; Garovic, V.D.; Hladunewich, M.A.; Jesudason, S.; Prakash, J.; Webster, A.C.; Zakharova, E.; Cheung, M.; et al. Women and Kidney Health: Conclusions from a Kidney Disease: Improving Global Outcomes (KDIGO) Controversies Conference. Kidney Int. 2025, 108, 355–379. [Google Scholar] [CrossRef] [PubMed]
- Pinho-Gomes, A.-C.; Carcel, C.; Woodward, M.; Hockham, C. Women’s Representation in Clinical Trials of Patients with Chronic Kidney Disease. Clin. Kidney J. 2023, 16, 1457–1464. [Google Scholar] [CrossRef]
- Zucker, I.; Prendergast, B.J. Sex Differences in Pharmacokinetics Predict Adverse Drug Reactions in Women. Biol. Sex Differ. 2020, 11, 32. [Google Scholar] [CrossRef]
- Hendren, E.M.; Reynolds, M.L.; Mariani, L.H.; Zee, J.; O’Shaughnessy, M.M.; Oliverio, A.L.; Moore, N.W.; Hill-Callahan, P.; Rizk, D.V.; Almanni, S.; et al. Confidence in Women’s Health: A Cross Border Survey of Adult Nephrologists. J. Clin. Med. 2019, 8, 176. [Google Scholar] [CrossRef]
- Ramesh, S.; James, M.T.; Holroyd-Leduc, J.M.; Wilton, S.B.; Seely, E.W.; Wheeler, D.C.; Ahmed, S.B. Sex Hormone Status in Women with Chronic Kidney Disease: Survey of Nephrologists’ and Renal Allied Health Care Providers’ Perceptions. Can. J. Kidney Health Dis. 2017, 4, 2054358117734534. [Google Scholar] [CrossRef]
- Duffner, J.; Schulte-Kemna, L.; Reister, B.; Ludwig, U.; Keller, F.; Erp, R.V.; Schröppel, B. Survey among Nephrologists in Germany: Current Practice and Management of Pregnant Women on Dialysis. Clin. Nephrol. 2017, 88, 264–269. [Google Scholar] [CrossRef] [PubMed]
- Jazienicka, A.; Babicki, M.; Krajewska, M.; Oko, A.; Kłoda, K.; Biesiada, A.; Mastalerz-Migas, A. A Nationwide Epidemiological Study of Chronic Kidney Disease Prevalence in a High-Risk Patient Population Without Prior Diagnosis in Primary Health Care in Poland. J. Clin. Med. 2025, 14, 3600. [Google Scholar] [CrossRef]
- Jazienicka-Kiełb, A.; Babicki, M.; Krajewska, M.; Oko, A.; Kłoda, K.; Mastalerz-Migas, A. Assessment of Primary Care Physicians’ Knowledge of Chronic Kidney Disease in Poland. Front. Public Health 2022, 10, 1032240. [Google Scholar] [CrossRef] [PubMed]
- Perez-Garcia, L.F.; Dolhain, R.J.E.M.; Vorstenbosch, S.; Bramer, W.; Van Puijenbroek, E.; Hazes, J.M.W.; Te Winkel, B. The Effect of Paternal Exposure to Immunosuppressive Drugs on Sexual Function, Reproductive Hormones, Fertility, Pregnancy and Offspring Outcomes: A Systematic Review. Hum. Reprod. Update 2020, 26, 961–1001. [Google Scholar] [CrossRef]
- Stevens, P.E.; Ahmed, S.B.; Carrero, J.J.; Foster, B.; Francis, A.; Hall, R.K.; Herrington, W.G.; Hill, G.; Inker, L.A.; Kazancıoğlu, R.; et al. KDIGO 2024 Clinical Practice Guideline for the Evaluation and Management of Chronic Kidney Disease. Kidney Int. 2024, 105, S117–S314. [Google Scholar] [CrossRef]
- McEvoy, J.W.; McCarthy, C.P.; Bruno, R.M.; Brouwers, S.; Canavan, M.D.; Ceconi, C.; Christodorescu, R.M.; Daskalopoulou, S.S.; Ferro, C.J.; Gerdts, E.; et al. 2024 ESC Guidelines for the Management of Elevated Blood Pressure and Hypertension. Eur. Heart J. 2024, 45, 3912–4018. [Google Scholar] [CrossRef] [PubMed]
- Countouris, M.; Mahmoud, Z.; Cohen, J.B.; Crousillat, D.; Hameed, A.B.; Harrington, C.M.; Hauspurg, A.; Honigberg, M.C.; Lewey, J.; Lindley, K.; et al. Hypertension in Pregnancy and Postpartum: Current Standards and Opportunities to Improve Care. Circulation 2025, 151, 490–507. [Google Scholar] [CrossRef]
- Lovegrove, E.; Robson, J.; McGettigan, P. Pregnancy Protection and Pregnancies in Women Prescribed ACE Inhibitors or ARBs: A Cross-Sectional Study in Primary Care. Br. J. Gen. Pract. 2020, 70, e778–e784. [Google Scholar] [CrossRef]
- Webster, P.; Lightstone, L.; McKay, D.B.; Josephson, M.A. Pregnancy in Chronic Kidney Disease and Kidney Transplantation. Kidney Int. 2017, 91, 1047–1056. [Google Scholar] [CrossRef]
- Vrijlandt, W.A.L.; De Jong, M.F.C.; Prins, J.R.; Bramham, K.; Vrijlandt, P.J.W.S.; Janse, R.J.; Mazhar, F.; Carrero, J.J. Prevalence of Chronic Kidney Disease in Women of Reproductive Age and Observed Birth Rates. J. Nephrol. 2023, 36, 1341–1347. [Google Scholar] [CrossRef]
- Rojas, R.; Clegg, D.J.; Palmer, B.F. Amenorrhea and Estrogen Disorders in Kidney Disease. Semin. Nephrol. 2021, 41, 126–132. [Google Scholar] [CrossRef]
- Pyrgidis, N.; Mykoniatis, I.; Tishukov, M.; Sokolakis, I.; Nigdelis, M.P.; Sountoulides, P.; Hatzichristodoulou, G.; Hatzichristou, D. Sexual Dysfunction in Women with End-Stage Renal Disease: A Systematic Review and Meta-Analysis. J. Sex. Med. 2021, 18, 936–945. [Google Scholar] [CrossRef]
- Attini, R.; Cabiddu, G.; Ciabatti, F.; Montersino, B.; Carosso, A.R.; Gernone, G.; Gammaro, L.; Moroni, G.; Torreggiani, M.; Masturzo, B.; et al. Chronic Kidney Disease, Female Infertility, and Medically Assisted Reproduction: A Best Practice Position Statement by the Kidney and Pregnancy Group of the Italian Society of Nephrology. J. Nephrol. 2023, 36, 1239–1255. [Google Scholar] [CrossRef]
- De Jong, M.F.C.; Van Hamersvelt, H.W.; Van Empel, I.W.H.; Nijkamp, E.J.W.; Lely, A.T. Summary of the Dutch Practice Guideline on Pregnancy Wish and Pregnancy in CKD. Kidney Int. Rep. 2022, 7, 2575–2588. [Google Scholar] [CrossRef] [PubMed]
- Wiles, K.; Chappell, L.; Clark, K.; Elman, L.; Hall, M.; Lightstone, L.; Mohamed, G.; Mukherjee, D.; Nelson-Piercy, C.; Webster, P.; et al. Clinical Practice Guideline on Pregnancy and Renal Disease. BMC Nephrol. 2019, 20, 401. [Google Scholar] [CrossRef]
- Cabiddu, G.; Spotti, D.; Gernone, G.; Santoro, D.; Moroni, G.; Gregorini, G.; Giacchino, F.; Attini, R.; Limardo, M.; Gammaro, L.; et al. A Best-Practice Position Statement on Pregnancy after Kidney Transplantation: Focusing on the Unsolved Questions. The Kidney and Pregnancy Study Group of the Italian Society of Nephrology. J. Nephrol. 2018, 31, 665–681. [Google Scholar] [CrossRef] [PubMed]
- Schmidt, M.; Stracke, S.; Schneider, U.; Kuschel, B.; Feldkamp, T.; Habbig, S.; Mayer-Pickel, K.; Hartung, A.; Bader, B.; Weinmann-Menke, J.; et al. Chronic Kidney Disease and Pregnancy. Guideline of the DGGG, OEGGG, DGfN (S2k Level, AWMF Registry No. 015–090). Geburtshilfe Frauenheilkd 2022, 82, 795–830. [Google Scholar] [CrossRef] [PubMed]
- Rüegg, L.; Pluma, A.; Hamroun, S.; Cecchi, I.; Perez-Garcia, L.F.; Anderson, P.O.; Andreoli, L.; Wirström, S.B.; Boyadhzieva, V.; Chambers, C.; et al. EULAR Recommendations for Use of Antirheumatic Drugs in Reproduction, Pregnancy, and Lactation: 2024 Update. Ann. Rheum. Dis. 2025, 84, 910–926. [Google Scholar] [CrossRef] [PubMed]
- Lambertini, M.; Peccatori, F.A.; Demeestere, I.; Amant, F.; Wyns, C.; Stukenborg, J.-B.; Paluch-Shimon, S.; Halaska, M.J.; Uzan, C.; Meissner, J.; et al. Fertility Preservation and Post-Treatment Pregnancies in Post-Pubertal Cancer Patients: ESMO Clinical Practice Guidelines. Ann. Oncol. 2020, 31, 1664–1678. [Google Scholar] [CrossRef] [PubMed]
- Su, H.I.; Lacchetti, C.; Letourneau, J.; Partridge, A.H.; Qamar, R.; Quinn, G.P.; Reinecke, J.; Smith, J.F.; Tesch, M.; Wallace, W.H.; et al. Fertility Preservation in People with Cancer: ASCO Guideline Update. J. Clin. Oncol. 2025, 43, 1488–1515. [Google Scholar] [CrossRef] [PubMed]
- Ejaz, K.; Abid, D.; Juneau, P.; Chu, J.; Hasni, S. Use of Gonadotropin-Releasing Hormone Agonists for Ovarian Preservation in Patients Receiving Cyclophosphamide for Systemic Lupus Erythematosus: A Meta-Analysis. Lupus 2022, 31, 1706–1713. [Google Scholar] [CrossRef]
- Srialluri, N.; Thavarajah, S. CKD in Reproductive-Aged Women: A Call for Early Nephrology Referral and Multidisciplinary Care. BMC Nephrol. 2024, 25, 444. [Google Scholar] [CrossRef]



| Sex | Number | Percentage | |
|---|---|---|---|
| Female | 75 | 64.66% | |
| Male | 41 | 35.34% | |
| Years of the clinical experience | |||
| <5 | 21 | 18.10% | |
| 5–10 | 14 | 12.07% | |
| >10 | 81 | 69.83% | |
| Stage of professional career | |||
| Specialist | 89 | 76.72% | |
| Resident | 27 | 23.28% | |
| Completed or initiated specialization | |||
| Nephrology | 81 | 69.83% | |
| Internal medicine | 79 | 68.10% | |
| Family medicine | 4 | 3.45% | |
| Cardiology | 3 | 2.59% | |
| Diabetology | 1 | 0.86% | |
| Other | 36 | 31.03% | |
| Place(s) of professional employment | |||
| Multispecialty hospital | 84 | 72.41% | |
| District/municipal hospital | 41 | 35.34% | |
| Specialist outpatient practice | 32 | 27.59% | |
| Primary healthcare practice | 16 | 13.79% | |
| Non-public (private) facility | 8 | 6.90% |
| Predominant Age Group of Your Patient | Number | Percentage | |
|---|---|---|---|
| 18–40 | 5 | 4.31% | |
| 40–60 | 19 | 16.38% | |
| 60–80 | 89 | 76.72% | |
| >80 | 3 | 2.59% | |
| Estimated predominant sex of patients | |||
| More or less the same | 65 | 56.04% | |
| Majority of women | 25 | 21.55% | |
| Majority of men | 12 | 10.34% | |
| Difficult to estimate | 14 | 12.07% | |
| Estimated predominant education level of patients | |||
| Secondary/vocational education | 98 | 88.29% | |
| Primary education | 13 | 72.22% | |
| Higher education | 5 | 4.31% | |
| Estimated predominant form of professional activity of patients under care | |||
| Retired/pensioner | 94 | 83.93% | |
| Professionally active | 19 | 16.52% | |
| Student | 2 | 9.09% | |
| Unemployed | 1 | 0.85% | |
| Patients diagnosed with CKD | |||
| Yes | 113 | 97.41% | |
| No | 3 | 2.59% | |
| Estimated percentage of patients with the diagnosis of CKD | |||
| <10% | 12 | 10.62% | |
| 10–50% | 31 | 27.43% | |
| >50% | 70 | 61.95% | |
| Patients undergoing dialysis under care | |||
| Yes | 98 | 84.48% | |
| No | 18 | 15.52% | |
| Predominant form of dialysis therapy among the patients under care | |||
| Hemodialysis | 85 | 86.73% | |
| Peritoneal dialysis | 4 | 4.08% | |
| More or less the same percentage | 9 | 9.18% | |
| Pregnant patients under your care | |||
| Yes | 44 | 37.93% | |
| No | 72 | 62.07% | |
| Estimated number of pregnant patients under care annually | |||
| <50/year | 39 | 88.64% | |
| 50–100/year | 4 | 9.09% | |
| >100/year | 1 | 2.27% |
| Question 1: Managing patients with CKD. | |||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Number | 10 | 5 | 17 | 16 | 68 |
| Percentage | 8.62% | 4.31% | 14.66% | 13.79% | 58.62% |
| Question 2: The impact of gender-related factors on the development of kidney diseases. | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Number | 23 | 27 | 23 | 23 | 20 |
| Percentage | 19.83% | 23.28% | 19.83% | 19.83% | 17.24% |
| Question 3: Kidney diseases related to pregnancy. | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Number | 39 | 27 | 26 | 17 | 7 |
| Percentage | 33.62% | 23.28% | 22.41% | 14.66% | 6.03% |
| Question 4: The impact of immunosuppressive therapy on fertility. | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Number | 32 | 19 | 26 | 19 | 20 |
| Percentage | 27.59% | 16.38% | 22.41% | 16.38% | 17.24% |
| Question 1: Differences in the course and progression of CKD based on the patient’s gender. | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Number | 7 | 18 | 24 | 23 | 8 |
| Percentage | 8.75% | 22.50% | 30.00% | 28.75% | 10.00% |
| Question 2: Appropriate selection of immunosuppressive therapy for individuals of reproductive age. | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Number | 9 | 17 | 13 | 24 | 17 |
| Percentage | 11.25% | 21.25% | 16.25% | 30.00% | 21.25% |
| Question 3: Planning pregnancy in patients with CKD. | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Number | 5 | 21 | 21 | 19 | 14 |
| Percentage | 6.25% | 26.25% | 26.25% | 23.75% | 17.50% |
| Question 4: Differences in dialysis management during pregnancy. | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Number | 18 | 17 | 20 | 11 | 14 |
| Percentage | 22.50% | 21.25% | 25.00% | 13.75% | 17.50% |
| Question 5: The impact of CKD on fertility. | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Number | 6 | 12 | 25 | 22 | 15 |
| Percentage | 7.50% | 15.00% | 31.25% | 27.50% | 18.75% |
| Question 6: Assisted reproductive technologies (ART) in women with CKD. | |||||
| 1 | 2 | 3 | 4 | 5 | |
| Number | 36 | 24 | 12 | 6 | 2 |
| Percentage | 45.00% | 30.00% | 15.00% | 7.50% | 2.50% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Przybyszewska, W.; Gawalski, K.; Bijak, B.; Rymarz, A.; Małyszko, J. Toward Equitable Kidney Care: Insights from the Survey Among Polish Doctors on the Women’s Health in Chronic Kidney Disease Management. J. Clin. Med. 2026, 15, 196. https://doi.org/10.3390/jcm15010196
Przybyszewska W, Gawalski K, Bijak B, Rymarz A, Małyszko J. Toward Equitable Kidney Care: Insights from the Survey Among Polish Doctors on the Women’s Health in Chronic Kidney Disease Management. Journal of Clinical Medicine. 2026; 15(1):196. https://doi.org/10.3390/jcm15010196
Chicago/Turabian StylePrzybyszewska, Weronika, Karol Gawalski, Barbara Bijak, Aleksandra Rymarz, and Jolanta Małyszko. 2026. "Toward Equitable Kidney Care: Insights from the Survey Among Polish Doctors on the Women’s Health in Chronic Kidney Disease Management" Journal of Clinical Medicine 15, no. 1: 196. https://doi.org/10.3390/jcm15010196
APA StylePrzybyszewska, W., Gawalski, K., Bijak, B., Rymarz, A., & Małyszko, J. (2026). Toward Equitable Kidney Care: Insights from the Survey Among Polish Doctors on the Women’s Health in Chronic Kidney Disease Management. Journal of Clinical Medicine, 15(1), 196. https://doi.org/10.3390/jcm15010196







