Minimally Invasive Access Cavities: A Benefit/Risk Analysis
Abstract
1. Introduction
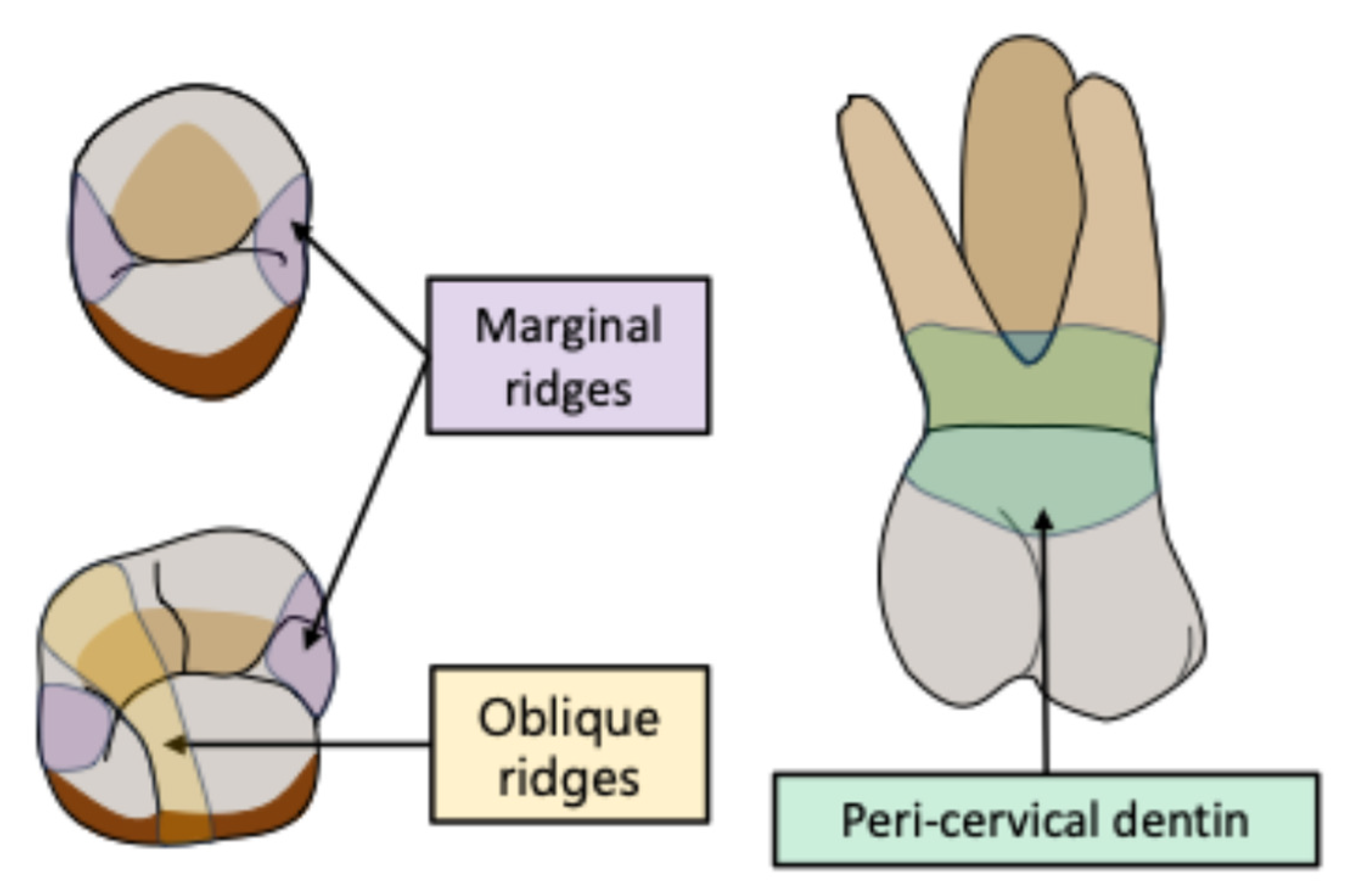
- Preservation of a more or less significant portion of the pulp chamber roof.
- Formation of soffits (parts of the pulp chamber roof left intact, resulting in the presence of undercut areas in the pulp chamber).
- Preservation of the peri-cervical dentin and of the tooth’s natural ferrule effect.
- Customized access cavity design for the treated tooth.
- Is there an improvement in mechanical properties when preparing MIACs compared to traditional ones? Such an improvement should correspond to the main objective of this kind of cavity.
- Does the MIAC approach compromise the quality of the endodontic treatment (including debridement, disinfection, obturation and procedural errors)?
- Finally, is it possible to meet the demands of high-quality endodontic treatment with a reduced access cavity?
2. Material and Method
- -
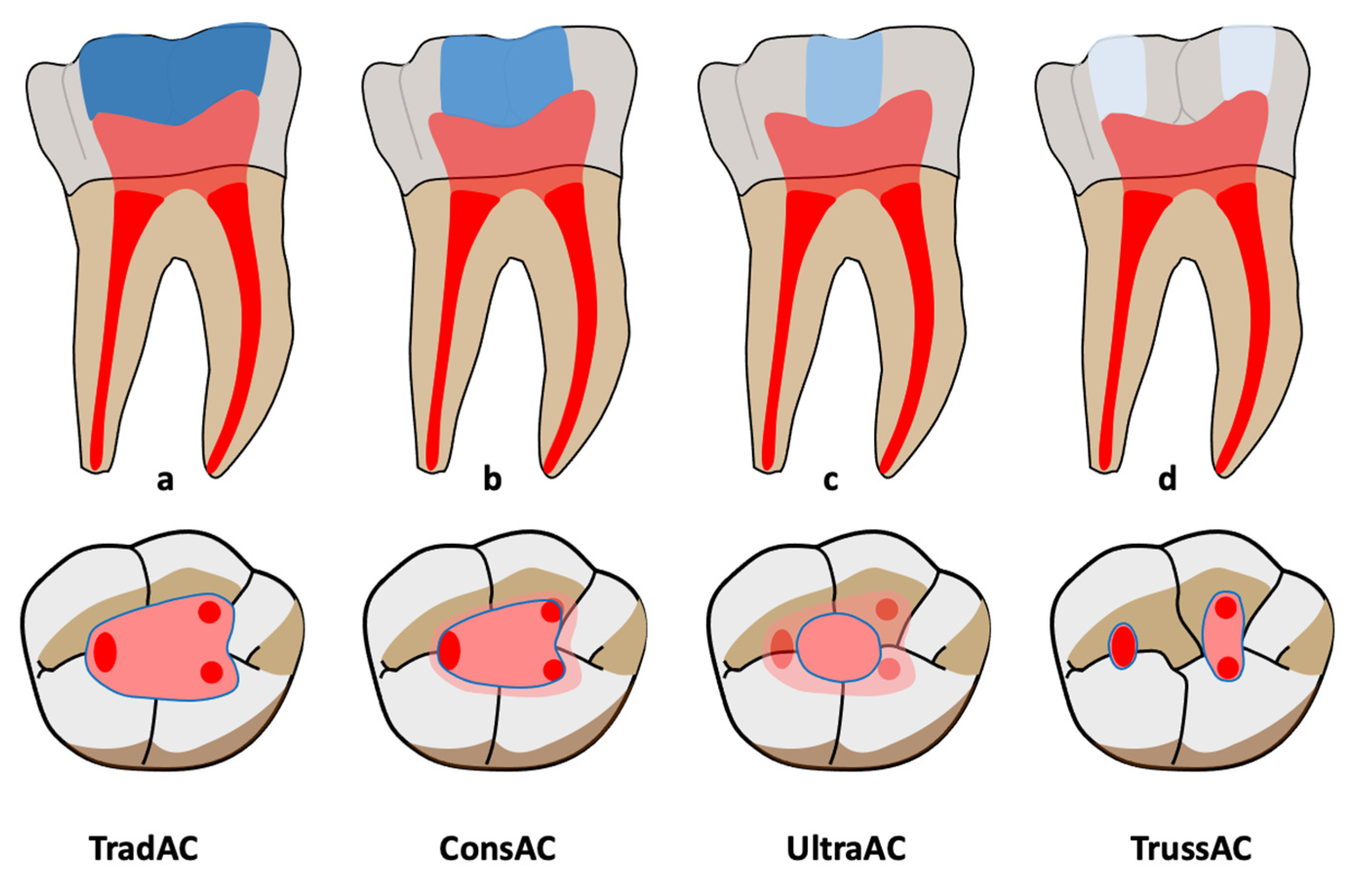
- Traditional access cavities (TradACs): Prepared using standardized occlusal landmarks. Complete removal of the pulp chamber roof, followed by a straight-line access to the canal orifices with slightly divergent walls, allowing a convenient form to be obtained. All orifices can be seen simultaneously from the entry point of the access cavity. Pre-enlargement of the canal openings is recommended.
- -
- Conservative access cavities (ConsACs): convergent cavity walls; a preserved pulp chamber roof which leads to the formation of soffits.
- -
- Ultra-conservative access cavities (UltraACs; ninja ACs): A single-entry point is created. No direct visual access to the canals is obtained.
- -
- Truss access cavities (TrussACs): multiple entry points are created for each canal. The preserved pulp chamber roof acts like a load-bearing beam.
3. Results
3.1. Mechanical Resistance
3.2. Canal Orifice Detection
3.3. Instrumentation Quality
3.4. Canal Deviation
3.5. Instruments’ Constraints
3.6. Obturation
3.7. Time
4. Discussion
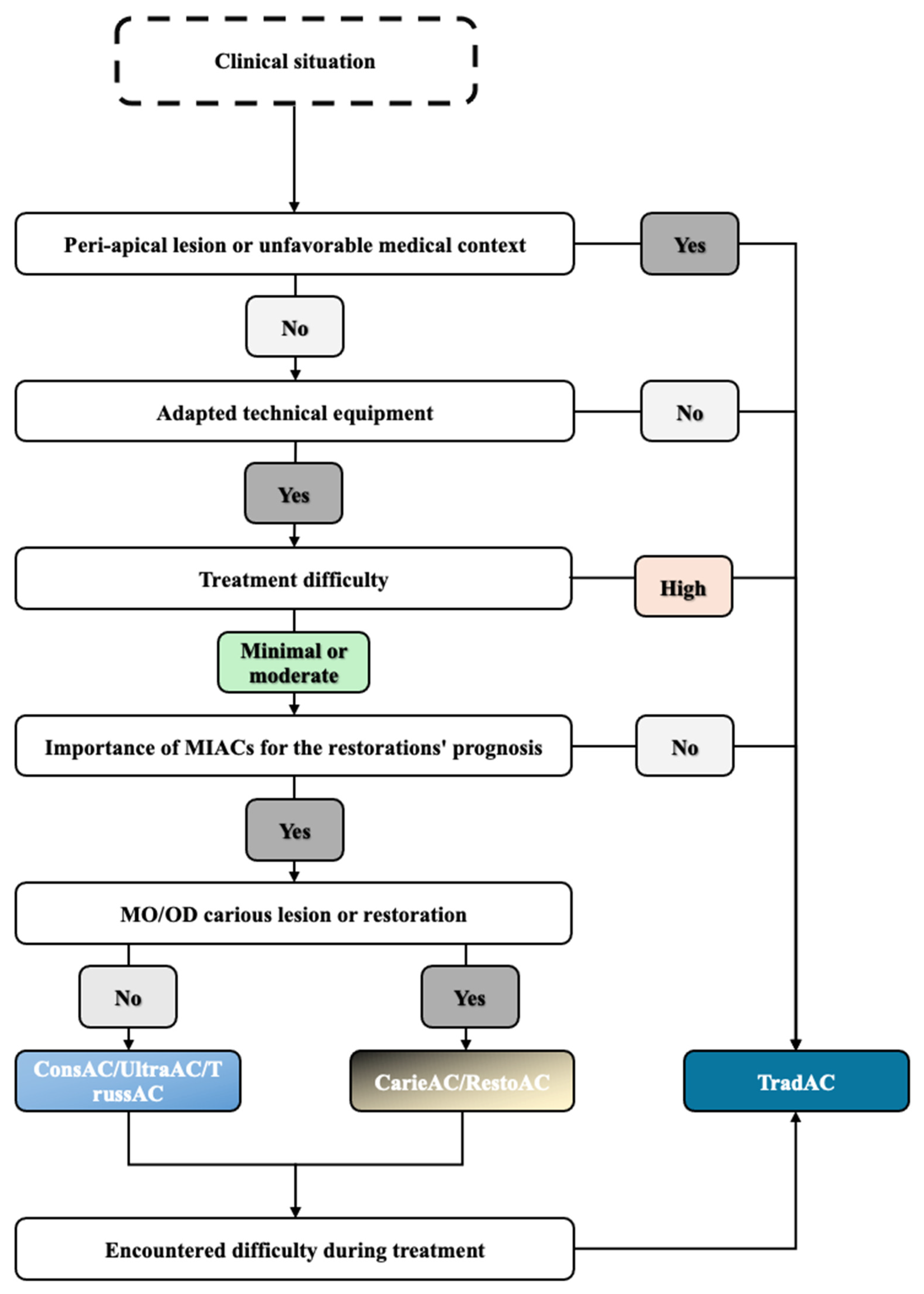
4.1. Decision-Making Process
4.1.1. Treatment Prognosis
4.1.2. Technical Equipment
4.1.3. Difficulty
4.1.4. Interest in Tooth Restoration
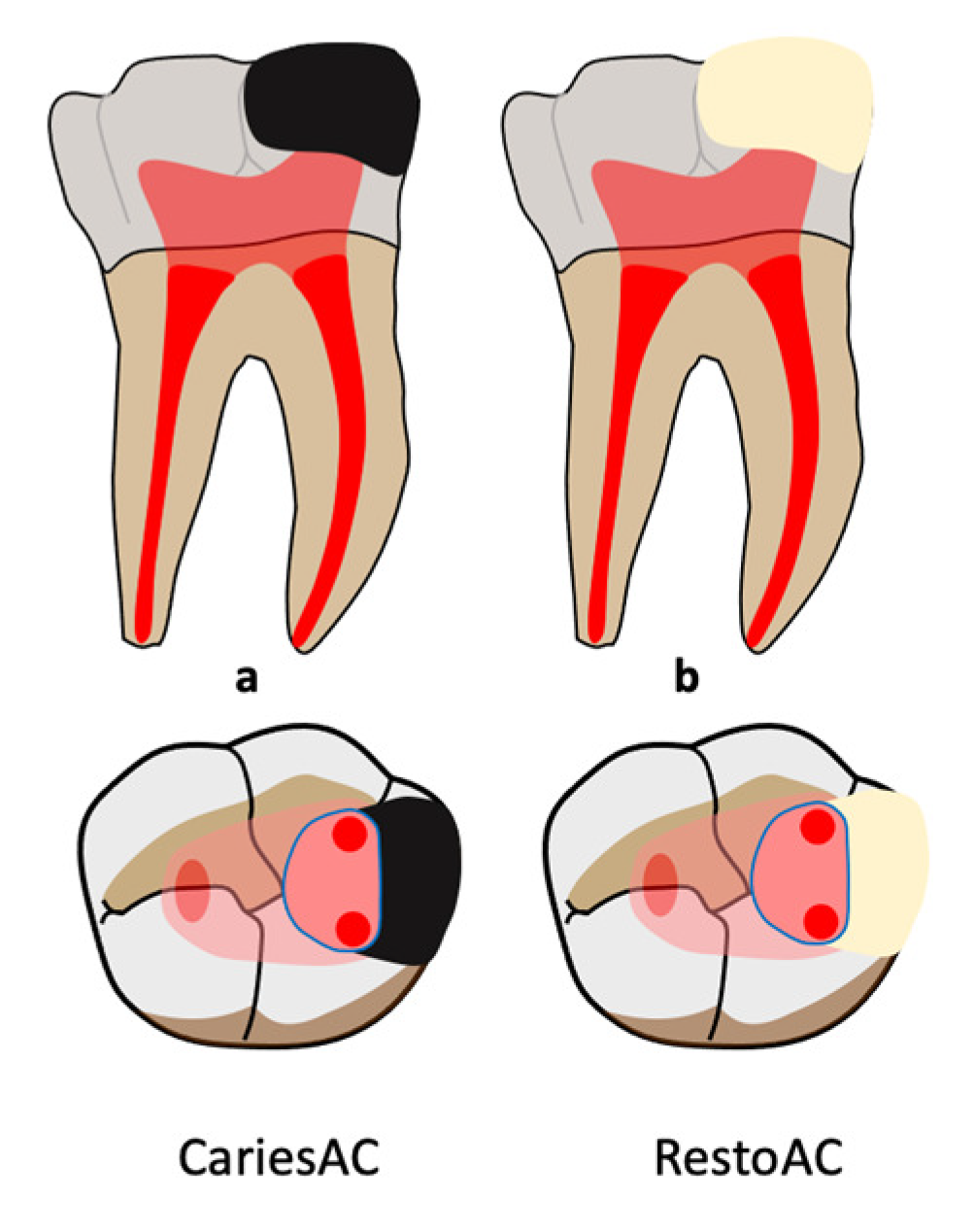
4.1.5. CariesACs or RestoACs
4.2. Synthesis and Proposed Decision Tree
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AAE | American Association of Endodontics. |
| CariesAC | Caries-driven access cavity. |
| ConsAC | Conservative access cavity. |
| EDTA | Ethylenediaminetetraacetic acid. |
| ESE | European Society of Endodontology. |
| MB2 | Second mesio-buccal. |
| MIAC | Minimally invasive access cavity. |
| NaOCl | Sodium hypochlorite. |
| NinjaAC | Ninja access cavity. |
| RestoAC | Restorative-driven access cavity. |
| TradAC | Traditional access cavity. |
| TrussAC | Truss access cavity. |
| UltraAC | Ultra-conservative access cavity. |
References
- American Association of Endodontists Treatment Standards 2020. Available online: https://www.aae.org/specialty/wp-content/uploads/sites/2/2018/04/TreatmentStandards_Whitepaper.pdf (accessed on 5 June 2024).
- Haute autorité de santé Traitement Endodontique: Rapport d’évaluation Technologique. 2008. Available online: https://docudent.fr/wp-content/uploads/2021/10/Traitements-endodontiques-%E2%80%93-Rapport-devaluation-HAS-2008.pdf (accessed on 5 June 2024).
- Dietschi, D.; Duc, O.; Krejci, I.; Sadan, A. Biomechanical Considerations for the Restoration of Endodontically Treated Teeth: A Systematic Review of the Literature, Part II (Evaluation of Fatigue Behavior, Interfaces, and in Vivo Studies). Quintessence Int. Berl. Ger. 1985 2008, 39, 117–129. [Google Scholar]
- Saeed, M.; Al-Obadi, M.; Salim, A.; Alsawaf, A.Y.; Hadi, K. Impact of Access Cavity Design on Fracture Resistance of Endodontically Treated Molars: A Systematic Review. Clin. Cosmet. Investig. Dent. 2021, 13, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Reeh, E.S.; Messer, H.H.; Douglas, W.H. Reduction in Tooth Stiffness as a Result of Endodontic and Restorative Procedures. J. Endod. 1989, 15, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Larson, T.; Douglas, W.H.; Geistfield, R. Effect of Prepared Cavities on the Strength of Teeth. Oper. Dent. 1981, 6, 2–5. [Google Scholar]
- Baniasadi, M.; Darijani, H.; Parirokh, M.; Hamze, F. Evaluating the Effect of Oblique Ridge Conservation on Stress Distribution in an Endodontically Treated Maxillary First Molar: A Finite Element Study. J. Endod. 2021, 47, 500–508. [Google Scholar] [CrossRef]
- European Society of Endodontology. Quality Guidelines for Endodontic Treatment: Consensus Report of the European Society of Endodontology. Int. Endod. J. 2006, 39, 921–930. [Google Scholar] [CrossRef]
- Boveda, C.; Kishen, A. Contracted Endodontic Cavities: The Foundation for Less Invasive Alternatives in the Management of Apical Periodontitis. Endod. Top. 2015, 33, 169–186. [Google Scholar] [CrossRef]
- Clark, D.; Khademi, J. Modern Molar Endodontic Access and Directed Dentin Conservation. Dent. Clin. N. Am. 2010, 54, 249–273. [Google Scholar] [CrossRef]
- Silva, E.J.N.L.; De-Deus, G.; Souza, E.M.; Belladonna, F.G.; Cavalcante, D.M.; Simões-Carvalho, M.; Versiani, M.A. Present Status and Future Directions—Minimal Endodontic Access Cavities. Int. Endod. J. 2022, 55, 531–587. [Google Scholar] [CrossRef]
- Tsotsis, P.; Dunlap, C.; Scott, R.; Arias, A.; Peters, O.A. A Survey of Current Trends in Root Canal Treatment: Access Cavity Design and Cleaning and Shaping Practices. Aust. Endod. J. 2021, 47, 27–33. [Google Scholar] [CrossRef]
- Rao, M.; Prasad, K.; Rao, M.; Narayana, V. Current Concepts in Bio-Minimal Endodontics: A Comprehensive Review on Modern Access Cavity Designs. J. Adv. Med. Med. Res. 2022, 34, 9–15. [Google Scholar] [CrossRef]
- Moore, B.; Verdelis, K.; Kishen, A.; Dao, T.; Friedman, S. Impacts of Contracted Endodontic Cavities on Instrumentation Efficacy and Biomechanical Responses in Maxillary Molars. J. Endod. 2016, 42, 1779–1783. [Google Scholar] [CrossRef]
- Chan, Y.C. A Literature Review of Minimally Invasive Endodontic Access Cavity—Past, Present and Future. Eur. Endod. J. 2022, 7, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Shabbir, J.; Zehra, T.; Najmi, N.; Hasan, A.; Naz, M.; Piasecki, L.; Azim, A.A. Access Cavity Preparations: Classification and Literature Review of Traditional and Minimally Invasive Endodontic Access Cavity Designs. J. Endod. 2021, 47, 1229–1244. [Google Scholar] [CrossRef] [PubMed]
- Abou-Elnaga, M.Y.; Alkhawas, M.-B.A.M.; Kim, H.-C.; Refai, A.S. Effect of Truss Access and Artificial Truss Restoration on the Fracture Resistance of Endodontically Treated Mandibular First Molars. J. Endod. 2019, 45, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Al-Ani, A.M.; Ali, A.H.; Koller, G. Assessment of Bacterial Load and Post-Endodontic Pain after One-Visit Root Canal Treatment Using Two Types of Endodontic Access Openings: A Randomized Controlled Clinical Trial. Dent. J. 2024, 12, 88. [Google Scholar] [CrossRef]
- Alovisi, M.; Pasqualini, D.; Musso, E.; Bobbio, E.; Giuliano, C.; Mancino, D.; Scotti, N.; Berutti, E. Influence of Contracted Endodontic Access on Root Canal Geometry: An In Vitro Study. J. Endod. 2018, 44, 614–620. [Google Scholar] [CrossRef]
- Barbosa, A.F.A.; Silva, E.J.N.L.; Coelho, B.P.; Ferreira, C.M.A.; Lima, C.O.; Sassone, L.M. The Influence of Endodontic Access Cavity Design on the Efficacy of Canal Instrumentation, Microbial Reduction, Root Canal Filling and Fracture Resistance in Mandibular Molars. Int. Endod. J. 2020, 53, 1666–1679. [Google Scholar] [CrossRef]
- Chandolu, V.; Mandava, J.; Borugadda, R.; Sirisha, K.; Kumar, K.R.; Goteti, S.; Nallamilli, L.S.R. Influence of Access Cavity Design on Root Canal Instrumentation Efficacy in Molars—An in Vitro Study. J. Conserv. Dent. Endod. 2024, 27, 268–273. [Google Scholar] [CrossRef]
- Corsentino, G.; Pedullà, E.; Castelli, L.; Liguori, M.; Spicciarelli, V.; Martignoni, M.; Ferrari, M.; Grandini, S. Influence of Access Cavity Preparation and Remaining Tooth Substance on Fracture Strength of Endodontically Treated Teeth. J. Endod. 2018, 44, 1416–1421. [Google Scholar] [CrossRef]
- Kishan, K.V.; Savaliya, K.; Shroff, M.; Saklecha, P. Comparative Evaluation of the Effect of Conventional and Truss Access Cavities on Remaining Dentin Thickness, Canal Transportation, and Canal Centering Ability in Mandibular Molars Using Cone-Beam Computed Tomography. Endodontology 2023, 35, 137–141. [Google Scholar] [CrossRef]
- Koohnavard, M.; Celikten, B.; Buyuksungur, A.; Orhan, K. Effect of Traditional and Conservative Endodontic Access Cavities on Instrumentation Efficacy of Two Different Ni-Ti Systems: A Micro-CT Study. Appl. Sci. 2023, 13, 5803. [Google Scholar] [CrossRef]
- Krishan, R.; Paqué, F.; Ossareh, A.; Kishen, A.; Dao, T.; Friedman, S. Impacts of Conservative Endodontic Cavity on Root Canal Instrumentation Efficacy and Resistance to Fracture Assessed in Incisors, Premolars, and Molars. J. Endod. 2014, 40, 1160–1166. [Google Scholar] [CrossRef] [PubMed]
- Kadhim, S.A.; Ali, A.H.; Mahdee, A. Comparison of Root Canal Transportation and Centering after Instrumentation through Conservative and Traditional Access Cavities Using Different File Systems: An in Vitro Study. Saudi Endod. J. 2023, 13, 74. [Google Scholar] [CrossRef]
- Lima, C.O.; Barbosa, A.F.A.; Ferreira, C.M.; Ferretti, M.A.; Aguiar, F.H.B.; Lopes, R.T.; Fidel, S.R.; Silva, E.J.N.L. Influence of Ultraconservative Access Cavities on Instrumentation Efficacy with XP-endo Shaper and Reciproc, Filling Ability and Load Capacity of Mandibular Molars Subjected to Thermomechanical Cycling. Int. Endod. J. 2021, 54, 1383–1393. [Google Scholar] [CrossRef]
- Marchesan, M.A.; Lloyd, A.; Clement, D.J.; McFarland, J.D.; Friedman, S. Impacts of Contracted Endodontic Cavities on Primary Root Canal Curvature Parameters in Mandibular Molars. J. Endod. 2018, 44, 1558–1562. [Google Scholar] [CrossRef]
- Neelakantan, P.; Khan, K.; Hei Ng, G.P.; Yip, C.Y.; Zhang, C.; Pan Cheung, G.S. Does the Orifice-Directed Dentin Conservation Access Design Debride Pulp Chamber and Mesial Root Canal Systems of Mandibular Molars Similar to a Traditional Access Design? J. Endod. 2018, 44, 274–279. [Google Scholar] [CrossRef]
- Özyürek, T.; Ülker, Ö.; Demiryürek, E.Ö.; Yılmaz, F. The Effects of Endodontic Access Cavity Preparation Design on the Fracture Strength of Endodontically Treated Teeth: Traditional Versus Conservative Preparation. J. Endod. 2018, 44, 800–805. [Google Scholar] [CrossRef]
- Pereira, R.D.; Leoni, G.B.; Silva-Sousa, Y.T.; Gomes, E.A.; Dias, T.R.; Brito-Júnior, M.; Sousa-Neto, M.D. Impact of Conservative Endodontic Cavities on Root Canal Preparation and Biomechanical Behavior of Upper Premolars Restored with Different Materials. J. Endod. 2021, 47, 989–999. [Google Scholar] [CrossRef]
- Plotino, G.; Grande, N.M.; Isufi, A.; Ioppolo, P.; Pedullà, E.; Bedini, R.; Gambarini, G.; Testarelli, L. Fracture Strength of Endodontically Treated Teeth with Different Access Cavity Designs. J. Endod. 2017, 43, 995–1000. [Google Scholar] [CrossRef]
- Rover, G.; Belladonna, F.G.; Bortoluzzi, E.A.; De-Deus, G.; Silva, E.J.N.L.; Teixeira, C.S. Influence of Access Cavity Design on Root Canal Detection, Instrumentation Efficacy, and Fracture Resistance Assessed in Maxillary Molars. J. Endod. 2017, 43, 1657–1662. [Google Scholar] [CrossRef] [PubMed]
- Rover, G.; De Lima, C.O.; Belladonna, F.G.; Garcia, L.F.R.; Bortoluzzi, E.A.; Silva, E.J.N.L.; Teixeira, C.S. Influence of Minimally Invasive Endodontic Access Cavities on Root Canal Shaping and Filling Ability, Pulp Chamber Cleaning and Fracture Resistance of Extracted Human Mandibular Incisors. Int. Endod. J. 2020, 53, 1530–1539. [Google Scholar] [CrossRef] [PubMed]
- Sabeti, M.; Kazem, M.; Dianat, O.; Bahrololumi, N.; Beglou, A.; Rahimipour, K.; Dehnavi, F. Impact of Access Cavity Design and Root Canal Taper on Fracture Resistance of Endodontically Treated Teeth: An Ex Vivo Investigation. J. Endod. 2018, 44, 1402–1406. [Google Scholar] [CrossRef] [PubMed]
- Selvakumar, R.J.; Surendran, S.; Sundar, S.; Arul, B.; Natanasabapathy, V. Impact of Contracted Endodontic Access Cavities on the Fracture Resistance of Endodontically Treated Teeth After Mechanical Aging by Simulated Chewing Forces. J. Endod. 2023, 49, 1176–1182. [Google Scholar] [CrossRef]
- Silva, A.A.; Belladonna, F.G.; Rover, G.; Lopes, R.T.; Moreira, E.J.L.; De-Deus, G.; Silva, E.J.N.L. Does Ultraconservative Access Affect the Efficacy of Root Canal Treatment and the Fracture Resistance of Two-rooted Maxillary Premolars? Int. Endod. J. 2020, 53, 265–275. [Google Scholar] [CrossRef]
- Silva, E.J.N.L.; Attademo, R.S.; Da Silva, M.C.D.; Pinto, K.P.; Antunes, H.D.S.; Vieira, V.T.L. Does the Type of Endodontic Access Influence in the Cyclic Fatigue Resistance of Reciprocating Instruments? Clin. Oral Investig. 2021, 25, 3691–3698. [Google Scholar] [CrossRef]
- Vieira, G.C.S.; Pérez, A.R.; Alves, F.R.F.; Provenzano, J.C.; Mdala, I.; Siqueira, J.F.; Rôças, I.N. Impact of Contracted Endodontic Cavities on Root Canal Disinfection and Shaping. J. Endod. 2020, 46, 655–661. [Google Scholar] [CrossRef]
- Ballester, B.; Giraud, T.; Ahmed, H.M.A.; Nabhan, M.S.; Bukiet, F.; Guivarc’h, M. Current Strategies for Conservative Endodontic Access Cavity Preparation Techniques—Systematic Review, Meta-Analysis, and Decision-Making Protocol. Clin. Oral Investig. 2021, 25, 6027–6044. [Google Scholar] [CrossRef]
- Motiwala, M.A.; Gul, M.; Ghafoor, R. Effect of Different Access Cavity Designs on Fracture Toughness of Endodontically Treated Teeth: A Systematic Review and Network Meta-Analysis. Evid. Based Dent. 2022, 1–9. [Google Scholar] [CrossRef]
- Rahbani Nobar, B.; Dianat, O.; Rahbani Nobar, B.; Kazem, M.; Hicks, M.L. Influence of Minimally Invasive Access Cavities on Load Capacity of Root-canal-treated Teeth: A Systematic Review and Meta-analysis. Aust. Endod. J. 2023, 49, 213–236. [Google Scholar] [CrossRef]
- Wolcott, J.; Ishley, D.; Kennedy, W.; Johnson, S.; Minnich, S.; Meyers, J. A 5 Yr Clinical Investigation of Second Mesiobuccal Canals in Endodontically Treated and Retreated Maxillary Molars. J. Endod. 2005, 31, 262–264. [Google Scholar] [CrossRef] [PubMed]
- Nair, P.N.R. On the Causes of Persistent Apical Periodontitis: A Review. Int. Endod. J. 2006, 39, 249–281. [Google Scholar] [CrossRef] [PubMed]
- Silva, E.J.N.L.; Rover, G.; Belladonna, F.G.; De-Deus, G.; Da Silveira Teixeira, C.; Da Silva Fidalgo, T.K. Impact of Contracted Endodontic Cavities on Fracture Resistance of Endodontically Treated Teeth: A Systematic Review of in Vitro Studies. Clin. Oral Investig. 2018, 22, 109–118. [Google Scholar] [CrossRef] [PubMed]
- Ricucci, D.; Siqueira, J.F. Biofilms and Apical Periodontitis: Study of Prevalence and Association with Clinical and Histopathologic Findings. J. Endod. 2010, 36, 1277–1288. [Google Scholar] [CrossRef]
- Shroff, M.; Kishan, K.V.; Shah, N.; Saklecha, P. Impact of Contracted Endodontic Cavities on Instrumentation Efficacy—A Systematic Review. Aust. Endod. J. 2023, 49, 202–212. [Google Scholar] [CrossRef]
- Mergoni, G.; Ganim, M.; Lodi, G.; Figini, L.; Gagliani, M.; Manfredi, M. Single versus Multiple Visits for Endodontic Treatment of Permanent Teeth. Cochrane Database Syst. Rev. 2022, 2023, CD005296. [Google Scholar] [CrossRef]
- Ng, Y.-L.; Mann, V.; Gulabivala, K. A Prospective Study of the Factors Affecting Outcomes of Nonsurgical Root Canal Treatment: Part 1: Periapical Health: Outcome of Nonsurgical Root Canal Treatment. Int. Endod. J. 2011, 44, 583–609. [Google Scholar] [CrossRef]
- Azim, A.A.; Griggs, J.A.; Huang, G.T.-J. The Tennessee Study: Factors Affecting Treatment Outcome and Healing Time Following Nonsurgical Root Canal Treatment. Int. Endod. J. 2016, 49, 6–16. [Google Scholar] [CrossRef]
- Arya, S.; Duhan, J.; Tewari, S.; Sangwan, P.; Ghalaut, V.; Aggarwal, S. Healing of Apical Periodontitis after Nonsurgical Treatment in Patients with Type 2 Diabetes. J. Endod. 2017, 43, 1623–1627. [Google Scholar] [CrossRef]
- Silva, E.J.N.L.; Pinto, K.P.; Ferreira, C.M.; Belladonna, F.G.; De-Deus, G.; Dummer, P.M.H.; Versiani, M.A. Current Status on Minimal Access Cavity Preparations: A Critical Analysis and a Proposal for a Universal Nomenclature. Int. Endod. J. 2020, 53, 1618–1635. [Google Scholar] [CrossRef]
| Authors | Mechanical Resistance | Canal Orifice Detection | Instrumentation Quality | Canal Deviation | Instrument Constraints | Obturation | Time | Method |
|---|---|---|---|---|---|---|---|---|
| Abou-Elnaga 2019 [17] | X | TrussAC/TradAC, mandibular molars, n = 12 | ||||||
| Al-Ani 2024 [18] | X | ConsAC/TradAC, mandibular and maxillary premolars/molars, n = 91, in vivo study | ||||||
| Alovisi 2018 [19] | X | X | X | ConsAC/TradAC, mandibular molars, n = 15 | ||||
| Barbosa 2020 [20] | X | X | X | X | X | TradAC/ConsAC/TrussAC, mandibular molars, n = 10 | ||
| Chandolu 2024 [21] | X | X | TradAC/ConsAC, maxillary molar, n = 80 | |||||
| Corsentino 2018 [22] | X | TradAC/ConsAC/TrussAC, mandibular molars, n = 10 | ||||||
| Kishan 2023 [23] | X | TradAC/TrussAC, mandibular molars, n = 15 | ||||||
| Koohnavard 2023 [24] | X | X | TradAC/ConsAC, mandibular molars, n = 15 | |||||
| Krishan 2014 [25] | X | X | X | Trad/ConsAC, maxillary molars, premolars and incisors, n = 30 | ||||
| Kadhim 2023 [26] | X | X | TradAC/ConsAC, 2-rooted maxillary first premolars, n = 10 | |||||
| Lima 2021 [27] | X | X | X | X | X | X | TradAC/UltraAC, mandibular molars n = 10 | |
| Marchessan 2018 [28] | X | X | X | TradAC/ConsAC, mandibular molars, n = 12 | ||||
| Moore 2016 [14] | X | X | X | TradAC/ConsAC, maxillary molars, n = 12 | ||||
| Neelakan 2018 [29] | X | TradAC/TrussAC, mandibular molars, n = 12 | ||||||
| Ozyürek 2018 [30] | X | TradAC/ConsAC, mandibular molars, n = 20 | ||||||
| Pereira 2021 [31] | X | X | X | X | TradAC/ConsAC, maxillary premolars, n = 10 | |||
| Plotino 2017 [32] | X | TradAC/ConsAC/UltraAC, maxillary and mandibular molars and premolars, n = 40 | ||||||
| Rover 2017 [33] | X | X | X | X | X | TradAC/ConsAC, maxillary molars, n = 15 | ||
| Rover 2020 [34] | X | X | X | X | TradAC/ConsAC (incisal edge), mandibular incisors, n = 10 | |||
| Sabeti 2018 [35] | X | TradAC/ConsAC, maxillary molars, n = 16 | ||||||
| Selvakumar 2023 [36] | X | TradAC/ConsAC, mandibular molars, n = 8 | ||||||
| Silva 2020 [37] | X | X | X | X | TradAC/UltraAC, maxillary premolars, n = 10 | |||
| Silva 2021 [38] | X | TradAC/UltraAC, mandibular molars, n = 10 | ||||||
| Vieira 2020 [39] | X | TradAC/ConsAC, mandibular incisors, n = 30 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sevin, M.; Orio, E.; Collignon, A.-M. Minimally Invasive Access Cavities: A Benefit/Risk Analysis. J. Clin. Med. 2025, 14, 2476. https://doi.org/10.3390/jcm14072476
Sevin M, Orio E, Collignon A-M. Minimally Invasive Access Cavities: A Benefit/Risk Analysis. Journal of Clinical Medicine. 2025; 14(7):2476. https://doi.org/10.3390/jcm14072476
Chicago/Turabian StyleSevin, Marie, Edouard Orio, and Anne-Margaux Collignon. 2025. "Minimally Invasive Access Cavities: A Benefit/Risk Analysis" Journal of Clinical Medicine 14, no. 7: 2476. https://doi.org/10.3390/jcm14072476
APA StyleSevin, M., Orio, E., & Collignon, A.-M. (2025). Minimally Invasive Access Cavities: A Benefit/Risk Analysis. Journal of Clinical Medicine, 14(7), 2476. https://doi.org/10.3390/jcm14072476







