Developmental Trends of Metabolic Syndrome in the Past Two Decades: A Narrative Review
Abstract
1. Introduction
2. Methods
3. Metabolic Syndrome: Historical Overview
4. Metabolic Syndrome: Definition
5. Metabolic Syndrome: Prevalence
6. Pediatric Metabolic Syndrome
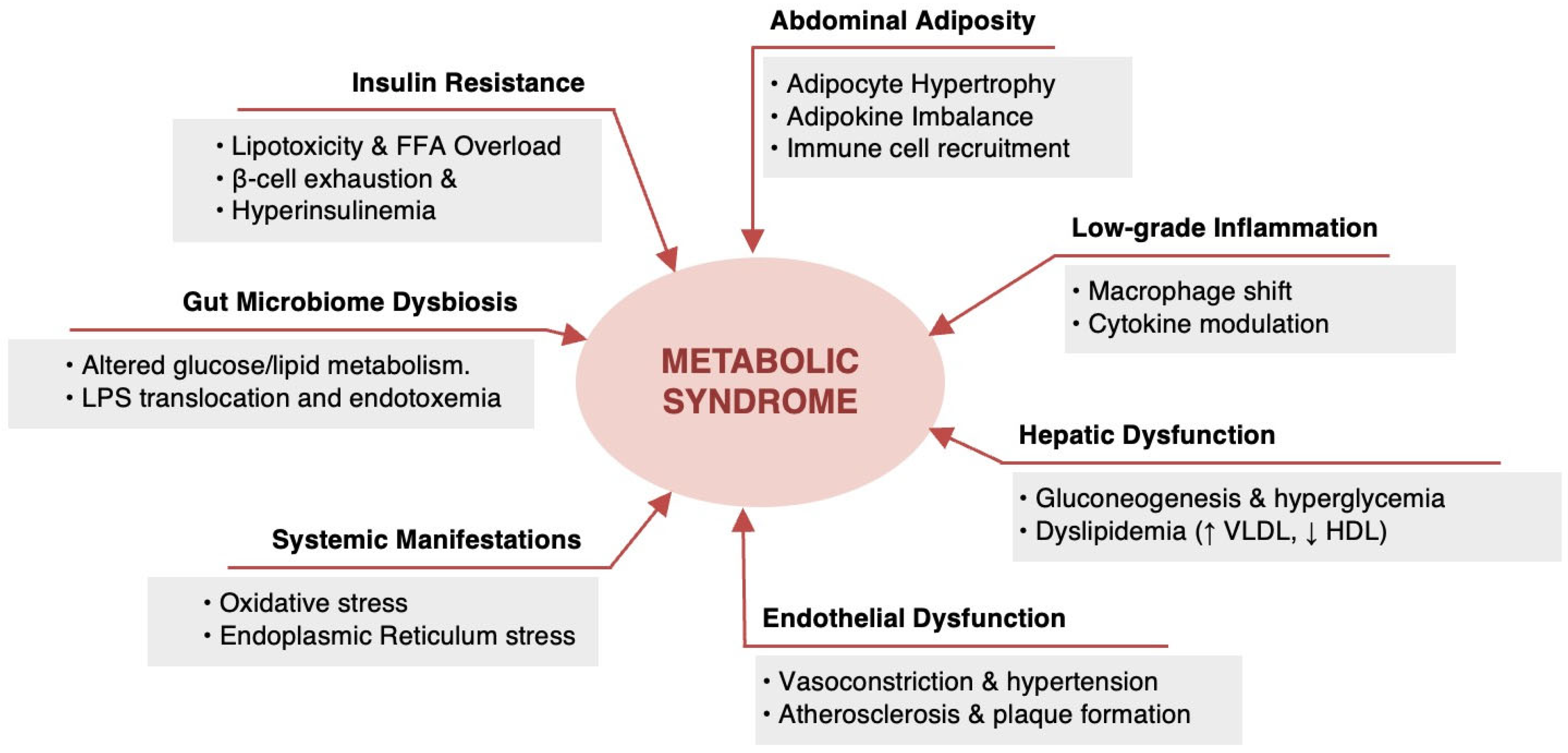
7. Metabolic Syndrome: Pathophysiology
8. Conclusions
Funding
Acknowledgments
Conflicts of Interest
References
- Rothwell, J.A.; Jenab, M.; Karimi, M.; Truong, T.; Mahamat-Saleh, Y.; Ferrari, P.; Dashti, S.G.; Kühn, T.; Cross, A.J.; Severi, G.; et al. Metabolic Syndrome and Risk of Gastrointestinal Cancers: An Investigation Using Large-Scale Molecular Data. Clin. Gastroenterol. Hepatol. 2021, 20, E1338–E1352. [Google Scholar] [CrossRef] [PubMed]
- Tobi, E.W.; Goeman, J.J.; Monajemi, R.; Gu, H.; Putter, H.; Zhang, Y.; Slieker, R.C.; Stok, A.P.; Thijssen, P.E.; Müller, F.; et al. DNA Methylation Signatures Link Prenatal Famine Exposure to Growth and Metabolism. Nat. Commu. 2014, 5, 5592. [Google Scholar] [CrossRef]
- Alberti, K.G.M.M.; Zimmet, P.Z. Definition, Diagnosis and Classification of Diabetes Mellitus and Its Complications. Part 1: Diagnosis and Classification of Diabetes Mellitus. Provisional Report of a WHO Consultation. Diabet. Med. 1998, 15, 539–553. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Yan, W.; Zhu, L.; Chen, Y.; Liu, J.; Xu, Y.; Ji, L.; He, J. Comparative Analysis of IDF, ATPIII and CDS in the Diagnosis of Metabolic Syndrome among Adult Inhabitants in Jiangxi Province, China. PLoS ONE 2017, 12, e0189046. [Google Scholar] [CrossRef]
- Ginsberg, H.N.; Zhang, Y.-L.; Hernandez-Ono, A. Metabolic Syndrome: Focus on Dyslipidemia. Obesity 2006, 14, 41S–49S. [Google Scholar] [CrossRef]
- Sui, X.; Church, T.S.; Meriwether, R.A.; Lobelo, F.; Blair, S.N. Uric Acid and the Development of Metabolic Syndrome in Women and Men. Metabolism 2008, 57, 845–852. [Google Scholar] [CrossRef]
- Gallagher, E.J.; LeRoith, D.; Karnieli, E. The Metabolic Syndrome—From Insulin Resistance to Obesity and Diabetes. Endocrinol. Metabo. Clin. N. Am. 2008, 37, 559–579. [Google Scholar] [CrossRef]
- LaMori, J.C.; Mody, S.H.; Gross, H.J.; daCosta DiBonaventura, M.; Patel, A.A.; Schein, J.R.; Nelson, W.W. Burden of Comorbidities among Patients with Atrial Fibrillation. Ther. Adv. Cardiovasc. Dis. 2012, 7, 53–62. [Google Scholar] [CrossRef]
- Scuteri, A.; Laurent, S.; Cucca, F.; Cockcroft, J.; Cunha, P.G.; Mañas, L.R.; Mattace Raso, F.U.; Muiesan, M.L.; Ryliškytė, L.; Rietzschel, E.; et al. Metabolic Syndrome across Europe: Different Clusters of Risk Factors. Eur. J. Prev. Cardiol. 2015, 22, 486–491. [Google Scholar] [CrossRef]
- Aye, M. Metabolic Syndrome (MetS). J. Metab. Syndr. 2014, 3. [Google Scholar] [CrossRef]
- Athyros, V. W09.203 the Prevalence of the Metabolic Syndrome in Greece: The MetS-Greece Study. Atherosclerosis 2004, 5, 47. [Google Scholar] [CrossRef]
- Hu, G. Prevalence of the Metabolic Syndrome and Its Relation to All-Cause and Cardiovascular Mortality in Nondiabetic European Men and Women. Arch. Intern. Med. 2004, 164, 1066. [Google Scholar] [CrossRef] [PubMed]
- Ryu, S.Y.; Kweon, S.; Park, H.; Shin, J.; Rhee, J. Obesity and the Metabolic Syndrome in Korean Adolescents. J. Korean Med. Sci. 2007, 22, 513. [Google Scholar] [CrossRef]
- Ryu, S.; Song, J.; Choi, B.-Y.; Lee, S.-J.; Kim, W.S.; Chang, Y.; Kim, D.I.; Suh, B.-S.; Sung, K.C. Incidence and Risk Factors for Metabolic Syndrome in Korean Male Workers, Ages 30 to 39. Ann. Epidemiol. 2007, 17, 245–252. [Google Scholar] [CrossRef]
- Fezeu, L.; Balkau, B.; Kengne, A.-P.; Sobngwi, E.; Mbanya, J.-C. Metabolic Syndrome in a Sub-Saharan African Setting: Central Obesity May Be the Key Determinant. Atherosclerosis 2007, 193, 70–76. [Google Scholar] [CrossRef]
- Harzallah, F.; Alberti, H.; Ben Khalifa, F. The Metabolic Syndrome in an Arab Population: A First Look at the New International Diabetes Federation Criteria. Diabet. Med. 2006, 23, 441–444. [Google Scholar] [CrossRef]
- Lemieux, I.; Després, J.-P. Metabolic Syndrome: Past, Present and Future. Nutrients 2020, 12, 3501. [Google Scholar] [CrossRef]
- Reaven, G.M. The Metabolic Syndrome: Time to Get off the Merry-Go-Round? J. Intern. Med. 2010, 269, 127–136. [Google Scholar] [CrossRef]
- Kassi, E.; Pervanidou, P.; Kaltsas, G.; Chrousos, G. Metabolic Syndrome: Definitions and Controversies. BMC Med. 2011, 9, 48. [Google Scholar] [CrossRef]
- van der Pal, K.C.; Koopman, A.D.M.; Lakerveld, J.; van der Heijden, A.A.; Elders, P.J.; Beulens, J.W.; Rutters, F. The Association between Multiple Sleep-Related Characteristics and the Metabolic Syndrome in the General Population: The New Hoorn Study. Sleep Med. 2018, 52, 51–57. [Google Scholar] [CrossRef]
- Chantler, P.; Burrage, E.; Marshall, K.; Santanam, N. Cerebrovascular Dysfunction with Stress and Depression. Brain Circ. 2018, 4, 43. [Google Scholar] [CrossRef]
- Sibley, B.A.; Etnier, J.L. The Relationship between Physical Activity and Cognition in Children: A Meta-Analysis. Pediatr. Exerc. Sci. 2003, 15, 243–256. [Google Scholar] [CrossRef]
- Guzder, R.N.; Gatling, W.; Mullee, M.A.; Byrne, C.D. Impact of Metabolic Syndrome Criteria on Cardiovascular Disease Risk in People with Newly Diagnosed Type 2 Diabetes. Diabetologia 2005, 49, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Khader, Y.; Bateiha, A.; El-Khateeb, M.; Al-Shaikh, A.; Ajlouni, K. High Prevalence of the Metabolic Syndrome among Northern Jordanians. J. Diabetes Complicat. 2007, 21, 214–219. [Google Scholar] [CrossRef]
- Obeidat, A.A.; Ahmad, M.N.; Haddad, F.H.; Azzeh, F.S. Alarming High Prevalence of Metabolic Syndrome among Jordanian Adults. Pak. J. Med. Sci. 2015, 31. [Google Scholar] [CrossRef]
- Mahadik, S.R.; Deo, S.S.; Mehtalia, S.D. Increased Prevalence of Metabolic Syndrome in Non-Obese Asian Indian—An Urban-Rural Comparison. Metab. Syndr. Relat. Disord. 2007, 5, 142–152. [Google Scholar] [CrossRef]
- Alberti, K.G.M.; Zimmet, P.; Shaw, J. The Metabolic Syndrome—A New Worldwide Definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2001, 285, 2486–2497. [Google Scholar] [CrossRef]
- Nilsson, P.M.; Tuomilehto, J.; Rydén, L. The Metabolic Syndrome—What Is It and How Should It Be Managed? Eur. J. Prev. Cardiol. 2019, 26, 33–46. [Google Scholar] [CrossRef]
- Alemany, M. Steroid Hormones Interrelationships in the Metabolic Syndrome: An Introduction to the Ponderostat Hypothesis. Hormones 2012, 11, 272–289. [Google Scholar] [CrossRef]
- Crispín-Isidro, G.; Lobato-Calleros, C.; Espinosa-Andrews, H.; Alvarez-Ramirez, J.; Vernon-Carter, E.J. Effect of Inulin and Agave Fructans Addition on the Rheological, Microstructural and Sensory Properties of Reduced-Fat Stirred Yogurt. LWT—Food Sci. Technol. 2015, 62, 438–444. [Google Scholar] [CrossRef]
- Reaven, G.M. Role of Insulin Resistance in Human Disease. Nutrition 1997, 13, 64. [Google Scholar] [CrossRef] [PubMed]
- Kaplan, N.M. The Deadly Quartet. Arch. Intern. Med. 1989, 149, 1514. [Google Scholar] [CrossRef] [PubMed]
- Eleuterio, F. The Ivsulin Resistance Syndrome. Curr. Opin. Nephrol. Hypertens. 1992, 1, 291–298. [Google Scholar] [CrossRef]
- Low, J.A. Intrapartum Fetal Asphyxia: Definition, Diagnosis, and Classification. Am. J. Obstet. Gynecol. 1997, 176, 957–959. [Google Scholar] [CrossRef]
- Etiologic Classification of Diabetes Mellitus. Can. J. Diabetes 2018, 42, S308. [CrossRef]
- Fahed, G.; Aoun, L.; Bou Zerdan, M.; Allam, S.; Bou Zerdan, M.; Bouferraa, Y.; Assi, H.I. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int. J. Mol. Sci. 2022, 23, 786. [Google Scholar] [CrossRef]
- Yu, X.; Wang, L.; Zhang, W.; Ming, J.; Jia, A.; Xu, S.; Li, Q.; Ji, Q. Fasting Triglycerides and Glucose Index Is More Suitable for the Identification of Metabolically Unhealthy Individuals in the Chinese Adult Population: A Nationwide Study. J. Diabetes Investig. 2019, 10, 1050–1058. [Google Scholar] [CrossRef]
- Anderson, P.; Critchley, J.; Chan, J.; Cockram, C.; Lee, Z.; Thomas, G.; Tomlinson, B. Factor Analysis of the Metabolic Syndrome: Obesity vs Insulin Resistance as the Central Abnormality. Int. J. Obes. 2001, 25, 1782–1788. [Google Scholar] [CrossRef]
- Li, R.; Li, W.; Lun, Z.; Zhang, H.; Sun, Z.; Kanu, J.S.; Qiu, S.; Cheng, Y.; Liu, Y. Prevalence of Metabolic Syndrome in Mainland China: A Meta-Analysis of Published Studies. BMC Public Health 2016, 16, 1–10. [Google Scholar] [CrossRef]
- Pistrosch, F. The Metabolic Syndrome and Cardiovascular Diseases: An Update of Medical Treatment. J. Metab. Synd. 2014, 3, 160–167. [Google Scholar] [CrossRef]
- Tee, J.Y.H.; Gan, W.Y.; Lim, P.Y. Comparisons of Body Mass Index, Waist Circumference, Waist-To-Height Ratio and a Body Shape Index (ABSI) in Predicting High Blood Pressure among Malaysian Adolescents: A Cross-Sectional Study. BMJ Open 2020, 10, e032874. [Google Scholar] [CrossRef]
- Saklayen, M.G. The Global Epidemic of the Metabolic Syndrome. Curr. Hypertens. Rep. 2018, 20, 1–8. [Google Scholar] [CrossRef]
- Stančáková, A.; Laakso, M. Genetics of Metabolic Syndrome. Rev. Endocr. Metab. Disord. 2014, 15, 243–252. [Google Scholar] [CrossRef]
- Isomaa, B. A Major Health Hazard: The Metabolic Syndrome. Life Sci. 2003, 73, 2395–2411. [Google Scholar] [CrossRef]
- Thomas, G.N.; Ho, S.-Y.; Janus, E.D.; Lam, K.S.L.; Hedley, A.J.; Lam, T.H. The US National Cholesterol Education Programme Adult Treatment Panel III (NCEP ATP III) Prevalence of the Metabolic Syndrome in a Chinese Population. Diabetes Res. Clin. Pract. 2005, 67, 251–257. [Google Scholar] [CrossRef]
- Ford, E.S.; Giles, W.H. A Comparison of the Prevalence of the Metabolic Syndrome Using Two Proposed Definitions. Diabetes Care 2003, 26, 575–581. [Google Scholar] [CrossRef]
- Bhandari, R.; Kelley, G.A.; Hartley, T.A.; Rockett, I.R.H. Metabolic Syndrome Is Associated with Increased Breast Cancer Risk: A Systematic Review with Meta-Analysis. Int. J. Breast Cancer 2014, 2014, 1–13. [Google Scholar] [CrossRef]
- Dobrowolski, P.; Prejbisz, A.; Kuryłowicz, A.; Baska, A.; Burchardt, P.; Chlebus, K.; Dzida, G.; Jankowski, P.; Jaroszewicz, J.; Jaworski, P.; et al. Metabolic Syndrome—A New Definition and Management Guidelines: A Joint Position Paper by the Polish Society of Hypertension, Polish Society for the Treatment of Obesity, Polish Lipid Association, Polish Association for Study of Liver, Polish Society of Family Medicine, Polish Society of Lifestyle Medicine, Division of Prevention and Epidemiology Polish Cardiac Society, “Club 30” Polish Cardiac Society, and Division of Metabolic and Bariatric Surgery Society of Polish Surgeons. Arch. Med. Sci. 2022, 18, 1133–1156. [Google Scholar] [CrossRef]
- Iacobini, C.; Pugliese, G.; Blasetti Fantauzzi, C.; Federici, M.; Menini, S. Metabolically Healthy versus Metabolically Unhealthy Obesity. Metabolism 2019, 92, 51–60. [Google Scholar] [CrossRef]
- O’Neill, S.; O’Driscoll, L. Metabolic Syndrome: A Closer Look at the Growing Epidemic and Its Associated Pathologies. Obesity Rev. 2014, 16, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Andriankaja, O.; Sreenivasa, S.; Dunford, R.; DeNardin, E. Association between Metabolic Syndrome and Periodontal Disease. Aust. Dent. J. 2010, 55, 252–259. [Google Scholar] [CrossRef] [PubMed]
- Parikh, R.; Mohan, V. Changing Definitions of Metabolic Syndrome. Indian J. Endocrinol. Metab. 2012, 16, 7. [Google Scholar] [CrossRef] [PubMed]
- Ignatius, U.; Onesi, S. Metabolic Syndrome: Performance of Five Different Diagnostic Criterias. Indian J. Endocrinol. Metab. 2014, 18, 496. [Google Scholar] [CrossRef]
- Wang, M.; Tan, Y.; Shi, Y.; Wang, X.; Liao, Z.; Wei, P. Diabetes and Sarcopenic Obesity: Pathogenesis, Diagnosis, and Treatments. Front. Endocrinol. 2020, 11, 568. [Google Scholar] [CrossRef]
- Laaksonen, D.E.; Lakka, H.-M.; Salonen, J.T.; Niskanen, L.K.; Rauramaa, R.; Lakka, T.A. Low Levels of Leisure-Time Physical Activity and Cardiorespiratory Fitness Predict Development of the Metabolic Syndrome. Diabetes Care 2002, 25, 1612–1618. [Google Scholar] [CrossRef]
- Wong, Y.; Cook, P.; Roderick, P.; Somani, B.K. Metabolic Syndrome and Kidney Stone Disease: A Systematic Review of Literature. J. Endourol. 2016, 30, 246–253. [Google Scholar] [CrossRef]
- Kali, A.; Gusmanov, A.; Aripov, M.; Chan, M.-Y. Proposing New Body Mass Index and Waist Circumference Cut-Offs Based on Cardiometabolic Risks for a Central Asia Population: A Feasibility Study. Front. Endocrinol. 2022, 13. [Google Scholar] [CrossRef]
- Santanasto, A.J.; Miljkovic, I.; Cvejkus, R.K.; Boudreau, R.M.; Wheeler, V.W.; Zmuda, J.M. Body Composition across the Adult Lifespan in African Caribbean Men: The Tobago Longitudinal Study of Aging. J. Frailty Aging 2021, 11, 40–44. [Google Scholar] [CrossRef]
- Al-Rubean, K.; Youssef, A.M.; Yousuf, A.; Al-Sharqawi, A.H.; Bawazeer, N.; Alotaibi, M.H.; Alrumaih, F.I. Anthropometric Cutoff Values for Predicting Metabolic Syndrome in a Saudi Community: From the SAUDI-DM Study. Ann. Saudi Med. 2017, 37, 21–30. [Google Scholar] [CrossRef]
- Ford, E.S. Prevalence of the Metabolic Syndrome Defined by the International Diabetes Federation among Adults in the U.S. Diabetes Care 2005, 28, 2745–2749. [Google Scholar] [CrossRef] [PubMed]
- Akhouayri, O.; El Brini, O.; Mesfioui, A.; Benazzouz, B.; Gamal, A. Prevalence of Metabolic Syndrome and Its Components Based on a Harmonious Definition among Adults in Morocco. Diabetes Metab. Syndr. Obes. Targets Ther. 2014, 341. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.M.; Gurka, M.J.; DeBoer, M.D. Trends in Metabolic Syndrome Severity and Lifestyle Factors among Adolescents. Pediatrics 2016, 137, e20153177. [Google Scholar] [CrossRef]
- Kapila, M. Noncommunicable Diseases Need an Urgent and Systematic Response. Int. J. Noncommun. Dis. 2019, 4, 35. [Google Scholar] [CrossRef]
- Leonardi, B.F.; Gosmann, G.; Zimmer, A.R. Modeling Diet-Induced Metabolic Syndrome in Rodents. Mol. Nutr. Food Res. 2020, 64, 2000249. [Google Scholar] [CrossRef]
- Tabeshpour, J.; Razavi, B.M.; Hosseinzadeh, H. Effects of Avocado (Persea Americana) on Metabolic Syndrome: A Comprehensive Systematic Review. Phytother. Res. 2017, 31, 819–837. [Google Scholar] [CrossRef]
- Srinivas, S.K.; Sammel, M.D.; Bastek, J.A.; Ofori, E.; Andrela, C.M.; Wolfe, M.L.; Reilly, M.P.; Elovitz, M.A. Evaluating the Association between All Components of the Metabolic Syndrome and Pre-Eclampsia. J. Matern.-Fetal Neonatal Med. 2009, 22, 501–509. [Google Scholar] [CrossRef]
- Tong, W.; Lai, H.; Yang, C.; Ren, S.; Dai, S.; Lai, S. Age, Gender and Metabolic Syndrome-Related Coronary Heart Disease in U.S. Adults. Int. J. Cardiol. 2005, 104, 288–291. [Google Scholar] [CrossRef]
- Gaillard, T.R. The Metabolic Syndrome and Its Components in African-American Women: Emerging Trends and Implications. Front. Endocrinol. 2018, 8. [Google Scholar] [CrossRef]
- Ranasinghe, P.; Mathangasinghe, Y.; Jayawardena, R.; Hills, A.P.; Misra, A. Prevalence and Trends of Metabolic Syndrome among Adults in the Asia-Pacific Region: A Systematic Review. BMC Public Health 2017, 17, 101. [Google Scholar] [CrossRef]
- Yu, S.; Guo, X.; Yang, H.; Zheng, L.; Sun, Y. An Update on the Prevalence of Metabolic Syndrome and Its Associated Factors in Rural Northeast China. BMC Public Health 2014, 14, 877. [Google Scholar] [CrossRef]
- Hajat, C.; Shather, Z. Prevalence of Metabolic Syndrome and Prediction of Diabetes Using IDF versus ATPIII Criteria in a Middle East Population. Diabetes Res. Clin. Pract. 2012, 98, 481–486. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Spence, C.; Yang, W.J.; Ma, G.X. The IDF Definition Is Better Suited for Screening Metabolic Syndrome and Estimating Risks of Diabetes in Asian American Adults: Evidence from NHANES 2011–2016. J. Clin. Med. 2020, 9, 3871. [Google Scholar] [CrossRef] [PubMed]
- Fotouhi, A.; Ebrahimi, H.; Emamian, M.; Khosravi, A.; Hashemi, H. Comparison of the Accuracy of Three Diagnostic Criteria and Estimating the Prevalence of Metabolic Syndrome: A Latent Class Analysis. J. Res. Med. Sci. 2019, 24, 108. [Google Scholar] [CrossRef]
- Fan, N.; Zhang, L.; Xia, Z.; Peng, L.; Wang, Y.; Peng, Y. Sex-Specific Association between Serum Uric Acid and Nonalcoholic Fatty Liver Disease in Type 2 Diabetic Patients. J. Diabetes Res. 2016, 2016, 1–6. [Google Scholar] [CrossRef]
- Shin, D.; Kongpakpaisarn, K.; Bohra, C. Trends in the Prevalence of Metabolic Syndrome and Its Components in the United States 2007–2014. Int. J. Cardiol. 2018, 259, 216–219. [Google Scholar] [CrossRef]
- Krishnamoorthy, Y.; Rajaa, S.; Murali, S.; Rehman, T.; Sahoo, J.; Kar, S.S. Prevalence of Metabolic Syndrome among Adult Population in India: A Systematic Review and Meta-Analysis. PLoS ONE 2020, 15, e0240971. [Google Scholar] [CrossRef]
- Nasreddine, L.; Tamim, H.; Itani, L.; Nasrallah, M.P.; Isma’eel, H.; Nakhoul, N.F.; Abou-Rizk, J.; Naja, F. A Minimally Processed Dietary Pattern Is Associated with Lower Odds of Metabolic Syndrome among Lebanese Adults. Public Health Nutr. 2018, 21, 160–171. [Google Scholar] [CrossRef]
- Massad, S.; Khalili, M.; Karmally, W.; Abdalla, M.; Khammash, U.; Mehari, G.-M.; Deckelbaum, R. Metabolic Syndrome among Refugee Women from the West Bank, Palestine: A Cross-Sectional Study. Nutrients 2018, 10, 1118. [Google Scholar] [CrossRef]
- Zhang, L.; Wang, Z.; Wang, X.; Chen, Z.; Shao, L.; Tian, Y.; Zheng, C.; Li, S.; Zhu, M.; Gao, R. Prevalence of Overweight and Obesity in China: Results from a Cross-Sectional Study of 441 Thousand Adults, 2012–2015. Obesity Res. Clin. Pract. 2020, 14, 119–126. [Google Scholar] [CrossRef]
- Flegal, K.M.; Kruszon-Moran, D.; Carroll, M.D.; Fryar, C.D.; Ogden, C.L. Trends in Obesity among Adults in the United States, 2005 to 2014. JAMA 2016, 315, 2284. [Google Scholar] [CrossRef] [PubMed]
- Revels, S.; Kumar, S.A.P.; Ben-Assuli, O. Predicting Obesity Rate and Obesity-Related Healthcare Costs Using Data Analytics. Health Policy Technol. 2017, 6, 198–207. [Google Scholar] [CrossRef]
- Hirode, G.; Wong, R.J. Trends in the Prevalence of Metabolic Syndrome in the United States, 2011–2016. JAMA 2020, 323, 2526. [Google Scholar] [CrossRef] [PubMed]
- Khan, M.A.; Hashim, M.J.; King, J.; Govender, R.D.; Mustafa, H.; Al Kaabi, J. Epidemiology of Type 2 Diabetes—Global Burden of Disease and Forecasted Trends. J. Epidemiol. Glob. Health 2020, 10, 107–111. [Google Scholar] [CrossRef]
- Sacks, F.M.; Lichtenstein, A.H.; Wu, J.H.Y.; Appel, L.J.; Creager, M.A.; Kris-Etherton, P.M.; Miller, M.; Rimm, E.B.; Rudel, L.L.; Robinson, J.G.; et al. Dietary Fats and Cardiovascular Disease: A Presidential Advisory from the American Heart Association. Circulation 2017, 136, e1–e23. [Google Scholar] [CrossRef]
- Rochlani, Y.; Pothineni, N.V.; Mehta, J.L. Metabolic Syndrome: Does It Differ between Women and Men? Cardiovasc. Drugs Ther. 2015, 29, 329–338. [Google Scholar] [CrossRef]
- Moore, J.X.; Chaudhary, N.; Akinyemiju, T. Metabolic Syndrome Prevalence by Race/Ethnicity and Sex in the United States, National Health and Nutrition Examination Survey, 1988–2012. Preventing Chronic Disease 2017, 14, E24. [Google Scholar] [CrossRef]
- Wong, M.C.S.; Huang, J.; Wang, J.; Chan, P.S.F.; Lok, V.; Chen, X.; Leung, C.; Wang, H.H.X.; Lao, X.Q.; Zheng, Z.-J. Global, Regional and Time-Trend Prevalence of Central Obesity: A Systematic Review and Meta-Analysis of 13.2 Million Subjects. Eur. J. Epidemiol. 2020, 35, 673–683. [Google Scholar] [CrossRef]
- Jeong, H.G.; Park, H. Metabolic Disorders in Menopause. Metabolites 2022, 12, 954. [Google Scholar] [CrossRef]
- da Silva Moura, A.R.; da Paz, S.M.R.S.; de Macêdo Gonçalves Frota, K.; de Carvalho, C.M.R.G. Lifestyle Associated with Risk of Metabolic Syndrome in Adults and the Elderly. Nutrition 2022, 99–100, 111647. [Google Scholar] [CrossRef]
- Noubiap, J.J.; Nansseu, J.R.; Lontchi-Yimagou, E.; Nkeck, J.R.; Nyaga, U.F.; Ngouo, A.T.; Tounouga, D.N.; Tianyi, F.L.; Foka, A.J.; Ndoadoumgue, A.L.; et al. Global, Regional, and Country Estimates of Metabolic Syndrome Burden in Children and Adolescents in 2020: A Systematic Review and Modelling Analysis. Lancet Child Adolesc. Health 2022, 6, 158–170. [Google Scholar] [CrossRef] [PubMed]
- Koskinen, J.; Magnussen, C.G.; Sinaiko, A.; Woo, J.; Urbina, E.; Jacobs, D.R.; Steinberger, J.; Prineas, R.; Sabin, M.A.; Burns, T.; et al. Childhood Age and Associations between Childhood Metabolic Syndrome and Adult Risk for Metabolic Syndrome, Type 2 Diabetes Mellitus and Carotid Intima Media Thickness: The International Childhood Cardiovascular Cohort Consortium. J. Am. Heart Assoc. 2017, 6, e005632. [Google Scholar] [CrossRef] [PubMed]
- Morrison, J.A.; Friedman, L.A.; Gray-McGuire, C. Metabolic Syndrome in Childhood Predicts Adult Cardiovascular Disease 25 Years Later: The Princeton Lipid Research Clinics Follow-up Study. Pediatrics 2007, 120, 340–345. [Google Scholar] [CrossRef] [PubMed]
- DeBoer, M.D. Assessing and Managing the Metabolic Syndrome in Children and Adolescents. Nutrients 2019, 11, 1788. [Google Scholar] [CrossRef]
- Wentzel, A.; Mabhida, S.E.; Ndlovu, M.; Mokoena, H.; Esterhuizen, B.; Sekgala, M.D.; Dludla, P.V.; Kengne, A.P.; Mchiza, Z.J. Prevalence of Metabolic Syndrome in Children and Adolescents with Obesity: A Systematic Review and Meta-Analysis. Obesity 2024, 33, 12–32. [Google Scholar] [CrossRef]
- Lloyd, L.J.; Langley-Evans, S.C.; McMullen, S. Childhood Obesity and Risk of the Adult Metabolic Syndrome: A Systematic Review. Int. J. Obes. 2011, 36, 1–11. [Google Scholar] [CrossRef]
- Ford, E.S.; Li, C. Defining the Metabolic Syndrome in Children and Adolescents: Will the Real Definition Please Stand Up? J. Pediatr. 2008, 152, 160–164.e13. [Google Scholar] [CrossRef]
- Reisinger, C.; Nkeh-Chungag, B.N.; Fredriksen, P.M.; Goswami, N. The Prevalence of Pediatric Metabolic Syndrome—A Critical Look on the Discrepancies between Definitions and Its Clinical Importance. Int. J. Obes. 2020, 45, 12–24. [Google Scholar] [CrossRef]
- Zong, X.; Kelishadi, R.; Kim, H.S.; Schwandt, P.; Matsha, T.E.; Mill, J.G.; Caserta, C.A.; Medeiros, C.C.M.; Kollias, A.; Whincup, P.H.; et al. A Proposed Simplified Definition of Metabolic Syndrome in Children and Adolescents: A Global Perspective. BMC Med. 2024, 22, 190. [Google Scholar] [CrossRef]
- Lim, S. Journal of Obesity & Metabolic Syndrome: A New International Journal Targeting the Pathophysiology and Treatment of Obesity and Metabolic Syndrome. J. Obes. Metab. Synd. 2017, 26, 81–83. [Google Scholar] [CrossRef]
- Srinivasan, V.; Ohta, Y.; Espino, J.; A. Pariente, J.; B. Rodriguez, A.; Mohamed, M.; Zakaria, R. Metabolic Syndrome, Its Pathophysiology and the Role of Melatonin. Recent Pat. Endoc. Metab. Immune Drug Discov. 2012, 7, 11–25. [Google Scholar] [CrossRef]
- McCarty, M.F. Diet/Lifestyle Strategies for Preventing Benign Prostatic Hyperplasia. J. Metab. Synd. 2014, 3. [Google Scholar] [CrossRef]
- Akter, S.; Akhter, H.; Chaudhury, H.S.; Rahman, M.H.; Gorski, A.; Hasan, M.N.; Shin, Y.; Rahman, M.A.; Nguyen, M.N.; Choi, T.G.; et al. Dietary Carbohydrates: Pathogenesis and Potential Therapeutic Targets to Obesity-Associated Metabolic Syndrome. BioFactors 2022, 48, 1036–1059. [Google Scholar] [CrossRef]
- Cifuentes, M.; Verdejo, H.E.; Castro, P.F.; Corvalan, A.H.; Ferreccio, C.; Quest, A.F.G.; Kogan, M.J.; Lavandero, S. Low-Grade Chronic Inflammation: A Shared Mechanism for Chronic Diseases. Physiology 2024, 40, 4–25. [Google Scholar] [CrossRef]
- Maury, E.; Brichard, S.M. Adipokine Dysregulation, Adipose Tissue Inflammation and Metabolic Syndrome. Mol. Cell. Endocrinol. 2010, 314, 1–16. [Google Scholar] [CrossRef]
- Kawai, T.; Autieri, M.V.; Scalia, R. Adipose Tissue Inflammation and Metabolic Dysfunction in Obesity. Am. J. Physiol.-Cell Physiol. 2021, 320, C375–C391. [Google Scholar]
- Jialal, I.; Kaur, H.; Devaraj, S. Toll-like Receptor Status in Obesity and Metabolic Syndrome: A Translational Perspective. J. Clin. Endocrinol. Metab. 2014, 99, 39–48. [Google Scholar] [CrossRef]
| MetS Component | WHO, 1999 | NCEP: ATPIII, 2001 | IDF, 2005 | IDF and AHA/NHLBI, 2009 |
|---|---|---|---|---|
| Obesity | BMI > 30 kg/m2 and/or WHpR > 0.9 in men, >0.85 in women | WC ≥ 102 cm for men and ≥88 cm for women | WC ≥ 94 cm for European men and ≥80 cm for European women, with specific values for other ethnic groups | Increased WC (Population- and country-specific cut-off points) |
| Hypertension | blood pressure ≥ 140/90 mmHg or on antihypertensive treatment | blood pressure ≥ 130/85 mmHg | blood pressure ≥ 130/85 mmHg or treatment of previously diagnosed hypertension | blood pressure ≥ 130/85 mmHg or treatment of previously diagnosed hypertension |
| Hypertriglyceridemia | ≥1.7 mmol/L | ≥1.7 mmol/L | ≥1.7 mmol/L or specific treatment for this lipid abnormality | ≥1.7 mmol/L or specific treatment for this lipid abnormality |
| Low HDL-C | <0.9 mmol/L in men or <1.0 mmol/L in women | <1.04 mmol/L in men or <1.29 mmol/L in women | <1.03 mmol/L in men or <1.29 mmol/L in women or specific treatment for this lipid abnormality | <1.0 mmol/L in men or <1.3 mmol/L in women or specific treatment for this lipid abnormality |
| Hyperglycemia | IR, identified by one of the following: T2DM, IFG ≥ 6.1 mmol/L, IGT ≥ 7.8 mmol/L, Hyperinsulinemia, euglycemic conditions with low glucose uptake | IFG ≥ 6.1 mmol/L | FBG ≥ 5.6 mmol/L or previously diagnosed T2DM | FBG ≥ 5.6 mmol/L or previously diagnosed T2DM |
| Others | Microalbuminuria: Urinary albumin excretion rate ≥ 20 µg/min or albumin/creatinine ratio ≥ 30 mg/g | |||
| MetS criteria | IR PLUS any TWO other components | three or more needed | Obesity PLUS any TWO other components | three or more needed |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Obeidat, A.A.; Ahmad, M.N.; Ghabashi, M.A.; Alazzeh, A.Y.; Habib, S.M.; Abu Al-Haijaa, D.; Azzeh, F.S. Developmental Trends of Metabolic Syndrome in the Past Two Decades: A Narrative Review. J. Clin. Med. 2025, 14, 2402. https://doi.org/10.3390/jcm14072402
Obeidat AA, Ahmad MN, Ghabashi MA, Alazzeh AY, Habib SM, Abu Al-Haijaa D, Azzeh FS. Developmental Trends of Metabolic Syndrome in the Past Two Decades: A Narrative Review. Journal of Clinical Medicine. 2025; 14(7):2402. https://doi.org/10.3390/jcm14072402
Chicago/Turabian StyleObeidat, Ahmad A., Mousa N. Ahmad, Mai A. Ghabashi, Awfa Y. Alazzeh, Salam M. Habib, Dalia Abu Al-Haijaa, and Firas S. Azzeh. 2025. "Developmental Trends of Metabolic Syndrome in the Past Two Decades: A Narrative Review" Journal of Clinical Medicine 14, no. 7: 2402. https://doi.org/10.3390/jcm14072402
APA StyleObeidat, A. A., Ahmad, M. N., Ghabashi, M. A., Alazzeh, A. Y., Habib, S. M., Abu Al-Haijaa, D., & Azzeh, F. S. (2025). Developmental Trends of Metabolic Syndrome in the Past Two Decades: A Narrative Review. Journal of Clinical Medicine, 14(7), 2402. https://doi.org/10.3390/jcm14072402










