Living Donor Liver Transplant Programs in the United States Need to Be Carefully Nurtured Amidst Expanding Use of Perfusion Technology
Abstract
1. Introduction
2. Methods
3. Discussion
3.1. Change in Transplant Trends
3.2. Impact of the Use of Newer Perfusion Technology on Transplant Centers
3.3. Benefits of a Viable LDLT Program
3.4. Status of LDLT in the USA
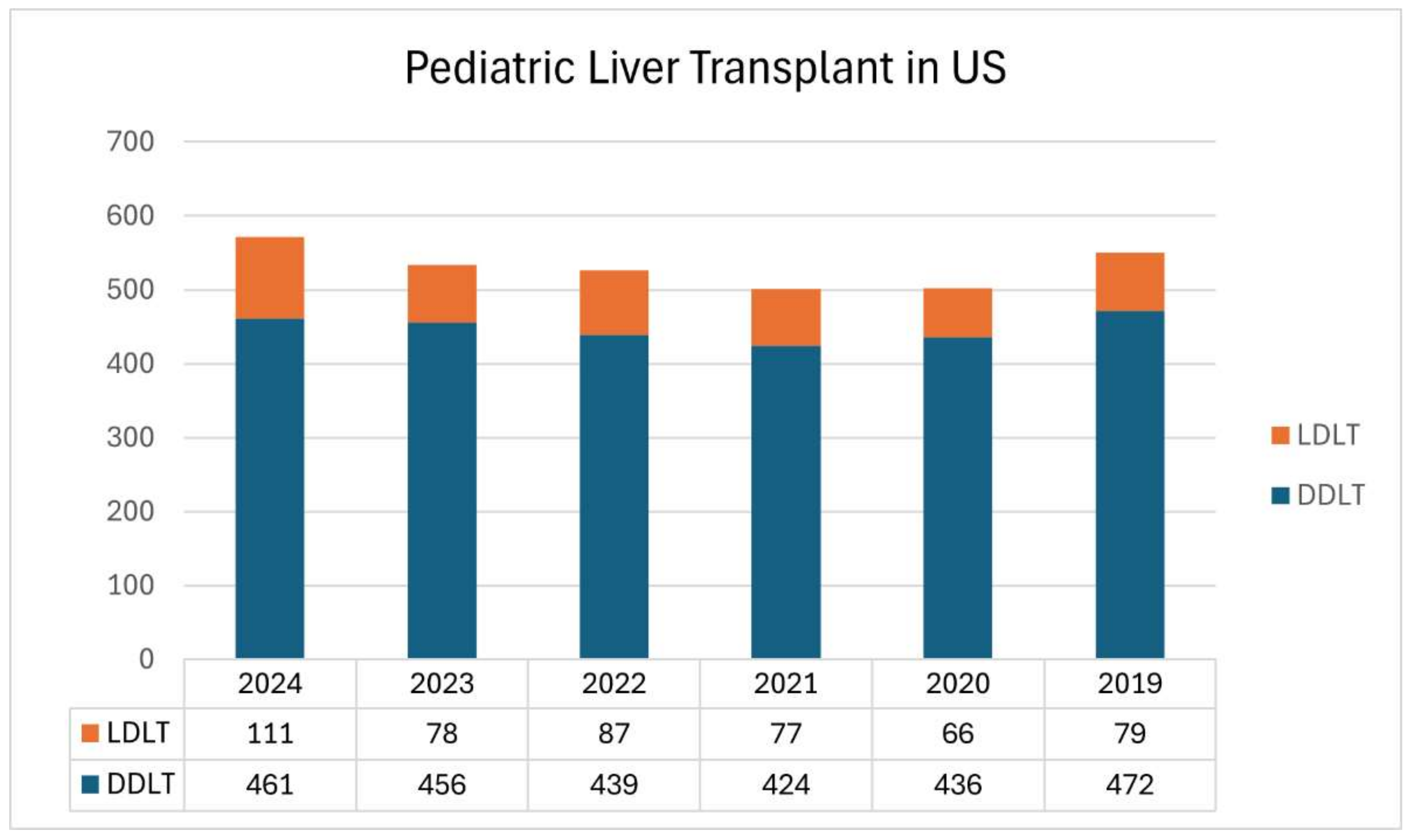
3.5. Pediatric LDLT in the USA
3.6. Can Wider Expansion of DCD Livers in the USA Replicate European Experience?
3.7. Why LDLT Continues to Stagnate in the USA
3.8. The Way Forward
4. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| MASLD | Metabolic Dysfunction-Associated Steatotic Liver Disease |
| DCD | Donation after Cardiac Death |
| DBD | Donation after Brain Death |
| NMP | Normothermic Machine Perfusion |
| HMP | Hypothermic Machine Perfusion |
| NRP | Normothermic Regional Perfusion |
| LDLT | Living Donor Liver Transplantation |
| MELD | Model for End Stage Liver Disease |
| UNOS | United Network for Organ Sharing |
| CRLM | Colorectal Liver metastasis |
| HCC | Hepatocellular Carcinoma |
| ICC | Intrahepatic Cholangiocarcinoma |
| MMAT | Median Meld at Transplantation |
| QALY | Quality Adjusted Life Years |
References
- Matevish, L.E.; Vagefi, P.A.; Patel, M.S. Trends in current use of machine perfusion for donation after cardiac death donors in the US. J. Hepatol. 2024, 81, e187–e188. [Google Scholar] [CrossRef] [PubMed]
- Organ Procurement and Transplantation Network. National Data. Available online: https://optn.transplant.hrsa.gov/data/view-data-reports/national-data/ (accessed on 30 January 2025).
- De Carlis, R.; Muiesan, P.; Taner, B. Donation after circulatory death: Novel strategies to improve the liver transplant outcome. J. Hepatol. 2023, 78, 1169–1180. [Google Scholar] [PubMed]
- Nguyen, M.C.; Zhang, C.; Chang, Y.H.; Li, X.; Ohara, S.Y.; Kumm, K.R.; Cosentino, C.P.; Aqel, B.A.; Lizaola-Mayo, B.C.; Frasco, P.E.; et al. Improved Outcomes and Resource Use with Normothermic Machine Perfusion in Liver Transplantation. JAMA Surg. 2025, 160, 322–330. [Google Scholar] [PubMed]
- Ahmed, O.; Doyle, M.B.M.; Abouljoud, M.S.; Alonso, D.; Batra, R.; Brayman, K.L.; Brockmeier, D.; Cannon, R.M.; Chavin, K.; Delman, A.M.; et al. Liver Transplant Costs and Activity After United Network for Organ Sharing Allocation Policy Changes. JAMA Surg. 2024, 159, 939–947. [Google Scholar]
- Borja-Cacho, D.; Dietch, Z.; Nadig, S.N. Machine Perfusion and Liver Transplantation—The Future Is Now. JAMA Surg. 2025, 160, 330–331. [Google Scholar] [CrossRef]
- Di Napoli, M.; Baimas-George, M.; Bakhtiyar, S.S.; Nydam, T.; Choudhury, R. Cost of Normothermic Regional Perfusion vs Normothermic Machine Perfusion in DCD Liver Transplants: A Markov Decision Analysis. Am. J. Transpl. 2025, 25, s17–s18. [Google Scholar] [CrossRef]
- Kaplan, A.; Winters, A.; Klarman, S.; Kriss, M.; Hughes, D.; Sharma, P.; Asrani, S.; Hutchison, A.; Myoung, P.; Fortune, B.; et al. The rising cost of liver transplantation in the United States. Liver Transpl. 2024. [Google Scholar] [CrossRef]
- Taner, C.B.; Croome, K.P. What is the true cost of DCD liver transplant from a value-based perspective? Liver Transpl. 2024, 30, 769–770. [Google Scholar]
- Boteon, Y.L.; Hessheimer, A.J.; Brüggenwirth, I.M.A.; Boteon, A.P.C.S.; Padilla, M.; de Meijer, V.E.; Domínguez-Gil, B.; Porte, R.J.; Perera, M.T.P.R.; Martins, P.N. The economic impact of machine perfusion technology in liver transplantation. Artif. Organs. 2022, 46, 191–200. [Google Scholar] [CrossRef]
- Omelianchuk, A.; Capron, A.M.; Ross, L.F.; Derse, A.R.; Bernat, J.L.; Magnus, D. Neither Ethical nor Prudent: Why Not to Choose Normothermic Regional Perfusion. Hastings Cent. Rep. 2024, 54, 14–23. [Google Scholar]
- Murphy, N.B.; Slessarev, M.; Basmaji, J.; Blackstock, L.; Blaszak, M.; Brahmania, M.; Chandler, J.A.; Dhanani, S.; Gaulton, M.; Gross, J.A.; et al. Ethical Issues in Normothermic Regional Perfusion in Controlled Organ Donation After Determination of Death by Circulatory Criteria: A Scoping Review. Transplantation 2024. [Google Scholar] [CrossRef] [PubMed]
- Jackson, W.E.; Malamon, J.S.; Kaplan, B.; Saben, J.L.; Schold, J.D.; Pomposelli, J.J.; Pomfret, E.A. Survival Benefit of Living-Donor Liver Transplant. JAMA Surg. 2022, 157, 926–932. [Google Scholar] [CrossRef] [PubMed]
- Humar, A.; Ganesh, S.; Jorgensen, D.; Tevar, A.; Ganoza, A.; Molinari, M.; Hughes, C. Adult Living Donor Versus Deceased Donor Liver Transplant (LDLT Versus DDLT) at a Single Center: Time to Change Our Paradigm for Liver Transplant. Ann. Surg. 2019, 270, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Lai, Q.; Sapisochin, G.; Gorgen, A.; Vitale, A.; Halazun, K.J.; Iesari, S.; Schaefer, B.; Bhangui, P.; Mennini, G.; Wong, T.C.L.; et al. Evaluation of the Intention-to-Treat Benefit of Living Donation in Patients with Hepatocellular Carcinoma Awaiting a Liver Transplant. JAMA Surg. 2021, 156, e213112. [Google Scholar] [CrossRef]
- Magyar, C.T.J.; Li, Z.; Aceituno, L.; Claasen, M.P.A.W.; Ivanics, T.; Choi, W.J.; Rajendran, L.; Sayed, B.A.; Bucur, R.; Rukavina, N.; et al. Temporal evolution of living donor liver transplantation survival-A United Network for Organ Sharing registry study. Am. J. Transplant. 2025, 25, 406–416. [Google Scholar] [CrossRef]
- Li, Z.; Jones, O.; Magyar, C.T.J.; Claasen, M.P.A.W.; Ivanics, T.; Choi, W.J.; Rajendran, L.; Winter, E.; Bucur, R.; Rukavina, N.; et al. Living Donor Availability Improves Patient Survival in a North American Center: An Intention-to-treat Analysis. Ann. Surg. 2024. [Google Scholar] [CrossRef] [PubMed]
- Kwong, A.J.; Jowell, A.; Bambha, K.; Biggins, S.W. Longer-Term Follow-up on Acuity Circle Allocation Strategies in Liver Transplantation. Curr. Transpl. Rep. 2024, 11, 77–83. [Google Scholar] [CrossRef]
- Cussa, D.; Catalano, S.; Labellarte, G.; Novaresio, A.; Pinon, M.; Calvo, P.L.; Peruzzi, L.; Spada, M.; Patrono, D.; Romagnoli, R. An Overview on pediatric living donor liver transplantation. EJT 2024, 2, 44–56. [Google Scholar] [CrossRef]
- Li, Z.; Jones, O.; Takamatsu, F.; Stunguris, J.; Sapisochin, G.; Cattral, M.; Ghanekar, A.; Siddiqui, A.; Ng, V.; Sayed, B.A. Survival benefit of living donor availability for pediatric liver transplantation in a large North American center: An intention-to-treat analysis. Transplantation 2024, 108. [Google Scholar] [CrossRef]
- Hehl, S.J.; Petrowsky, H.; Nadalin, S. Actual perspectives on LDLT in Europe. Updates Surg. 2024. [Google Scholar] [CrossRef]
- Eden, J.; Sousa Da Silva, R.; Cortes-Cerisuelo, M.; Croome, K.; De Carlis, R.; Hessheimer, A.J.; Muller, X.; de Goeij, F.; Banz, V.; Magini, G.; et al. Utilization of livers donated after circulatory death for transplantation—An international comparison. J. Hepatol. 2023, 78, 1007–1016. [Google Scholar] [CrossRef] [PubMed]
- Rela, M.; Rammohan, A. Why are there so many liver transplants from living donors in Asia and so few in Europe and the US? J. Hepatol. 2021, 75, 975–980. [Google Scholar] [CrossRef] [PubMed]
- Pillai, A.; Verna, E.C.; Parikh, N.D.; Cooper, M.; Thiessen, C.; Heimbach, J.; Gordon, E.J.; Sapisochin, G.; Selzner, N.; Mathur, A.; et al. AST LDLT Consensus Conference Working Group. Financial, policy, and ethical barriers to the expansion of living donor liver transplant: Meeting report from a living donor liver transplant consensus conference. Clin. Transplant. 2023, 37, e14955. [Google Scholar] [CrossRef]
- Liapakis, A.; Agbim, U.; Bittermann, T.; Dew, M.A.; Deng, Y.; Gan, G.; Emre, S.; Hunt, H.F.; Olthoff, K.M.; Locke, J.E.; et al. AST LDLT Consensus Conference Working Group. A survey of transplant providers regarding attitudes, barriers, and facilitators to living donor liver transplantation in the United States. Clin. Transpl. 2023, 37, e14967. [Google Scholar] [CrossRef] [PubMed]
- Donor Shield. Donor Shield Direct for Liver Donors. Available online: https://www.donorshield.com/liver-donors/ (accessed on 8 March 2025).


Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kapoor, S.; Desai, C.S. Living Donor Liver Transplant Programs in the United States Need to Be Carefully Nurtured Amidst Expanding Use of Perfusion Technology. J. Clin. Med. 2025, 14, 2259. https://doi.org/10.3390/jcm14072259
Kapoor S, Desai CS. Living Donor Liver Transplant Programs in the United States Need to Be Carefully Nurtured Amidst Expanding Use of Perfusion Technology. Journal of Clinical Medicine. 2025; 14(7):2259. https://doi.org/10.3390/jcm14072259
Chicago/Turabian StyleKapoor, Sorabh, and Chirag S. Desai. 2025. "Living Donor Liver Transplant Programs in the United States Need to Be Carefully Nurtured Amidst Expanding Use of Perfusion Technology" Journal of Clinical Medicine 14, no. 7: 2259. https://doi.org/10.3390/jcm14072259
APA StyleKapoor, S., & Desai, C. S. (2025). Living Donor Liver Transplant Programs in the United States Need to Be Carefully Nurtured Amidst Expanding Use of Perfusion Technology. Journal of Clinical Medicine, 14(7), 2259. https://doi.org/10.3390/jcm14072259





