Lessons Learned from Reconstructing Severe Hand Injuries During the COVID-19 Pandemic
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Statistics and Data Management
3. Results
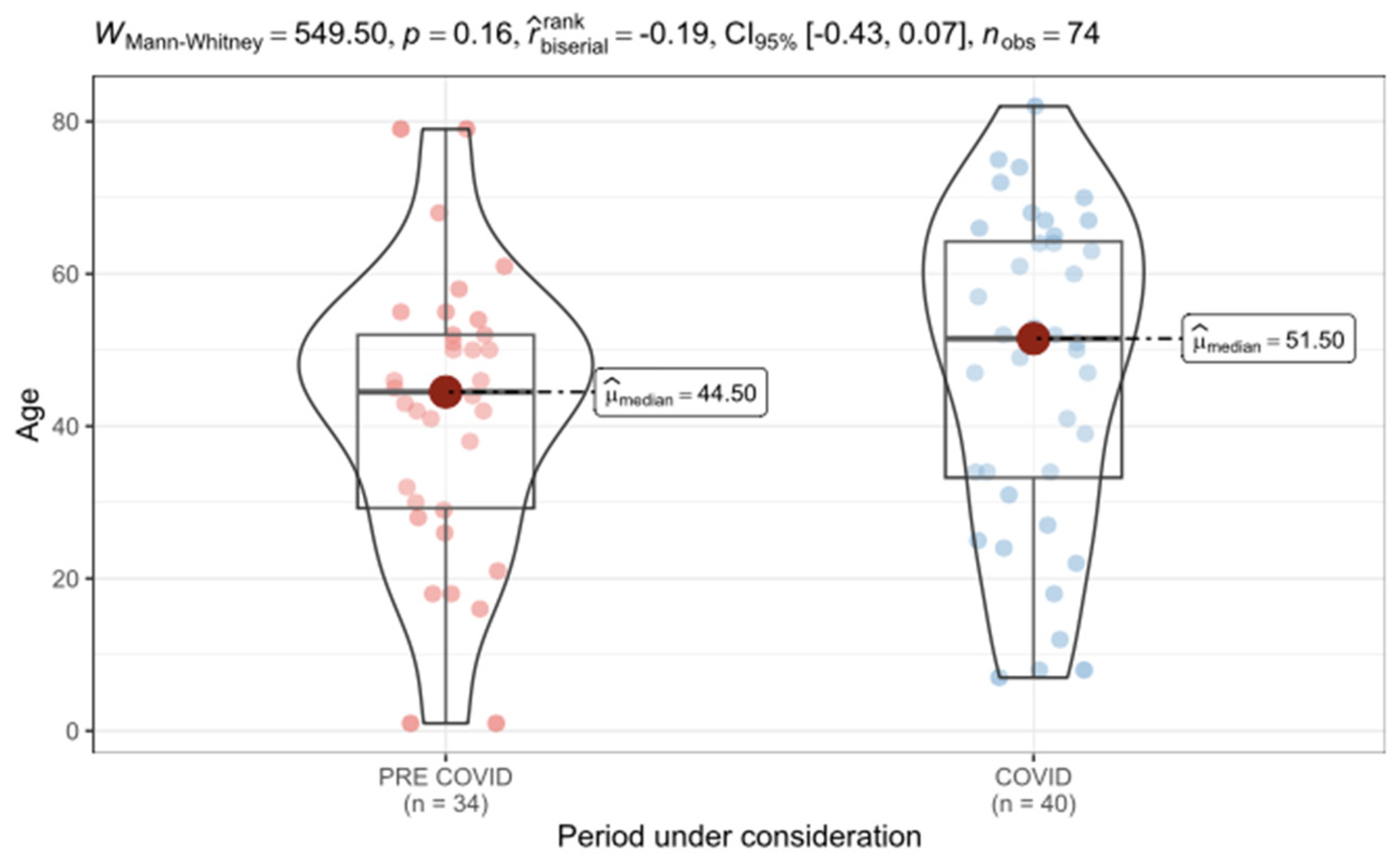
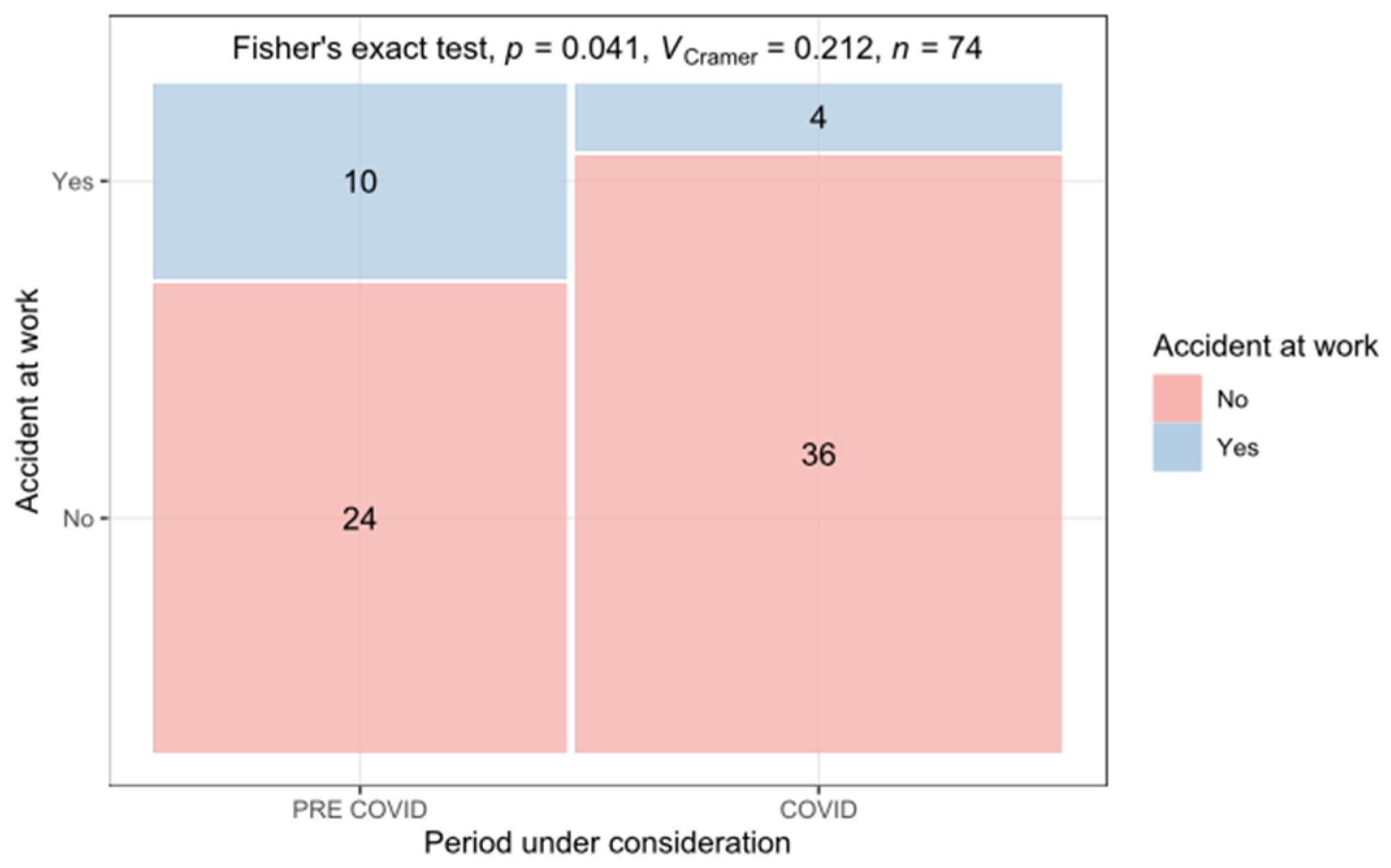
3.1. Trauma Characteristics
3.2. Anatomical Zones of Injury
3.3. Reconstruction/Surgery
3.4. Treatment Characteristics and Postoperative Care
3.5. COVID-19-Specific Challenges and Solutions
3.6. Limitations
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Rosberg, H.E.; Carlsson, K.S.; Cederlund, R.I.; Ramel, E.; Dahlin, L.B. Costs and outcome for serious hand and arm injuries during the first year after trauma—A prospective study. BMC Public Health 2013, 13, 501. [Google Scholar]
- Komatsu, S.; Tamai, S. Successful replantation of a completely cut-off thumb: Case report. Plast. Reconstr. Surg. 1968, 42, 374–377. [Google Scholar] [CrossRef]
- Yoon, A.P.; Mahajani, T.; Hutton, D.W.; Chung, K.C.; for the Finger Replantation and Amputation Challenges in Assessing Impairment, Satisfaction, and Effectiveness (FRANCHISE) Group. Cost-effectiveness of Finger Replantation Compared with Revision Amputation. JAMA Netw. Open 2019, 2, e1916509. [Google Scholar] [CrossRef] [PubMed]
- Hattori, Y.; Doi, K.; Ikeda, K.; Estrella, E.P. A retrospective study of functional outcomes after successful replantation versus amputation closure for single fingertip amputations. J. Hand Surg. Am. 2006, 31, 811–818. [Google Scholar] [CrossRef] [PubMed]
- Giunta, R.E.; Frank, K.; Costa, H.; Demirdöver, C.; di Benedetto, G.; Elander, A.; Henley, M.; Murray, D.J.; Schaefer, D.; Spendel, S.; et al. The COVID-19 Pandemic and its Impact on Plastic Surgery in Europe—An ESPRAS Survey. Handchir. Mikrochir. Plast. Chir. 2020, 52, 221–232. [Google Scholar] [PubMed]
- Qazi, U.A.; Sutton, J.; Farner, S.C.; Bhandari, L. Impact of the COVID-19 Pandemic on the Practice of Hand and Upper Extremity Surgeons. Cureus 2020, 12, e12072. [Google Scholar] [CrossRef] [PubMed]
- Ho, E.; Riordan, E.; Nicklin, S. Hand injuries during COVID-19: Lessons from lockdown. J. Plast. Reconstr. Aesthet. Surg. 2021, 74, 1408–1412. [Google Scholar] [PubMed]
- Kamolz, L.P.; Spendel, S. [The COVID-19 Pandemic and its Consequences for Plastic Surgery and Hand Surgery: A comment from the Graz University Hospital]. Handchir. Mikrochir. Plast. Chir. 2020, 52, 242–243. [Google Scholar] [PubMed]
- Facchin, F.; Messana, F.; Sonda, R.; Faccio, D.; Tiengo, C.; Bassetto, F. COVID-19: Initial experience of hand surgeons in Northern Italy. Hand Surg. Rehabil. 2020, 39, 332–333. [Google Scholar] [PubMed]
- Garude, K.; Natalwala, I.; Hughes, B.; West, C.; Bhat, W. Patterns of Adult and Paediatric Hand Trauma During the COVID-19 Lockdown. J. Plast. Reconstr. Aesthet. Surg. 2020, 73, 1575–1592. [Google Scholar] [CrossRef] [PubMed]
- Mathai, N.J.; Venkatesan, A.S.; Key, T.; Wilson, C.; Mohanty, K. COVID-19 and orthopaedic surgery: Evolving strategies and early experience. Bone Jt. Open. 2020, 1, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Menendez, M.E.; Jawa, A.; Haas, D.A.; Warner, J.J.P.; Codman Shoulder Society. Orthopedic surgery post COVID-19: An opportunity for innovation and transformation. J. Shoulder Elbow Surg. 2020, 29, 1083–1086. [Google Scholar] [CrossRef] [PubMed]
- Grandizio, L.C.; Mettler, A.W.; Caselli, M.E.; Pavis, E.J. Telemedicine After Upper Extremity Surgery: A Prospective Study of Program Implementation. J. Hand Surg. Am. 2020, 45, 795–801. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, C.; Mathiot, A.; Boumediane, M.; Vernet, P.; Schwebel, M.; de Figueiredo, C.; Gouzou, S.; Sauleau, E.; Liverneaux, P.; Facca, S. Organization of outpatient consultations at a hand surgery department in a French university hospital during the COVID-19 lockdown. Hand Surg. Rehabil. 2021, 40, 17–24. [Google Scholar] [CrossRef] [PubMed]
- Pichard, R.; Kopel, L.; Lejeune, Q.; Masmoudi, R.; Masmejean, E.H. Impact of the COronaVIrus Disease 2019 lockdown on hand and upper limb emergencies: Experience of a referred university trauma hand centre in Paris, France. Int. Orthop. 2020, 44, 1497–1501. [Google Scholar] [PubMed]
- McGwin, G.; Taylor, A.J.; MacLennan, P.A.; Rue, L.W. Unusual job activities as a risk factor for occupational injuries. Occup. Med. 2005, 55, 66–68. [Google Scholar] [CrossRef] [PubMed]


| Pre-COVID-19 | COVID-19 | |
|---|---|---|
| MCP/prox. phalanx | 22 (16.9%) | 21 (16.2%) |
| PIP/intermediate phalanx | 22 (16.9%) | 23 (17.7%) |
| DIP/distal phalanx | 11 (8.5%) | 15 (11.5%) |
| IP/distal phalanx | 9 (6.9%) | 7 (5.4%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Glisic, C.; Flores, T.; Konul, E.; Sabitzer, H.; Bartellas, G.; Rohrbacher, A.; Sakar, B.; Klee, S.; Graichen, U.; Platzer, P.; et al. Lessons Learned from Reconstructing Severe Hand Injuries During the COVID-19 Pandemic. J. Clin. Med. 2025, 14, 2169. https://doi.org/10.3390/jcm14072169
Glisic C, Flores T, Konul E, Sabitzer H, Bartellas G, Rohrbacher A, Sakar B, Klee S, Graichen U, Platzer P, et al. Lessons Learned from Reconstructing Severe Hand Injuries During the COVID-19 Pandemic. Journal of Clinical Medicine. 2025; 14(7):2169. https://doi.org/10.3390/jcm14072169
Chicago/Turabian StyleGlisic, Christina, Tonatiuh Flores, Erol Konul, Hugo Sabitzer, Giovanni Bartellas, Alexander Rohrbacher, Berfin Sakar, Sascha Klee, Uwe Graichen, Patrick Platzer, and et al. 2025. "Lessons Learned from Reconstructing Severe Hand Injuries During the COVID-19 Pandemic" Journal of Clinical Medicine 14, no. 7: 2169. https://doi.org/10.3390/jcm14072169
APA StyleGlisic, C., Flores, T., Konul, E., Sabitzer, H., Bartellas, G., Rohrbacher, A., Sakar, B., Klee, S., Graichen, U., Platzer, P., Schrögendorfer, K. F., & Bergmeister, K. (2025). Lessons Learned from Reconstructing Severe Hand Injuries During the COVID-19 Pandemic. Journal of Clinical Medicine, 14(7), 2169. https://doi.org/10.3390/jcm14072169





