Effectiveness of Radiation Shields to Minimize Operator Dose in the Bronchoscopy Suite: A Phantom Study and Clinical Application
Abstract
1. Introduction
2. Materials and Methods
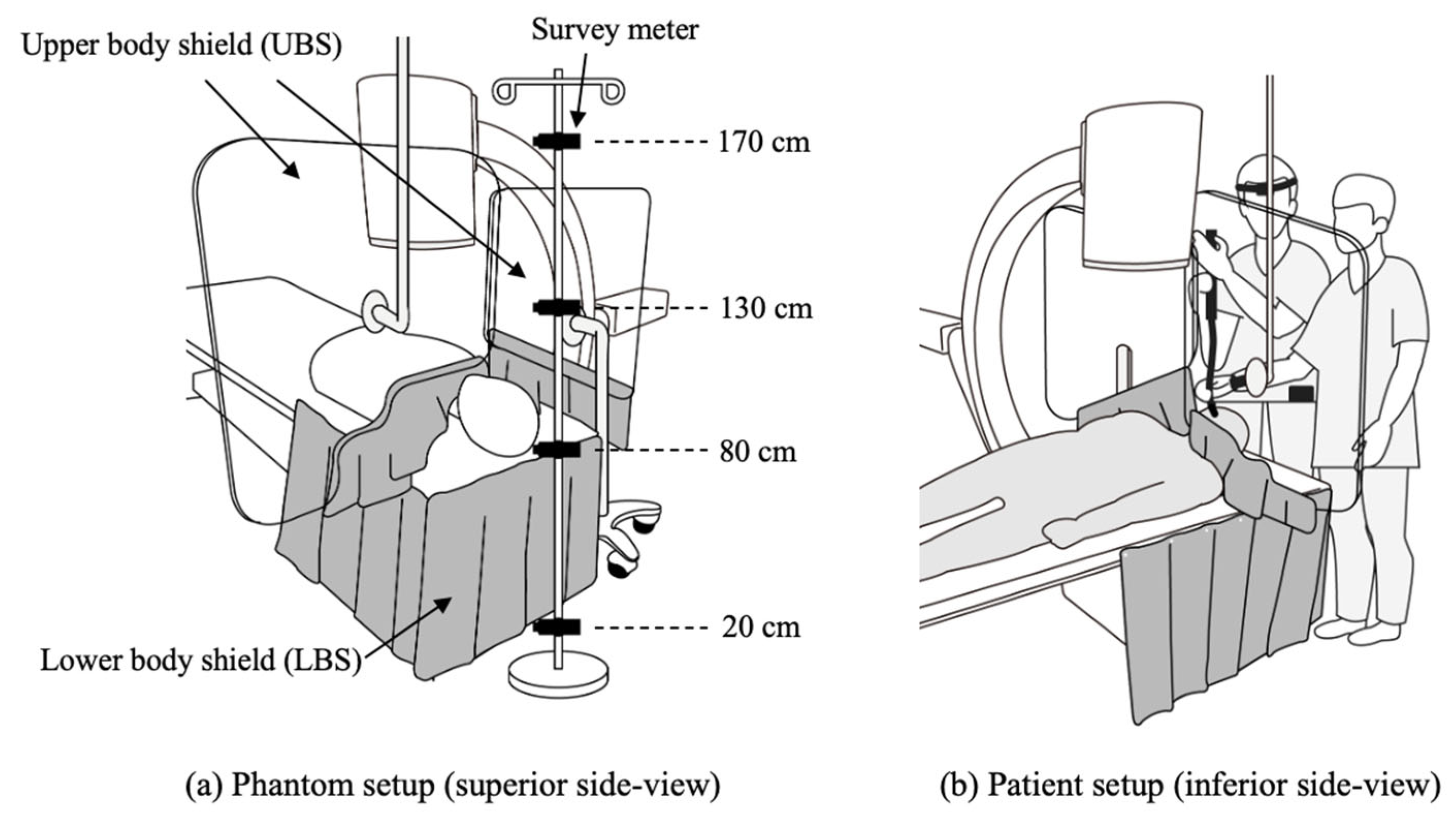
2.1. An X-Ray Unit and Radiation Shielding Devices
2.2. Phantom Study
2.3. Clinical Application
2.4. Analysis
3. Results
3.1. Phantom Study
3.2. Clinical Application
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Asano, F.; Ishida, T.; Shinagawa, N.; Sukoh, N.; Anzai, M.; Kanazawa, K.; Tsuzuku, A.; Morita, S. Virtual bronchoscopic navigation without X-ray fluoroscopy to diagnose peripheral pulmonary lesions: A randomized trial. BMC Pulm. Med. 2017, 17, 184. [Google Scholar] [CrossRef]
- Folch, E.E.; Pritchett, M.A.; Nead, M.A.; Bowling, M.R.; Murgu, S.D.; Krimsky, W.S.; Murillo, B.A.; LeMense, G.P.; Minnich, D.J.; Bansal, S.; et al. Electromagnetic Navigation Bronchoscopy for Peripheral Pulmonary Lesions: One-Year Results of the Prospective, Multicenter NAVIGATE Study. J. Thorac. Oncol. 2019, 14, 445–458. [Google Scholar] [CrossRef] [PubMed]
- Mondoni, M.; Sotgiu, G.; Bonifazi, M.; Dore, S.; Parazzini, E.M.; Carlucci, P.; Gasparini, S.; Centanni, S. Transbronchial needle aspiration in peripheral pulmonary lesions: A systematic review and meta-analysis. Eur. Respir. J. 2016, 48, 196–204. [Google Scholar] [CrossRef]
- Verhoeven, R.L.J.; van der Sterren, W.; Kong, W.; Langereis, S.; van der Tol, P.; van der Heijden, E. Cone-beam CT and Augmented Fluoroscopy-guided Navigation Bronchoscopy: Radiation Exposure and Diagnostic Accuracy Learning Curves. J. Bronchol. Interv. Pulmonol. 2021, 28, 262–271. [Google Scholar] [CrossRef] [PubMed]
- Politi, L.; Biondi-Zoccai, G.; Nocetti, L.; Costi, T.; Monopoli, D.; Rossi, R.; Sgura, F.; Modena, M.G.; Sangiorgi, G.M. Reduction of scatter radiation during transradial percutaneous coronary angiography: A randomized trial using a lead-free radiation shield. Catheter. Cardiovasc. Interv. 2012, 79, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Shorrock, D.; Christopoulos, G.; Wosik, J.; Kotsia, A.; Rangan, B.; Abdullah, S.; Cipher, D.; Banerjee, S.; Brilakis, E.S. Impact of a Disposable Sterile Radiation Shield on Operator Radiation Exposure During Percutaneous Coronary Intervention of Chronic Total Occlusions. J. Invasive Cardiol. 2015, 27, 313–316. [Google Scholar] [CrossRef]
- Domienik, J.; Bissinger, A.; Grabowicz, W.; Jankowski, L.; Krecki, R.; Makowski, M.; Masiarek, K.; Plewka, M.; Lubinski, A.; Peruga, J.Z. The impact of various protective tools on the dose reduction in the eye lens in an interventional cardiology-clinical study. J. Radiol. Prot. 2016, 36, 309–318. [Google Scholar] [CrossRef]
- Morishima, Y.; Chida, K.; Meguro, T. Effectiveness of additional lead shielding to protect staff from scattering radiation during endoscopic retrograde cholangiopancreatography procedures. J. Radiat. Res. 2018, 59, 225–232. [Google Scholar] [CrossRef]
- Chung, K.H.; Park, Y.S.; Ahn, S.B.; Son, B.K. Radiation protection effect of mobile shield barrier for the medical personnel during endoscopic retrograde cholangiopancreatography: A quasi-experimental prospective study. BMJ Open 2019, 9, e027729. [Google Scholar] [CrossRef]
- Minami, T.; Sasaki, T.; Serikawa, M.; Kamigaki, M.; Yukutake, M.; Ishigaki, T.; Ishii, Y.; Mouri, T.; Yoshimi, S.; Shimizu, A.; et al. Occupational Radiation Exposure during Endoscopic Retrograde Cholangiopancreatography and Usefulness of Radiation Protective Curtains. Gastroenterol. Res. Pract. 2014, 2014, 926876. [Google Scholar] [CrossRef]
- Meisinger, Q.C.; Stahl, C.M.; Andre, M.P.; Kinney, T.B.; Newton, I.G. Radiation protection for the fluoroscopy operator and staff. Am. J. Roentgenol. 2016, 207, 745–754. [Google Scholar] [CrossRef] [PubMed]
- Wijma, I.N.; Casal, R.F.; Cheng, G.Z.; Einsiedel, P.F.; Fantin, A.; Hall, D.J.; Herth, F.J.; Ng, C.S.; Pritchett, M.A.; Shah, P.L. Radiation Principles, Protection, and Reporting for Interventional Pulmonology: A World Association of Bronchology and Interventional Pulmonology White Paper. Respiration 2024, 103, 707–721. [Google Scholar] [CrossRef] [PubMed]
- Steinfort, D.P.; Einsiedel, P.; Irving, L.B. Radiation dose to patients and clinicians during fluoroscopically-guided biopsy of peripheral pulmonary lesions. Respir. Care 2010, 55, 1469–1474. [Google Scholar]
- Katsurada, M.; Izumo, T.; Nagai, Y.; Chavez, C.; Kitagawa, M.; Torii, J.; Iwase, T.; Aso, T.; Tsuchida, T.; Sasada, S. The dose and risk factors for radiation exposure to medical staff during endobronchial ultrasonography with a guide sheath for peripheral pulmonary lesions under X-ray fluoroscopy. Jpn. J. Clin. Oncol. 2014, 44, 257–262. [Google Scholar] [CrossRef] [PubMed]
- Haga, Y.; Chida, K.; Kimura, Y.; Yamanda, S.; Sota, M.; Abe, M.; Kaga, Y.; Meguro, T.; Zuguchi, M. Radiation eye dose to medical staff during respiratory endoscopy under X-ray fluoroscopy. J. Radiat. Res. 2020, 61, 691–696. [Google Scholar] [CrossRef]
- Lundvall, L.L.; Sandborg, M. Does Radiological Protection Training or a Real-Time Staff Dosemeter Display Reduce Staff Doses during X-Ray-Guided Pulmonary Bronchoscopy? Radiat. Prot. Dosim. 2022, 198, 265–273. [Google Scholar] [CrossRef]
- Sainz Zuniga, P.V.; Vakil, E.; Molina, S.; Bassett, R.L., Jr.; Ost, D.E. Sensitivity of Radial Endobronchial Ultrasound-Guided Bronchoscopy for Lung Cancer in Patients With Peripheral Pulmonary Lesions: An Updated Meta-analysis. Chest 2020, 157, 994–1011. [Google Scholar] [CrossRef]
- Ulanowski, A.; Kaiser, J.C.; Schneider, U.; Walsh, L. Lifetime radiation risk of stochastic effects—Prospective evaluation for space flight or medicine. Ann. ICRP 2020, 49, 200–212. [Google Scholar] [CrossRef]
- Miller, D.L.; Vano, E.; Bartal, G.; Balter, S.; Dixon, R.; Padovani, R.; Schueler, B.; Cardella, J.F.; de Baere, T.; Cardiovscular; et al. Occupational radiation protection in interventional radiology: A joint guideline of the Cardiovascular and Interventional Radiology Society of Europe and the Society of Interventional Radiology. Cardiovasc. Interv. Radiol. 2010, 33, 230–239. [Google Scholar] [CrossRef]
- McCaffrey, J.; Tessier, F.; Shen, H. Radiation shielding materials and radiation scatter effects for interventional radiology (IR) physicians. Med. Phys. 2012, 39, 4537–4546. [Google Scholar] [CrossRef]
- Yu, C.-Y.; Chou, W.-T.; Liao, Y.-J.; Lee, J.-H.; Liang, J.-A.; Hsu, S.-M. Impact of radiation attenuation by a carbon fiber couch on patient dose verification. Sci. Rep. 2017, 7, 43336. [Google Scholar] [CrossRef] [PubMed]
- Chida, K.; Takahashi, T.; Ito, D.; Shimura, H.; Takeda, K.; Zuguchi, M. Clarifying and visualizing sources of staff-received scattered radiation in interventional procedures. Am. J. Roentgenol. 2011, 197, W900–W903. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H. Three principles for radiation safety: Time, distance, and shielding. Korean J. Pain. 2018, 31, 145–146. [Google Scholar] [CrossRef] [PubMed]
- Chida, K. What are useful methods to reduce occupational radiation exposure among radiological medical workers, especially for interventional radiology personnel? Radiol. Phys. Technol. 2022, 15, 101–115. [Google Scholar] [CrossRef]
- The 2007 Recommendations of the International Commission on Radiological Protection. ICRP publication 103. Ann ICRP 2007, 37, 9–34. [Google Scholar] [CrossRef]

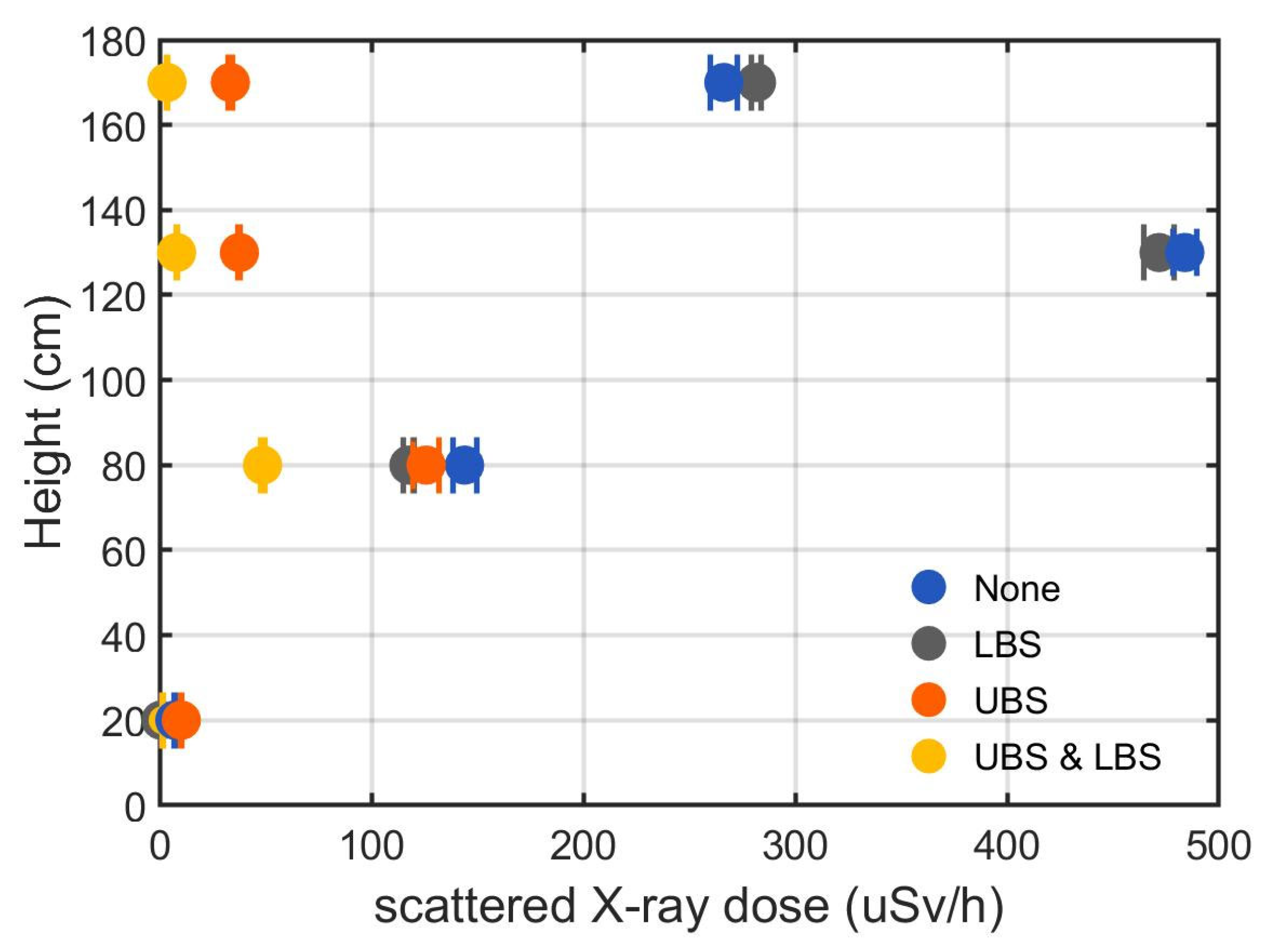
| Shielding Condition | Height | Scattered X-Ray Dose Rate | Shielding Efficacy | |
|---|---|---|---|---|
| UBS | LBS | (cm) | (μSv/h) | |
| No | No | 170 | 266.34 ± 8.86 | - |
| 130 | 483.90 ± 8.01 | - | ||
| 80 | 143.97 ± 8.20 | - | ||
| 20 | 7.22 ± 0.28 | - | ||
| Yes | No | 170 | 33.44 ± 1.16 | 87.4% |
| 130 | 37.71 ± 0.73 | 92.2% | ||
| 80 | 125.84 ± 8.71 | 12.6% | ||
| 20 | 10.29 ± 0.41 | −42.5% | ||
| No | Yes | 170 | 281.75 ± 3.41 | −5.8% |
| 130 | 471.74 ± 10.38 | 2.5% | ||
| 80 | 117.69 ± 3.68 | 18.3% | ||
| 20 | 0.68 ± 0.20 | 90.5% | ||
| Yes | Yes | 170 | 3.52 ± 0.27 | 98.7% |
| 130 | 8.05 ± 0.31 | 98.3% | ||
| 80 | 48.64 ± 1.31 | 66.2% | ||
| 20 | 1.45 ± 0.38 | 79.9% | ||
| General Information of Examination | Scattered X-Ray Dose (uSv/Procedure) | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| ID | Diagnosis | Procedure | Location | Procedure Time (min) | Fluoroscopy Time (min) | Eye (Bronchoscopist) | Chest (Bronchoscopist) | Hypogastrium (Bronchoscopist) | Wrist (Assistant) |
| 1 | Squamous cell carcinoma | EBUS-GS | LUL | 19 | 1.6 | 0.1 | 0.1 | 1.7 | 2.5 |
| 2 | Bronchial tissue | EBUS-GS | LLL | 40 | 7.1 | 0.2 | 0.5 | 1 | 1.7 |
| 3 | A few atypical cell clusters | EBUS-GS | LUL | 21 | 1.6 | 0.1 | 0.2 | 0.2 | 0.2 |
| 4 | Adenocarcinoma | ultrathinTBLB | LUL | 36 | 5.9 | 0.2 | 0.8 | 1.5 | 1.3 |
| 5 | Vague granulomatous reactions | EBUS-GS | RML | 21 | 2.8 | 0.2 | 0.3 | 1.1 | 0.4 |
| 6 | Benign lung tissue | ultrathinTBLB | RLL | 28 | 7.2 | 0.1 | 0.3 | 0.3 | 0.1 |
| 7 | Granulomas without necrosis | EBUS-GS | RUL | 39 | 3.2 | 0.2 | 2.3 | 1.6 | 0.3 |
| 8 | Chronic inflammation with organizing pneumonia pattern | EBUS-GS | LLL | 36 | 5.5 | 0.1 | 0.4 | 0.4 | 2.3 |
| 9 | Chronic inflammation | EBUS-GS | RLL | 27 | 2.8 | 0.2 | 0.2 | 0.2 | 0.3 |
| 10 | Chronic inflammation | EBUS-GS | RLL, RML | 21 | 2.2 | 0.1 | 1.3 | 0.3 | 0.7 |
| 11 | Invasive mucinous adenocarcinoma | EBUS-GS | LLL | 22 | 2.8 | 0.1 | 0.2 | 0.2 | 1.3 |
| 12 | Organizing pneumonia | EBUS-GS | LLL | 25 | 4.6 | 0.1 | 0.1 | 0.4 | 11.9 |
| 13 | Foamy histiocytes in lung alveoli | EBUS-GS | LUL | 33 | 5.0 | 0.1 | 0.3 | 0.4 | 6.4 |
| 14 | Bronchiolitis obliterans (early CLAD) | TBLC | RLL | 66 | 5.7 | 0.2 | 0.4 | 0.2 | 0.3 |
| 15 | Invasive mucinous adenocarcinoma | EBUS-GS | LLL | 35 | 7.3 | 0.1 | 0.2 | 0.52 | 0.5 |
| 16 | Adenocarcinoma | EBUS-GS | RLL | 25 | 3.0 | 0.1 | 0.3 | 0.8 | 0.1 |
| 17 | Adenocarcinoma | EBUS-GS | RUL | 39 | 1.9 | 0.2 | 0.3 | 0.5 | 0.2 |
| 18 | Squamous cell carcinoma | EBUS-GS | RLL | 43 | 4.1 | 0.1 | 0.3 | 1.1 | 0.7 |
| 19 | Bronchial tissue | TBLC | RLL | 50 | 0.9 | 0.1 | 0.5 | 0.2 | 0.1 |
| 20 | Adenocarcinoma | TBLC | RLL | 48 | 0.9 | 0.1 | 0.2 | 0.8 | 0.1 |
| Mean | 33.7 | 3.8 | 0.14 | 0.46 | 0.67 | 1.57 | |||
| Standard deviation | 12.1 | 2.1 | 0.05 | 0.51 | 0.50 | 2.84 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jeon, H.; Kim, D.W.; Joo, J.H.; Ki, Y.; Kang, S.-W.; Shin, W.C.; Yoon, S.H.; Kim, Y.S.; Yong, S.H.; Chung, H.S.; et al. Effectiveness of Radiation Shields to Minimize Operator Dose in the Bronchoscopy Suite: A Phantom Study and Clinical Application. J. Clin. Med. 2025, 14, 2114. https://doi.org/10.3390/jcm14062114
Jeon H, Kim DW, Joo JH, Ki Y, Kang S-W, Shin WC, Yoon SH, Kim YS, Yong SH, Chung HS, et al. Effectiveness of Radiation Shields to Minimize Operator Dose in the Bronchoscopy Suite: A Phantom Study and Clinical Application. Journal of Clinical Medicine. 2025; 14(6):2114. https://doi.org/10.3390/jcm14062114
Chicago/Turabian StyleJeon, Hosang, Dong Woon Kim, Ji Hyeon Joo, Yongkan Ki, Suk-Woong Kang, Won Chul Shin, Seong Hoon Yoon, Yun Seong Kim, Seung Hyun Yong, Hyun Sung Chung, and et al. 2025. "Effectiveness of Radiation Shields to Minimize Operator Dose in the Bronchoscopy Suite: A Phantom Study and Clinical Application" Journal of Clinical Medicine 14, no. 6: 2114. https://doi.org/10.3390/jcm14062114
APA StyleJeon, H., Kim, D. W., Joo, J. H., Ki, Y., Kang, S.-W., Shin, W. C., Yoon, S. H., Kim, Y. S., Yong, S. H., Chung, H. S., Lee, T., & Seol, H. Y. (2025). Effectiveness of Radiation Shields to Minimize Operator Dose in the Bronchoscopy Suite: A Phantom Study and Clinical Application. Journal of Clinical Medicine, 14(6), 2114. https://doi.org/10.3390/jcm14062114






