Short- and Long-Term Mortality in Severely Injured Older Trauma Patients: A Retrospective Analysis
Abstract
1. Introduction
2. Materials and Methods
Statistical Analyses
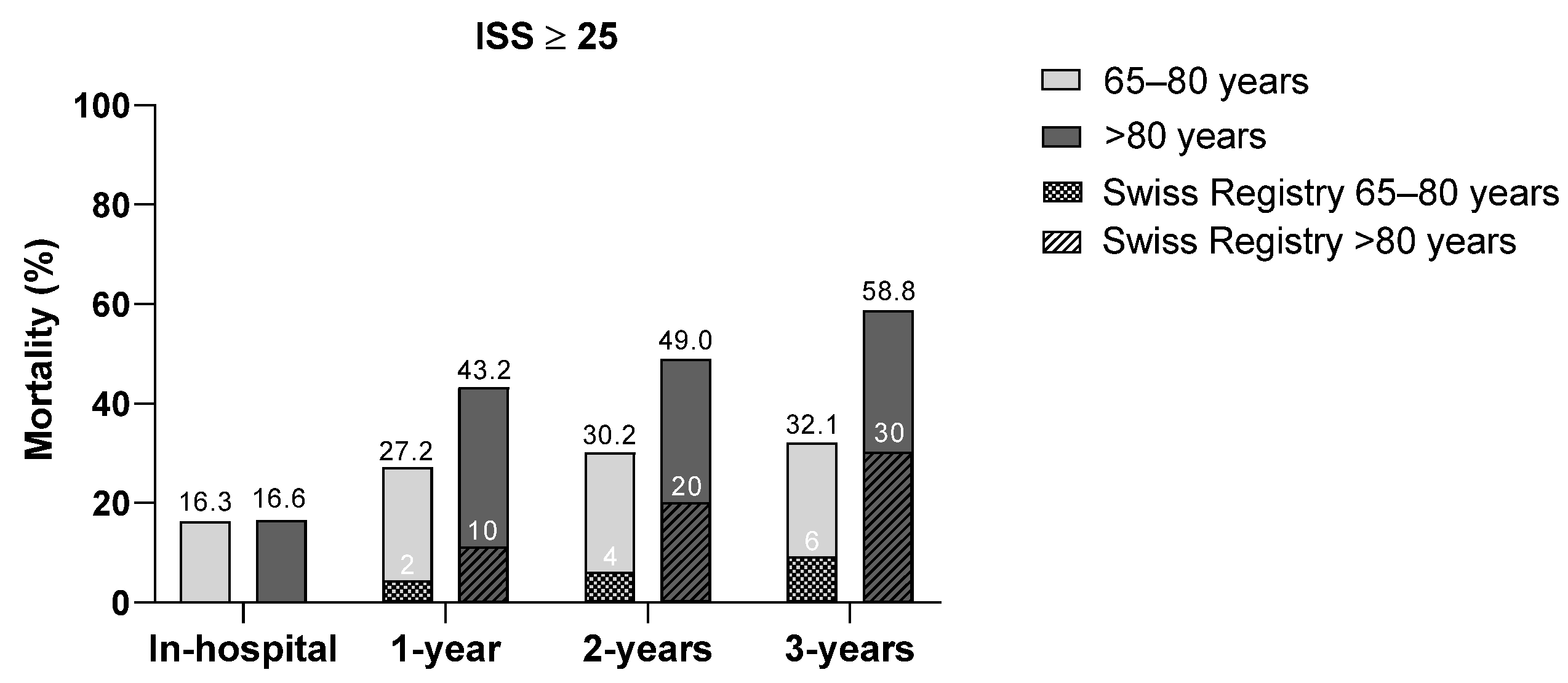
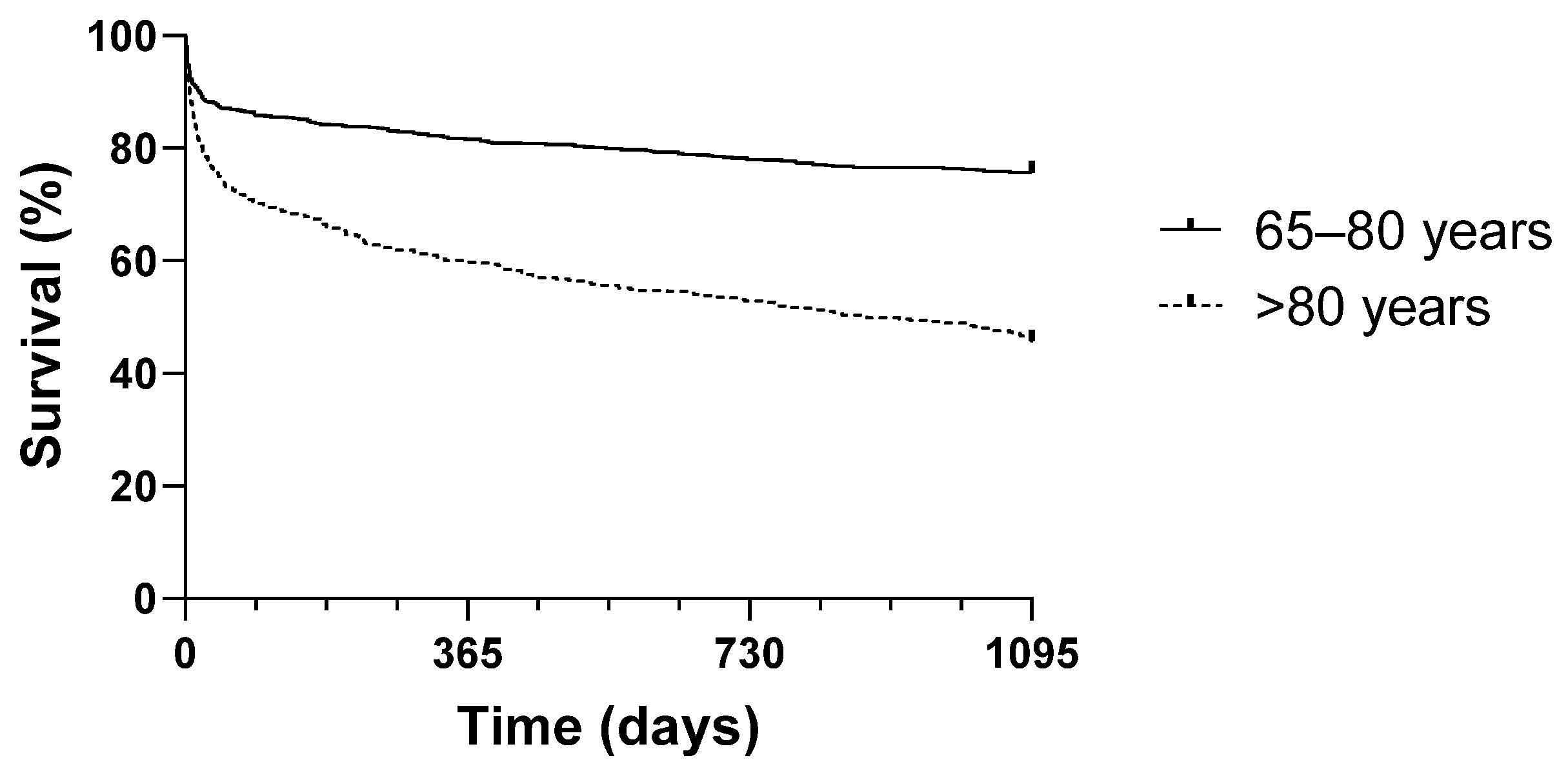
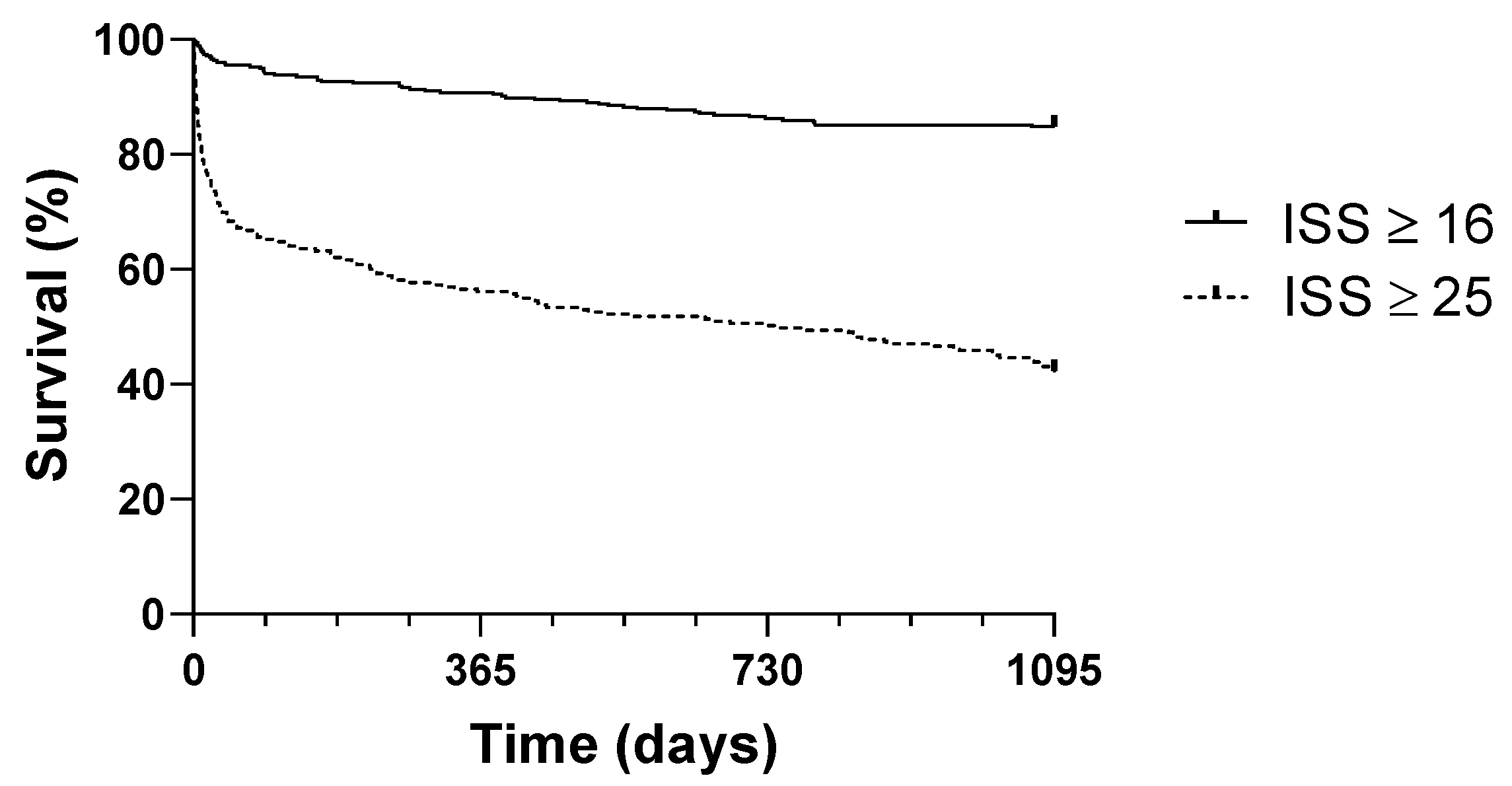
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ISS | Injury Severity Score |
| AIS | Abbreviated Injury Scale |
| SPSS | Statistical Package for Social Sciences |
| GTOS | Geriatric Trauma Outcome Score |
| ICU | intensive care unit |
| PRBCs | packed red blood cells |
| TBI | traumatic brain injury |
References
- World Population Ageing 2020 Highlights Living Arrangements of Older Person; United Nations Department of Economic and Social Affairs, Population Division: New York, NY, USA, 2020.
- Abdelfattah, A.; Core, M.D.; Cannada, L.K.; Watson, J.T. Geriatric High-Energy Polytrauma with Orthopedic Injuries: Clinical Predictors of Mortality. Geriatr. Orthop. Surg. Rehabil. 2014, 5, 173–177. [Google Scholar] [CrossRef] [PubMed]
- McGwin, G., Jr.; Melton, S.M.; May, A.K.; Rue, L.W. Long-term survival in the elderly after trauma. J. Trauma. 2000, 49, 470–476. [Google Scholar] [CrossRef] [PubMed]
- Kuhne, C.A.; Ruchholtz, S.; Kaiser, G.M.; Nast-Kolb, D. Mortality in severely injured elderly trauma patients--when does age become a risk factor? World J. Surg. 2005, 29, 1476–1482. [Google Scholar] [CrossRef] [PubMed]
- Susman, M.; DiRusso, S.M.; Sullivan, T.; Risucci, D.; Nealon, P.; Cuff, S.; Haider, A.; Benzil, D. Traumatic brain injury in the elderly: Increased mortality and worse functional outcome at discharge despite lower injury severity. J. Trauma. 2002, 53, 219–223; discussion 223–214. [Google Scholar] [CrossRef]
- Benhamed, A.; Batomen, B.; Boucher, V.; Yadav, K.; Mercier, É.; Isaac, C.J.; Bérubé, M.; Bernard, F.; Chauny, J.M.; Moore, L.; et al. Epidemiology, injury pattern and outcome of older trauma patients: A 15-year study of level-I trauma centers. PLoS ONE 2023, 18, e0280345. [Google Scholar] [CrossRef]
- El-Qawaqzeh, K.; Anand, T.; Alizai, Q.; Colosimo, C.; Hosseinpour, H.; Spencer, A.; Ditillo, M.; Magnotti, L.J.; Stewart, C.; Joseph, B. Trauma in the Geriatric and the Super-Geriatric: Should They Be Treated the Same? J. Surg. Res. 2024, 293, 316–326. [Google Scholar] [CrossRef]
- Maek, T.; Fochtmann, U.; Jungbluth, P.; Pass, B.; Lefering, R.; Schoeneberg, C.; Lendemans, S.; Hussmann, B. Reality of treatment for severely injured patients: Are there age-specific differences? BMC Emerg. Med. 2024, 24, 14. [Google Scholar] [CrossRef]
- de Vries, R.; Reininga, I.H.F.; de Graaf, M.W.; Heineman, E.; El Moumni, M.; Wendt, K.W. Older polytrauma: Mortality and complications. Injury 2019, 50, 1440–1447. [Google Scholar] [CrossRef]
- Haentjens, P.; Magaziner, J.; Colón-Emeric, C.S.; Vanderschueren, D.; Milisen, K.; Velkeniers, B.; Boonen, S. Meta-analysis: Excess mortality after hip fracture among older women and men. Ann. Intern. Med. 2010, 152, 380–390. [Google Scholar] [CrossRef]
- Jojczuk, M.; Pawlikowski, J.; Kamiński, P.; Głuchowski, D.; Naylor, K.; Gajewski, J.; Karpiński, R.; Krakowski, P.; Jonak, J.; Nogalski, A.; et al. Evaluating Changes in Trauma Epidemiology during the COVID-19 Lockdown: Insights and Implications for Public Health and Disaster Preparedness. Healthcare 2023, 11, 2436. [Google Scholar] [CrossRef]
- Jojczuk, M.; Naylor, K.; Serwin, A.; Dolliver, I.; Głuchowski, D.; Gajewski, J.; Karpiński, R.; Krakowski, P.; Torres, K.; Nogalski, A.; et al. Descriptive Analysis of Trauma Admission Trends Before and During the COVID-19 Pandemic. J. Clin. Med. 2024, 13, 259. [Google Scholar] [CrossRef] [PubMed]
- Majdan, M.; Plancikova, D.; Brazinova, A.; Rusnak, M.; Nieboer, D.; Feigin, V.; Maas, A. Epidemiology of traumatic brain injuries in Europe: A cross-sectional analysis. Lancet Public Health 2016, 1, e76–e83. [Google Scholar] [CrossRef] [PubMed]
- Roozenbeek, B.; Maas, A.I.; Menon, D.K. Changing patterns in the epidemiology of traumatic brain injury. Nat. Rev. Neurol. 2013, 9, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Ranson, R.; Esper, G.W.; Woodruff, R.; Solasz, S.J.; Egol, K.A.; Konda, S.R. The effect of traumatic head injuries on the outcome of middle-aged and geriatric orthopedic trauma patients. Injury 2024, 55, 111299. [Google Scholar] [CrossRef]
- Forssten, S.P.; Ahl Hulme, R.; Forssten, M.P.; Ribeiro, M.A.F., Jr.; Sarani, B.; Mohseni, S. Predictors of outcomes in geriatric patients with moderate traumatic brain injury after ground level falls. Front. Med. 2023, 10, 1290201. [Google Scholar] [CrossRef]
- Klang, A.; Molero, Y.; Lichtenstein, P.; Larsson, H.; D’Onofrio, B.M.; Marklund, N.; Oldenburg, C.; Rostami, E. Access to Rehabilitation After Hospitalization for Traumatic Brain Injury: A National Longitudinal Cohort Study in Sweden. Neurorehabilit. Neural Repair. 2023, 37, 763–774. [Google Scholar] [CrossRef]
- Bradley, L.; Wheelwright, S. The impact of delays in transfer to specialist rehabilitation on outcomes in patients with acquired brain injury. Clin. Rehabil. 2024, 38, 1552–1558. [Google Scholar] [CrossRef]
- Andelic, N.; Røe, C.; Tenovuo, O.; Azouvi, P.; Dawes, H.; Majdan, M.; Ranta, J.; Howe, E.I.; Wiegers, E.J.A.; Tverdal, C.; et al. Unmet Rehabilitation Needs After Traumatic Brain Injury Across Europe: Results from the CENTER-TBI Study. J. Clin. Med. 2021, 10, 1035. [Google Scholar] [CrossRef]
- Tyll, T.; Bubeníková, A.; Votava, J.; Pochop, M.; Soták, M. Survival and predictive factors of clinical outcome in patients with severe acquired brain injury. Eur. J. Phys. Rehabil. Med. 2024, 60, 597–603. [Google Scholar] [CrossRef]
- Kuo, S.C.H.; Kuo, P.J.; Chen, Y.C.; Chien, P.C.; Hsieh, H.Y.; Hsieh, C.H. Comparison of the new Exponential Injury Severity Score with the Injury Severity Score and the New Injury Severity Score in trauma patients: A cross-sectional study. PLoS ONE 2017, 12, e0187871. [Google Scholar] [CrossRef]
- Zhao, F.Z.; Wolf, S.E.; Nakonezny, P.A.; Minhajuddin, A.; Rhodes, R.L.; Paulk, M.E.; Phelan, H.A. Estimating Geriatric Mortality After Injury Using Age, Injury Severity, and Performance of a Transfusion: The Geriatric Trauma Outcome Score. J. Palliat. Med. 2015, 18, 677–681. [Google Scholar] [CrossRef]
- Scherer, J.; Kalbas, Y.; Ziegenhain, F.; Neuhaus, V.; Lefering, R.; Teuben, M.; Sprengel, K.; Pape, H.C.; Jensen, K.O. The GERtality Score: The Development of a Simple Tool to Help Predict in-Hospital Mortality in Geriatric Trauma Patients. J. Clin. Med. 2021, 10, 1362. [Google Scholar] [CrossRef]

| All Patients (n = 1189) | 65–80 Years (n = 755) | >80 Years (n = 434) | p-Value | |
|---|---|---|---|---|
| Males, % (n) | 61.9 (736) | 67.0 (506) | 53.0 (230) | <0.001 |
| GCS, mean ± SD | 13.0 ± 3.6 | 12.8 ± 3.8 | 13.4 ±3.1 | <0.001 |
| GCS ≤ 8, % (n) | 10.7 (127) | 12.6 (95) | 7.4 (32) | 0.005 |
| ISS, mean ± SD | 24.3 ± 7.9 | 24.4 ± 8.4 | 23.9 ± 6.9 | 0.004 |
| ISS ≥ 25, % (n) | 54.8 (651) | 52.7 (398) | 58.3 (253) | 0.063 |
| AIS head ≥ 3, % (n) | 70.6 (839) | 67.9 (513) | 75.1 (326) | 0.009 |
| AIS thorax ≥ 3, % (n) | 28.2 (335) | 31.1 (235) | 23 (100) | 0.003 |
| AIS abdomen ≥ 3, % (n) | 5.6 (66) | 6.4 (48) | 4.1 (18) | 0.109 |
| AIS upper extremity ≥ 3, % (n) | 1.2 (14) | 1.5 (11) | 0.7 (3) | 0.239 |
| AIS lower extremity ≥ 3, % (n) | 16.6 (197) | 17.1 (129) | 15.7 (68) | 0.527 |
| Duration in intensive care (h) | 58.7 ± 78 | 66.3 ± 98.4 | 90.4 ± 47.8 | <0.001 |
| Length of stay (d) | 9.3 ± 13.7 | 10.1 ±15.5 | 8 ± 9.9 | 0.01 |
| Injury mechanism | ||||
| Blunt trauma, % (n) | 98.7 (1173) | 98.3 (742) | 99.3 (431) | 0.279 |
| Traffic accident, % (n) | 22.5 (267) | 27.5 (208) | 13.7 (59) | <0.001 |
| Fall at ground level, % (n) | 13.5 (160) | 10.5 (79) | 18.7 (81) | <0.001 |
| Fall < 3 m, % (n) | 43.8 (521) | 38.4 (290) | 53.2 (231) | <0.001 |
| Fall > 3 m, % (n) | 11.2 (133) | 13.9 (105) | 6.5 (28) | <0.001 |
| All Patients (n = 1189) | 65–80 Years (n = 755) | >80 Years (n = 434) | p-Value | |
|---|---|---|---|---|
| Mortality | ||||
| In-hospital mortality, % (n) | 10.3 (123) | 9.5 (72) | 11.8 (51) | 0.227 |
| 1-year mortality, % (n) | 26.5 (315) | 18.8 (142) | 39.9 (173) | <0.001 |
| 2-year mortality, % (n) | 31.5 (310) | 22.8 (143) | 46.5 (167) | <0.001 |
| 3-year mortality, % (n) | 36.3 (297) | 24.9 (130) | 56.4 (167) | <0.001 |
| Discharge status | ||||
| Home, % (n) | 19.2 (228) | 24.0 (181) | 10.8 (47) | <0.001 |
| Elderly home, % (n) | 5.8 (69) | 4.0 (30) | 9.0 (39) | <0.001 |
| Rehabilitation, % (n) | 15.7 (187) | 18.4 (139) | 11.1 (48) | <0.001 |
| Other hospital, % (n) | 48.2 (573) | 43.3 (327) | 56.7 (246) | <0.001 |
| Other/unknown, % (n) | 0.6 (7) | 0.7 (5) | 0.5 (2) | 1.0 |
| Risk Factors for In-Hospital Mortality in All Patients | p-Value | Adjusted OR (95% CI) |
|---|---|---|
| Age | 0.001 | 1.05 (1.02–1.08) |
| AIS head ≥ 3 | <0.001 | 5.98 (3.71–9.63) |
| ISS | <0.001 | 1.12 (1.09–1.16) |
| Risk Factors for 1-Year Mortality in Patients Surviving Hospital Discharge | ||
| Age | <0.001 | 1.12 (1.09–1.15) |
| AIS head ≥ 3 | 0.001 | 2.59 (1.46–4.58) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ivanova, S.; Hilverdink, E.F.; Bastian, J.D.; Jakob, D.A.; Exadaktylos, A.K.; Keel, M.J.B.; Schefold, J.C.; Anwander, H.; Lustenberger, T. Short- and Long-Term Mortality in Severely Injured Older Trauma Patients: A Retrospective Analysis. J. Clin. Med. 2025, 14, 2064. https://doi.org/10.3390/jcm14062064
Ivanova S, Hilverdink EF, Bastian JD, Jakob DA, Exadaktylos AK, Keel MJB, Schefold JC, Anwander H, Lustenberger T. Short- and Long-Term Mortality in Severely Injured Older Trauma Patients: A Retrospective Analysis. Journal of Clinical Medicine. 2025; 14(6):2064. https://doi.org/10.3390/jcm14062064
Chicago/Turabian StyleIvanova, Silviya, Elsa F. Hilverdink, Johannes D. Bastian, Dominik A. Jakob, Aristomenis K. Exadaktylos, Marius J. B. Keel, Joerg C. Schefold, Helen Anwander, and Thomas Lustenberger. 2025. "Short- and Long-Term Mortality in Severely Injured Older Trauma Patients: A Retrospective Analysis" Journal of Clinical Medicine 14, no. 6: 2064. https://doi.org/10.3390/jcm14062064
APA StyleIvanova, S., Hilverdink, E. F., Bastian, J. D., Jakob, D. A., Exadaktylos, A. K., Keel, M. J. B., Schefold, J. C., Anwander, H., & Lustenberger, T. (2025). Short- and Long-Term Mortality in Severely Injured Older Trauma Patients: A Retrospective Analysis. Journal of Clinical Medicine, 14(6), 2064. https://doi.org/10.3390/jcm14062064







