Cardiorespiratory Effects of Inverse Ratio Ventilation in Obese Patients During Laparoscopic Surgery: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Eligibility Criteria
- Population (P): This study included adult patients (aged ≥18 years) with obesity (BMI ≥30 kg/m2) who underwent laparoscopic surgery.
- Intervention (I): Patients received IRV (I:E >1) during mechanical ventilation under general anesthesia.
- Comparison (C): Patients in the control group were ventilated using conventional ventilation without prolonged inspiratory time or IRV.
- Outcomes (O): The primary outcome of interest is the change in respiratory mechanics, including peak inspiratory pressure (PPeak), plateau pressure (PPlat), mean airway pressure (PMean), PEEP, auto-PEEP, dynamic compliance (CDyn), and static compliance (CStat). The secondary outcomes include the effect on oxygenation (e.g., peripheral arterial oxygenation [SaO2], arterial oxygen pressure [PaO2], arterial CO2 pressure [PaCO2], pH, and the PaO2/Fraction of inspired oxygen [FiO2] ratio [P/F ratio]), hemodynamic parameters (mean arterial pressure [MAP], heart rate [HR]), inflammatory response cytokines (e.g., tumor necrosis factor-alpha [TNF-α], interleukin-1, 6, or 8 [IL-1, IL-6, or IL-8]), intraoperative complications, and postoperative complications. Postoperative complications will be evaluated as a composite of postoperative pulmonary complications (POPCs) [9,10] and non-POPCs, all observed within the postoperative monitoring timeframe. The evaluation was conducted using only pre- and post-pneumoperitoneum measurements. In cases where multiple measurements were available, preference was given to those taken immediately before and after pneumoperitoneum, rather than those taken earlier or later.
- Study Design (S): This review included prospective randomized controlled trials (RCTs) published in English, focusing on adult patients undergoing laparoscopic surgery. Studies were excluded if they were observational, non-clinical, lacked sufficient data or full-text availability, involved obese adults not undergoing laparoscopic surgery, addressed pediatric populations, or were not peer-reviewed.
2.2. Search Strategy
2.3. Study Selection, Data Extraction, and Data Retrieval
2.4. Quality Assessment and Certainty of Evidence Assessment
2.5. Statistical Analysis
3. Results
3.1. Paper Selection
3.2. Study Characteristics
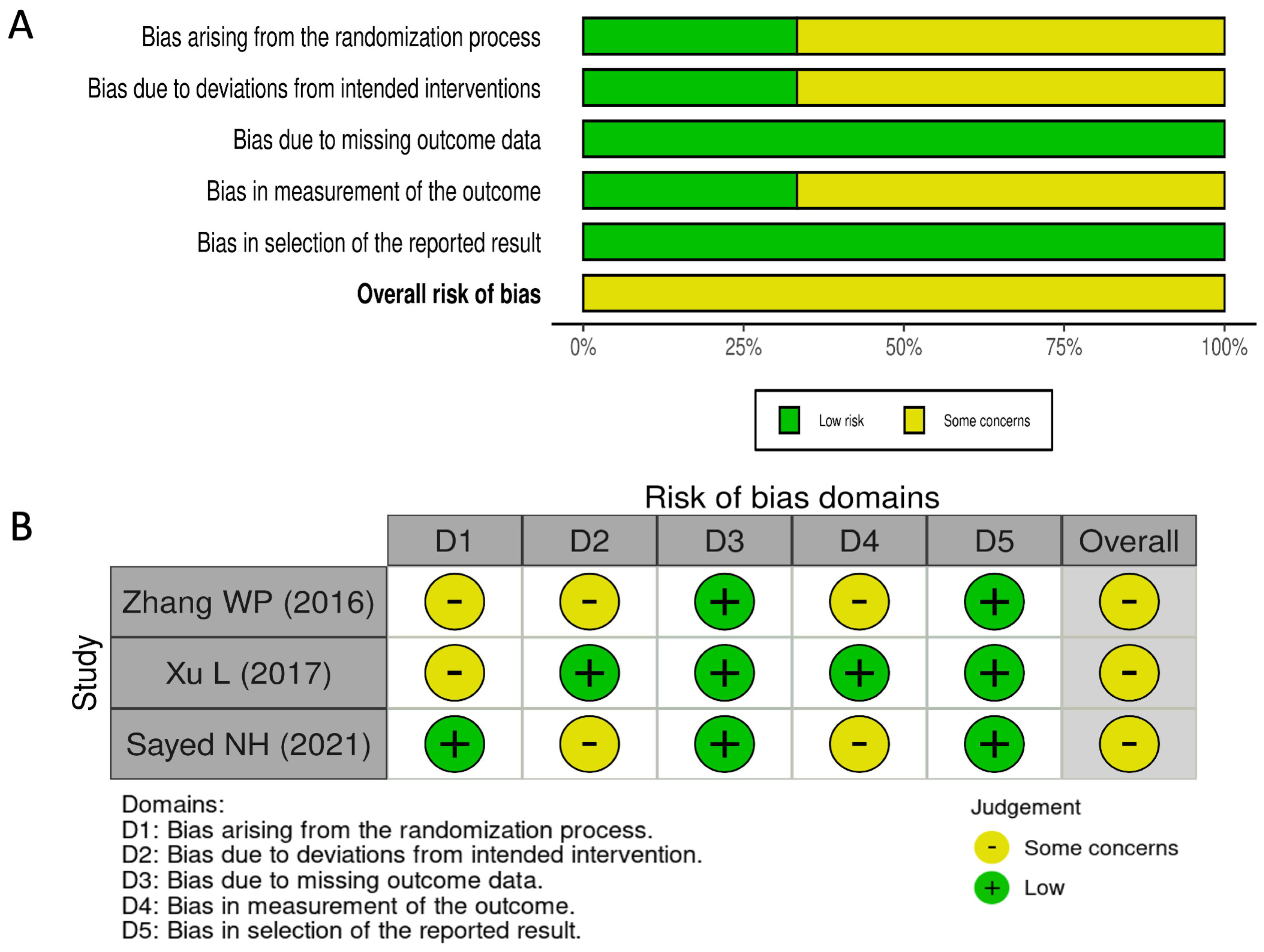
3.3. Risk of Bias Assessment
3.4. Primary Endpoint
3.5. Secondary Endpoints
3.5.1. Gas Exchange
3.5.2. Hemodynamics
3.5.3. Inflammatory Cytokines
3.5.4. Postoperative Complications
4. Discussion
Strengths and Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Carron, M.; Safaee Fakhr, B.; Ieppariello, G.; Foletto, M. Perioperative care of the obese patient. J. Br. Surg. 2020, 107, e39–e55. [Google Scholar] [CrossRef] [PubMed]
- Pelosi, P.; Gregoretti, C. Perioperative management of obese patients. Best Pract. Res. Clin. Anaesthesiol. 2010, 24, 211–225. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Zeng, J.; Zhang, C.; Zheng, W.; Huang, X.; Zhao, N.; Duan, G.; Yu, C. Optimized ventilation strategy for surgery on patients with obesity from the perspective of lung protection: A network meta-analysis. Front. Immunol. 2022, 13, 1032783. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, N.T.; Wolfe, B.M. The physiologic effects of pneumoperitoneum in the morbidly obese. Ann. Surg. 2005, 241, 219–226. [Google Scholar] [CrossRef]
- Hirabayashi, G.; Yokose, Y.; Oshika, H.; Saito, M.; Maruyama, K.; Andoh, T. Effects of volume-targeted pressure-controlled inverse ratio ventilation on functional residual capacity and dead space in obese patients undergoing robot-assisted laparoscopic radical prostatectomy. BJA Open. 2022, 3, 100020. [Google Scholar] [CrossRef]
- Jinghua, W.; Xiong, N.; Min, L. The effect of inverse ratio ventilation on cardiopulmonary function in obese laparoscopic surgery patients: A systematic review and meta-analysis. Saudi J. Anaesth. 2024, 18, 77–85. [Google Scholar] [CrossRef]
- Jones, R.L.; Nzekwu, M.M. The effects of body mass index on lung volumes. Chest 2006, 130, 827–833. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef]
- Miskovic, A.; Lumb, A.B. Postoperative pulmonary complications. Br. J. Anaesth. 2017, 118, 317–334. [Google Scholar] [CrossRef]
- Writing Committee for the PROBESE Collaborative Group of the PROtective VEntilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology; Bluth, T.; Bobek, I.; Canet, J.C.; Cinnella, G.; de Baerdemaeker, L.; Gama de Abreu, M.; Gregoretti, C.; Hedenstierna, G.; Hemmes, S.N.T.; et al. Effect of Intraoperative High Positive End-Expiratory Pressure (PEEP) With Recruitment Maneuvers vs Low PEEP on Postoperative Pulmonary Complications in Obese Patients: A Randomized Clinical Trial. JAMA 2019, 321, 2292–2305. [Google Scholar]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Puhan, M.A.; Schünemann, H.J.; Murad, M.H.; Li, T.; Brignardello-Petersen, R.; Singh, J.A.; Kessels, A.G.; Guyatt, G.H.; GRADE Working Group. A GRADE Working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ 2014, 349, g5630. [Google Scholar] [CrossRef] [PubMed]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 135. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Sterne, J.A.; Sutton, A.J.; Ioannidis, J.P.; Terrin, N.; Jones, D.R.; Lau, J.; Carpenter, J.; Rücker, G.; Harbord, R.M.; Schmid, C.H.; et al. Recommendations for Examining and Interpreting Funnel Plot Asymmetry in Meta-Analyses of Randomised Controlled Trials. BMJ 2011, 343, d4002. [Google Scholar] [CrossRef]
- Zhang, W.P.; Zhu, S.M. The effects of inverse ratio ventilation on cardiopulmonary function and inflammatory cytokine of bronchoaveolar lavage in obese patients undergoing gynecological laparoscopy. Acta Anaesthesiol. Taiwanica 2016, 54, 1–5. [Google Scholar] [CrossRef]
- Xu, L.; Shen, J.; Yan, M. The effect of pressure-controlled inverse ratio ventilation on lung protection in obese patients undergoing gynecological laparoscopic surgery. J. Anesth. 2017, 31, 651–656. [Google Scholar] [CrossRef]
- Sayed, N.H.; Elaziz, M.S.A.; Elkholy, A.S.; Taeimah, M.O. Effect of inverse ratio ventilation on hemodynamics and respiratory mechanics in obese patients undergoing laparoscopic sleeve gastrectomy. Ain-Shams J. Anesthesiol. 2021, 13, 31. [Google Scholar] [CrossRef]
- Fahy, B.G.; Barnas, G.M.; Nagle, S.E.; Flowers, J.L.; Njoku, M.J.; Agarwal, M. Effects of Trendelenburg and reverse Trendelenburg postures on lung and chest wall mechanics. J. Clin. Anesth. 1996, 8, 236–244. [Google Scholar] [CrossRef]
- Tamburini, E.; Ocagli, H.; Carron, M. Role of recruitment manoeuvres in reducing postoperative pulmonary complications during driving pressure-guided ventilation: A meta-analysis and sequential analysis. Br. J. Anaesth. 2025, in press. [Google Scholar] [CrossRef]
- Frank, J.A.; Parsons, P.E.; Matthay, M.A. Pathogenetic significance of biological markers of ventilator-associated lung injury in experimental and clinical studies. Chest 2006, 130, 1906–1914. [Google Scholar] [CrossRef] [PubMed]
- Bolther, M.; Henriksen, J.; Holmberg, M.J.; Jessen, M.K.; Vallentin, M.F.; Hansen, F.B.; Holst, J.M.; Magnussen, A.; Hansen, N.S.; Johannsen, C.M.; et al. Ventilation Strategies During General Anaesthesia for Noncardiac Surgery: A Systematic Review and Meta-Analysis. Anesth. Analg. 2022, 135, 971–985. [Google Scholar] [CrossRef] [PubMed]
- Neto, A.S.; Hemmes, S.N.; Barbas, C.S.; Beiderlinden, M.; Fernandez-Bustamante, A.; Futier, E.; Gajic, O.; El-Tahan, M.R.; Ghamdi, A.A.; PROVE Network Investigators; et al. Association between driving pressure and development of postoperative pulmonary complications in patients undergoing mechanical ventilation for general anaesthesia: A meta-analysis of individual patient data. Lancet Respir. Med. 2016, 4, 272–280. [Google Scholar] [CrossRef] [PubMed]

| Author Study (Year) | Country | Surgery | Population (BMI) Intervention/Control | Intervention Group I:E | Intervention Group Ventilatory Setting | Control Group I:E | Control Group Ventilatory Setting | Position (Pneumo-Pressure) | Primary Endpoint |
|---|---|---|---|---|---|---|---|---|---|
| Zhang WP et al. (2016) [16] | China | Gynecological LPS surgery, duration >1 h | Obese (30 < BMI < 35 kg/m2) 30/30 | 2:1 | VCV TV 8 mL/kg (ABW) PEEP 0 cmH2O RR 12 breath/min FiO2: 100% | 1:2 | VCV TV 8 mL/kg (ABW) PEEP 0 cmH2O RR 12 breath/min FiO2: 100% | 30° Trendelemburg (15 mmHg) | Changes in PaO2 |
| Xu L et al. (2017) [17] | China | Gynecological LPS surgery, duration >2 h | Obese (BMI > 30 kg/m2) 30/30 | 1.5:1 | PCIRV PInsp = PPeak with VCV PEEP 5 cmH2O RR to PetCO2 < 50 mmHg FiO2: 21–89% | 1:2 | VCV TV 8 mL/kg (IBW) PEEP 5 cmH2O RR to PetCO2 < 50 mmHg FiO2: 21–89% | 30° Reverse Trendelemburg (14–15 mmHg) | Changes in VT dynamic CRS, ΔP, PaO2/FiO2, PaCO2, SP-A, TNF-α. |
| Sayed NH et al. (2021) [18] | Egypt | LSG | Obese (35 < BMI < 50 kg/m2) 26/26 | 2:1 | VCV TV 8 mL/kg (IBW) PEEP 0 cmH2O RR 12 breath/min FiO2: 60% | 1:2 | VCV TV 8 mL/kg (IBW) PEEP 0 cmH2O RR 12 breath/min FiO2: 60% | 30° Reverse Trendelemburg (15 mmHg) | Changes in PaO2 |
| Respiratory Mechanics | ||||||||
|---|---|---|---|---|---|---|---|---|
| Variable | MD | 95%CI | p-Value | τ2 | τ | I2 [95%CI] | p = at Q test | QoE |
| PPeak (cmH2O) | −2.23 | [−3.60;−0.86] | 0.001 | 0.821 | 0.906 | 83.8% [33.1%; 96.1%] | 0.012 | ⊕⊕⊕⊖ Moderate § |
| PPlat (cmH2O) | −1.82 | [−2.80;−0.84] | <0.001 | 0.353 | 0.594 | 70.6% [0.0%; 93.4%] | 0.065 | ⊕⊕⊕⊖ Moderate § |
| PMean (cmH2O) | 2.23 | [1.94; 2.51] | <0.001 | 0.0 | 0.0 | 0.0% [0.0%; 0.0%] | 0.613 | ⊕⊕⊕⊕ High |
| CDyn (mL/cmH2O) | 2.03 | [0.81; 3.24] | 0.001 | 0.256 | 0.506 | 21.5% [0.0%; 91.8%] | 0.279 | ⊕⊕⊕⊖ Moderate § |
| Gas exchange | ||||||||
| Variable | MD | 95%CI | p-Value | τ2 | τ | I2 [95%CI] | p = at Q test | QoE |
| PaO2 (mmHg) | 2.49 | [−6.32; 11.31] | 0.579 | 36.391 | 6.032 | 89.9% [62.6%;97.2%] | 0.001 | ⊕⊕⊖⊖ Low §# |
| PaCO2 (mmHg) | −0.09 | [−1.75;1.56] | 0.911 | 0.881 | 0.938 | 61% [0.0%;90.9%] | 0.109 | ⊕⊕⊖⊖ Low §# |
| pH | −0.001 | [−0.02;0.01] | 0.899 | <0.001 | 0.012 | 79.2% [9.8%;95.2%] | 0.028 | ⊕⊕⊖⊖ Low §# |
| Hemodynamics | ||||||||
| Variable | MD | 95%CI | p-value | τ2 | τ | I2 [95%CI] | p = at Q test | QoE |
| PAM (mmHg) | −1.11 | [−2.41; 0.18] | 0.092 | 0.0 | 0.0 | 0.0% [0.0%; 0.0%] | 0.696 | ⊕⊕⊕⊖ Moderate # |
| HR (beats/min) | −0.45 | [−1.60; 0.69] | 0.440 | 0.0 | 0.0 | 0.0% [0.0%; 0.0%] | 0.464 | ⊕⊕⊕⊖ Moderate # |
| Inflammatory cytokines | ||||||||
| Variable | MD | 95%CI | p-Value | τ2 | τ | I2 [95%CI] | p = at Q test | QoE |
| TNF-α (pg/mL) | −1.76 | [−10.74; 7.22] | 0.700 | 37.477 | 6.121 | 88.6% [56.5%; 97%] | 0.003 | ⊕⊕⊖⊖ Low §# |
| Respiratory Mechanics | ||||||||
| Variable | MD | 95%CI | p-Value | τ2 | τ | I2 [95%CI] | p = at Q test | QoE |
| PPeak (cmH2O) | −3.15 | [−3.88; −2.42] | <0.001 | 0.0 | 0.0 | 0.0% [0.0%; 0.0%] | 0.537 | ⊕⊕⊕⊕ High |
| PPlat (cmH2O) | −3.13 | [−3.80; −2.47] | <0.001 | 0.0 | 0.0 | 0.0% [0.0%; 0.0%] | 0.886 | ⊕⊕⊕⊕ High |
| PMean (cmH2O) | 4.17 | [3.11; 5.24] | <0.001 | 0.489 | 0.699 | 80.9% [18.5%; 95.5%] | 0.022 | ⊕⊕⊕⊖ Moderate § |
| CDyn (mL/cmH2O) | 2.64 | [0.95; 4.32] | 0.002 | 1.64 | 1.28 | 74.2% [14%; 92.3%] | 0.020 | ⊕⊕⊕⊖ Moderate § |
| Gas exchange | ||||||||
| Variable | MD | 95%CI | p-Value | τ2 | τ | I2 [95%CI] | p = at Q test | QoE |
| PaO2 (mmHg) | 20.96 | [−1.55; 43.48] | 0.068 | 203.794 | 14.275 | 71.4% [0.0%; 93.6%] | 0.061 | ⊕⊕⊖⊖ Low §# |
| PaCO2 (mmHg) | −0.96 | [−6.15; 4.22] | 0.716 | 12.893 | 3.590 | 91.8% [71.5%; 97.6%] | 0.000 | ⊕⊕⊖⊖ Low §# |
| pH | −0.03 | [−0.05; −0.01] | <0.001 | <0.001 | 0.005 | 12.5% [0.0%; 99.9%] | 0.285 | ⊕⊕⊕⊖ Moderate § |
| Hemodynamics | ||||||||
| Variable | MD | 95%CI | p-Value | τ2 | τ | I2 [95%CI] | p = at Q test | QoE |
| PAM (mmHg) | −2.93 | [−3.95; −1.91] | <0.001 | 0.030 | 0.175 | 1.9% [0.0%; 99.9%] | 0.312 | ⊕⊕⊕⊖ Moderate § |
| HR (beats/min) | −1.08 | [−3.19; 1.01] | 0.310 | 0.747 | 0.864 | 23.9% [0.0%;99.9%] | 0.251 | ⊕⊕⊖⊖ Low §# |
| Inflammatory cytokines | ||||||||
| Variable | MD | 95%CI | p-Value | τ2 | τ | I2 [95%CI] | p= at Q test | QoE |
| TNF-α (pg/mL) | −9.65 | [−17.89;−1.40] | 0.021 | 29.510 | 5.432 | 81.7% [22.4%;95.7%] | 0.019 | ⊕⊕⊕⊖ Moderate § |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carron, M.; Tamburini, E.; Maggiolo, A.; Linassi, F.; Sella, N.; Navalesi, P. Cardiorespiratory Effects of Inverse Ratio Ventilation in Obese Patients During Laparoscopic Surgery: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 2063. https://doi.org/10.3390/jcm14062063
Carron M, Tamburini E, Maggiolo A, Linassi F, Sella N, Navalesi P. Cardiorespiratory Effects of Inverse Ratio Ventilation in Obese Patients During Laparoscopic Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(6):2063. https://doi.org/10.3390/jcm14062063
Chicago/Turabian StyleCarron, Michele, Enrico Tamburini, Alessandra Maggiolo, Federico Linassi, Nicolò Sella, and Paolo Navalesi. 2025. "Cardiorespiratory Effects of Inverse Ratio Ventilation in Obese Patients During Laparoscopic Surgery: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 6: 2063. https://doi.org/10.3390/jcm14062063
APA StyleCarron, M., Tamburini, E., Maggiolo, A., Linassi, F., Sella, N., & Navalesi, P. (2025). Cardiorespiratory Effects of Inverse Ratio Ventilation in Obese Patients During Laparoscopic Surgery: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(6), 2063. https://doi.org/10.3390/jcm14062063







