Does Adherence to Treatment Guidelines from the Ghailane–Gille Classification for Degenerative Spondylolisthesis of the Lumbar Spine Impact Surgical Outcomes? A Match–Mismatch Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Population
- Age > 18 years;
- Surgical treatment for DSLS;
- Complete patient-reported outcomes, including the following:
- ○
- Demographic information: gender, age, Body Mass Index (BMI), smoking status, and comorbidities;
- ○
- Health-Related Quality of Life Scores (HRQOLS): Oswestry Disability Index (ODI), visual analog scales for back pain (BP-VAS), and leg pain (LP-VAS);
- ○
- Radiological parameters: slippage level, segmental lordosis (SL), lumbar lordosis (LL), pelvic incidence (PI), pelvic tilt (PT), PI-LL mismatch, L4-S1 distribution, and sagittal vertical axis (SVA).
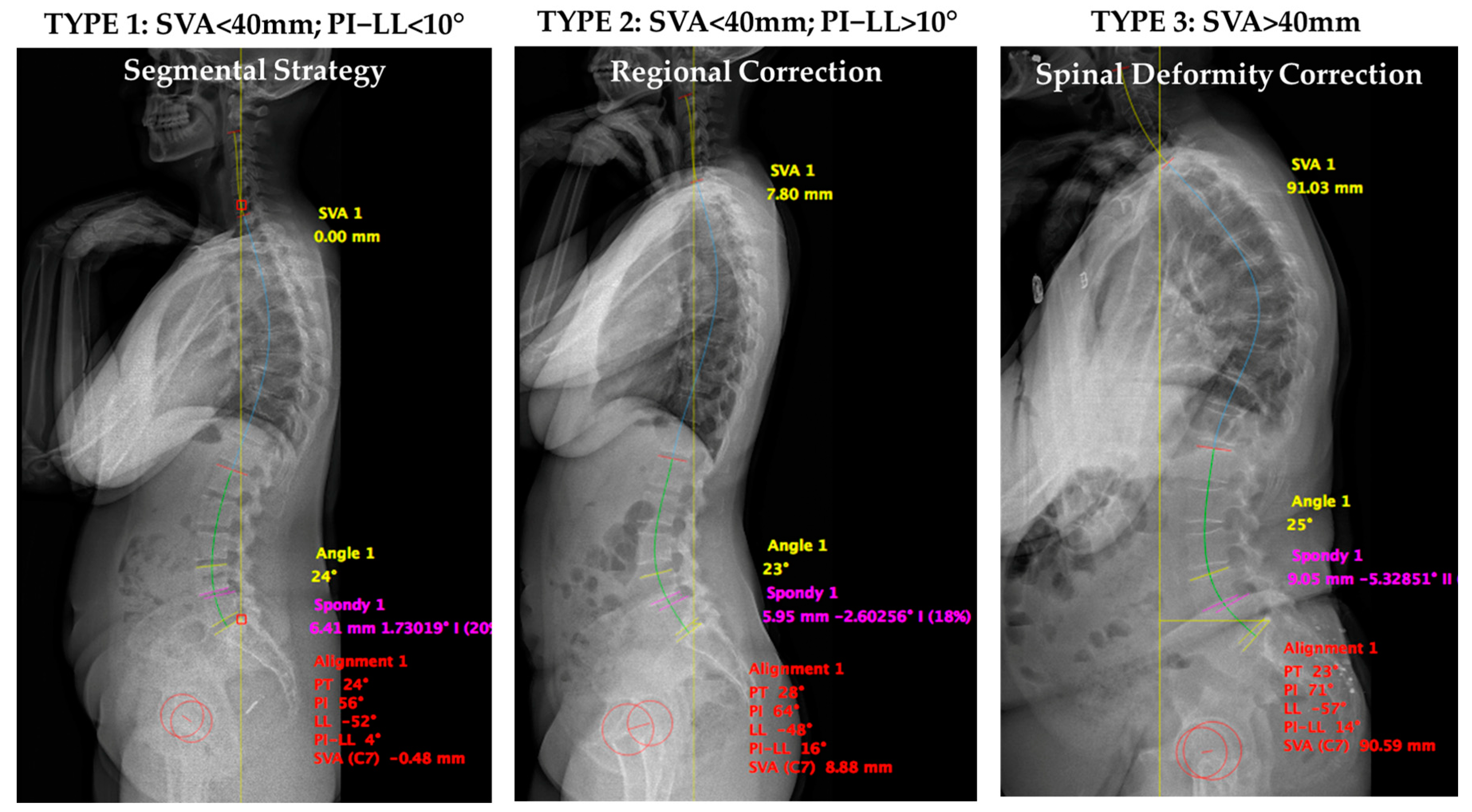
- Type 1 corresponds to a harmonious and aligned spine: SVA < 40 mm, PI-LL < 10°;
- Type 2 corresponds to compensated spinal malalignment: SVA < 40 mm, PI-LL > 10°, with thoracic compensation (Type 2A: PT < 25°) or pelvic compensation (Type 2B: PT > 25°);
- Type 3 corresponds to altered global sagittal alignment: SVA > 40 mm.
2.2. Statistical Analysis
3. Results
3.1. Patient Cohort
3.2. Baseline Characteristics
3.3. Operative Details
3.4. Clinical Outcomes Following MATCH or MISMATCH Distribution
4. Discussion
5. Conclusions
6. Patents
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| DSLS | Degenerative Spondylolisthesis of the Lumbar Spine |
| GG | Ghailane–Gille |
| ODI | Oswestry Disability Index |
| ASA | American Society of Anesthesiologists |
| HRQOL | Health-Related Quality of Life Scores |
| VAS | Visual Analog Scales |
| SL | Segmental Lordosis |
| LL | Lumbar Lordosis |
| PI | Pelvic Incidence |
| PT | Pelvic Tilt |
| SVA | Sagittal Vertical Axis |
References
- Wang, Y.X.J.; Káplár, Z.; Deng, M.; Leung, J.C. Lumbar Degenerative Spondylolisthesis Epidemiology: A Systematic Review with a Focus on Gender-Specific and Age-Specific Prevalence. J. Orthop. Transl. 2017, 11, 39–52. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, S.; Sonne-Holm, S.; Rovsing, H.; Monrad, H.; Gebuhr, P. Degenerative Lumbar Spondylolisthesis: An Epidemiological Perspective: The Copenhagen Osteoarthritis Study. Spine 2007, 32, 120–125. [Google Scholar] [CrossRef]
- Chan, A.K.; Sharma, V.; Robinson, L.C.; Mummaneni, P.V. Summary of Guidelines for the Treatment of Lumbar Spondylolisthesis. Neurosurg. Clin. 2019, 30, 353–364. [Google Scholar] [CrossRef]
- Meyerding, H.W. Spondylolisthesis. Surg. Gynecol. Obs. 1932, 54, 371–377. [Google Scholar]
- Matsunaga, S.; Ijiri, K.; Hayashi, K. Nonsurgically Managed Patients with Degenerative Spondylolisthesis: A 10-to 18-Year Follow-up Study. J. Neurosurg. Spine 2000, 93, 194–198. [Google Scholar] [CrossRef]
- Kepler, C.K.; Hilibrand, A.S.; Sayadipour, A.; Koerner, J.D.; Rihn, J.A.; Radcliff, K.E.; Vaccaro, A.R.; Albert, T.J.; Anderson, D.G. Clinical and Radiographic Degenerative Spondylolisthesis (CARDS) Classification. Spine J. 2015, 15, 1804–1811. [Google Scholar] [CrossRef]
- Simmonds, A.M.; Rampersaud, Y.R.; Dvorak, M.F.; Dea, N.; Melnyk, A.D.; Fisher, C.G. Defining the Inherent Stability of Degenerative Spondylolisthesis: A Systematic Review. J. Neurosurg. Spine 2015, 23, 178–189. [Google Scholar] [CrossRef] [PubMed]
- Kulkarni, A.G.; Kunder, T.S.; Dutta, S. Degenerative Spondylolisthesis: When to Fuse and When Not to? A New Scoring System. Clin. Spine Surg. 2020, 33, E391–E400. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, H.; Endo, K.; Sawaji, Y.; Matsuoka, Y.; Nishimura, H.; Murata, K.; Takamatsu, T.; Suzuki, H.; Aihara, T.; Yamamoto, K. Global Sagittal Spinal Alignment in Patients with Degenerative Low-Grade Lumbar Spondylolisthesis. J. Orthop. Surg. 2019, 27, 2309499019885190. [Google Scholar] [CrossRef]
- Roussouly, P.; Pinheiro-Franco, J.L. Biomechanical Analysis of the Spino-Pelvic Organization and Adaptation in Pathology. Eur. Spine J. 2011, 20, 609–618. [Google Scholar] [CrossRef]
- Kim, M.K.; Lee, S.-H.; Kim, E.-S.; Eoh, W.; Chung, S.-S.; Lee, C.-S. The Impact of Sagittal Balance on Clinical Results after Posterior Interbody Fusion for Patients with Degenerative Spondylolisthesis: A Pilot Study. BMC Musculoskelet. Disord. 2011, 12, 69. [Google Scholar] [CrossRef] [PubMed]
- Radovanovic, I.; Urquhart, J.C.; Ganapathy, V.; Siddiqi, F.; Gurr, K.R.; Bailey, S.I.; Bailey, C.S. Influence of Postoperative Sagittal Balance and Spinopelvic Parameters on the Outcome of Patients Surgically Treated for Degenerative Lumbar Spondylolisthesis. J. Neurosurg. Spine 2017, 26, 448–453. [Google Scholar] [CrossRef]
- Barrey, C.; Jund, J.; Noseda, O.; Roussouly, P. Sagittal Balance of the Pelvis-Spine Complex and Lumbar Degenerative Diseases. A Comparative Study about 85 Cases. Eur. Spine J. 2007, 16, 1459–1467. [Google Scholar] [CrossRef]
- He, S.; Zhang, Y.; Ji, W.; Liu, H.; He, F.; Chen, A.; Yang, H.; Pi, B. Analysis of Spinopelvic Sagittal Balance and Persistent Low Back Pain (PLBP) for Degenerative Spondylolisthesis (DS) Following Posterior Lumbar Interbody Fusion (PLIF). Pain Res. Manag. 2020, 2020, 5971937. [Google Scholar] [CrossRef] [PubMed]
- Karim, S.M.; Fisher, C.; Glennie, A.; Rampersaud, R.; Street, J.; Dvorak, M.; Paquette, S.; Kwon, B.K.; Charest-Morin, R.; Ailon, T. Preoperative Patient-Reported Outcomes Are Not Associated with Sagittal and Spinopelvic Alignment in Degenerative Lumbar Spondylolisthesis. Spine 2022, 47, 1128–1136. [Google Scholar] [CrossRef]
- Wang, D.; Chen, X.; Han, D.; Wang, W.; Kong, C.; Lu, S. Radiographic and Surgery-Related Predictive Factors for Increased Segmental Lumbar Lordosis Following Lumbar Fusion Surgery in Patients with Degenerative Lumbar Spondylolisthesis. Eur. Spine J. 2024, 33, 2813–2823. [Google Scholar] [CrossRef]
- Rangwalla, K.; Filley, A.; El Naga, A.; Gendelberg, D.; Baldwin, A.; Maziad, A.; Arora, A.; Wague, A.; O’Donnell, J.; Chryssikos, T.; et al. Correction: Degenerative Lumbar Spondylolisthesis: Review of Current Classifications and Proposal of a Novel Classification System. Eur. Spine J. 2024, 33, 366. [Google Scholar] [CrossRef] [PubMed]
- Gille, O.; Bouloussa, H.; Mazas, S.; Vergari, C.; Challier, V.; Vital, J.-M.; Coudert, P.; Ghailane, S. A New Classification System for Degenerative Spondylolisthesis of the Lumbar Spine. Eur. Spine J. 2017, 26, 3096–3105. [Google Scholar] [CrossRef]
- Ghailane, S.; Bouloussa, H.; Challier, V.; Vergari, C.; Yoshida, G.; Obeid, I.; Boissière, L.; Vital, J.-M.; Mazas, S.; Coudert, P.; et al. Radiographic Classification for Degenerative Spondylolisthesis of the Lumbar Spine Based on Sagittal Balance: A Reliability Study. Spine Deform. 2018, 6, 358–365. [Google Scholar] [CrossRef]
- Schwab, F.; Patel, A.; Ungar, B.; Farcy, J.-P.; Lafage, V. Adult Spinal Deformity—Postoperative Standing Imbalance: How Much Can You Tolerate? An Overview of Key Parameters in Assessing Alignment and Planning Corrective Surgery. Spine 2010, 35, 2224–2231. [Google Scholar] [CrossRef]
- Liu, H.; Li, S.; Zheng, Z.; Wang, J.; Wang, H.; Li, X. Pelvic Retroversion Is the Key Protective Mechanism of L4–5 Degenerative Spondylolisthesis. Eur. Spine J. 2015, 24, 1204–1211. [Google Scholar] [CrossRef] [PubMed]
- Protopsaltis, T.; Schwab, F.; Bronsard, N.; Smith, J.S.; Klineberg, E.; Mundis, G.; Ryan, D.J.; Hostin, R.; Hart, R.; Burton, D. The T1 Pelvic Angle, a Novel Radiographic Measure of Global Sagittal Deformity, Accounts for Both Spinal Inclination and Pelvic Tilt and Correlates with Health-Related Quality of Life. JBJS 2014, 96, 1631–1640. [Google Scholar] [CrossRef] [PubMed]
- Weinstein, J.N.; Lurie, J.D.; Tosteson, T.D.; Hanscom, B.; Tosteson, A.N.A.; Blood, E.A.; Birkmeyer, N.J.O.; Hilibrand, A.S.; Herkowitz, H.; Cammisa, F.P.; et al. Surgical versus Nonsurgical Treatment for Lumbar Degenerative Spondylolisthesis. N. Engl. J. Med. 2007, 356, 2257–2270. [Google Scholar] [CrossRef]
- Challier, V.; Boissiere, L.; Obeid, I.; Vital, J.-M.; Castelain, J.-E.; Bénard, A.; Ong, N.; Ghailane, S.; Pointillart, V.; Mazas, S.; et al. One-Level Lumbar Degenerative Spondylolisthesis and Posterior Approach: Is Transforaminal Lateral Interbody Fusion Mandatory?: A Randomized Controlled Trial With 2-Year Follow-Up. Spine 2017, 42, 531–539. [Google Scholar] [CrossRef]
- Weinstein, J.; Pearson, A. Fusion in Degenerative Spondylolisthesis Becomes Controversial… Again. BMJ Evid. Based Med. 2016, 21, 148–149. [Google Scholar] [CrossRef] [PubMed]
- Passias, P.G.; Pierce, K.E.; Naessig, S.; Ahmad, W.; Raman, T.; Maglaras, C.; Schwab, F.J.; Buckland, A.J.; Protopsaltis, T.S.; Diebo, B.G. 291. Adjustment of the Global Alignment and Proportion Scores Accounting for Frailty in Adult Spinal Deformity Surgical Patients. Spine J. 2020, 20, S144–S145. [Google Scholar] [CrossRef]
- Ferrero, E.; Ould-Slimane, M.; Gille, O.; Guigui, P.; Society (SFCR), F.S. Sagittal Spinopelvic Alignment in 654 Degenerative Spondylolisthesis. Eur. Spine J. 2015, 24, 1219–1227. [Google Scholar] [CrossRef]
- Asher, A.L.; Kerezoudis, P.; Mummaneni, P.V.; Bisson, E.F.; Glassman, S.D.; Foley, K.T.; Slotkin, J.R.; Potts, E.A.; Shaffrey, M.E.; Shaffrey, C.I. Defining the Minimum Clinically Important Difference for Grade I Degenerative Lumbar Spondylolisthesis: Insights from the Quality Outcomes Database. Neurosurg. Focus 2018, 44, E2. [Google Scholar] [CrossRef]
- Buckland, A.J.; Ramchandran, S.; Day, L.; Bess, S.; Protopsaltis, T.; Passias, P.G.; Diebo, B.G.; Lafage, R.; Lafage, V.; Sure, A.; et al. Radiological Lumbar Stenosis Severity Predicts Worsening Sagittal Malalignment on Full-Body Standing Stereoradiographs. Spine J. 2017, 17, 1601–1610. [Google Scholar] [CrossRef] [PubMed]
- Korovessis, P.; Syrimpeis, V.; Tsekouras, V. Short Lumbosacral Decompression Plus Fixation Does Not Change the Spinopelvic Balance on Patients With Moderate Degenerative Spondylolisthesis and Associated Spinal Stenosis. Spine Deform. 2019, 7, 346–355. [Google Scholar] [CrossRef]
- Ou-Yang, D.; Burger, E.L.; Kleck, C.J. Pre-Operative Planning in Complex Deformities and Use of Patient-Specific UNiDTM Instrumentation. Glob. Spine J. 2022, 12, 40S–44S. [Google Scholar] [CrossRef] [PubMed]
- Haglin, J.M.; Eltorai, A.E.M.; Gil, J.A.; Marcaccio, S.E.; Botero-Hincapie, J.; Daniels, A.H. Patient-Specific Orthopaedic Implants. Orthop. Surg. 2016, 8, 417–424. [Google Scholar] [CrossRef] [PubMed]
- Burnard, J.L.; Parr, W.C.H.; Choy, W.J.; Walsh, W.R.; Mobbs, R.J. 3D-Printed Spine Surgery Implants: A Systematic Review of the Efficacy and Clinical Safety Profile of Patient-Specific and off-the-Shelf Devices. Eur. Spine J. 2020, 29, 1248–1260. [Google Scholar] [CrossRef] [PubMed]
- Reitman, C.A.; Cho, C.H.; Bono, C.M.; Ghogawala, Z.; Glaser, J.; Kauffman, C.; Mazanec, D.; O’Brien, D.; O’Toole, J.; Prather, H.; et al. Management of Degenerative Spondylolisthesis: Development of Appropriate Use Criteria. Spine J. 2021, 21, 1256–1267. [Google Scholar] [CrossRef]
- Mannion, A.F.; Mariaux, F.; Werth, P.M.; Pearson, A.M.; Lurie, J.D.; Fekete, T.F.; Kohler, M.; Haschtmann, D.; Kleinstueck, F.S.; Jeszenszky, D.; et al. Evaluation of “Appropriate Use Criteria” for Surgical Decision-Making in Lumbar Degenerative Spondylolisthesis. A Controlled, Multicentre, Prospective Observational Study. Eur. Spine J. 2024, 33, 1773–1785. [Google Scholar] [CrossRef] [PubMed]
- Baltic, S.; Lyons, K.; Mariaux, F.B.; Werth, P.; Winklhofer, S.; Fekete, T.; Porchet, F.; Kepler, C.K.; McGuire, K.J.; Lurie, J.D. 66. Can Classification Systems and Baseline Radiographic Findings Guide Surgical Technique Selection for Degenerative Spondylolisthesis? Spine J. 2022, 22, S34–S35. [Google Scholar] [CrossRef]
- Little, D.G.; MacDonald, D. The Use of the Percentage Change in Oswestry Disability Index Score as an Outcome Measure in Lumbar Spinal Surgery. Spine 1994, 19, 2139–2143. [Google Scholar] [CrossRef] [PubMed]
- Federici, S.; Bracalenti, M.; Meloni, F.; Luciano, J.V. World Health Organization Disability Assessment Schedule 2.0: An International Systematic Review. Disabil. Rehabil. 2017, 39, 2347–2380. [Google Scholar] [CrossRef]
- Wong, J.J.; DeSouza, A.; Hogg-Johnson, S.; De Groote, W.; Southerst, D.; Belchos, M.; Lemeunier, N.; Alexopulos, S.; Varmazyar, H.; Mior, S.A.; et al. Measurement Properties and Minimal Important Change of the World Health Organization Disability Assessment Schedule 2.0 in Persons with Low Back Pain: A Systematic Review. Arch. Phys. Med. Rehabil. 2023, 104, 287–301. [Google Scholar] [CrossRef]
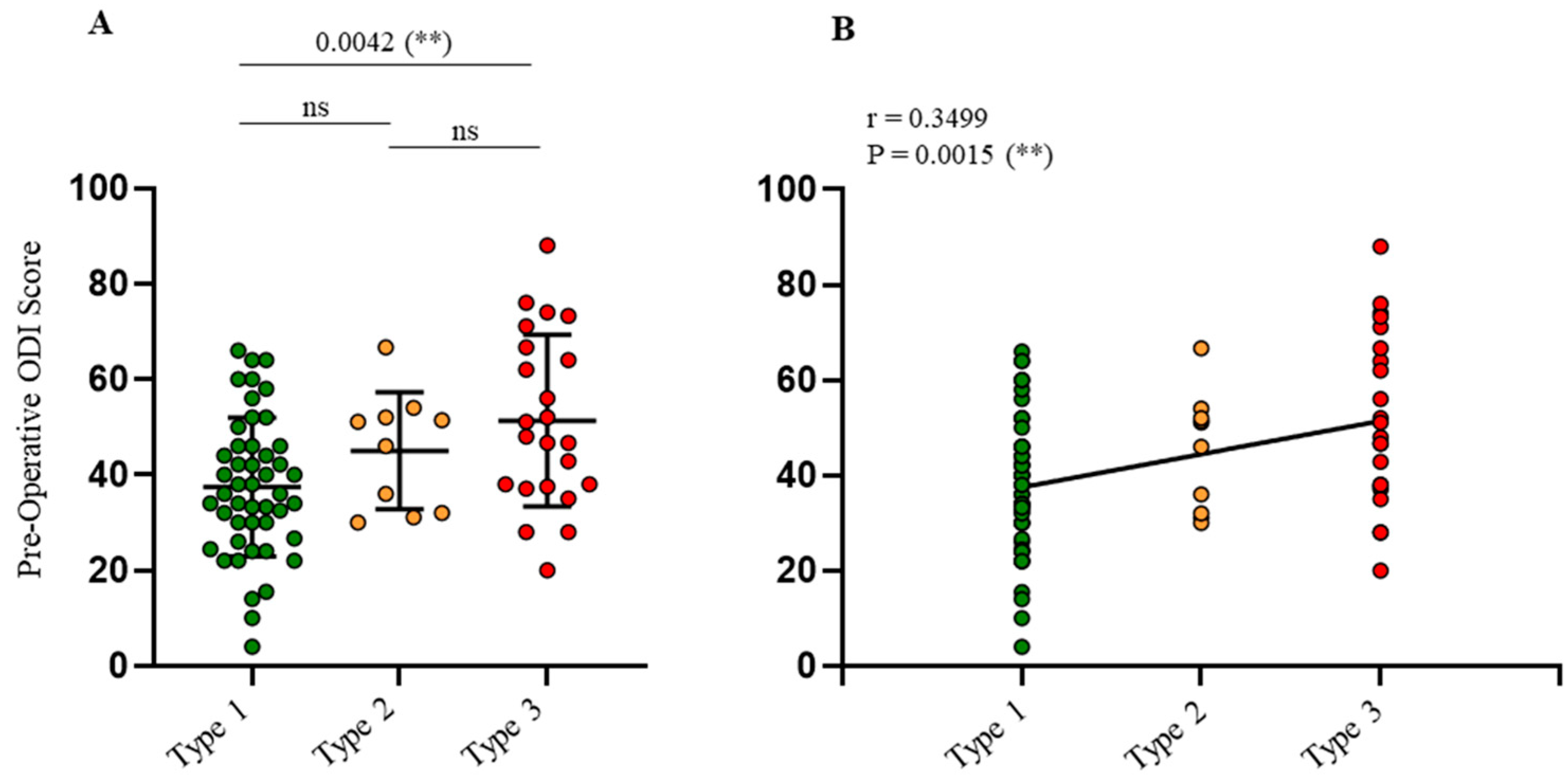
| ALL PATIENTS (N = 80) | TYPE 3 (N = 23) | TYPE 2 (N = 10) | TYPE 1 (N = 47) | TYPE 3 vs. 2 | TYPE 3 vs. 1 | TYPE 2 vs. 1 | |
|---|---|---|---|---|---|---|---|
| Mean (±SD) | p-Value | ||||||
| Gender | |||||||
| Women | 59 (73.75%) | 20 (86.95%) | 7 (70%) | 32 (68.08%) | 0.3364 | 0.1446 | >0.9999 |
| Men | 21 (26.25%) | 3 (13.05%) | 3 (30%) | 15 (31.92%) | |||
| Age (mean, ±SD) | 68.8 ± 9.9 | 72.7 ± 9.2 | 71.7 ± 8.8 | 66.8 ± 9.9 | 0.9931 | 0.0536 | 0.3905 |
| Body Mass Index, kg/m2 | 27.8 ± 4.9 | 27.6 ± 5.1 | 25.5 ± 3.6 | 28.5 ± 5 | 0.6760 | 0.9015 | 0.3147 |
| Smoker (%) | 14 (17.5%) | 4 (17.4%) | 3 (30%) | 7 (14.9%) | 0.6456 | >0.9999 | 0.3568 |
| ODI | 42.4 ± 16.4 | 51.3 ± 17.9 | 45 ± 12.2 | 37.5 ± 16.4 | 0.7236 | 0.0042 (**) | 0.5187 |
| VAS Back (Scale 0–10) | 7.3 ± 1.9 | 8 ± 1.5 | 6.7 ± 2.5 | 7.1 ± 1.9 | 0.3153 | 0.3091 | 0.9300 |
| VAS Legs (Scale 0–10) | 7.2 ± 1.9 | 6.9 ± 2.3 | 7.5 ± 1 | 7.3 ± 1.9 | 0.8556 | 0.8233 | 0.9954 |
| DSLS Diagnosis | |||||||
| L3L4 | 8 (10%) | 3 (13.1%) | 1 (10%) | 4 (8.5%) | |||
| L4L5 | 62 (77.5%) | 13 (56.5%) | 9 (90%) | 40 (85.1%) | |||
| L5S1 | 2 (2.5%) | 1 (4.3%) | 0 | 1 (2.1%) | |||
| Multiple | 8 (10%) | 6 (26.1%) | 0 | 2 (4.3%) | |||
| ALL PATIENTS (N = 80) | TYPE 3 (N = 23) | TYPE 2 (N = 10) | TYPE 1 (N = 47) | TYPE 3 vs. 2 | TYPE 3 vs. 1 | TYPE 2 vs. 1 | |
|---|---|---|---|---|---|---|---|
| Mean (±SD) | p Value | ||||||
| Pre PT (°) | 22.6 ± 7.4 | 27.6 ± 8.8 | 21.8 ± 6.6 | 19.6 ± 6.9 | 0.0392 (*) | <0.0001 (****) | 0.2462 |
| Pre PI (°) | 60.4 ± 11.4 | 66.6 ± 13 | 60.5 ± 12.3 | 57.4 ± 9.2 | 0.1764 | 0.0007 (***) | 0.4522 |
| Pre PI-LL (°) | 6.2 ± 14.1 | 17.3 ± 16.3 | 2.3 ± 10.7 | 1.6 ± 10.2 | 0.0095 (**) | <0.0001 (****) | 0.8484 |
| Pre SL (°) | 54.2 ± 12 | 4.3 ± 3.2 | 5.4 ± 3.6 | 7 ± 4.2 | 0.4344 | 0.0071 (**) | 0.1931 |
| Pre LL (°) | 54.2 ± 13 | 49.3 ± 15.1 | 58.2 ± 14.1 | 55.8 ± 11.1 | 0.2097 | 0.0861 | 0.8565 |
| Pre L4S1 (°) | 30.4 ± 10.3 | 24.3 ± 11.3 | 31.9 ± 9.6 | 33.1 ± 8.6 | 0.1207 | 0.0005 (***) | 0.5519 |
| Pre SVA (mm) | 44.3 ± 44.3 | 86.9 ± 35.3 | 38.4 ± 35.2 | 24.7 ± 35 | 0.0016 (**) | <0.0001 (****) | 0.2461 |
| ALL PATIENTS (N = 80) | TYPE 3 (N = 23) | TYPE 2 (N = 10) | TYPE 1 (N = 47) | TYPE 3 vs. 2 | TYPE 3 vs. 1 | TYPE 2 vs. 1 | |
|---|---|---|---|---|---|---|---|
| Mean (±SD) | p-Value | ||||||
| Operative time (min) | 96.9 ± 45.9 | 108 ± 46.6 | 97.8 ± 63.4 | 91.4 ± 41.3 | 0.9361 | 0.4866 | 0.9779 |
| Blood loss (cc) | 229.6 ± 147.9 | 233.9 ± 175.1 | 185 ± 97.3 | 237 ± 143.4 | 0.8202 | 0.9998 | 0.7461 |
| Hospital stay (days) | 4.4 ± 2.9 | 4.7 ± 3.9 | 4.2 ± 1.5 | 4.4 ± 2.7 | 0.9635 | 0.9590 | 0.9986 |
| Surgical Approach | |||||||
| Anterior | 4 (5%) | 0 | 1 (10%) | 3 (6.4%) | |||
| Posterior | 66 (82.5%) | 20 (87%) | 7 (70%) | 39 (83%) | |||
| Combined | 10 (12.5%) | 3 (13%) | 2 (20%) | 5 (10.6%) | |||
| Intraoperative complications | |||||||
| Incidental durotomy | 2 (2.5%) | 1 (4.3%) | 0 | 1 (2.1%) | |||
| High blood loss | 0 | 0 | 0 | 0 | |||
| Hemodynamic instability | 0 | 0 | 0 | 0 | |||
| Postoperative complications | |||||||
| Within 30 days | |||||||
| Early surgical revision | 1 (1.25%) | 0 | 0 | 1 (2.1%) | |||
| Epidural hematoma | 1 (1.25%) | 0 | 0 | 1 (2.1%) | |||
| Sepsis | 1 (1.25%) | 0 | 0 | 1 (2.1%) | |||
| Screw/cage malposition | 3 (3.75%) | 0 | 0 | 3 (6.4%) | |||
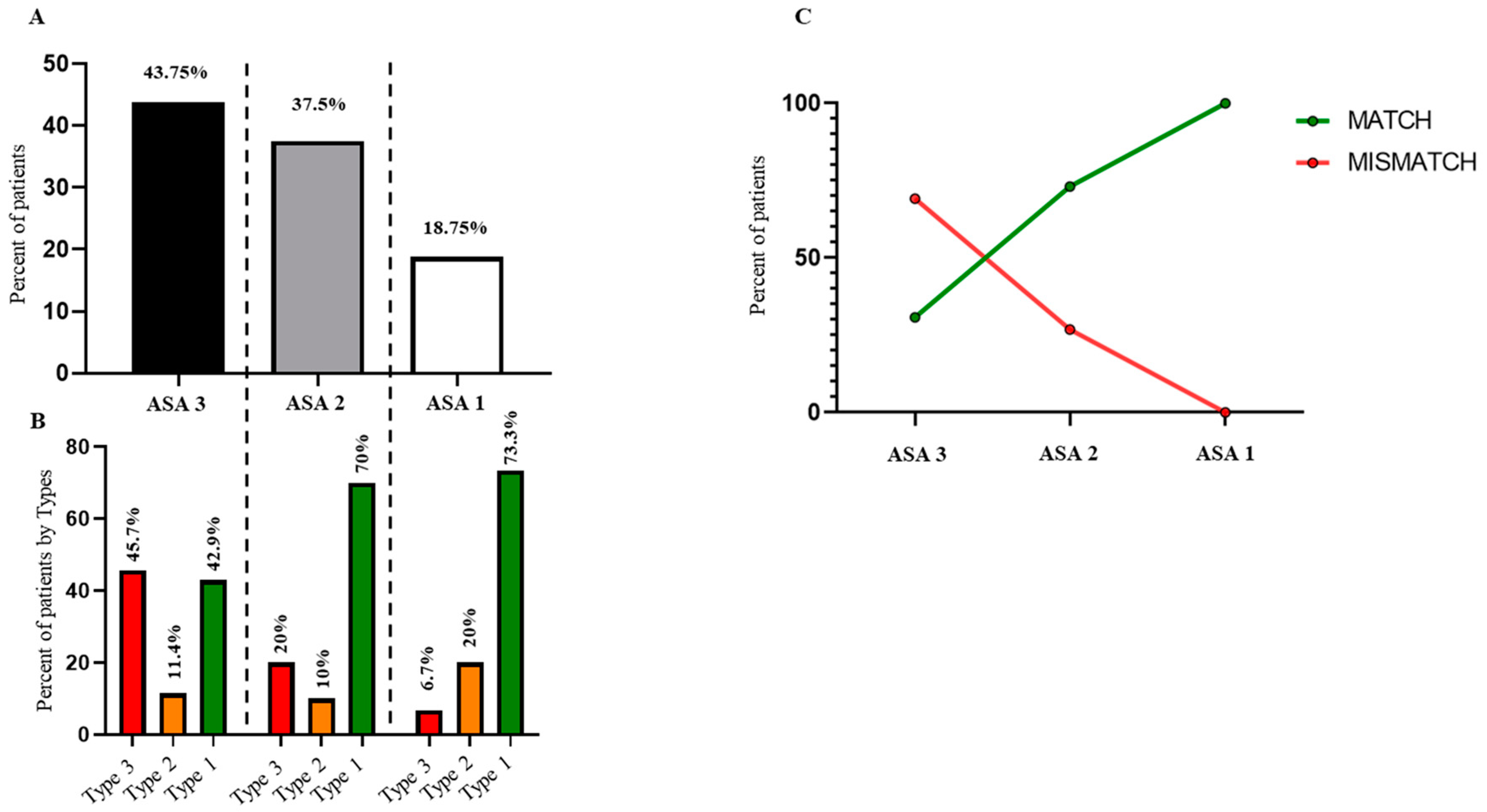
| ASA Score | |||||||
| 1 | 15 (18.75%) | 1 (4.3%) | 3 (30%) | 11 (23.4%) | |||
| 2 | 30 (37.5%) | 6 (26.1%) | 3 (30%) | 21 (44.7%) | |||
| 3 | 35 (43.75%) | 16 (69.6%) | 4 (40%) | 15 (31.9%) | |||
| MATCH (n = 51) | MISMATCH (n = 29) | p-Value | |
|---|---|---|---|
| ODI | 18.9 ± 12.9 | 29.4 ± 18.9 | 0.0121 (*) |
| VAS Back (Scale 0–10) | 4.2 ± 2.9 | 4.8 ± 3 | 0.4663 |
| VAS Legs (Scale 0–10) | 3.6 ± 3.1 | 3.8 ± 3 | 0.9018 |
| Surgery Satisfaction score (%) | 69.7 ± 20.7 | 62.6 ± 20.6 | 0.1611 |
| Satisfaction | |||
| Highly satisfied | 15 (29.4%) | 6 (20.7%) | |
| Satisfied | 23 (45.1%) | 17 (58.6%) | |
| No answer | 3 (5.9%) | 2 (6.9%) | |
| Unsatisfied | 10 (19.6%) | 3 (10.3%) | |
| Very unsatisfied | 0 | 1 (3.5%) | |
| Pain medication | 23 (45.1%) | 14 (48.3%) | |
| Analgesic drug | 15/23 | 10/14 | |
| Non-steroidal anti-inflammatory drugs (NSAIDs) | 3/23 | 2/14 | |
| Both Analgesic + NSAIDs | 2/23 | 1/14 | |
| Opioids | 3/23 | 1/14 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ghailane, S.; Campana, M.; Gille, O.; Bouloussa, H.; Jacquemin, C.; Castelain, J.-E.; Challier, V. Does Adherence to Treatment Guidelines from the Ghailane–Gille Classification for Degenerative Spondylolisthesis of the Lumbar Spine Impact Surgical Outcomes? A Match–Mismatch Study. J. Clin. Med. 2025, 14, 2041. https://doi.org/10.3390/jcm14062041
Ghailane S, Campana M, Gille O, Bouloussa H, Jacquemin C, Castelain J-E, Challier V. Does Adherence to Treatment Guidelines from the Ghailane–Gille Classification for Degenerative Spondylolisthesis of the Lumbar Spine Impact Surgical Outcomes? A Match–Mismatch Study. Journal of Clinical Medicine. 2025; 14(6):2041. https://doi.org/10.3390/jcm14062041
Chicago/Turabian StyleGhailane, Soufiane, Matthieu Campana, Olivier Gille, Houssam Bouloussa, Clément Jacquemin, Jean-Etienne Castelain, and Vincent Challier. 2025. "Does Adherence to Treatment Guidelines from the Ghailane–Gille Classification for Degenerative Spondylolisthesis of the Lumbar Spine Impact Surgical Outcomes? A Match–Mismatch Study" Journal of Clinical Medicine 14, no. 6: 2041. https://doi.org/10.3390/jcm14062041
APA StyleGhailane, S., Campana, M., Gille, O., Bouloussa, H., Jacquemin, C., Castelain, J.-E., & Challier, V. (2025). Does Adherence to Treatment Guidelines from the Ghailane–Gille Classification for Degenerative Spondylolisthesis of the Lumbar Spine Impact Surgical Outcomes? A Match–Mismatch Study. Journal of Clinical Medicine, 14(6), 2041. https://doi.org/10.3390/jcm14062041





