Comparative Outcomes of Treatment Strategies for Traumatic Distal Humerus Physeal Separation in Children: A Systematic Review
Abstract
1. Introduction
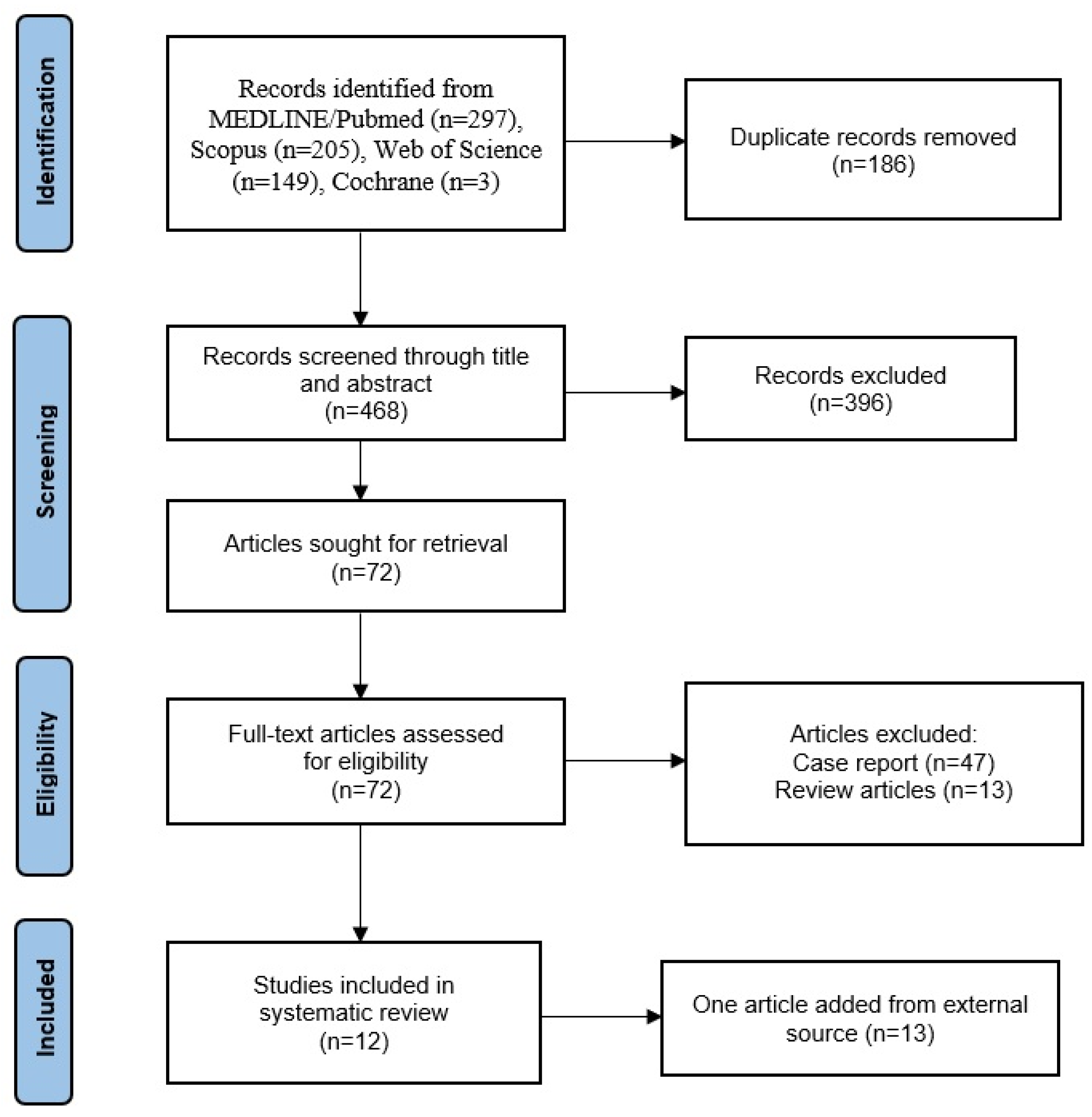
2. Materials and Methods
2.1. Study Type
2.2. Search Strategy
2.3. Inclusion Criteria and Study Selection
2.4. Data Extraction
2.5. Assessment of Risk of Bias
2.6. Data Synthesis and Analysis
3. Results
3.1. Search Results
3.2. Risk of Bias
3.3. Demographic Data
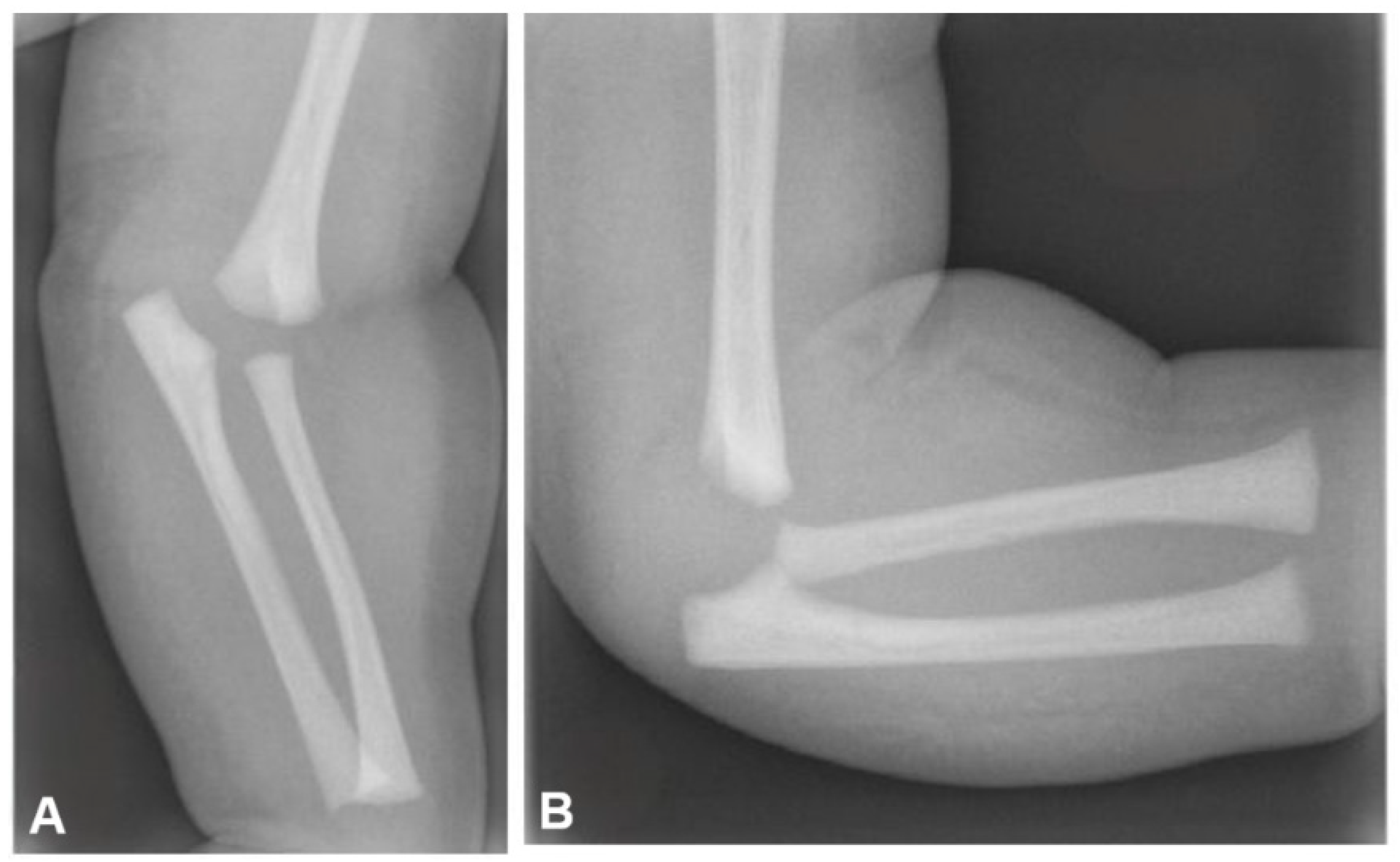
3.4. Diagnosis and Classification
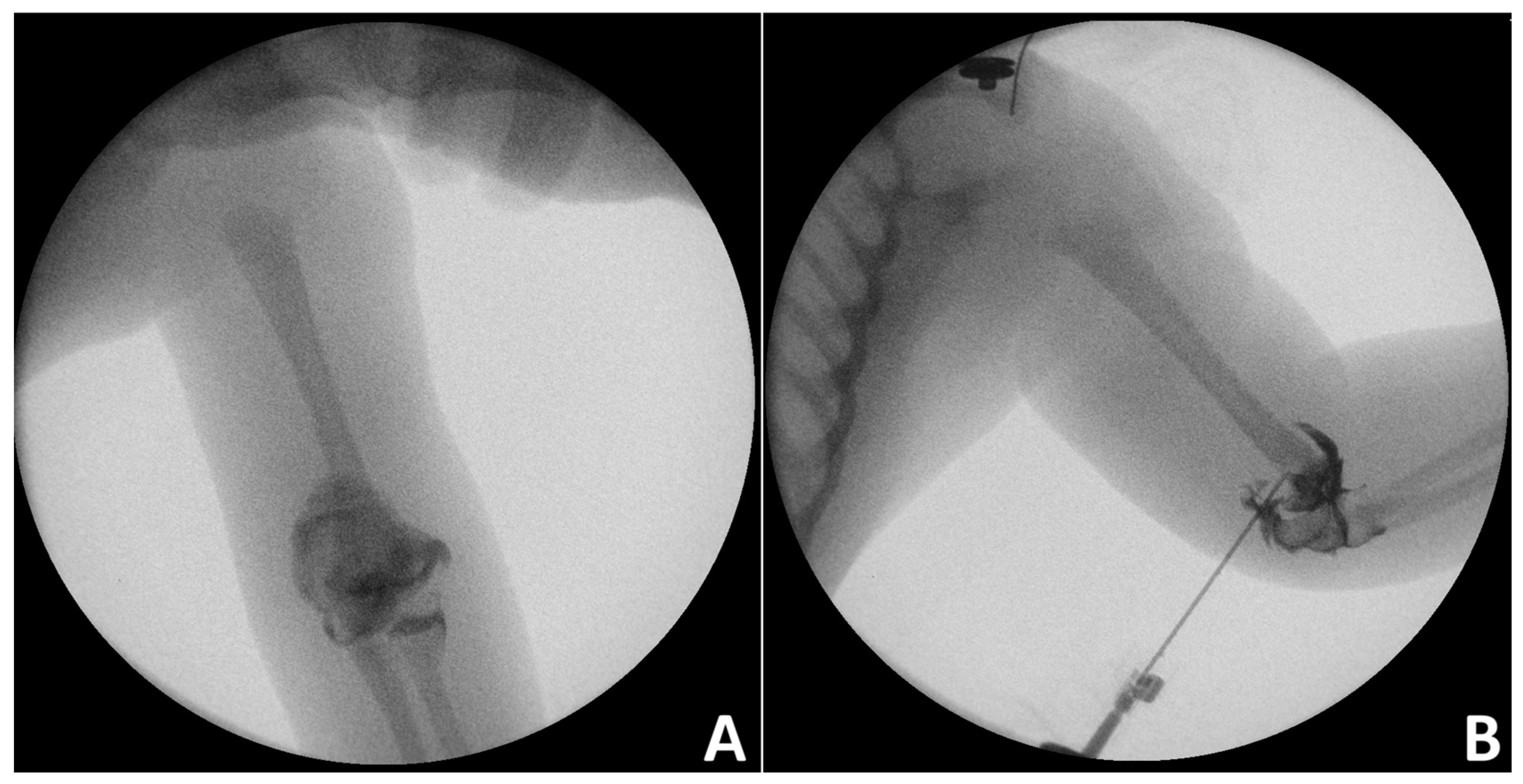
3.5. Treatment and Outcome
3.6. Complications
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| ANT | avascular necrosis of trochlea |
| CR+cast | closed reduction and cast immobilization |
| CRPP | closed reduction and percutaneous pinning |
| DHPS | distal humerus physeal separation |
| f-e | flexion–extension |
| MEPS | Mayo Elbow Performance Score |
| Mod | modified |
| MRI | magnetic resonance imaging |
| n/a | not applicable |
| NoP | number of patients |
| ORPP | open reduction and percutaneous pinning |
| PRISMA | Preferred Reporting Items for Systematic Review and Meta-Analysis |
| ROM | range of motion |
| S-H | Salter-Harris classification |
| U/S | ultrasound |
References
- Smith, R.W. Observations on disjunction of the lower epiphysis of the humerus. Dublin Q. J. Med. Sci. 1850, 9, 63–74. [Google Scholar] [CrossRef]
- Oda, R.; Fujiwara, H.; Ichimaru, K.; Morihara, T.; Ikeda, T.; Kubo, T. Chronic slipping of bilateral distal humeral epiphyses in a gymnastist. J. Pediatr. Orthop. Part B 2015, 24, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Kawamoto, K.; Kim, W.C.; Tsuchida, Y.; Tsuji, Y.; Fujioka, M.; Horii, M.; Mikami, Y.; Tokunaga, D.; Kubo, T. Incidence of physeal injuries in Japanese children. J. Pediatr. Orthop. Part B 2006, 15, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Sabat, D.; Maini, L.; Gautam, V.K. Neonatal separation of distal humeral epiphysis during Caesarean section: A case report. J. Orthop. Surg. 2011, 19, 376–378. [Google Scholar] [CrossRef]
- Kamaci, S.; Danisman, M.; Marangoz, S. Neonatal physeal separation of distal humerus during cesarean section. Am. J. Orthop. 2014, 43, E279–E281. [Google Scholar]
- Abzug, J.M.; Ho, C.A.; Ritzman, T.F.; Brighton, B.K. Transphyseal Fracture of the Distal Humerus. J. Am. Acad. Orthop. Surg. 2016, 24, e39–e44. [Google Scholar] [CrossRef]
- Moucha, C.S.; Mason, D.E. Distal humeral epiphyseal separation. Am. J. Orthop. 2003, 32, 497–500. [Google Scholar]
- Crowe, M.; Byerly, L.; Mehlman, C.T. Transphyseal Distal Humeral Fractures: A 13-Times-Greater Risk of Non-Accidental Trauma Compared with Supracondylar Humeral Fractures in Children Less Than 3 Years of Age. J. Bone Jt. Surg. 2022, 104, 1204–1211. [Google Scholar] [CrossRef]
- Malik, S.; Khopkar, S.R.; Korday, C.S.; Jadhav, S.S.; Bhaskar, A.R. Transphyseal Injury of Distal Humerus: A Commonly Missed Diagnosis in Neonates. J. Clin. Diagn. Res. JCDR 2015, 9, Sd01–Sd02. [Google Scholar] [CrossRef]
- Cheng, J.C.; Wing-Man, K.; Shen, W.Y.; Yurianto, H.; Xia, G.; Lau, J.T.; Cheung, A.Y. A new look at the sequential development of elbow-ossification centers in children. J. Pediatr. Orthop. 1998, 18, 161–167. [Google Scholar] [CrossRef]
- Ratti, C.; Guindani, N.; Riva, G.; Callegari, L.; Grassi, F.A.; Murena, L.J.M.s. Transphyseal elbow fracture in newborn: Review of literature. Musculoskelet. Surg. 2015, 99, 99–105. [Google Scholar] [CrossRef]
- Persiani, P.; Di Domenica, M.; Gurzi, M.; Martini, L.; Lanzone, R.; Villani, C. Adequacy of treatment, bone remodeling, and clinical outcome in pediatric supracondylar humeral fractures. J. Pediatr. Orthop. Part B 2012, 21, 115–120. [Google Scholar] [CrossRef]
- Gamble, J.G.; Vorhies, J.S. Remodeling of Sagittal Plane Malunion After Pediatric Supracondylar Humerus Fractures. J. Pediatr. Orthop. 2020, 40, e903–e909. [Google Scholar] [CrossRef]
- Shrader, M.W. Pediatric supracondylar fractures and pediatric physeal elbow fractures. Orthop. Clin. N. Am. 2008, 39, 163–171. [Google Scholar] [CrossRef]
- Patil, M.N.; Palled, E. Epihyseal Separation of Lower end Humerus in A Neonate-Diagnostic and Management Difficulty. J. Orthop. Case Rep. 2015, 5, 7–9. [Google Scholar]
- Munoz-Ortus, J.M.; Downey-Carmona, F.J.; Tatay-Diaz, A.; Farrington, D.M. Physeal fracture of the distal femur in a newborn: Role of arthrography. Am. J. Orthop. 2013, 42, E14–E15. [Google Scholar]
- Kay, M.; Simpkins, C.; Shipman, P.; Whitewood, C. Diagnosing neonatal transphyseal fractures of the distal humerus. J. Med. Imaging Radiat. Oncol. 2017, 61, 494–499. [Google Scholar] [CrossRef]
- Tan, W.; Wang, F.H.; Yao, J.H.; Wu, W.P.; Li, Y.B.; Ji, Y.L.; Qian, Y.P. Percutaneous fixation of neonatal humeral physeal fracture: A case report and review of the literature. World J. Clin. Cases 2020, 8, 4535–4543. [Google Scholar] [CrossRef]
- Cheong, W.L.; Kamisan, N.; Ismail, I.I. Distal Humerus Physeal Separation: Diagnostic Challenges and Implications. Cureus 2024, 16, e76248. [Google Scholar] [CrossRef]
- Oh, C.W.; Park, B.C.; Ihn, J.C.; Kyung, H.S. Fracture separation of the distal humeral epiphysis in children younger than three years old. J. Pediatr. Orthop. 2000, 20, 173–176. [Google Scholar] [CrossRef]
- Verka, P.S.; Kejariwal, U.; Singh, B. Management of Cubitus Varus Deformity in Children by Closed Dome Osteotomy. J. Clin. Diagn. Res. JCDR 2017, 11, Rc08–Rc12. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Levine, R.H.; Thomas, A.; Nezwek, T.A.; Waseem, M. Salter-Harris Fracture. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2025. [Google Scholar]
- Zhou, W.; Canavese, F.; Zhang, L.; Li, L. Functional outcome of the elbow in toddlers with transphyseal fracture of the distal humerus treated surgically. J. Child. Orthop. 2019, 13, 47–56. [Google Scholar] [CrossRef]
- DeLee, J.C.; Wilkins, K.E.; Rogers, L.F.; Rockwood, C.A. Fracture-separation of the distal humeral epiphysis. J. Bone Jt. Surg. 1980, 62, 46–51. [Google Scholar] [CrossRef]
- Chen, K.; Chen, X.; Su, Y. Open anatomical reduction by anterior transverse mini approach for the treatment of distal humeral epiphyseal separation in young children. J. Pediatr. Orthop. Part B 2022, 31, 449–456. [Google Scholar] [CrossRef]
- Ma, L.-L.; Wang, Y.-Y.; Yang, Z.-H.; Huang, D.; Weng, H.; Zeng, X.-T. Methodological quality (risk of bias) assessment tools for primary and secondary medical studies: What are they and which is better? Mil. Med. Res. 2020, 7, 7. [Google Scholar] [CrossRef]
- Cha, S.M.; Shin, H.D.; Choi, E.S. Long-term outcomes of distal humeral epiphyseal separations treated via closed reduction and pinning under arthrogram. Injury 2020, 51, 207–211. [Google Scholar] [CrossRef]
- Chou, A.C.C.; Wong, H.Y.K.; Kumar, S.; Mahadev, A. Using the Medial and Lateral Humeral Lines as an Adjunct to Intraoperative Elbow Arthrography to Guide Intraoperative Reduction and Fixation of Distal Humerus Physeal Separations Reduces the Incidence of Postoperative Cubitus Varus. J. Pediatr. Orthop. 2018, 38, e262–e266. [Google Scholar] [CrossRef]
- Galeotti, A.; Zanardi, A.; Giacinto, S.D.; Beltrami, G.; Cucca, G.; Lazzeri, S. Transphyseal distal humeral separation in neonates: A case series. Injury 2023, 54, 1601–1607. [Google Scholar] [CrossRef]
- Gigante, C.; Kini, S.G.; Origo, C.; Volpin, A. Transphyseal separation of the distal humerus in newborns. Chin. J. Traumatol. Zhonghua Chuang Shang Za Zhi 2017, 20, 183–186. [Google Scholar] [CrossRef]
- Gilbert, S.R.; Conklin, M.J. Presentation of distal humerus physeal separation. Pediatr. Emerg. Care 2007, 23, 816–819. [Google Scholar] [CrossRef]
- Hariharan, A.R.; Ho, C.; Bauer, A.; Mehlman, C.T.; Sponseller, P.D.; O'Hara, N.; Elliott, M.; Abzug, J.M. Transphyseal Humeral Separations: What Can We Learn? A Retrospective, Multicenter Review of Surgically Treated Patients Over a 25-Year Period. J. Pediatr. Orthop. 2020, 40, e424–e429. [Google Scholar] [CrossRef]
- Jacobsen, S.; Hansson, G.; Nathorst-Westfelt, J. Traumatic separation of the distal epiphysis of the humerus sustained at birth. J. Bone Jt. Surg. Br. Vol. 2009, 91, 797–802. [Google Scholar] [CrossRef]
- Kruse, F.; Dizin, F.; Ilharreborde, B.; Jehanno, P.; Simon, A.L.; Mas, V. Management of the supposed elbow dislocation in newborns. J. Child. Orthop. 2025, 19, 48–55. [Google Scholar] [CrossRef]
- Supakul, N.; Hicks, R.A.; Caltoum, C.B.; Karmazyn, B. Distal humeral epiphyseal separation in young children: An often-missed fracture-radiographic signs and ultrasound confirmatory diagnosis. AJR. Am. J. Roentgenol. 2015, 204, W192–W198. [Google Scholar] [CrossRef]
- Wu, X.; Wu, L.; Canavese, F.; Huang, D.; Chen, S. Closed reduction with percutaneous Kirschner wire fixation for delayed treatment of distal humeral epiphyseal fracture separation. J. Child. Orthop. 2024, 18, 642–651. [Google Scholar] [CrossRef]
- Calogero, V.; Aulisa, A.G.; Careri, S.; Masci, G.; Mastantuoni, G.; Falciglia, F.; Toniolo, R.M. Evaluation of Gartland Classification, Baumann Angle and Anterior Humeral Line in Paediatrics Supracondylar Fractures: An Inter and Intra-Observer Reliability Study. J. Clin. Med. 2023, 13, 167. [Google Scholar] [CrossRef]
- Fette, A.; Mayr, J. Slipped distal humerus epiphysis in tiny infants easily detected and followed-up by ultrasound. Ultraschall Med. 2012, 33, E361–E363. [Google Scholar] [CrossRef]
- Generoso, T.O.; Braga, S.D.R.; Blumetti, F.C.; Pegoraro, M.; Ramalho Júnior, A. Epiphyseal displacement of the distal humerus in a neonate: A case report. Einstein 2024, 22, eRC0868. [Google Scholar] [CrossRef]
- Mane, P.P.; Challawar, N.S.; Shah, H. Late presented case of distal humerus epiphyseal separation in a newborn. BMJ Case Rep. 2016, 2016, bcr2016215296. [Google Scholar] [CrossRef]
- Mathew, D.K.; Gangadharan, S.; Krishnamoorthy, V.; Shanmughanathan, R. Anterior Physeal Separation of Distal Humerus: Report of a Rare Case with Review of Literature. Indian J. Orthop. 2021, 55, 208–212. [Google Scholar] [CrossRef] [PubMed]
- Sherr-Lurie, N.; Bialik, G.M.; Ganel, A.; Schindler, A.; Givon, U. Fractures of the humerus in the neonatal period. Isr. Med. Assoc. J. IMAJ 2011, 13, 363–365. [Google Scholar] [PubMed]
- Villafañe, J.H.; Valdes, K.; Pedersini, P.; Berjano, P. Osteoarthritis: A call for research on central pain mechanism and personalized prevention strategies. Clin. Rheumatol. 2019, 38, 583–584. [Google Scholar] [CrossRef] [PubMed]
- Siddiqui, Y.S.; Abbas, M.B.; Anwer, A.; Abbas, M.; Chowdhry, M.; Khurana, S. Bilateral Distal Humeral Physeal Separation-From Birth Trauma to Family Trauma. J. Orthop. Case Rep. 2023, 13, 88–92. [Google Scholar] [CrossRef]
- Yigitbay, A.; Çelik, M. A Rare Case:Transphyseal Distal Humerus Fracture in a Newborn. Acta Chir. Orthop. Traumatol. Cechoslov. 2024, 91, 120–122. [Google Scholar] [CrossRef]
- Laliotis, N.; Konstantinidis, P.; Chrysanthou, C.; Nikolaides, N.; Chrysopoulou, T. Neonatal Transphyseal Separation of the Distal Humeral Epiphysis: Early Diagnosis and Immediate Treatment with Radiographic Evaluation. J. Orthop. Case Rep. 2023, 13, 61–66. [Google Scholar] [CrossRef]
- de Jager, L.T.; Hoffman, E.B. Fracture-separation of the distal humeral epiphysis. J. Bone Jt. Surg. Br. Vol. 1991, 73, 143–146. [Google Scholar] [CrossRef]
- McIntyre, W.M.; Wiley, J.J.; Charette, R.J. Fracture-separation of the distal humeral epiphysis. Clin. Orthop. Relat. Res. 1984, 188, 98–102. [Google Scholar] [CrossRef]
- Villafañe, J.H.; Valdes, K. Reliability of pinch strength testing in elderly subjects with unilateral thumb carpometacarpal osteoarthritis. J. Phys. Ther. Sci. 2014, 26, 993–995. [Google Scholar] [CrossRef]
- Aldossari, A.M.; Alsagr, G.A.; Alotaibi, R.A.; Shogair, M.M.; Alharbi, H.; Alrashedan, B.S. Birth-related distal humerus epiphyseal separation: Outcome following surgical management. J. Musculoskelet. Surg. Res. 2020, 4, 232. [Google Scholar]
- Navallas, M.; Díaz-Ledo, F.; Ares, J.; Sánchez-Buenavida, A.; López-Vilchez, M.A.; Solano, A.; García García, J.; Maiques, J.M.; Mur-Sierra, A.; Alier, A. Distal humeral epiphysiolysis in the newborn: Utility of sonography and differential diagnosis. Clin. Imaging 2013, 37, 180–184. [Google Scholar] [CrossRef] [PubMed]
- Tudisco, C.; Mancini, F.; De Maio, F.; Ippolito, E. Fracture-separation of the distal humeral epiphysis. Long-term follow-up of five cases. Injury 2006, 37, 843–848. [Google Scholar] [CrossRef] [PubMed]
- Hoffman, B.; Lee, A.; DiGiacomo, D.; Maag, S.; Liu, J.; Skie, M. A systematic review of the operative techniques for treating cubitus varus deformity in children. J. Pediatr. Orthop. Part B 2024, 33, 590–599. [Google Scholar] [CrossRef] [PubMed]
- Abe, M.; Ishizu, T.; Nagaoka, T.; Onomura, T. Epiphyseal separation of the distal end of the humeral epiphysis: A follow-up note. J. Pediatr. Orthop. 1995, 15, 426–434. [Google Scholar] [CrossRef]
| Author | Year | Type of Study | Level of Evidence | Quality of Study | Risk of Bias |
|---|---|---|---|---|---|
| Cha [28] | 2019 | Case series | IV | Good | Low |
| Chen [26] | 2022 | Retrospective cohort study | IV | Good | Low |
| Chou [29] | 2018 | Case series | IV | Good | Low |
| Galeotti [30] | 2023 | Case series | IV | Fair | Moderate |
| Gigante [31] | 2017 | Case series | IV | Fair | Moderate |
| Gilbert [32] | 2007 | Case series | IV | Fair | Moderate |
| Hariharan [33] | 2019 | Case series | IV | Fair | Moderate |
| Jacobsen [34] | 2009 | Case series | IV | Fair | Moderate |
| Kruse [35] | 2024 | Case series | IV | Fair | Moderate |
| Oh [20] | 2000 | Case series | IV | Fair | Moderate |
| Supakul [36] | 2015 | Case series | IV | Fair | Moderate |
| Wu [37] | 2024 | Case series | IV | Good | Low |
| Zhou [24] | 2019 | Case series | IV | Good | Low |
| Author | Year | Number of Patients | Mean Age (Months) (Range) | Gender (Males/ Females) | Side (Right/Left) | Mechanism | Follow-Up (Months) (Range) |
|---|---|---|---|---|---|---|---|
| Cha [28] | 2019 | 12 | 23.5 | 4/8 | 116.2 (84–152) | ||
| Chen [26] | 2022 | 70 | 19.6 | 46/24 | 44 (12–70) | ||
| Chou [29] | 2018 | 13 | 20.4 (7–36) | 5/8 | 13.1 (1–74) | ||
| Galeotti [30] | 2023 | 10 | 0.1 (0–0.3) | 7/3 | 5/5 | 10 birth trauma | 37 (12–120) |
| Gigante [31] | 2017 | 5 | 0.1 (0–0.1) | 5/0 | 4/1 | 5 birth trauma | 30 (12–60) |
| Gilbert [32] | 2007 | 7 | 14.8 (0.5–23) | 5 accidental trauma 1 birth trauma 1 abuse | |||
| Hariharan [33] | 2019 | 79 | 17.9 (0–46) | 50/29 | 49 accidental trauma 21 nonaccidental trauma 9 birth trauma | 2 (0.5–83.4) | |
| Jacobsen [34] | 2009 | 6 | 0.4 (0–1) | 2/4 | 4/2 | 6 birth trauma | 58 (16–120) |
| Kruse [35] | 2024 | 9 | 0.6 (0–3) | 6 birth trauma 1 accidental trauma | 79 (24–201) | ||
| Oh [20] | 2000 | 12 | 18.9 (13–36) | 8/4 | 12 accidental trauma | 23.5 (12–46) | |
| Supakul [36] | 2015 | 16 | 8.6 (0–28) | 10/6 | 11/5 | 6 accidental trauma 6 birth trauma 4 abuse | 5.6 (0.5–14) |
| Wu [37] | 2024 | 11 | 14.3 (0–20) | 8/3 | 5/6 | 43.3 (10–83) | |
| Zhou [24] | 2019 | 16 | 18 (11–37) | 10/6 | 7/9 | 16 accidental trauma | 42.3 (6–98) |
| Author | Number of Patients | Diagnosis | Number of Misdiagnoses | Classification (NoP per Type) |
|---|---|---|---|---|
| Cha [28] | 12 | 12 X-rays | 0 | Mod DeLee (2 A, 7 B, 3 C) S-H (3 I, 9 II) |
| Chen [26] | 70 | 0 | DeLee (16 A, 14 B, 40 C) | |
| Chou [29] | 13 | 13 X-rays | 0 | |
| Galeotti [30] | 10 | 10 X-rays 9 U/S 2 MRI | 0 | |
| Gigante [31] | 5 | 5 X-rays | 1 (elbow dislocation) | |
| Gilbert [32] | 7 | 7 X-rays | 4 (3 other fracture, 1 septic elbow arthritis) | |
| Hariharan [33] | 79 | 79 X-rays 4 U/S 4 MRI | 0 | |
| Jacobsen [34] | 6 | 6 X-rays 3 U/S 1 MRI 1 arthrogram | 3 (1 elbow dislocation, 1 elbow pain, 1 Erb’s palsy) | |
| Kruse [35] | 9 | 4 X-rays 7 U/S 5 MRI | 0 | Gartland (2 I, 1 II, 2 III, 4 IV) |
| Oh [20] | 12 | 0 | S-H (12 II) | |
| Supakul [36] | 16 | 16 X-rays 12 U/S | 9 (4 other fracture, 3 elbow dislocation, 2 elbow pain) | |
| Wu [37] | 11 | 11 X-rays | 3 (not specified) | Mod DeLee (1 A, 7 B, 3 C) |
| Zhou [24] | 16 | 16 X-rays | 0 | Mod DeLee (6 A, 3 B, 7 C) S-H (3 I, 13 II) |
| Author | Number of Patients | Treatment (NoP) | Range of Motion | Radiographic Findings | Functional Outcome | Outcome |
|---|---|---|---|---|---|---|
| Cha [28] | 12 | 12 CRPP | Mean f-e arch: 0.42–127.9° | Bauman’s angle: 71.7° Shaft–condylar angle: 43.3° Humeral length: 24 cm Carrying angle: 10.8° | MEPS: 92.9 | Decreased carrying angle *. No difference * in f-e arch, Bauman’s angle, shaft–condyle angle, humeral length, MEPS. |
| Chen [26] | 70 | 56 ORPP 14 CR+cast | Flynn’s criteria: 45 excellent, 13 good, 2 fair, 10 poor | Better functional outcome after ORPP. No difference in complication rate between two treatment methods. | ||
| Chou [29] | 13 | 13 CRPP | No difference in ROM * | |||
| Galeotti [30] | 10 | 6 CRPP 4 CR+cast | Bauman’s angle: 73.3° (range: 66–79) Shaft–condylar angle: 39.3° (range: 37–43) | Pain score: 6 score 0, 4 score 1 | 1 patient with reduced ROM * after CRPP | |
| Gigante [31] | 5 | 4 CR+cast 1 CRPP | No difference in ROM *. | |||
| Gilbert [32] | 7 | 4 cast 3 CRPP | 2 patients with extension loss (1 after cast, 1 after CRPP) | |||
| Hariharan [33] | 79 | 77 CRPP 2 ORPP | 4 with decreased ROM * | |||
| Jacobsen [34] | 6 | 4 cast 2 CR+cast | 1 with decreased ROM * after cast | |||
| Kruse [35] | 9 | 5 cast 3 ORPP 1 CR+cast | No difference in ROM *. | |||
| Oh [20] | 12 | 6 CRPP 4 CR+cast 2 cast | Carrying angle: 6.1° varus (range: 0–16 varus) | |||
| Supakul [36] | 16 | 11 cast 5 ORPP | No difference in ROM * | |||
| Wu [37] | 11 | 11 CRPP | Mean f-e arch: −1.7–132.7° | Carrying angle: 5.7° (range: 0–12) | Flynn’s criteria: 7 excellent, 4 good | Increased age and injury to surgery interval are correlated with changes * in ROM, carrying angle and Flynn’s rating. |
| Zhou [24] | 16 | 11 CRPP 5 ORPP | Mean f-e arch: 5.9–124.4° | Shaft–condylar angle: 47.1° (range: 25–59) Humeral length: 20.3 cm (range: 15.5–25.8) Carrying angle: 8.8° (range: 2–19) | MEPS: 85.5 (range; 70–95) | Difference * in carrying angle and MEPS score. No difference * in humeral shaft–condylar angle. 15/16 returned to everyday activity and sport. |
| Author | Number of Patients | Treatment (NoP) | Number of Cubitus Varus | Other Complications |
|---|---|---|---|---|
| Cha [28] | 12 | 12 CRPP | 2 (2 CRPP) | 0 |
| Chen [26] | 70 | 56 ORPP 14 CR+cast | 9 (4 ORPP, 5 CR+cast) | 1 ANT (ORPP) |
| Chou [29] | 13 | 13 CRPP | 1 | |
| Galeotti [30] | 10 | 6 CRPP 4 CR+cast | 0 | 0 |
| Gigante [31] | 5 | 4 CR+cast 1 CRPP | 1 (CR+cast) | 0 |
| Gilbert [32] | 7 | 4 cast 3 CRPP | n/a | n/a |
| Hariharan [33] | 79 | 77 CRPP 2 ORPP | 6 cubitus varus or valgus, 1 additional surgery (distal humeral osteotomy for varus deformity) | |
| Jacobsen [34] | 6 | 4 cast 2 CR+cast | 1 (CR+cast) | 0 |
| Kruse [35] | 9 | 5 cast 3 ORPP 1 CR+cast | 1 (CR+cast) | |
| Oh [20] | 12 | 6 CRPP 4 CR+cast 2 cast | 7 (2 CRPP, 3 CR+cast, 2 cast) | 6 ANT (1 CRPP, 3 CR+cast, 2 cast) |
| Supakul [36] | 16 | 11 cast 5 ORPP | 2 | 0 |
| Wu [37] | 11 | 11 CRPP | 2 (2 CRPP) | 0 |
| Zhou [24] | 16 | 11 CRPP 5 ORPP | 8 (6 CRPP, 2 ORPP) | 0 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chalidis, B.; Rigkos, D.; Giouleka, S.; Pitsilos, C. Comparative Outcomes of Treatment Strategies for Traumatic Distal Humerus Physeal Separation in Children: A Systematic Review. J. Clin. Med. 2025, 14, 2037. https://doi.org/10.3390/jcm14062037
Chalidis B, Rigkos D, Giouleka S, Pitsilos C. Comparative Outcomes of Treatment Strategies for Traumatic Distal Humerus Physeal Separation in Children: A Systematic Review. Journal of Clinical Medicine. 2025; 14(6):2037. https://doi.org/10.3390/jcm14062037
Chicago/Turabian StyleChalidis, Byron, Dimitrios Rigkos, Sonia Giouleka, and Charalampos Pitsilos. 2025. "Comparative Outcomes of Treatment Strategies for Traumatic Distal Humerus Physeal Separation in Children: A Systematic Review" Journal of Clinical Medicine 14, no. 6: 2037. https://doi.org/10.3390/jcm14062037
APA StyleChalidis, B., Rigkos, D., Giouleka, S., & Pitsilos, C. (2025). Comparative Outcomes of Treatment Strategies for Traumatic Distal Humerus Physeal Separation in Children: A Systematic Review. Journal of Clinical Medicine, 14(6), 2037. https://doi.org/10.3390/jcm14062037






