Association Between Mild Thrombocytopenia Prior to Cesarean Section and Postpartum Hemorrhage
Abstract
1. Introduction
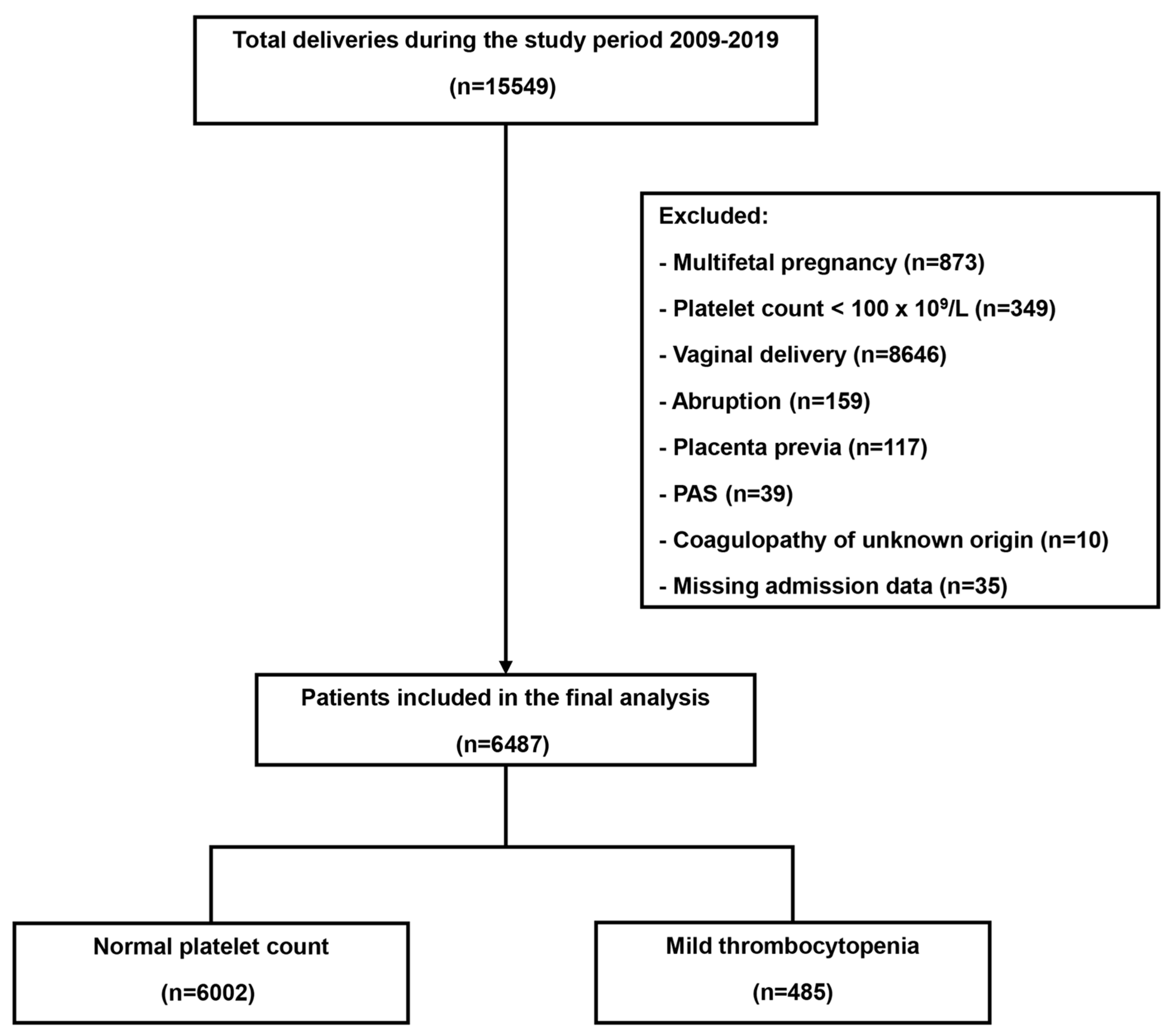
2. Materials and Methods
2.1. Study Design
2.2. Study Population
2.3. Outcomes
2.4. Covariates
2.5. Statistical Analysis
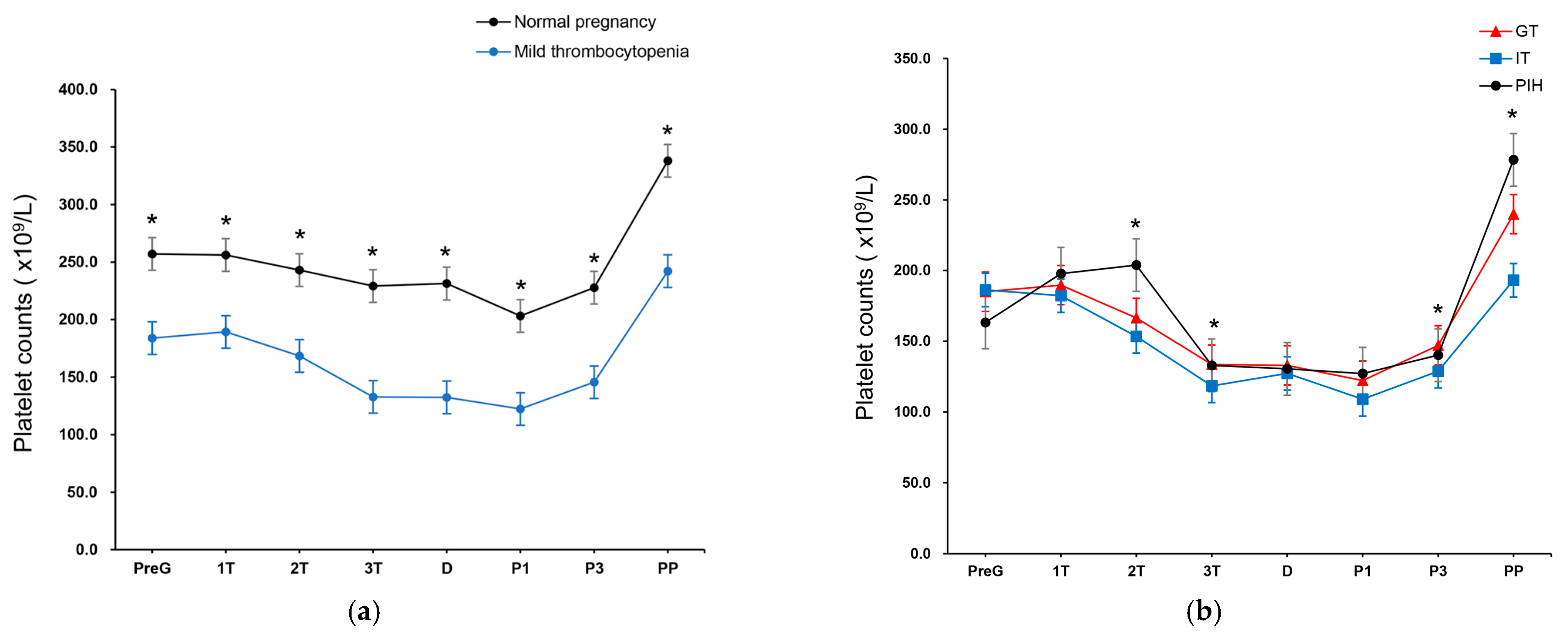
3. Results
4. Discussion
4.1. Main Findings
4.2. Interpretation
4.3. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AA | aplastic anemia |
| aOR | adjusted odds ratio |
| APS | antiphospholipid syndrome |
| BMI | body mass index |
| CI | confidence interval |
| GT | gestational thrombocytopenia |
| Hb | hemoglobin |
| HELLP | hemolysis, elevated liver enzymes, low platelet count |
| ICU | intensive care unit |
| IT | immune-mediated thrombocytopenia |
| ITP | immune thrombocytopenic purpura |
| OR | odds ratio |
| PIH | pregnancy-induced hypertension |
| PP | postpartum period |
| PPH | postpartum hemorrhage |
| PreG | pregestational |
| RBC | red blood cell |
| SLE | systemic lupus erythematosus |
| UAE | uterine artery embolization |
References
- Lee, K.E.; Lee, S.U.; Kang, J.; Lim, H.W.; Park, I.Y.; Kim, M.J. Prognosis of subsequent pregnancy in uterine necrosis after uterine artery embolization. Obstet. Gynecol. Sci. 2024, 67, 335–338. [Google Scholar] [CrossRef] [PubMed]
- Kim, M.J.; Kim, I.J.; Kim, S.; Park, I.Y. Postpartum hemorrhage with uterine artery embolization: The risk of complications of uterine artery embolization. Minim. Invasive Ther. Allied Technol. 2022, 31, 276–283. [Google Scholar] [CrossRef]
- Brown, M.; Hong, M., Jr.; Lindquist, J. Uterine Artery Embolization for Primary Postpartum Hemorrhage. Tech. Vasc. Interv. Radiol. 2021, 24, 100727. [Google Scholar] [CrossRef]
- Lutomski, J.E.; Byrne, B.M.; Devane, D.; Greene, R.A. Increasing trends in atonic postpartum haemorrhage in Ireland: An 11-year population-based cohort study. BJOG Int. J. Obstet. Gynaecol. 2012, 119, 306–314. [Google Scholar] [CrossRef]
- Malabarey, O.; Almog, B.; Brown, R.; Abenhaim, H.A.; Shrim, A. Postpartum hemorrhage in low risk population. J. Perinat. Med. 2011, 39, 495–498. [Google Scholar] [CrossRef] [PubMed]
- Corbetta-Rastelli, C.M.; Friedman, A.M.; Sobhani, N.C.; Arditi, B.; Goffman, D.; Wen, T. Postpartum Hemorrhage Trends and Outcomes in the United States, 2000–2019. Obstet. Gynecol. 2023, 141, 152–161. [Google Scholar] [CrossRef] [PubMed]
- Knight, M.; Callaghan, W.M.; Berg, C.; Alexander, S.; Bouvier-Colle, M.H.; Ford, J.B.; Joseph, K.S.; Lewis, G.; Liston, R.M.; Roberts, C.L.; et al. Trends in postpartum hemorrhage in high resource countries: A review and recommendations from the International Postpartum Hemorrhage Collaborative Group. BMC Pregnancy Childbirth 2009, 9, 55. [Google Scholar] [CrossRef]
- Reale, S.C.; Easter, S.R.; Xu, X.; Bateman, B.T.; Farber, M.K. Trends in Postpartum Hemorrhage in the United States From 2010 to 2014. Anesth. Analg. 2020, 130, e119–e122. [Google Scholar] [CrossRef]
- Al-Zirqi, I.; Vangen, S.; Forsen, L.; Stray-Pedersen, B. Prevalence and risk factors of severe obstetric haemorrhage. BJOG Int. J. Obstet. Gynaecol. 2008, 115, 1265–1272. [Google Scholar] [CrossRef]
- Nagrebetsky, A.; Al-Samkari, H.; Davis, N.M.; Kuter, D.J.; Wiener-Kronish, J.P. Perioperative thrombocytopenia: Evidence, evaluation, and emerging therapies. Br. J. Anaesth. 2019, 122, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Kawakita, T.; Mokhtari, N.; Huang, J.C.; Landy, H.J. Evaluation of Risk-Assessment Tools for Severe Postpartum Hemorrhage in Women Undergoing Cesarean Delivery. Obstet. Gynecol. 2019, 134, 1308–1316. [Google Scholar] [CrossRef] [PubMed]
- Reese, J.A.; Peck, J.D.; Deschamps, D.R.; McIntosh, J.J.; Knudtson, E.J.; Terrell, D.R.; Vesely, S.K.; George, J.N. Platelet Counts during Pregnancy. N. Engl. J. Med. 2018, 379, 32–43. [Google Scholar] [CrossRef] [PubMed]
- Cines, D.B.; Levine, L.D. Thrombocytopenia in pregnancy. Blood 2017, 130, 2271–2277. [Google Scholar] [CrossRef]
- Palta, A.; Dhiman, P. Thrombocytopenia in pregnancy. J. Obstet. Gynaecol. 2016, 36, 146–152. [Google Scholar] [CrossRef] [PubMed]
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 207: Thrombocytopenia in Pregnancy. Obstet. Gynecol. 2019, 133, e181–e193. [Google Scholar] [CrossRef]
- Bergmann, F.; Rath, W. The Differential Diagnosis of Thrombocytopenia in Pregnancy. Dtsch. Ärztebl. Int. 2015, 112, 795–802. [Google Scholar] [CrossRef]
- Fogerty, A.E. Thrombocytopenia in Pregnancy: Mechanisms and Management. Transfus. Med. Rev. 2018, 32, 225–229. [Google Scholar] [CrossRef]
- Rottenstreich, M.; Rotem, R.; Glick, I.; Shen, O.; Grisaru-Granovsky, S.; Sela, H.Y. Mild gestational thrombocytopenia in primiparous women, does it affect risk of early postpartum hemorrhage? A retrospective cohort study. J. Matern. Fetal Neonatal Med. 2022, 35, 8426–8433. [Google Scholar] [CrossRef]
- Isikalan, M.M.; Ozkaya, E.B.; Ozkaya, B.; Ferlibas, E.; Sengul, N.; Acar, A. Does mild thrombocytopenia increase peripartum hemorrhage in elective cesarean deliveries? A retrospective cohort study. Int. J. Gynaecol. Obstet. 2021, 153, 89–94. [Google Scholar] [CrossRef]
- Carlson, L.M.; Dotters-Katz, S.K.; Smid, M.C.; Manuck, T.A. How Low Is Too Low? Postpartum Hemorrhage Risk among Women with Thrombocytopenia. Am. J. Perinatol. 2017, 34, 1135–1141. [Google Scholar]
- Attali, E.; Epstein, D.; Reicher, L.; Lavie, M.; Yogev, Y.; Hiersch, L. Mild thrombocytopenia prior to elective cesarean section is an independent risk factor for blood transfusion. Arch. Gynecol. Obstet. 2021, 304, 627–632. [Google Scholar] [CrossRef]
- Govindappagari, S.; Moyle, K.; Burwick, R.M. Mild Thrombocytopenia and Postpartum Hemorrhage in Nulliparous Women With Term, Singleton, Vertex Deliveries. Obstet. Gynecol. 2020, 135, 1338–1344. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Zhang, Y.; Yu, X.; Huang, Y. Preoperative moderate thrombocytopenia is not associated with increased blood loss for low-risk cesarean section: A retrospective cohort study. BMC Pregnancy Childbirth 2019, 19, 269. [Google Scholar] [CrossRef] [PubMed]
- Lin, Y.H.; Lo, L.M.; Hsieh, C.C.; Chiu, T.H.; Hsieh, T.T.; Hung, T.H. Perinatal outcome in normal pregnant women with incidental thrombocytopenia at delivery. Taiwan J. Obstet. Gynecol. 2013, 52, 347–350. [Google Scholar] [CrossRef] [PubMed]
- DiSciullo, A.; Mokhtari, N.; Landy, H.; Kawakita, T. Effect of mild preoperative thrombocytopenia on postpartum hemorrhage after cesarean deliveries. Am. J. Obstet. Gynecol. MFM 2021, 3, 100368. [Google Scholar] [CrossRef]
- Liu, C.N.; Yu, F.B.; Xu, Y.Z.; Li, J.S.; Guan, Z.H.; Sun, M.N.; Liu, C.A.; He, F.; Chen, D.J. Prevalence and risk factors of severe postpartum hemorrhage: A retrospective cohort study. BMC Pregnancy Childbirth 2021, 21, 332. [Google Scholar] [CrossRef]
- Wang, X.; Xu, Y.; Luo, W.; Feng, H.; Luo, Y.; Wang, Y.; Liao, H. Thrombocytopenia in pregnancy with different diagnoses: Differential clinical features, treatments, and outcomes. Medicine 2017, 96, e7561. [Google Scholar] [CrossRef]
- Fadiloglu, E.; Unal, C.; Tanacan, A.; Portakal, O.; Beksac, M.S. 5 Years’ Experience of a Tertiary Center with Thrombocytopenic Pregnancies: Gestational Thrombocytopenia, Idiopathic Thrombocytopenic Purpura and Hypertensive Disorders of Pregnancy. Geburtshilfe Frauenheilkd. 2020, 80, 76–83. [Google Scholar]
| Normal Platelet Counts (n = 6002) | Mild Thrombocytopenia (n = 485) | p-Value | |
|---|---|---|---|
| Maternal age, years * | 33.7 ± 4.1 | 33.8 ± 4.0 | 0.549 |
| Primiparity, n (%) | 3278 (54.6) | 278 (57.3) | 0.270 |
| Gestational age at delivery, wk | 36.9 ± 3.1 | 37.0 ± 2.9 | 0.701 |
| Neonatal birth weight, kg | 2.9 ± 0.7 | 2.9 ± 0.8 | 0.304 |
| Pregestational BMI (kg/m2) | 21.0 ± 3.7 | 20.6 ± 4.0 | 0.057 |
| Pregestational AA | 5 (0.1) | 4 (0.8) | <0.001 |
| Pregestational ITP | 19 (0.3) | 4 (0.8) | 0.157 |
| Pregestational hypertension, n (%) | 302 (5.0) | 15 (3.1) | 0.073 |
| Pregestational SLE | 51 (0.8) | 15 (3.1) | <0.001 |
| Pregestational APS syndrome | 21 (0.3) | 11 (2.3) | <0.001 |
| Previous uterine operation | 890 (14.8) | 50 (10.3) | 0.008 |
| Emergency cesarean section, n (%) | 2937 (48.9) | 256 (52.9) | 0.103 |
| Pregnancy-induced hypertension, n (%) | 455 (7.6) | 67 (13.8) | <0.001 |
| Gestational diabetes mellitus, n (%) | 371 (6.2) | 29 (6.0) | 0.936 |
| Uterine atony, n (%) | 5 (0.1) | 2 (0.4) | 0.034 |
| Hospital days, d * | 4.3 ± 5.1 | 4.2 ± 3.4 | 0.382 |
| Normal Platelet Counts (n = 6002) | Mild Thrombocytopenia (n = 485) | p-Value | Crude OR (95% CI) | aOR (95% CI) | |
|---|---|---|---|---|---|
| Postpartum hemorrhage, n (%) | 17 (0.3) | 5 (1.0) | 0.020 | 3.67 (1.35, 9.98) | 3.74 (1.36, 10.30) |
| Intrauterine device, n (%) | 68 (1.1) | 9 (1.9) | 0.232 | 1.65 (0.82, 3.33) | 1.02 (0.99, 1.04) |
| Uterine artery embolization, n (%) | 3 (0.0) | 1 (0.2) | 0.183 | 4.13 (0.43, 39.79) | 3.64 (0.38, 35.29) |
| Hysterectomy, n (%) | 5 (0.1) | 0 (0) | 0.524 | 0 | 0 |
| Blood transfusion, n (%) | 194 (3.2) | 35 (7.2) | <0.001 | 2.33 (1.60, 3.38) | 2.28 (1.57, 3.33) |
| ≥4 g/dL drop in hemoglobin level | 92 (1.5) | 22 (4.5) | <0.001 | 3.05 (1.90, 4.90) | 2.99 (1.86, 4.82) |
| Normal Platelet Counts (n = 5487) | Mild Thrombocytopenia (n = 400) | p-Value | Crude OR (95% CI) | aOR (95% CI) | |
|---|---|---|---|---|---|
| Postpartum hemorrhage, n (%) | 13 (0.2) | 2 (0.5) | 0.314 | 2.12 (0.48, 9.41) p = 0.325 | 2.14 (0.48, 9.55) p = 0.321 |
| Intrauterine device, n (%) | 66 (1.2) | 8 (2) | 0.167 | 1.68 (0.80 3.52) p = 0.172 | 1.70 (0.81, 3.58) p = 0.164 |
| Uterine artery embolization, n (%) | 3 (0.1) | 1 (0.2) | 0.148 | 4.58 (0.48, 44.15) p = 0.188 | 4.72 (0.47, 47.00) p = 0.186 |
| Hysterectomy, n (%) | 5 (0.1) | 0 (0) | 0.546 | 0 | 0 |
| Blood transfusion, n (%) | 168 (3.1) | 20 (5) | 0.033 | 1.67 (1.04, 2.68) p = 0.035 | 1.73 (1.07, 2.79) p = 0.025 |
| ≥4 g/dL drop in hemoglobin level | 76 (1.4) | 16 (4) | <0.001 | 2.97 (1.71, 5.13) p < 0.001 | 2.88 (1.66, 5.00) p < 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, K.-E.; Byeon, E.-J.; Kwon, M.-J.; Ko, H.-S.; Shin, J.-E. Association Between Mild Thrombocytopenia Prior to Cesarean Section and Postpartum Hemorrhage. J. Clin. Med. 2025, 14, 2031. https://doi.org/10.3390/jcm14062031
Lee K-E, Byeon E-J, Kwon M-J, Ko H-S, Shin J-E. Association Between Mild Thrombocytopenia Prior to Cesarean Section and Postpartum Hemorrhage. Journal of Clinical Medicine. 2025; 14(6):2031. https://doi.org/10.3390/jcm14062031
Chicago/Turabian StyleLee, Kyung-Eun, Eun-Jeong Byeon, Mi-Ju Kwon, Hyun-Sun Ko, and Jae-Eun Shin. 2025. "Association Between Mild Thrombocytopenia Prior to Cesarean Section and Postpartum Hemorrhage" Journal of Clinical Medicine 14, no. 6: 2031. https://doi.org/10.3390/jcm14062031
APA StyleLee, K.-E., Byeon, E.-J., Kwon, M.-J., Ko, H.-S., & Shin, J.-E. (2025). Association Between Mild Thrombocytopenia Prior to Cesarean Section and Postpartum Hemorrhage. Journal of Clinical Medicine, 14(6), 2031. https://doi.org/10.3390/jcm14062031






