New Tablet-Based Written Examination System for Metamorphopsia Quantification
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
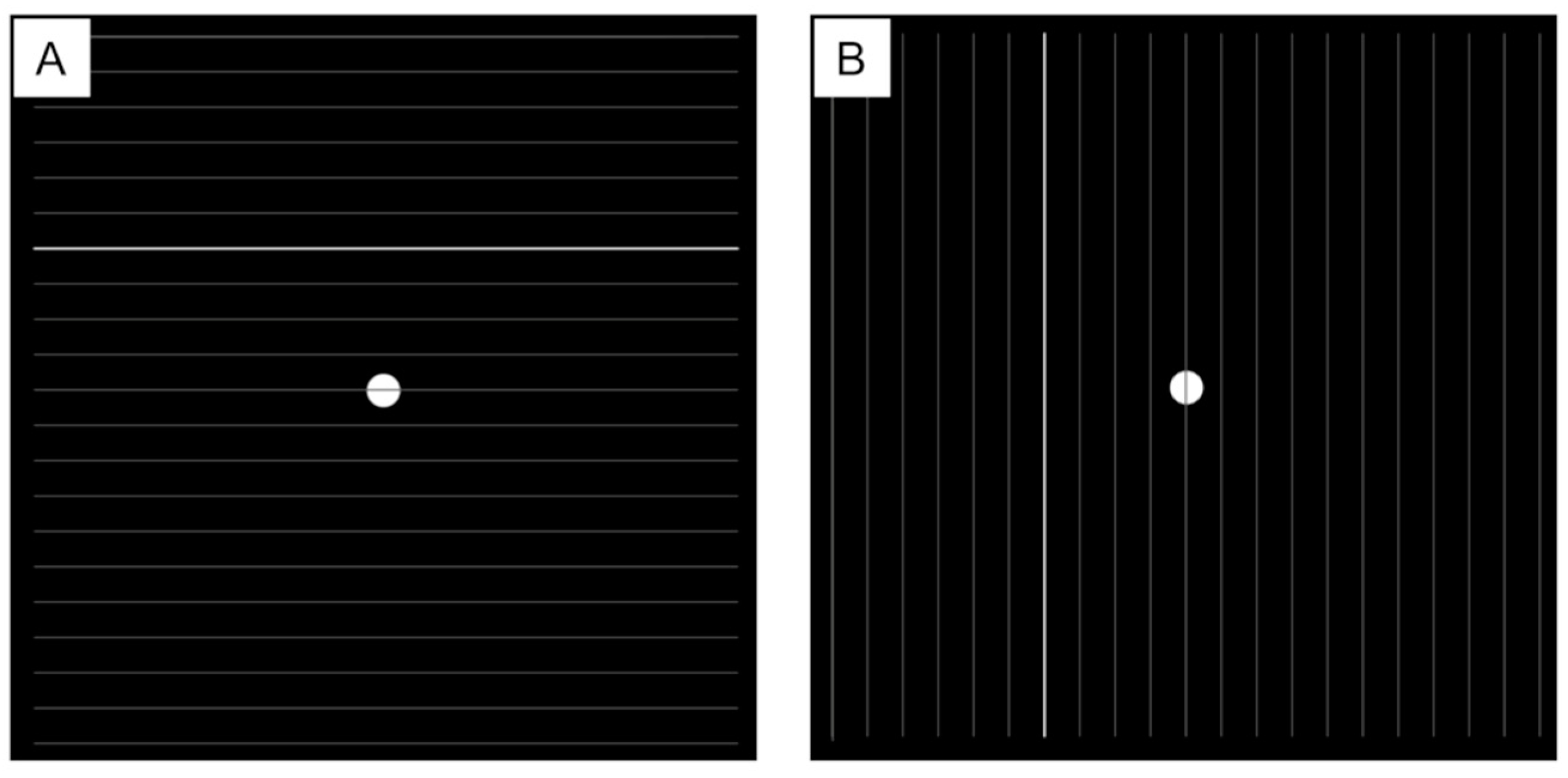
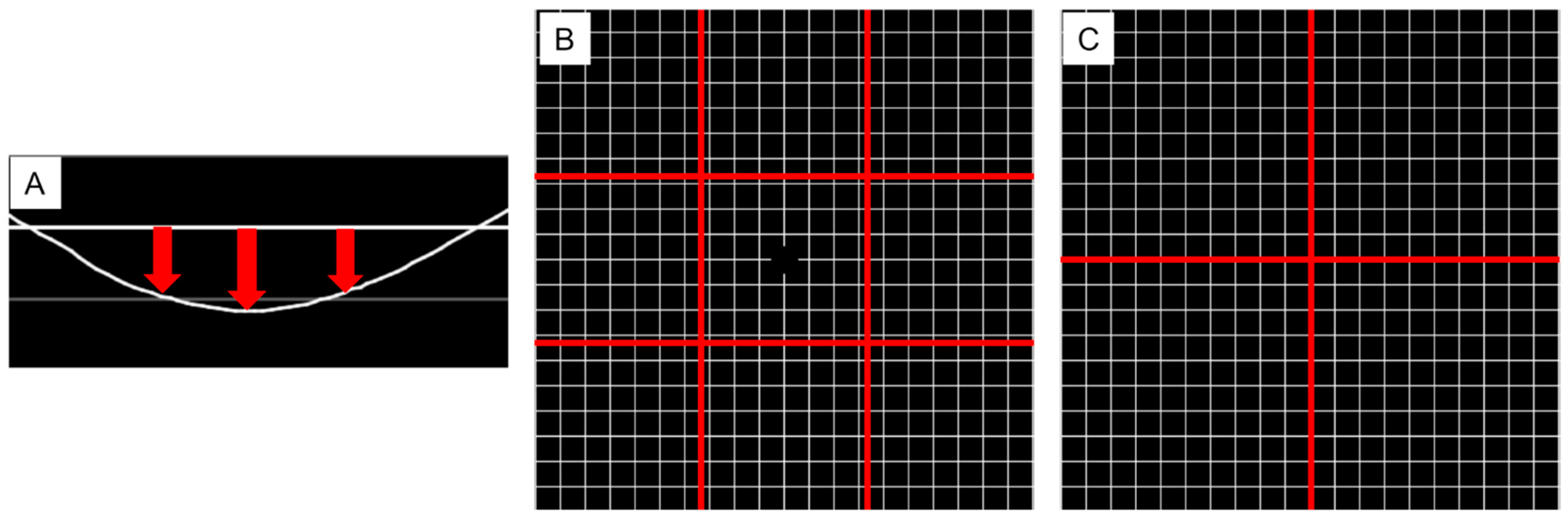
2.2. Procedure
2.3. Statistical Analysis
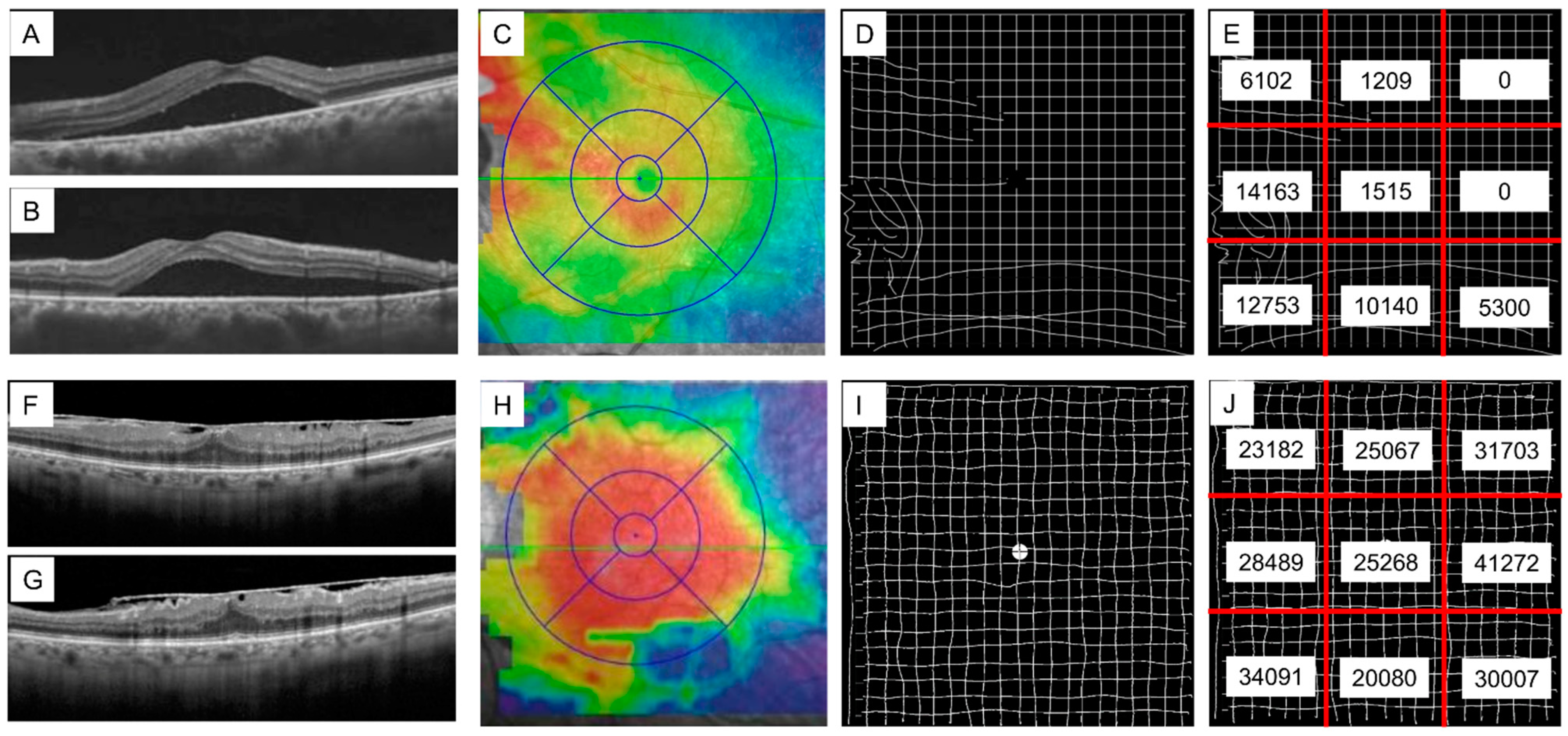
3. Results
3.1. Baseline Characteristics
3.2. IDAM Results
3.3. The Correlation Between M-Charts and IDAM
3.4. Location of Metamorphopsia on IDAM
3.5. Time Course of IDAM Results After Treatment
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Midena, E.; Vujosevic, S. Metamorphopsia: An overlooked visual symptom. Ophthalmic Res. 2015, 55, 26–36. [Google Scholar] [CrossRef] [PubMed]
- Fukuda, S.; Okamoto, F.; Yuasa, M.; Kunikata, T.; Okamoto, Y.; Hiraoka, T.; Oshika, T. Vision-related quality of life and visual function in patients undergoing vitrectomy, gas tamponade and cataract surgery for macular hole. Br. J. Ophthalmol. 2009, 93, 1595–1599. [Google Scholar] [CrossRef] [PubMed]
- Patel, P.J.; Steel, D.H.; Hirneiß, C.; Brazier, J.; Aly, A.; Lescrauwaet, B. Patient-reported prevalence of metamorphopsia and predictors of vision-related quality of life in vitreomacular traction: A prospective, multi-centre study. Eye 2019, 33, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Amsler, M. Earliest symptoms of diseases of the macula. Br. J. Ophthalmol. 1953, 37, 521–537. [Google Scholar] [CrossRef] [PubMed]
- Yannuzzi, L.A. A modified Amsler grid: A self-assessment test for patients with macular disease. Ophthalmology 1982, 89, 157–159. [Google Scholar] [CrossRef] [PubMed]
- Fine, S.L. Early detection of extrafoveal neovascular membranes by daily central field evaluation. Ophthalmology 1985, 92, 603–609. [Google Scholar] [CrossRef] [PubMed]
- Jensen, O.M.; Larsen, M. Objective assessment of photoreceptor displacement and metamorphopsia: A study of macular holes. Arch Ophthalmol. 1998, 116, 1303–1306. [Google Scholar] [CrossRef] [PubMed]
- Shinoda, K.; Ishida, S.; Kawashima, S.; Matsuzaki, T.; Yamada, K.; Katsura, H. A new method for quantification of metamorphopsia in patients with epiretinal membrane. Jpn. J. Ophthalmol. 2000, 44, 424–427. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.Z.; Wilson, E.; Locke, K.G.; Edwards, A.O. Shape discrimination in age-related macular degeneration. Investig. Ophthalmol. Vis. Sci. 2002, 43, 2055–2062. [Google Scholar]
- Bjerager, J.; Schneider, M.; Potapenko, I.; van Dijk, E.H.C.; Faber, C.; Grauslund, J.; Pfau, K.; Huemer, J.; Muttuvelu, D.V.; Rasmussen, M.L.R.; et al. Diagnostic Accuracy of the Amsler Grid Test for Detecting Neovascular Age-Related Macular Degeneration: A Systematic Review and Meta-analysis. JAMA Ophthalmol. 2023, 141, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Loewenstein, A.; Malach, R.; Goldstein, M.; Leibovitch, I.; Barak, A.; Baruch, E.; Alster, Y.; Rafaeli, O.; Avni, I.; Yassur, Y. Replacing the Amsler grid: A new method for monitoring patients with age-related macular degeneration. Ophthalmology 2003, 110, 966–970. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, C.; Arimura, E.; Okuyama, S.; Takada, S.; Hashimoto, S.; Shimomura, Y. Quantification of metamorphopsia in patients with epiretinal membranes. Investig. Ophthalmol. Vis. Sci. 2003, 44, 4012–4016. [Google Scholar] [CrossRef] [PubMed]
- McGowan, G.; Yorston, D.; Strang, N.C.; Manahilov, V. D-CHART: A novel method of measuring metamorphopsia in epiretinal membrane and macular hole. Retina 2016, 36, 703–708. [Google Scholar] [CrossRef] [PubMed]
- Kaiser, P.K.; Wang, Y.Z.; He, Y.G.; Weisberger, A.; Wolf, S.; Smith, C.H. Feasibility of a novel remote daily monitoring system for age-related macular degeneration using mobile handheld devices: Results of a pilot study. Retina 2013, 33, 1863–1870. [Google Scholar] [CrossRef] [PubMed]
- Chew, E.Y.; Clemons, T.E.; Bressler, S.B.; Elman, M.J.; Danis, R.P.; Domalpally, A.; Heier, J.S.; Kim, J.E.; Garfinkel, R.A. Appendix 1 for AREDS2-HOME Study Research Group. Randomized trial of the Foresee Home monitoring device for early detection of neovascular age-related macular degeneration. The HOme Monitoring of the Eye (HOME) study design—HOME Study report number 1. Contemp. Clin. Trials 2014, 37, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Islam, M.; Sansome, S.; Das, R.; Lukic, M.; Chong Teo, K.Y.; Tan, G.; Balaskas, K.; Thomas, P.B.M.; Bachmann, L.M.; Schimel, A.M.; et al. Smartphone-based remote monitoring of vision in macular disease enables early detection of worsening pathology and need for intravitreal therapy. BMJ Health Care Inform. 2021, 28, e100310. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, L.; Müller, S.; Bachmann, L.M.; Claessens, D.; Hatz, K. Prospective Study Comparing Quantitative Self-Monitoring Metamorphopsia Measurement Tools in Myopic Choroidal Neovascularization (mCNV). Clin. Ophthalmol. 2023, 17, 1347–1355. [Google Scholar] [CrossRef] [PubMed]
- Boon, J.; Rojas-Carabali, W.; Asad, Y.; Lim, J.T.Y.; Rajagopalan, R.; Agrawal, R. Evaluation of a digital Amsler grid (PocDoc) for macular disease screening: A comparative analysis with the conventional method. Ophthalmol. Ther. 2024, 13, 1289–1301. [Google Scholar] [CrossRef] [PubMed]
- Imai, A.; Fukuyama, H.; Gomi, F. Comparison of the detection of metamorphopsia between Amsler chart and M-CHARTS. Graefe’s Arch. Clin. Exp. Ophthalmol. 2023, 261, 1503–1504. [Google Scholar] [CrossRef] [PubMed]
| Total | ERM | CSC | |
|---|---|---|---|
| Number of patients | 31 | 11 | 20 |
| Number of eyes | 33 | 11 | 22 |
| Age (years) | 59.0 ± 13.2 | 69.8 ± 8.6 | 53.0 ± 11.5 |
| Gender (male) (%) | 24 (77.4%) | 7 (63.6%) | 17 (85.0%) |
| Eye (right) (%) | 17 (51.5%) | 4 (36.4%) | 12 (54.5%) |
| Log MAR BCVA | 0.142 ± 0.243 | 0.299 ± 0.247 | 0.064 ± 0.204 |
| Equivalent square | −1.5 ± 2.9 | −3.0 ± 3.1 | −0.82 ± 2.6 |
| M-charts (vertical) | 0.54 ± 0.59 | 1.12 ± 0.66 | 0.25 ± 0.25 |
| M-charts (horizontal) | 0.70 ± 0.61 | 0.89 ± 0.65 | 0.60 ± 0.58 |
| Questions | Answers | Total (n = 31) | ERM (n = 11) | CSC (n = 20) |
|---|---|---|---|---|
| Which method describes the metamorphopsia most accurately? | Amsler | 11 (35.1%) | 7 (63.6%) | 4 (20.0%) |
| IDAM | 14 (45.1%) | 2 (18.2%) | 12 (60.0%) | |
| Neutral | 6 (19.4%) | 2 (18.2%) | 4 (20.0%) | |
| Which method most accurately identifies the location of the metamorphopsia? | Amsler | 10 (32,3%) | 7 (63.6%) | 3 (15.0%) |
| IDAM | 14 (45.1%) | 4 (36.4%) | 10 (50.0%) | |
| Neutral | 7 (22.6%) | 0 (0%) | 7 (35.0%) |
| Total | ERM | CSC | |
|---|---|---|---|
| Number of eyes | 30 | 11 | 19 |
| Log MAR BCVA | |||
| Baseline | 0.138 ± 0.253 | 0.299 ± 0.247 | 0.045 ± 0.211 |
| Postoperative | 0.004 ± 0.194 | 0.144 ± 0.221 | −0.076 ± 0.120 |
| Equivalent square | |||
| Baseline | −1.7 ± 3.0 | −3.0 ± 3.1 | −0.88 ± 2.7 |
| Postoperative | −1.4 ± 2.5 | −1.75 ± 1.9 | −1.12 ± 2.8 |
| M-charts (vertical) | |||
| Baseline | 0.57 ± 0.61 | 1.12 ± 0.66 | 0.25 ± 0.23 |
| Postoperative | 0.30 ± 0.42 | 0.56 ± 0.51 | 0.15 ± 0.51 |
| M-charts (horizontal) | |||
| Baseline | 0.75 ± 0.61 | 0.89 ± 0.65 | 0.67 ± 0.59 |
| Postoperative | 0.43 ± 0.55 | 0.47 ± 0.66 | 0.40 ± 0.49 |
| CFT (µm) | |||
| Baseline | 353 ± 146 | 425 ± 167 | 313 ± 120 |
| Postoperative | 242 ± 107 | 350 ± 95 | 181 ± 49 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fukuyama, H.; Mikami, K.; Okita, Y.; Tahara, E.; Yamamoto, Y.; Imura, M.; Gomi, F. New Tablet-Based Written Examination System for Metamorphopsia Quantification. J. Clin. Med. 2025, 14, 1831. https://doi.org/10.3390/jcm14061831
Fukuyama H, Mikami K, Okita Y, Tahara E, Yamamoto Y, Imura M, Gomi F. New Tablet-Based Written Examination System for Metamorphopsia Quantification. Journal of Clinical Medicine. 2025; 14(6):1831. https://doi.org/10.3390/jcm14061831
Chicago/Turabian StyleFukuyama, Hisashi, Kazuma Mikami, Yoichi Okita, Eri Tahara, Yuki Yamamoto, Masataka Imura, and Fumi Gomi. 2025. "New Tablet-Based Written Examination System for Metamorphopsia Quantification" Journal of Clinical Medicine 14, no. 6: 1831. https://doi.org/10.3390/jcm14061831
APA StyleFukuyama, H., Mikami, K., Okita, Y., Tahara, E., Yamamoto, Y., Imura, M., & Gomi, F. (2025). New Tablet-Based Written Examination System for Metamorphopsia Quantification. Journal of Clinical Medicine, 14(6), 1831. https://doi.org/10.3390/jcm14061831







