Aortopexy for Tracheomalacia in Children: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Data Collection
3. Results
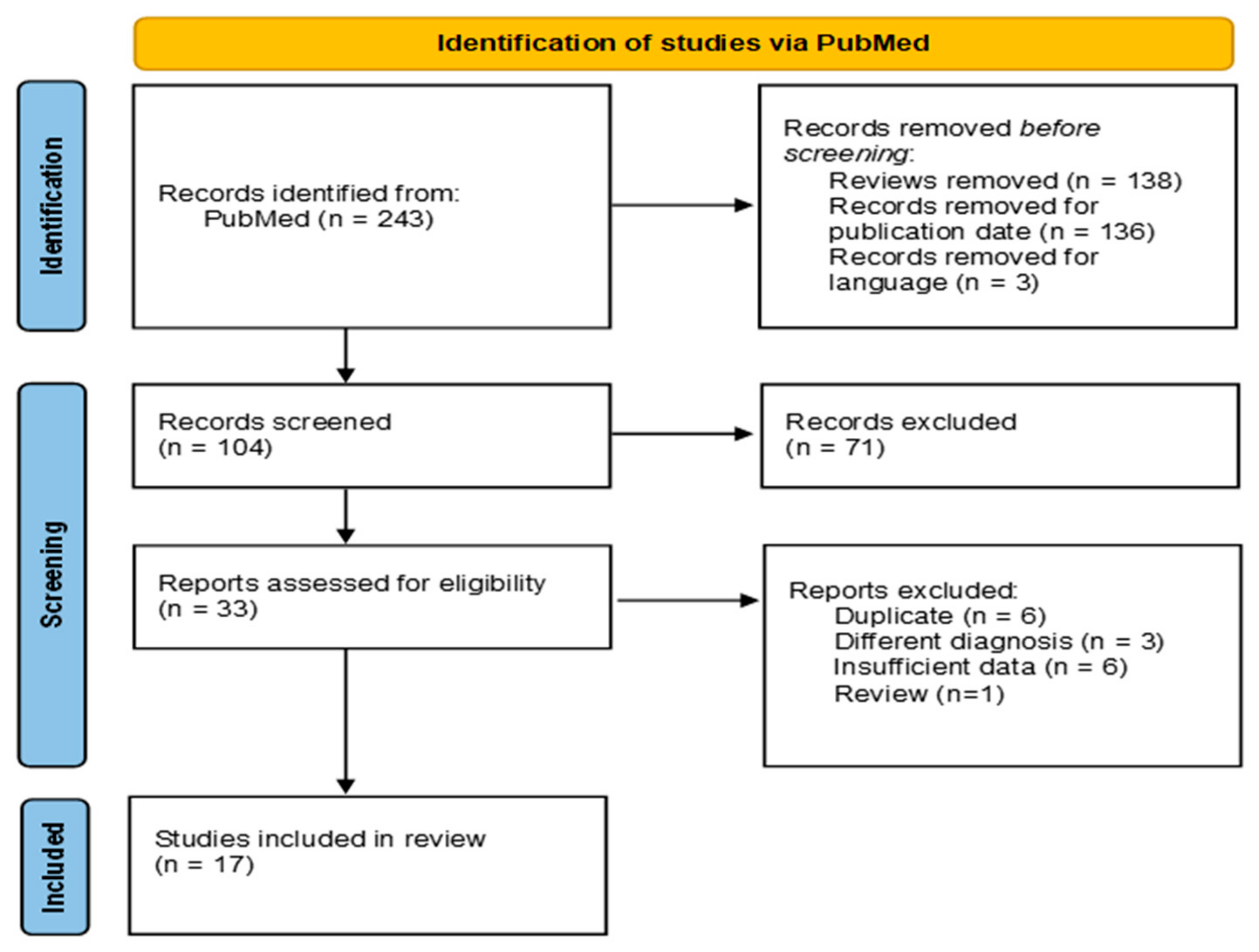
3.1. Literature Search Results
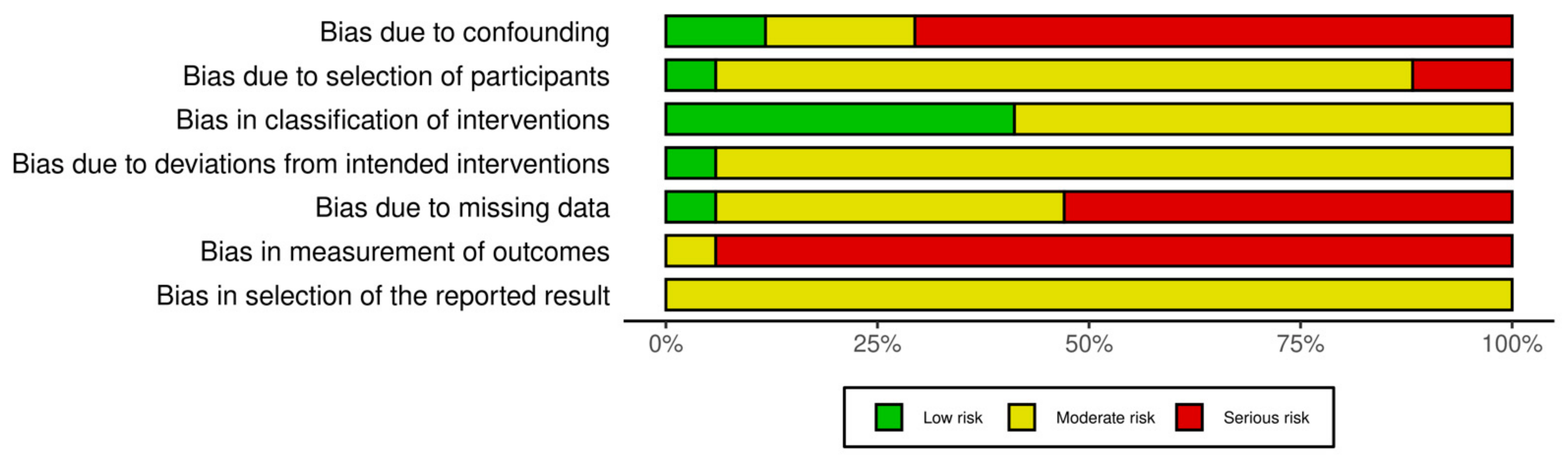
- Confounding Bias—The lack of randomization and retrospective designs limited control over patient characteristics and surgical evolution. Only three studies applied statistical adjustments;
- Classification Bias—Surgical approaches were well defined, but differences in surgeon experience and adjunctive procedures may have influenced outcomes;
- Selection Bias—Inclusion criteria varied, and long study periods introduced time-related selection bias. Some studies excluded lost-to-follow-up patients without adequate discussion of their characteristics, potentially introducing bias;
- Deviation from Intended Intervention Bias—Reporting on deviations (e.g., need for tracheostomy, revision surgeries) was inconsistent, and post-operative management varied across institutions;
- Missing Data Bias—Missing data was a significant concern, particularly in long-term follow-up assessments. While a few studies reported comprehensive follow-up data, many had high attrition rates, with follow-up periods ranging from as little as 6 weeks to over 14 years;
- Outcome Measurement Bias—Assessments relied on subjective symptom resolution, often without standardized scoring or objective follow-up (e.g., bronchoscopy). Parent-reported outcomes may introduce recall bias;
- Reporting Bias—Selective reporting favored positive findings, and few studies had pre-registered analysis plans, increasing the risk of post hoc analyses
3.2. Patients’ Epidemiology
3.3. Symptoms
3.4. Surgical Approach
3.5. Aortopexy Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Gross, R.E. Compression of the trachea by an anomalous innominate artery: An operation for its relief. Am. J. Dis. Child. 1948, 1911, 570–574. [Google Scholar] [CrossRef] [PubMed]
- Fraga, J.C.; Jennings, R.W.; Kim, P.C.W. Pediatric tracheomalacia. Semin. Pediatr. Surg. 2016, 25, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Wallis, C.; Alexopoulou, E.; Antón-Pacheco, J.L.; Bhatt, J.M.; Bush, A.; Chang, A.B.; Charatsi, A.-M.; Coleman, C.; Depiazzi, J.; Douros, K.; et al. ERS statement on tracheomalacia and bronchomalacia in children. Eur. Respir. J. 2019, 54, 1900382. [Google Scholar] [CrossRef] [PubMed]
- Muthialu, N.; Ramaswamy, M.; Beeman, A.; Yeh, Y.T. Management of Tracheal Diseases in Children. Front. Pediatr. 2020, 8, 297. [Google Scholar] [CrossRef] [PubMed]
- Hysinger, E.B.; Hart, C.K.; Burg, G.; De Alarcon, A.; Benscoter, D. Differences in Flexible and Rigid Bronchoscopy for Assessment of Tracheomalacia. Laryngoscope 2021, 131, 201–204. [Google Scholar] [CrossRef]
- Snijders, D.; Barbato, A. An Update on Diagnosis of Tracheomalacia in Children. Eur. J. Pediatr. Surg. Off. J. 2015, 25, 333–335. [Google Scholar] [CrossRef]
- Torre, M.; Carlucci, M.; Speggiorin, S.; Elliott, M.J. Aortopexy for the treatment of tracheomalacia in children: Review of the literature. Ital. J. Pediatr. 2012, 38, 62. [Google Scholar] [CrossRef]
- Wong, Z.H.; Hewitt, R.; Cross, K.; Butler, C.; Yeh, Y.-T.; Ramaswamy, M.; Blackburn, S.; Giuliani, S.; Muthialu, N.; De Coppi, P. Thoracoscopic aortopexy for symptomatic tracheobronchomalacia. J. Pediatr. Surg. 2020, 55, 229–233. [Google Scholar] [CrossRef]
- Jennings, R.W.; Hamilton, T.E.; Smithers, C.J.; Ngerncham, M.; Feins, N.; Foker, J.E. Surgical approaches to aortopexy for severe tracheomalacia. J. Pediatr. Surg. 2014, 49, 66–71. [Google Scholar] [CrossRef]
- Van Der Zee, D.C.; Straver, M. Thoracoscopic Aortopexy for Tracheomalacia. World J. Surg. 2015, 39, 158–164. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis) An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Syn. Meth. 2020, 12, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.Y. Statistical notes for clinical researchers: Chi-squared test and Fisher’s exact test. Restor. Dent. Endod. 2017, 42, 152–155. [Google Scholar] [CrossRef]
- Montgomery, J.; Sau, C.; Clement, W.; Danton, M.; Davis, C.; Haddock, G.; McLean, A.; Kubba, H.; Montgomery, J. Treatment of Tracheomalacia with Aortopexy in Children in Glasgow. Eur. J. Pediatr. Surg. 2013, 24, 389–393. [Google Scholar] [CrossRef]
- Kay-Rivest, E.; Baird, R.; Laberge, J.M.; Puligandla, P.S. Evaluation of aortopexy in the management of severe tracheomalacia after esophageal atresia repair: Aortopexy in severe tracheomalacia. Dis. Esophagus 2015, 28, 234–239. [Google Scholar] [CrossRef]
- Gruszka, A.; Sachweh, J.S.; Schnoering, H.; Tenbrock, K.; Muehler, E.G.; Laschat, M.; Vazquez-Jimenez, J.F. Aortopexy offers surgical options for a variety of pathological tracheal conditions in paediatric patients. Interact. Cardiovasc. Thorac. Surg. 2017, 25, 589–594. [Google Scholar] [CrossRef]
- Haveliwala, Z.; Yardley, I. Aortopexy for tracheomalacia via a suprasternal incision. J. Pediatr. Surg. 2019, 54, 247–250. [Google Scholar] [CrossRef]
- Williams, S.P.; Losty, P.D.; Dhannapuneni, R.; Lotto, A.; Guerrero, R.; Donne, A.J. Aortopexy for the management of paediatric tracheomalacia—The Alder Hey experience. J. Laryngol. Otol. 2020, 134, 174–177. [Google Scholar] [CrossRef]
- Dolmaci, O.B.; Fockens, M.M.; Oomen, M.W.; Van Woensel, J.B.; Hoekstra, C.E.L.; Koolbergen, D.R. A modified surgical technique for aortopexy in tracheobronchomalacia. Interact. Cardiovasc. Thorac. Surg. 2021, 33, 462–468. [Google Scholar] [CrossRef]
- Isik, O.; Akyuz, M.; Ozcifci, G.; Durak, F.; Mercan, I.; Anıl, A.B. Role of aortopexy in the treatment of aberrant innominate artery in children. Pediatr. Surg. Int. 2022, 39, 47. [Google Scholar] [CrossRef]
- Williamson, A.; Young, D.; Clement, W.A. Paediatric tracheobronchomalacia: Incidence, patient characteristics, and predictors of surgical intervention. J. Pediatr. Surg. 2022, 57, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, R.D.; Lapidus-Krol, E.; Honjo, O.; Propst, E.J.; Wolter, N.E.; Campisi, P.; Chiu, P. Surgical management of acute life-threatening events affecting esophageal atresia and/or tracheoesophageal fistula patients. J. Pediatr. Surg. 2023, 58, 803–809. [Google Scholar] [CrossRef]
- Poolthananant, N.; Thapmongkol, S.; Srisingh, K.; Phuaksaman, C.; Sripariwuth, A. Tracheopexy and aortopexy for circumflex aortic arch on a small infant. Asian Cardiovasc. Thorac. Ann. 2023, 31, 263–265. [Google Scholar] [CrossRef]
- Barreto, C.G.; Rombaldi, M.C.; Holanda, F.C.D.; Lucena, I.S.; Isolan, P.M.S.; Jennings, R.; Fraga, J.C. Surgical treatment for severe pediatric tracheobronchomalacia: The 20-year experience of a single center. J. Pediatr. 2024, 100, 250–255. [Google Scholar] [CrossRef]
- Mukharesh, L.; Krone, K.A.; Hamilton, T.E.; Shieh, H.F.; Smithers, C.J.; Winthrop, Z.A.; Muise, E.D.; Jennings, R.W.; Mohammed, S.; Demehri, F.R.; et al. Outcomes of surgical treatment of tracheobronchomalacia in children. Pediatr. Pulmonol. 2024, 59, 1922–1931. [Google Scholar] [CrossRef]
- Sainathan, S.; Meshulami, N.; Shah, P.A.; Murthy, R. Partial upper median sternotomy for anterior aortopexy for innominate artery compression syndrome: A case series. Transl. Pediatr. 2024, 13, 634–642. [Google Scholar] [CrossRef]
- Sutton, L.; Maughan, E.; Pianosi, K.; Jama, G.; Rouhani, M.J.; Hewitt, R.; Muthialu, N.; Butler, C.; De Coppi, P. Open and Thoracoscopic Aortopexy for Airway Malacia in Children: 15 Year Single Centre Experience. J. Pediatr. Surg. 2024, 59, 197–201. [Google Scholar] [CrossRef]
- Clayton Von Allmen, D.; Torres-Silva, C.; Rutter, M.J. Factors associated with success following transcervical innominate artery suspension. Int. J. Pediatr. Otorhinolaryngol. 2021, 150, 110939. [Google Scholar] [CrossRef]
- Vaidya, Y.; Segura, B.; Goldfarb, S.; Sinha, P. Aortopexy Using Upper Hemisternotomy. Innov. Technol. Technol. Cardiothorac. Vasc. Surg. 2024, 19, 310. [Google Scholar] [CrossRef]
- Masters, I.B.; Chang, A.B. Interventions for primary (intrinsic) tracheomalacia in children. Cochrane Database Syst. Rev. 2005, 19, CD005304. [Google Scholar] [CrossRef]
- Goyal, V.; Masters, I.B.; Chang, A.B. Interventions for primary (intrinsic) tracheomalacia in children. Cochrane Database Syst. Rev. 2012, 2012, CD005304. [Google Scholar] [CrossRef] [PubMed]
- Hysinger, E.B.; Panitch, H.B. Paediatric Tracheomalacia. Paediatr. Respir. Rev. 2016, 17, 9–15. [Google Scholar] [CrossRef] [PubMed]
- Kamran, A.; Zendejas, B.; Jennings, R.W. Current concepts in tracheobronchomalacia: Diagnosis and treatment. Semin. Pediatr. Surg. 2021, 30, 151062. [Google Scholar] [CrossRef] [PubMed]
- Sumida, W.; Yasui, A.; Shirota, C.; Makita, S.; Okamoto, M.; Ogata, S.; Takimoto, A.; Takada, S.; Nakagawa, Y.; Kato, D.; et al. Update on aortopexy and posterior tracheopexy for tracheomalacia in patients with esophageal atresia. Surg. Today. 2024, 54, 211–219. [Google Scholar] [CrossRef]
- Majid, A.; Gaurav, K.; Sanchez, J.M.; Berger, R.L.; Folch, E.; Fernandez-Bussy, S.; Ernst, A.; Gangadharan, S.P. Evaluation of tracheobronchomalacia by dynamic flexible bronchoscopy. A pilot study. Ann. Am. Thorac. Soc. 2014, 11, 951–955. [Google Scholar] [CrossRef]
- Kompare, M.; Weinberger, M. Protracted bacterial bronchitis in young children: Association with airway malacia. J. Pediatr. 2012, 160, 88–92. [Google Scholar] [CrossRef]
- Fayon, M.; Donato, L. Tracheomalacia (TM) or bronchomalacia (BM) in children: Conservative or invasive therapy. Arch. Pediatr. Organe Off. Soc. Francaise Pediatr. 2010, 17, 97–104. [Google Scholar] [CrossRef]
- Dave, S.; Currie, B.G. The role of aortopexy in severe tracheomalacia. J. Pediatr. Surg. 2006, 41, 533–537. [Google Scholar] [CrossRef]
- Okuyama, H.; Tazuke, Y.; Uenoa, T.; Yamanaka, H.; Takama, Y.; Saka, R.; Nara, K.; Usui, N. Long-term morbidity in adolescents and young adults with surgically treated esophageal atresia. Surg. Today. 2017, 47, 872–876. [Google Scholar] [CrossRef]
- Van Hal, A.F.R.L.; Aanen, I.P.; Wijnen, R.M.H.; Pullens, B.; Vlot, J. The Value of Preoperative Rigid Tracheobronchoscopy for the Diagnosis of Tracheomalacia in Oesophageal Atresia Patients. J. Pediatr. Surg. 2024, 59, 161620. [Google Scholar] [CrossRef]
- Van der Zee, D.C.; van Herwaarden, M.Y.A.; Hulsker, C.C.C.; Witvliet, M.J.; Tytgat, S.H.A. Esophageal Atresia and Upper Airway Pathology. Clin. Perinatol. 2017, 44, 753–762. [Google Scholar] [CrossRef] [PubMed]
- Brooks, G.; Gazzaneo, M.; Bertozzi, M.; Riccipetitoni, G.; Raffaele, A. Systematic review of long term follow-up and transitional care in adolescents and adults with esophageal atresia—Why is transitional care mandatory? Eur. J. Pediatr. 2023, 182, 2057–2066. [Google Scholar] [CrossRef] [PubMed]
- Krishnan, U.; Mousa, H.; Dall’Oglio, L.; Homaira, N.; Rosen, R.; Faure, C.; Gottrand, F. ESPGHAN-NASPGHAN Guidelines for the Evaluation and Treatment of Gastrointestinal and Nutritional Complications in Children with Esophageal Atresia-Tracheoesophageal Fistula. J. Pediatr. Gastroenterol. Nutr. 2016, 63, 550–570. [Google Scholar] [CrossRef] [PubMed]
- Kamran, A.; Jennings, R.W. Tracheomalacia and Tracheobronchomalacia in Pediatrics: An Overview of Evaluation, Medical Management, and Surgical Treatment. Front. Pediatr. 2019, 7, 512. [Google Scholar] [CrossRef]
- Kiblawi, R.; Zoeller, C.; Zanini, A.; Ure, B.M.; Dingemann, J.; Kuebler, J.F.; Schukfeh, N. Video-Assisted Thoracoscopic or Conventional Thoracic Surgery in Infants and Children: Current Evidence. Eur. J. Pediatr. Surg. 2021, 31, 54–64. [Google Scholar] [CrossRef]
- Macchini, F.; Zanini, A.; Morandi, A.; Ichino, M.; Leva, E. Thoracoscopic Surgery for Congenital Lung Malformation Using Miniaturized 3-mm Vessel Sealing and 5-mm Stapling Devices: Single-Center Experience. J. Laparoendosc. Adv. Surg. Technol. A 2020, 30, 444–447. [Google Scholar] [CrossRef]
- Shieh, H.F.; Smithers, C.J.; Hamilton, T.E.; Zurakowski, D.; Rhein, L.M.; Manfredi, M.A.; Baird, C.W.; Jennings, R.W. Posterior tracheopexy for severe tracheomalacia. J. Pediatr. Surg. 2017, 52, 951–955. [Google Scholar] [CrossRef]
- Torre, M.; Reali, S.; Rizzo, F.; Guerriero, V.; Palo, F.; Arrigo, S.; Sacco, O.; Mattioli, G. Posterior Tracheopexy for Tracheomalacia: A Study of Clinical and Radiological Consequences on Esophagus. Eur. J. Pediatr. Surg. 2024, 34, 306–313. [Google Scholar] [CrossRef]
- Tytgat, S.H.A.J.; van Herwaarden-Lindeboom, M.Y.A.; van Tuyll van Serooskerken, E.S.; van der Zee, D.C. Thoracoscopic posterior tracheopexy during primary esophageal atresia repair: A new approach to prevent tracheomalacia complications. J. Pediatr. Surg. 2018, 53, 1420–1423. [Google Scholar] [CrossRef]
- Mohammed, S.; Kamran, A.; Izadi, S.; Visner, G.; Frain, L.; Demehri, F.R.; Shieh, H.F.; Jennings, R.W.; Smithers, C.J.; Zendejas, B. Primary Posterior Tracheopexy at Time of Esophageal Atresia Repair Significantly Reduces Respiratory Morbidity. J. Pediatr. Surg. 2024, 59, 10–17. [Google Scholar] [CrossRef]
- Van Stigt, M.J.B.; van Hal, A.F.R.L.; Bittermann, A.J.N.; Butler, C.R.; Ceelie, I.; Cianci, D.; de Coppi, P.; Gahm, C.; Hut, J.E.; Joosten, K.F.M.; et al. Does primary posterior tracheopexy prevent collapse of the trachea in newborns with oesophageal atresia and tracheomalacia? A study protocol for an international, multicentre randomised controlled trial (PORTRAIT trial). BMJ Open. 2024, 14, e087272. [Google Scholar] [CrossRef] [PubMed]
- Serio, P.; Fainardi, V.; Leone, R.; Baggi, R.; Grisotto, L.; Biggeri, A.; Mirabile, L. Tracheobronchial obstruction: Follow-up study of 100 children treated with airway stenting. Eur. J. Cardio-Thorac. Surg. 2014, 45, e100–e109. [Google Scholar] [CrossRef] [PubMed]
- Serio, P.; Nenna, R.; Di Maurizio, M.; Avenali, S.; Leone, R.; Baggi, R.; Arcieri, L.; Murzi, B.; Quarti, A.; Pozzi, M.; et al. Outcome of long-term complications after permanent metallic left bronchial stenting in children. Eur. J. Cardio-Thorac. Surg. 2018, 53, 610–617. [Google Scholar] [CrossRef] [PubMed]
- Antón-Pacheco, J.L.; Luna, C.; García, E.; López, M.; Morante, R.; Tordable, C.; Palacios, A.; de Miguel, M.; Benavent, I.; Gómez, A. Initial experience with a new biodegradable airway stent in children: Is this the stent we were waiting for? Pediatr. Pulmonol. 2016, 51, 607–612. [Google Scholar] [CrossRef]
- Wallis, C.; McLaren, C.A. Tracheobronchial stenting for airway malacia. Paediatr. Respir. Rev. 2018, 27, 48–59. [Google Scholar] [CrossRef]
- Serio, P.; Nenna, R.; Fainardi, V.; Grisotto, L.; Biggeri, A.; Leone, R.; Arcieri, L.; Di Maurizio, M.; Colosimo, D.; Baggi, R.; et al. Residual tracheobronchial malacia after surgery for vascular compression in children: Treatment with stenting. Eur. J. Cardio-Thorac. Surg. 2017, 51, 211–217. [Google Scholar] [CrossRef][Green Version]

| Author | Period | N° | Age Months (Range) | Approach | Thymectomy | Pericardiotomy | Pledgets | Complications | Redo | Success | Follow-Up |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Jennings et al. J. Pediatr. Surg., 2014 [9] | 1997–2012 | 41 | 7.5 (1–136) | 20 ST 13 TT 8 TS | Partial, only open cases | 20/20 ST 13/13 TT 5/8 TS | 20/20 ST | 1 vocal cord palsy | 3 TS | 20/20 ST 10/13 TT 5/8 TS | 10 m–14 yr |
| Montgomery et al. Eur. J. Pediatr. Surg., 2014 [14] | 1993–2012 | 30 | 6.8 (0.5–31) | 20 TT 10 ST | NM | NM | NM | 2 PNX 1 vocal cord palsy | 0 | 22/30 3/30 partial relief | 25.5 (1 m–12 yr) |
| Kay-Rivest et al. Dis. Esophagus., 2015 [15] | 1989–2010 | 6 | 2.1 (0.6–3) | 6 TT | 6 total | NM | NM | 1 bleeding 1 phrenic nerve palsy | 0 | 6/6 | 2 yr |
| Van der Zee et al. World J. Surg., 2015 [10] | 2002–2012 | 16 | 5 (0.5–12) | 16 TS | No | No | No | 0 | 5 | 10/16 | 6 m–10 yr |
| Gruszka et al. Interact. Cardiovasc. Thorac. Surg., 2017 [16] | 1994–2012 | 53 | 13 (1–120) | 29 ST 21 TT | Partial or total | No | 53/53 | 1 pleural effusion 3 phrenic nerve palsy | 0 | 51/53 | 4.9 yr (0.3–14.9) |
| Haveliwala et al. J. Pediatr. Surg., 2018 [17] | 2016–2018 | 22 | 5 (0.5–60) | 22 CV | Partial or total | NM | 22/22 | 1 PNX | 0 | 16 | 6 wks |
| Williams et al. J. Laryngol. Otol., 2020 [18] | 2007–2017 | 25 | 9.4 (0.5–35) | 23 ST 2 TT | Total | NM | NM | 4 tracheostomy 3 respiratory infections 2 vocal cord palsy 2 wound infection | 1 | 20 | 5.2 yr (1.2–8.5) |
| Dolmaci et al. Interact. Cardiovasc. Thorac. Surg., 2021 [19] | 2010–2020 | 24 | 9 (2–117) | 24 ST | 20/24 partial or total | 24/24 | Straps | 1 PNX 1 pericardial effusion | 0 | 22 | 25.5 m (18–34) |
| Clayton von Allmen et al. Int. J. Pediatr. Otorhinolaryngol., 2021 [28] | 2011–2021 | 10 | 102.8 (3–192) | 10 CV | Partial or total | NM | 10/10 | 1 seroma 1 reintubation | 1 | 6 | NM |
| Isik et al. Pediatr. Surg. Int., 2022 [20] | 2018–2021 | 15 | 16.3 (1–31) | 15 ST | Partial | NM | 15/15 | NM | NM | NM | NM |
| Williamson et al. J Pediatr Surg2022 [21] | 2010–2010 | 10 | 2.2 (0–6) | NM | NM | NM | NM | NM | NM | NM | NM |
| Del Fernandes et al. J. Pediatr. Surg., 2023 [22] | 2000–2018 | 7 | 5 (1–15) | NM | NM | NM | NM | 1 vocal cord palsy | 0 | 7 | NM |
| Sutton et al. J. Pediatr. Surg., 2024 [27] | 2006–2021 | 169 | ST and TT: 7.7 (0–233) TS: 5.2 (2–27) | 135 ST 12 TT 22 TS | NM ST and TT 22/22 TS partial | 135/135 ST 12/12 TT 22/22 TS | 135/135 ST 12/12 TT 22/22 TS | 42 (PNX most common) | 9 ST 2 TS | NM ST and TT 19/22 TS | 8.6 yr (1–20 yr) |
| Sainathan et al. Transl. Pediatr., 2024 [26] | 2017–2020 | 9 | 9.6 (2–24) | 9 ST | 9/9 total | 9/9 | 9/9 | NM | 0 | 7/9 | 6 m |
| Vaidya et al. Innovations (Phila.), 2024 [29] | 2024 | 1 | 3 | 1 ST | No | 1/1 | 1/1 | 1 Dressler syndrome | 0 | 1 | 6 m |
| Barreto et al. J. Pediatr. (Rio J.), 2024 [24] | 2003–2023 | 15 | NM | Open approach | Partial or total | NM | 15/15 | NM | 0 | 11 | NM |
| Mukharesh et al. Pediatr. Pulmonol., 2024 [25] | 2013–2020 | 20 | NM | 20 ST | NM | NM | NM | NM | NM | NM | NM |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zanini, A.; Mazzoleni, S.; Arcieri, L.; Giordano, R.; Marianeschi, S.; Macchini, F. Aortopexy for Tracheomalacia in Children: A Systematic Review and Meta-Analysis. J. Clin. Med. 2025, 14, 1367. https://doi.org/10.3390/jcm14041367
Zanini A, Mazzoleni S, Arcieri L, Giordano R, Marianeschi S, Macchini F. Aortopexy for Tracheomalacia in Children: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2025; 14(4):1367. https://doi.org/10.3390/jcm14041367
Chicago/Turabian StyleZanini, Andrea, Stefano Mazzoleni, Luigi Arcieri, Raffaele Giordano, Stefano Marianeschi, and Francesco Macchini. 2025. "Aortopexy for Tracheomalacia in Children: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 14, no. 4: 1367. https://doi.org/10.3390/jcm14041367
APA StyleZanini, A., Mazzoleni, S., Arcieri, L., Giordano, R., Marianeschi, S., & Macchini, F. (2025). Aortopexy for Tracheomalacia in Children: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 14(4), 1367. https://doi.org/10.3390/jcm14041367







