Abstract
Background/Objectives: According to the modified Mason classification, radial head fractures can be treated with open reduction and internal fixation (ORIF), radial head arthroplasty, or resection. This study by the Department of Traumatology and Orthopedics of the Military Institute of Medicine aimed to compare the clinical and radiological outcomes of fractures treated with ORIF. Methods: This retrospective study analyzed 55 patients with radial head fractures treated between April 2020 and February 2023. Fractures were classified using Mason system as 15 type II, 26 type III, and 14 type IV. Clinical outcomes were evaluated using the VAS for pain, Broberg–Morrey scale, and the DASH questionnaire, alongside assessments of range of motion, grip strength, and elbow stability. Follow-up radiographs examined bone union, bone fragments displacement, degenerative changes and periarticular ossification. Results: The mean follow-up period was 21.0 ± 10.2 months. There were no statistically significant differences in VAS scale results for Mason types II, III, and IV fractures (4.0 vs. 6.0 vs. 5.0, respectively; p = 0.825), the Broberg–Morrey scale (82.0 ± 15.2 vs. 80.9 ± 15.5 vs. 84.2 ± 15.1, respectively; p = 0.845), or the DASH questionnaire (10.0 vs. 11.7 vs. 17.5, respectively; p = 0.937). Mean extension deficit and supination angles were at the limit of statistical significance (p = 0.076 and p = 0.051). No cases of lateral instability were observed, whereas medial instability was seen in only one case. Bone union was observed in 97.5% of cases, with elbow joint osteoarthritis and periarticular ossification in 15.0% and 45.0% of cases, respectively. Conclusions: Mason type II, III and IV radial head fractures treated with open reduction and internal fixation showed good functional and radiological outcomes with rare complications, including degenerative changes, periarticular ossifications and nonunion.
1. Introduction
Radial head fractures account for 1.5–4% of all fractures in adults [1,2]. The division of these fractures is based on the Mason classification [3], with a modification by Johnston [4]. The criteria for the division are the degree of fragmentation and displacement of fragments. According to Mason classification, type I fractures (non-displaced or with a displacement up to 2 mm) are most often treated non-operatively, with good treatment outcomes [5,6]. Simple fractures displaced >2 mm are classified as type II fractures. Due to the high risk of mechanical block with limited range of motion of the elbow joint, surgical treatment is most performed. According to some reports, treatment results are comparable to those of non-operative treatment [7,8].
Type III includes comminuted fractures involving the entire surface of the radial head, whereas type IV includes fractures coexisting with the elbow joint dislocation. In the past, the only treatment for such fractures was radial head resection, which is no longer commonly practiced [9]. Types III and IV fractures are treated with open reduction and internal fixation (ORIF) or radial head arthroplasty (RHA) when ORIF is contraindicated [10]. The most commonly chosen method for treating type III fractures is RHA [11] though no consensus has been reached yet. The choice between ORIF or RHA often depends on surgeon’s experience and preferences.
In the Department of Traumatology and Orthopedics of the Military Institute of Medicine, ORIF is preferred for the treatment of types II, III, and IV fractures, while other methods are not practiced due to surgeons’ individual experience and previous good clinical results [12]. Most of available publications on radial head fractures compare the results of treatment between different surgical methods for one type of fracture according to Mason classification [7,11,13,14,15,16,17,18,19,20]. However, there is a limited number of studies comparing the outcomes of different Mason type fractures treated with the same method (ORIF). We believe that the results of treatment are not determined only by the choice of surgical method but also by accompanying injuries and their management. Helmstetter et al. [21] suggested that minimally invasive approach and soft tissue repair reduced unsatisfactory results of ORIF, even in cases with comminution of radial head.
This study aimed to compare the clinical, functional, and radiological results of surgical treatment of type II, III, and IV radial head factures according to the Mason classification using open reduction internal fixation.
2. Materials and Methods
This retrospective study included patients with radial head fractures hospitalized in the Department of Traumatology and Orthopedics of the Military Institute of Medicine between April 2020 and February 2023.
Patients with polytrauma, terrible triad of the elbow and those treated nonoperatively were excluded. Fifty-three patients who underwent open reduction internal fixation were included in this study.
Data obtained from the Asseco Medical Management Solutions (AMMS) in-hospital information system (age at the time of injury, sex, side of the limb involved, dominant limb, mechanism of injury, associated fractures in the upper limb, occupational status, sporting activity, and smoking) were included in the analysis. Information regarding intraoperative observations was obtained from surgical descriptions (number of intermediate fragments, accompanying articular cartilage exfoliation of the radial head, assessment of ligamentous damage to the elbow joint i.e., LCL and MCL, assessment of bony defects of the radial head, and postoperative neurovascular disorders). Data from the postoperative follow-up visits, duration of immobilization after surgery, and postoperative complications were analyzed.
The affected limb was placed on a lateral table during surgery. We used Esmarch’s tourniquet in most cases. Either a posterolateral approach (known as Kocher approach) was usually chosen. The radial head and other intraarticular structures were assessed. Then a stability of elbow in full extension and 30° flexion was examined under fluoroscopy. The next step was to reduce the fracture, most often in order from the largest to the smallest bone fragments. If a radial head was anatomically reduced, then it was temporary fixed with K wires inserted parallel to the cartilage. If the reduction was stable, then the ASNIS Micro cannulated screws (Asnis Micro Cannulated Screw System; Stryker Inc., Kalamazoo, MI, USA) were tighten along the K wires. If the reduction stability was not clear, a fracture was also fixated with a buttress plate (VariAx Hand Plating System; Stryker Inc., Kalamazoo, MI, USA). During tightening screws into bone, care must be taken not to lose the reduction. In case of capitulum fracture, another one cannulated screw (Asnis Micro Cannulated Screw System; Stryker Inc., Kalamazoo, MI, USA) was used to fixate the fracture. Delamination of articular cartilage was usually managed with tissue adhesive. Ligament ruptures were repaired with suture anchors (JuggerKnot Soft Anchor System; Zimmer Biomet, Warsaw, IN, USA). The anchors were placed in lateral or medial epicondyle due to LCL complex or MCL rupture, respectively. Ligament fragments were fixed with Krackow suture.
Postoperatively, patients were immobilized with a cast in 90° flexion and neutral forearm rotation for about 2 weeks. After that, passive ROM exercises (including gravity-assisted and contralateral-arm-assisted) were implemented in physiotherapy protocol for about 2 weeks. Patients were then gradually encouraged to perform active elbow exercises under physiotherapist supervision until 6 weeks after surgery. There was neither indomethacin nor any other nonsteroidal anti-inflammatory drug was used for periprosthetic ossification prevention.
Long-term treatment outcomes were assessed based on the data obtained during follow-up visits. Visits were conducted at an outpatient orthopedic clinic. The patients completed visual analog scale (VAS) pain questionnaire and Disabilities of Arm, Shoulder, and Hand (DASH) functional assessment questionnaire. Physical examination was performed by senior assistant from the Department of Traumatology and Orthopedics. Flexion and extension angles of the elbow joint, as well as the pronation and supination of the forearm, were measured using a goniometer. Elbow joint stability was assessed in full extension and 30° flexion. Dynamometric measurement of grip strength of both operated and uninjured limbs was analyzed, and the operated-to-uninjured grip strength ratio was used in the analysis. The Broberg–Morrey scale was used for clinical assessment (scores include very good 95–100 points, good, 80–94 points, sufficient 60–79 points, and bad <60 points).
Radiological examinations from the Digital Imaging and Communications in Medicine database were analyzed i.e., X-rays and CT scans after injury (Figure 1), X-rays after surgery and X-rays at the last follow-up visit (Figure 2). Bone union, fracture displacement, periarticular ossification (the Hastings–Graham scale), elbow osteoarthritis, and signs of avascular necrosis of radial head were assessed.
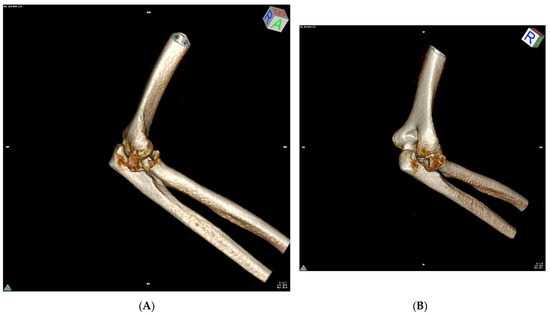
Figure 1.
Example of a CT scan (three-dimensional volume reconstruction) showing a Mason type III radial head fracture with significant fracture displacement—P.O. 35y (A,B).
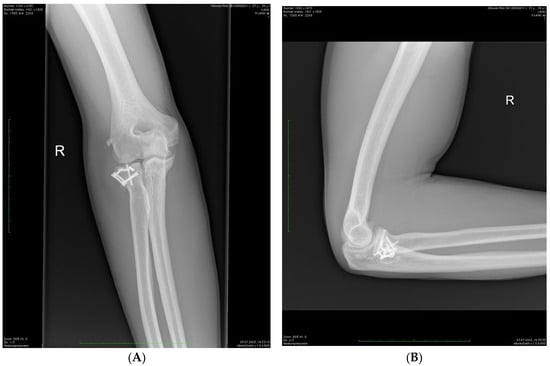
Figure 2.
Control X-ray in the same patient 23 months after surgery—AP (A) and lateral (B) projections. Complete bone union and asymptomatic periarticular ossification (Hastings–Graham 1).
The analysis was performed using R software (version 4.1.2). Basic descriptive statistics were used to describe numerical variables. Categorical variables are presented as number of observations and percentage of group participation. Normality of the distributions was checked with the Shapiro–Wilk test and verified using the skewness and kurtosis coefficients. Comparisons between groups were made using analysis of variance analysis and the Kruskal–Walli’s test for numerical variables and Pearson’s chi-square and Fisher’s exact tests for categorical variables. Throughout the analysis, p values less than 0.05 were regarded as evidence for statistical significance.
3. Results
The analyzed group included 55 cases from 53 patients. Age ranged between 18–78 years, with a mean of 43.5 ± 15.1 years. In two patients, the fracture occurred bilaterally, with one patient having a simultaneous fracture and the other having fractures of the individual limbs occurring at different times. More than half of the participants were women (56.6%). Average body mass index was 28.4 ± 5.9 kg/m2. Smoking was observed in five cases. Office work is the most common occupation. In more than half of the patients, participation in sports was declared (57.1%).
The most common injury occurred as a result of a fall on an extended limb (61.8%). In one patient, the injury resulted from a fall on the elbow-bent limb. In 47.1% of the patients, the fracture involved the dominant limb. No vascular injuries were observed in the study group, whereas one patient showed signs of post-traumatic brachial plexus injury. The general characteristics and occupational status of the patients are shown in Table 1.

Table 1.
General characteristics of patients.
According to the Mason scale, 27.3% of the cases were classified as type II and 47.3% as type III. A fracture with concomitant dislocation of the elbow joint (type IV according to the modified Mason scale) was diagnosed in 25.5% cases. An open fracture was diagnosed in one patient. Comminuted fractures (with > 2 fragments, including the shaft of the radius as a single fragment) were diagnosed in 61.8% cases. Articular cartilage degeneration occurred in nine cases. Lateral collateral ligament complex injury (LCL) was observed in 76.4 per cent cases, while the medial collateral ligament rupture (MCL) affected 20.0% cases. A concurrent capitellum fracture occurred in 21.8% cases. In 76.4% cases, the fracture was stabilized with ASNiS cannulated screws (Stryker) and anatomic buttress plate VariAx (Stryker), in 20.0% cases with ASNiS 2.0 cannulated screws (Stryker), and only in two cases with anatomic VariAx plate (Stryker).
Postoperatively, immobilization was used for 9–49 days, with a mean of 21.7 ± 10.4 days.
Characteristics of the groups during the operative period according to fracture type are presented in Table 2.

Table 2.
Characteristics of the group during the surgical period with breakdown by fracture type.
Thirty-nine patients attended the follow-up visits, yielding data from 41 cases. Follow-up time varied between 4.0–40.0 months, with a mean of 21.0 ± 10.2 months. The mean values and ranges of the individual parameters are listed in Table 3.

Table 3.
Comparison of treatment effects according to fracture type using the modified Mason scale.
The mean visual analog scale (VAS) pain score was 13.9 ± 20.6 and no statistically significant differences were observed among cases with individual fracture types (p = 0.825). Similarly, no statistically significant differences were observed between the groups for the DASH and Broberg-Morrey functional scale scores (p = 0.937 and p = 0.845, respectively). The mean scores for these scales in the study group were 20.8 ± 22.4 and 82.0 ± 15.0, respectively. The results of the clinical assessments are presented in Table 4. Very good and good scores were obtained in 83.0% of the cases (41.5% for each score). A sufficient score affected 12.2% of the patients. Only two patients had poor treatment outcomes.

Table 4.
Clinical outcomes by fracture type.
The mean flexion angle at the elbow joint was 134.6 ± 12.1 degrees, while the mean extension deficit was 11.6 ± 15.7 degrees. While the flexion angle values in different fracture types did not differ significantly, the extension deficit angle values varied at the limit of statistical significance (p = 0.076). Regarding rotational movements of the forearm, the mean pronation angle was 79.5 ± 16.3° and supination 58.3 ± 28.1 degrees. The supination angles for each fracture type were also at the limit of statistical significance (p = 0.051). The operated-to-uninjured grip strength ratio averaged 80.4 ± 24.5% and did not differ significantly between groups. No cases showed features of lateral elbow instability, whereas medial instability was observed in one patient with a Mason type IV fracture.
Radiological results of treatment are presented in Table 3. The results were obtained for 40 patients. Follow-up radiographs were waived for one patient due to pregnancy. Bone union was observed in 97.5% of the patients. No secondary fragments displacement was observed. Osteoarthritis was observed in 15.0% cases. Periarticular ossification occurred in 45.0% cases, six of which were asymptomatic (type 1 according to the Hastings–Graham scale). Only one patient had ankylosis of the elbow joint with significant limitations in flexion and extension movements (type 3a). Considering the division of fracture types according to the modified Mason scale, the individual results did not differ significantly.
4. Discussion
Despite improvements in surgical techniques, comminuted radial head fractures remain challenging [22,23,24]. No clear guidelines for the management of such fractures have emerged to date. The criteria used by Ring et al. [25], who recommended the use of ORIF methods in fractures with fewer than three intermediate fractures and the use of RHA in complex fractures, have been widely adopted. In contrast, Burkhart et al. [26] recommend ORIF in all cases where anatomical reduction and stable fixation is achievable.
The present study showed that the clinical results of radial head fractures treatment with ORIF methods were satisfactory. There were 41.5% very good and 41.5% good responses. There were no statistically significant differences in the treatment results for individual fracture types. Several studies reported similar results [21,22,24,27,28,29,30,31,32,33,34,35]. Walsh et al. [36] reported no difference in outcomes between simple and complex radial head fractures treated with ORIF. Additionally, Müller et al. showed that ORIF with a plate or screws provided good results [37]. In contrast, better functional outcomes were obtained in patients with type II fractures than in those with type III fractures.
Radiographic examination revealed bone union in 97.5% of patients. Displacement of the fragments was not observed. Nonunion occurred in only one patient with morbid obesity (body mass index, 52.0 kg/m2). The patient experienced little pain, and the supination movement of the forearm was limited. We found no reports in the literature supporting the hypothesis that obesity affects nonunion of the radial head. Post-traumatic osteoarthritis occurred in 15.0% cases and periarticular ossification in 45.0% cases.
Importantly, 33.3% of patients with periarticular ossification had no functional impairment of the operated limb (grade 1 according to Hastings–Graham). These results did not differ from those obtained by other authors [17,21,22,24,38,39]. In some studies, post-traumatic osteoarthritis and periarticular ossifications occurred less frequently [15,23,27,29,31,33,40]. In the present study, we did not use indomethacin or radiotherapy to prevent periarticular ossification.
Most of available studies present a comparative analysis of the results of radial head fractures treatment using different surgical methods. The results of these analyses vary. Some studies have shown the superiority of ORIF over other treatment modalities [14,15,19,27,41]; however, in the majority of publications, RHA yields better clinical results [11,13,16,42,43] or the results do not differ significantly [9,17,18,40]. To the best of our knowledge, only one meta-analysis has demonstrated the superiority of ORIF over other treatments [44]. In the other meta-analyses, radial head prosthesis yields better functional outcomes and fewer complications compared to ORIF [16,20]. However, RHA has some limitations (risk of periprosthetic osteolysis, implant loosening, and displacement). Additionally, the implantation of an overly large endoprosthesis may result in overstuffing [45]. Furthermore, the radial bone head can show substantial morphologic variations, making it difficult to fit an implant that is perfectly congruent with the articular surface of the elbow joint [46].
When comparing the treatment results of different surgical methods, the continuous technological progress and development of biomedical engineering should be considered [33,47]. Gruszka et al. [38] emphasize that the use of modern anatomical locking plates provides good results in the treatment of fractures of the head and neck of the radial bone, even in comminuted fractures associated with damage to other structures of the elbow joint. The authors used both rim and buttress plates but showed no statistically significant differences in treatment outcomes. Good results in radial head fractures treatment with cannulated screw stabilization using the ‘tripod’ technique have also been described [39].
The associated injuries and stability of elbow joint in radial head fractures are important issues. Many authors emphasize the role of radial head as a secondary stabilizer of the elbow joint against valgus forces and axial loading [10,43,48,49]. Rhyou et al. [50] believed that radial head fractures are always accompanied by collateral ligaments rupture and comminuted fractures are associated with medial collateral ligament rupture. In contrast, van Riet et al. [51] showed that associated ligamentous injury occurred in 11% of radial head fractures. In the present study, injuries to the lateral and medial collateral ligaments accounted for as many as 76.4% and 20.0% cases, respectively. These results are supported by the work of Kaas et al. [52] and Itamura et al. [53], who assessed injuries associated with radial head fractures using magnetic resonance imaging. The authors emphasized that magnetic resonance imaging allows for a better understanding of the mechanism of injury and the planning of appropriate treatment. In the present study, magnetic resonance imaging was not routinely performed when radial head fractures were diagnosed. Associated injuries were identified during surgery.
Harbrecht et al. [54] presented a case series of radial head fracture nonunion caused by interrupting cartilage fragments released from capitulum. In our study, capitulum fracture (21.8%) and exfoliation of radial head cartilage (16.4%) were also observed but did not significantly affect the results of treatment.
In terrible triad of the elbow, apart from a radial head fracture, there is a coronoid process fracture with dislocation of the elbow. The treatment of associated injuries is even more difficult and complex and can affect the final results of the treatment—both functionally and radiologically. This is the reason why we excluded this group of patients from the study. The same argument applies to the Monteggia fracture, but in most cases radial head is luxated, not broken. Moreover, at the time of the study, a small group of patients with these injuries (‘terrible triad’ n = 19, Monteggia fracture n = 5) were treated in the Department of Traumatology and Orthopedics, the results of statistical analysis would have been unrepresentative.
In the present article, no statistically significant differences were obtained in the clinical, functional or radiological results. This means that the treatment outcomes are not determined solely by the type of fracture. Instead, factors such as the quality of reduction, stable fixation, and associated injuries (articular cartilage damage, ligamentous rupture, accompanying capitulum fracture, etc.) play an important role. The experience of the surgeon and the use of more appropriate implants are also important [38]. Besides, ORIF is a technically more demanding procedure to perform compared to RHA [11]. Furthermore, according to Jakobi et al. [55], when ORIF methods fails, conversion to secondary prosthesis of the radial head yields good results.
The present study has several limitations. First, it was retrospective in nature and did not include a control group. To our knowledge, only one prospective study has evaluated the results of the treatment of radial head fractures using ORIF [32]. Second, the small sample size of the study group may have significantly affected the statistical analysis. It was also impossible to perform a comparative analysis; neither radial head resections nor arthroplasty was performed at the study center. Third, in some cases, it was impossible to obtain complete data from the in-hospital information systems. Fourth, the study did not consider concomitant fractures in the upper limbs except capitulum fracture (e.g., Monteggia fractures and terrible triad of the elbow). According to Pike et al., associated fractures can affect functional outcomes of radial head fractures treatment [35]. Fifth, the follow-up duration varied widely. The longer the time that has passed since the fracture, the more advanced adaptive processes that occur in the functionality of the limb. However, the long-term increasing risk of post-traumatic osteoarthritis must be considered.
5. Conclusions
Types II, III, and IV radial head fractures, according to the Mason classification, treated with open reduction and internal fixation provide good clinical results. Complications such as osteoarthritis, periarticular ossification and nonunion are rare. These fracture types should always be considered as complex injuries (articular cartilage and ligament rupture). The surgeon’s skills, preferences, and appropriate hardware are very important factors in determining good clinical and radiological outcomes of ORIF.
Author Contributions
Conceptualization, P.N., Ł.J., D.L. and P.C.; Methodology, P.N., Ł.J., D.L., P.P, T.Z. and P.C.; Formal analysis, P.N., Ł.J., D.L., T.Z. and P.C.; investigation, P.N., P.P. and P.C.; resources, P.C.; data curation, P.N. and P.C.; writing—original draft preparation, P.N., Ł.J., D.L., P.P. and P.C.; visualization, P.C.; supervision, Ł.J., D.L. and P.C.; project administration, P.N, K.C. and P.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study, due to retrospective studies.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are contained within the article.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| AMMS | Asseco Medical Management Solutions |
| AP | anteroposterior view |
| BMI | Body Mass Index |
| CT | Computed Tomography |
| DASH | Disabilities of Arm, Shoulder, and Hand Questionnaire |
| IQR | interquartile range |
| K | females |
| LCL | lateral collateral ligament |
| M | males |
| M ± SD | mean ± standard deviation |
| MCL | medial collateral ligament |
| ORIF | Open Reduction and Internal Fixation |
| RHA | Radial Head Arthroplasty |
| ROM | range of motion |
| VAS | Visual Analog Scale |
References
- Kovar, F.M.; Jaindl, M.; Thalhammer, G.; Rupert, S.; Platzer, P.; Endler, G.; Vielgut, I.; Kutscha-Lissberg, F. Incidence and analysis of radial head and neck fractures. World J. Orthop. 2013, 4, 80–84. [Google Scholar] [CrossRef] [PubMed]
- Duckworth, A.D.; Clement, N.D.; Jenkins, P.J.; Aitken, S.A.; Court-Brown, C.M.; McQueen, M.M. The epidemiology of radial head and neck fractures. J. Hand Surg. Am. 2012, 37, 112–119. [Google Scholar] [CrossRef]
- Mason, M. Some observations on fractures of the head of the radius with a review of one hundred cases. Br. J. Surg. 1954, 42, 123–132. [Google Scholar] [CrossRef] [PubMed]
- Johnston, G.W. A follow-up of one hundred cases of fracture of the head of the radius with a review of the literature. Ulster Med. J. 1962, 31, 51–56. [Google Scholar]
- Akesson, T.; Herbertsson, P.; Josefsson, P.O.; Hasserius, R.; Besjakov, J.; Karlsson, M.K. Primary nonoperative treatment of moderately displaced two-part fractures of the radial head. J. Bone Joint Surg. 2006, 88-A, 1909–1914. [Google Scholar]
- Weseley, M.S.; Barenfeld, P.A.; Eisenstein, A.L. Closed treatment of isolated radial head fractures. J. Trauma. 1983, 23, 36–39. [Google Scholar] [CrossRef]
- von Glinski, A.; Rausch, V.; Königshausen, M.; Dudda, M.; Schildhauer, T.A.; Seybold, D.; Geßmann, J. Instabilität nach operativer und konservativer Versorgung von isolierten Mason-II Frakturen. Unfallchirurg 2019, 122, 219–224. [Google Scholar] [CrossRef]
- Yoon, A.; King, G.J.; Grewal, R. Is ORIF Superior to Nonoperative Treatment in Isolated Displaced Partial Articular Fractures of the Radial Head? Clin. Orthop. Relat. Res. 2014, 472, 2105–2112. [Google Scholar] [CrossRef]
- VanBeek, C.; Levine, W. Radial head—Resect, fix or replace. Oper. Tech. Orthop. 2010, 20, 2–10. [Google Scholar] [CrossRef]
- Charalambous, C.P.; Stanley, J.K.; Mills, S.P.; Hayton, M.J.; Hearnden, A.; Trail, I.; Gagey, O. Comminuted radial head fractures: Aspects of current management. J. Shoulder Elbow Surg. 2011, 20, 996–1007. [Google Scholar] [CrossRef]
- Chen, H.W.; Tian, J.L.; Zhang, Y.Z. Therapeutic Effect of Resection, Prosthetic Replacement and Open Reduction and Internal Fixation for the Treatment of Mason Type III Radial Head Fracture. J. Invest. Surg. 2021, 34, 30–38. [Google Scholar] [CrossRef] [PubMed]
- Chwedczuk, B.; Piekarczyk, P.; Kwiatkowski, P.; Piątkowski, K. Surgical Treatment of Radial Head Fractures: Outcomes and Complications. Ortop. Traumatol. Rehabil. 2016, 18, 435–444. [Google Scholar] [CrossRef] [PubMed]
- Lanzerath, F.; Hackl, M.; Wegmann, K.; Müller, L.P.; Leschinger, T. The treatment of isolated Mason type II radial head fractures: A systematic review. J. Shoulder Elbow Surg. 2021, 30, 487–494. [Google Scholar] [CrossRef]
- Zarifian, A.; Shoorin, H.R.; Moghaddam, M.H.; Vavsari, M.F.; Gharedaghi, M.; Moradi, A. The Best Option in Treatment of Modified Mason Type III Radial Head Fractures: Open Reduction and Internal Fixation Versus Radial Head Excision. Arch. Bone Jt. Surg. 2018, 6, 365–370. [Google Scholar]
- Ikeda, M.; Sugiyama, K.; Kang, C.; Takagaki, T.; Oka, Y. Comminuted Fractures of the Radial Head. Comparison of Resection and Internal Fixation. J. Bone Joint Surg. 2005, 87, 76–84. [Google Scholar] [CrossRef]
- Li, N.; Chen, S. Open reduction and internal fixation versus radial head replacement in treatment of Mason type III radial head fractures. Eur. J. Ortop. Surg. Traumatol. 2014, 24, 851–855. [Google Scholar] [CrossRef]
- Kusnezov, N.; Eisenstein, E.; Dunn, J.C.; Fares, A.; Mitchell, J.; Kilcoyne, K.; Waterman, B.R. Operative Management of Unstable Radial Head Fractures in a Young Active Population. Hand 2018, 13, 473–480. [Google Scholar] [CrossRef]
- Al-Burdeni, S.; Abuodeh, Y.; Ibrahim, T.; Ahmed, G. Open reduction and internal fixation versus radial head arthroplasty in the treatment of adult closed comminuted radial head fractures (modified Mason type III and IV). Int. Orthop. (SICOT) 2015, 39, 1659–1664. [Google Scholar] [CrossRef]
- Ryu, S.M.; Park, S.G.; Kim, J.H.; Yang, H.S.; Na, H.D.; Seo, J.S. Treatment of Modified Mason Type III or IV Radial Head Fracture: Open Reduction and Internal Fixation versus Arthroplasty. Indian. J. Orthop. 2018, 52, 590–595. [Google Scholar] [CrossRef]
- Sun, H.; Duan, J.; Li, F. Comparison between radial head arthroplasty and open reduction and internal fixation in patients with radial head fractures (modified Mason type III and IV): A meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2016, 26, 283–291. [Google Scholar] [CrossRef]
- Helmstetter, T.; Maniglio, M.; Fornaciari, P.; Tannast, M.; Vial, P. Open reduction and internal fixation of modified Mason type III/IV radial head fractures with more than three fragments: An analysis of the clinical outcome and reoperation rate. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 1121–1130. [Google Scholar] [CrossRef] [PubMed]
- Kastenberger, T.; Kaiser, P.; Spicher, A.; Stock, K.; Benedikt, S.; Schmidle, G.; Arora, R. Clinical and radiological outcome of Mason-Johnston types III and IV radial head fractures treated by an on-table reconstruction. J. Orthop. Surg. Res. 2022, 17, 503. [Google Scholar] [CrossRef] [PubMed]
- Kumar, K.; Sharma, G.; Farooque, K.; Sharma, V.; Jain, V.; Singh, R.; Morey, V. On-table reconstruction and fixation of Mason type III radial head fractures. Chin. J. Traumatol. 2015, 18, 288–292. [Google Scholar] [CrossRef] [PubMed]
- Koslowsky, T.C.; Mader, K.; Gausepohl, T.; Pennig, D. Reconstruction of Mason type-III and type-IV radial head fractures with a new fixation device. Acta Orthop. 2007, 78, 151–156. [Google Scholar] [CrossRef]
- Ring, D.; Quintero, J.; Jupiter, J.B. Open reduction and internal fixation of fractures of the radial head. J. Bone Joint Surg. Am. 2002, 84, 181101815. [Google Scholar] [CrossRef]
- Burkhart, K.J.; Wegmann, K.; Dargel, J.; Ries, C.; Mueller, L.P. Treatment of radial head and neck fractures: In favor of anatomic reconstruction. Eur. J. Trauma. Emerg. Surg. 2012, 38, 593–603. [Google Scholar] [CrossRef]
- Nalbantoglu, U.; Kocaoglu, B.; Gereli, A.; Aktas, S.; Guven, O. Open reduction and internal fixation of Mason type III radial head fractures with and without an associated elbow dislocation. J. Hand Surg. Am. 2007, 32, 1560–1568. [Google Scholar] [CrossRef]
- Zhang, D.; Dyer, G.S.; Earp, B.E.; Blazar, P. Complications, Reoperations, and Long-Term Outcomes after Open Reduction Internal Fixation of Mason Classification Type II and Type III Radial Head Fractures. J. Hand Microsurg. 2023, 15, 45–52. [Google Scholar] [CrossRef]
- Lee, Y.S.; Kang, Y.H.; Chung, Y.G.; Shin, S.H. Open reduction and internal fixation for Mason type III radial head fractures: Is it different from that from Mason II fractures? J. Orthop. Surg. 2018, 26, 1–8. [Google Scholar] [CrossRef]
- Crönlein, M.; Zyskowski, M.; Beirer, M.; Imhoff, F.B.; Pförringer, D.; Sandmann, G.H.; Kirchhoff, C.; Biberthaler, P.; Siebenlist, S. Using an anatomically preshaped low-profile locking plate system leads to reliable results in comminuted radial head fractures. Arch. Orthop. Trauma. Surg. 2017, 137, 789–795. [Google Scholar] [CrossRef]
- Xiang, Y.; Jiang, Z.; Zhi, X.; Wang, H. Outcomes of radial head fractures treated with pre-curved metacarpal plate. BMC Musculoskel Dis. 2023, 24, 437. [Google Scholar]
- Wu, P.H.; Dixit, A.; Tan, D.M.; Shen, L.; Chee, Y.H. Prospective study of surgical fixation of radial head fractures using cannulated headless compression screws for simple and complex radial head fractures. J. Orthop. Surg. 2017, 25, 1–8. [Google Scholar] [CrossRef]
- Shi, Y.; Wang, G.F.; Mei, K.; Zhang, J.; Yun, C.J.; Qian, C.; Sun, J.Y. Clinical and radiographic outcomes of treatment of comminuted Mason type II radial head fractures with a new implant. Medicine 2018, 97, e0086. [Google Scholar] [CrossRef] [PubMed]
- Yano, K.; Fukuda, M.; Uemura, T.; Kaneshiro, Y.; Yamanaka, K.; Teraura, H.; Yamamoto, K.; Sasaki, R.; Matsuura, T. Clinical Results of Surgical Treatment for Comminuted Radail Head and Neck Fracture: Headless Compression Screws Versus Plate Fixation. Indian. J. Orthop. 2022, 57, 253–261. [Google Scholar] [CrossRef]
- Pike, J.M.; Grewal, R.; Athwal, G.S.; Faber, K.J.; King, G.J. Open Reduction and Internal Fixation of Radial Head Fractures. Do Outcomes Differ Between Simple and Complex Injuries? Clin. Orthop. Relat. Res. 2014, 472, 2120–2127. [Google Scholar] [CrossRef] [PubMed]
- Walsh, A.; Zhang, Y.; McGough, J.; Kim, J.; Hausman, M. Open Reduction Internal Fixation of Simple Versus Comminuted Radial Head Fractures: Comparison of Clinical Outcomes. J. Hand Surg. Am. 2023, 48, 1059.e1–1059.e9. [Google Scholar] [CrossRef]
- Muller, M.; Mann, V.; Zapf, J.; Kirchhoff, K.; Zyskowski, M.; Biberthaler, P.; Kirchhoff, C.H.; Wurm, M. Functional Postoperative Outcome for 92 Cases of Radial Head Fractures: A PROM-Based Retrospective Study. J. Clin. Med. 2023, 18, 5870. [Google Scholar] [CrossRef]
- Gruszka, D.; Nowak, T.E.; Tkacz, T.; Wagner, D.; Rommens, P.M. Complex radial head and neck fractures treated with modern locking plate fixation. J. Shoulder Elbow Surg. 2019, 28, 1130–1138. [Google Scholar] [CrossRef]
- Model, Z.; Merchan, N.; Rozental, T.D.; Harper, C.M. Outcomes of Radial Head Fractures Treated With the “Tripod Technique”. J. Hand Surg. Am. 2022, 47, 582.e1–582.e5. [Google Scholar] [CrossRef]
- Gokaraju, K.; Domos, P.; Aweid, O.; Fisher, R.; White, A.; Rensburg, L.V.; Kang, S.N. Mid-term outcomes of surgical management of complex, isolated radial head fractures: A multicentre collaboration. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 1369–1376. [Google Scholar] [CrossRef]
- Wu, P.H.; Shen, L.; Chee, Y.H. Screw fixation versus arthroplasty versus plate fixation for 3-part radial head fractures. J. Orthop. Surg. 2016, 24, 57–61. [Google Scholar] [CrossRef]
- Chaijenkij, K.; Arirachakaran, A.; Kongtharvonskul, J. Clinical outcomes after internal fixation, arthroplasty and resection for treatment of comminuted radial head fractures: A systematic review and network meta-analysis. Musculoskelet. Surg. 2021, 105, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Kupperman, E.S.; Kupperman, A.I.; Mitchell, S.A. Treatment of Radial Head Fractures and Need for Revision Procedures at 1 and 2 Years. J. Hand Surg. Am. 2017, 43, 241–247. [Google Scholar] [CrossRef]
- Zwingmann, J.; Welzel, M.; Dovi-Akue, D.; Schmal, H.; Sudkamp, N.P.; Strohm, P.C. Clinical results after different operative treatment methods of radial head and neck fractures. A systematic review and meta-analysis of clinical outcome. Injury 2013, 44, 1540–1550. [Google Scholar] [CrossRef]
- Schnetzke, M.; Aytac, S.; Deuss, M.; Studier-Fischer, S.; Swartman, B.; Muenzberg, M.; Gruetzner, P.A.; Guehring, T. Radial head prosthesis in complex elbow dislocations: Effect of oversizing and comparison with ORIF. Int. Orthop. 2014, 38, 2295–2301. [Google Scholar] [CrossRef]
- Van Riet, R.P.; van Glabbeek, F.; Neale, P.G.; Bortier, H.; An, K.N.; O’Driscoll, S.W. The noncircular shape of the radial head. J. Hnad Surg. Am. 2003, 28, 972–978. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, K.J.; Nowak, T.E.; Appelmann, P.; Sternstein, W.; Rommens, P.M.; Mueller, L.P. Screw fixation of radial head fractures: Compression screw versus lag screw—A biomechanical comparison. Injury Int. J. Care Inj. 2010, 41, 1015–1019. [Google Scholar] [CrossRef]
- Morrey, B.F.; Chao, E.Y.; Hui, F.C. Biomechanical study of the elbow following excision of the radial head. J. Bone Joint Surg. Am. 1979, 61, 63–68. [Google Scholar] [CrossRef]
- Rymaszewski, L.A.; Mackay, I.; Amis, A.A.; Miller, J.H. Long-term effects of excision of the radial head in rheumatoid arthritis. J. Bone Joint Surg. Br. 1984, 66, 109–113. [Google Scholar] [CrossRef]
- Rhyou, I.H.; Kim, K.C.; Kim, K.W.; Lee, J.H.; Kim, S.Y. Collateral ligament injury in the displaced radial head and neck fracture: Correlation with fracture morphology and management strategy to the torn ulnar collateral ligament. J. Shoulder Bone Surg. 2013, 22, 261–267. [Google Scholar] [CrossRef]
- van Riet, R.P.; Morrey, B.F.; O’Driscoll, S.W.; Van Glabbeek, F. Associated Injuries Complicating Radial Head Fractures. A Demographic Study. Clin. Orthop. Rel Res. 2005, 441, 351–355. [Google Scholar] [CrossRef] [PubMed]
- Kaas, L.; Turkenburg, J.L.; van Riet, R.P.; Vroemen, P.A.; Eygendaal, D. Magnetic resonance imaging findings in 46 elbows with a radial head fracture. Acta Ortoped 2010, 81, 373–376. [Google Scholar] [CrossRef] [PubMed]
- Itamura, J.; Roidis, N.; Mirzayan, R.; Vaishnav, S.; Learch, T.; Shean, C. Radial head fractures: MRI evaluation of associated injuries. J. Shoulder Elbow Surg. 2005, 14, 421–424. [Google Scholar] [CrossRef]
- Harbrecht, A.; Hackl, M.; Leschinger, T.; Wegmann, K.; Seybold, D.; Müller, L.P. Radial head fractures with interposed capitellar cartilage fragment-hindrance to bone healing—A case series. Arch. Orthop. Trauma. Surg. 2021, 141, 1615–1624. [Google Scholar] [CrossRef]
- Jakobi, T.; Krieg, I.; Gramlich, Y.; Sauter, M.; Schnetz, M.; Hoffmann, R.; Klug, A. The outcomes of surgical treatment of complex radial head fractures. Bone Jt. J 2024, 106, 1158–1164. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).