Computer-Assisted Protocol-Adherent Blood Lipid Evaluation in Vascular Outpatients (CAPABLE-Vascular)
Abstract
1. Introduction
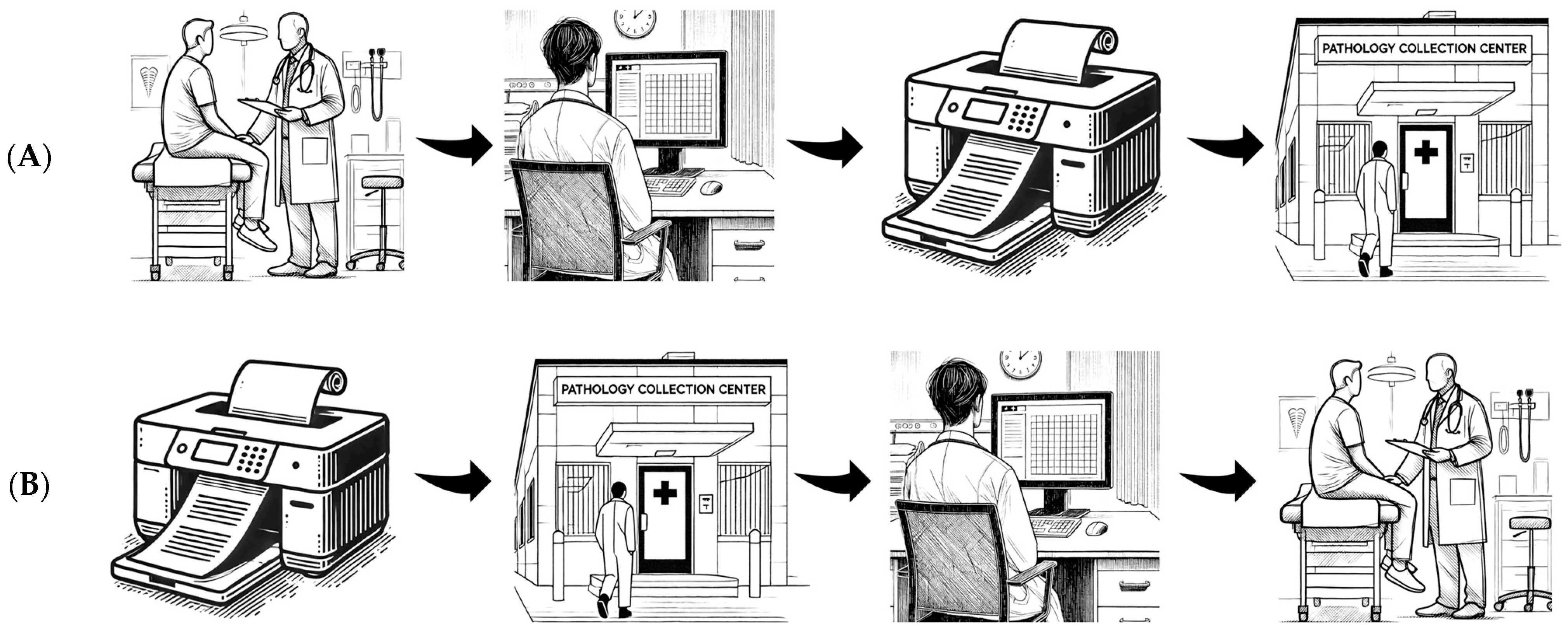
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lee, C.; Columbo, J.A.; Stone, D.H.; Creager, M.A.; Henkin, S. Preoperative evaluation and perioperative management of patients undergoing major vascular surgery. Vasc. Med. 2022, 27, 496–512. [Google Scholar] [CrossRef] [PubMed]
- Strauss, S.A.; Kobewka, D.; Vishnyakova, E. Optimizing Risk Factor Management and Referral Patterns to the Vascular Risk Factor Clinic for Vascular Surgery Patients: A Quality Improvement Initiative. J. Vasc. Surg. 2020, 72, e249. [Google Scholar] [CrossRef]
- Islam, S.M.S.; Siopis, G.; Sood, S.; Uddin, R.; Tegegne, T.; Porter, J.; Dunstan, D.W.; Colagiuri, S.; Zimmet, P.; George, E.S.; et al. The burden of type 2 diabetes in Australia during the period 1990–2019: Findings from the global burden of disease study. Diabetes Res. Clin. Pract. 2023, 199, 110631. [Google Scholar] [CrossRef] [PubMed]
- Faselis, C.; Katsimardou, A.; Imprialos, K.; Deligkaris, P.; Kallistratos, M.; Dimitriadis, K. Microvascular Complications of Type 2 Diabetes Mellitus. Curr. Vasc. Pharmacol. 2020, 18, 117–124. [Google Scholar] [CrossRef]
- Aikaeli, F.; Njim, T.; Gissing, S.; Moyo, F.; Alam, U.; Mfinanga, S.G.; Okebe, J.; Ramaiya, K.; Webb, E.L.; Jaffar, S.; et al. Prevalence of microvascular and macrovascular complications of diabetes in newly diagnosed type 2 diabetes in low-and-middle-income countries: A systematic review and meta-analysis. PLOS Glob. Public. Health 2022, 2, e0000599. [Google Scholar] [CrossRef]
- Health, A.I.o. Welfare. In Diabetes: Australian Facts; AIHW: Canberra, Australia, 2024. [Google Scholar]
- Hossain, M.J.; Al-Mamun, M.; Islam, M.R. Diabetes mellitus, the fastest growing global public health concern: Early detection should be focused. Health Sci. Rep. 2024, 7, e2004. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.; Refaat, M.; Mohammedi, K.; Jayyousi, A.; Al Suwaidi, J.; Abi Khalil, C. Macrovascular Complications in Patients with Diabetes and Prediabetes. Biomed. Res. Int. 2017, 2017, 7839101. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.V.; Shaw, L.; Grant, M. Inflammation in the pathogenesis of microvascular complications in diabetes. Front. Endocrinol. 2012, 3, 170. [Google Scholar] [CrossRef]
- Singareddy, S.; Sn, V.P.; Jaramillo, A.P.; Yasir, M.; Iyer, N.; Hussein, S.; Nath, T.S. Artificial Intelligence and Its Role in the Management of Chronic Medical Conditions: A Systematic Review. Cureus 2023, 15, e46066. [Google Scholar] [CrossRef] [PubMed]
- Satheakeerthy, S.; Stretton, B.; Booth, A.E.C.; Howson, S.; Evans, S.; Kovoor, J.; McNeil, K.; Hopkins, A.; Zeitz, K.; Leslie, A.; et al. Push or pull? Digital notification platform implementation reduces dysglycaemia. Intern. Med. J. 2024, 54, 1753–1756. [Google Scholar] [CrossRef] [PubMed]
- Satheakeerthy, S.; Booth, A.E.; Chan, W.O.; Moloney, B.; Farnan, A.; Gluck, S.; Rao, N.; Gilbert, T.; Bacchi, S. Rule-based clinician-developed programmes can facilitate haemodialysis clinical workflows. Intern. Med. J. 2024, 54, 2057–2060. [Google Scholar] [CrossRef] [PubMed]
- Teo, M.; Stretton, B.; Booth, A.E.C.; Satheakeerthy, S.; Howson, S.; Evans, S.; Kovoor, J.; Fu, S.; McNeil, K.; Menz, B.; et al. Medication shortage behaviour change with multidisciplinary clinician-designed digital notification intervention. Int. J. Pharm. Pr. 2024, 33, 124–126. [Google Scholar] [CrossRef] [PubMed]
- Squires, E.; Bacchi, S.; Maddison, J. We need to chat about artificial intelligence. Med. J. Aust. 2023, 219, 394. [Google Scholar] [CrossRef]
- Bacchi, S.; Kovoor, J.; Gupta, A.; Tan, S.; Sherbon, T.; Bersten, A.; O’Callaghan, P.G.; Chan, W.O. Improving health care efficiency one click at a time. Intern. Med. J. 2023, 53, 1261–1264. [Google Scholar] [CrossRef] [PubMed]
- Wiseman, T.J.; Tan, S.; Stretton, B.; Kovoor, J.; Gupta, A.; Fabian, J.; Chan, W.O.; Malycha, J.; Gluck, S.; Gilbert, T.; et al. Double or nothing: Costs of duplicate haematinic ordering in medical inpatients. Transfus. Med. 2023, 33, 423–425. [Google Scholar] [CrossRef]
- Tan, S.; Vuong, A.; Kovoor, J.; Gupta, A.; Chan, W.; Umapathysivam, M.; Wong, B.; Gluck, S.; Gilbert, T.; Bacchi, S. Beware of little expenses: Low-value endocrinological blood tests in geriatric medical inpatients. Australas. J. Ageing 2024, 43, 211–214. [Google Scholar] [CrossRef] [PubMed]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA Guideline on the Management of Blood Cholesterol: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation 2019, 139, e1082–e1143. [Google Scholar] [CrossRef] [PubMed]
- Imai, C.; Li, L.; Hardie, R.-A.; Georgiou, A. Adherence to guideline-recommended HbA1c testing frequency and better outcomes in patients with type 2 diabetes: A 5-year retrospective cohort study in Australian general practice. BMJ Qual. Saf. 2021, 30, 706–714. [Google Scholar] [CrossRef]
- d’Emden, M.C.; Shaw, J.E.; Jones, G.R.; Cheung, N.W. Guidance concerning the use of glycated haemoglobin (HbA1c) for the diagnosis of diabetes mellitus. Med. J. Aust. 2015, 203, 89–90. [Google Scholar] [CrossRef]
- Mant, J. Process versus outcome indicators in the assessment of quality of health care. Int. J. Qual. Health Care 2001, 13, 475–480. [Google Scholar] [CrossRef] [PubMed]
- Sonaglioni, A.; Rigamonti, E.; Nicolosi, G.L.; Lombardo, M. Appropriate use criteria implementation with modified Haller index for predicting stress echocardiographic results and outcome in a population of patients with suspected coronary artery disease. Int. J. Cardiovasc. Imaging 2021, 37, 2917–2930. [Google Scholar] [CrossRef] [PubMed]
- Gertz, Z.M.; O’Donnell, W.; Raina, A.; Litwack, A.J.; Balderston, J.R.; Goldberg, L.R. Application of appropriate use criteria to cardiac stress testing in the hospital setting: Limitations of the criteria and areas for improved practice. Clin. Cardiol. 2015, 38, 8–12. [Google Scholar] [CrossRef]
- Gandhi, S.; Ho, E.C.; Ong, G.; Zahrani, M.; Lu, J.; Leong-Poi, H.; Edwards, J.; Bhatia, S.R.S.; Levitt, K.; Chow, C.M.; et al. A Physician Education Tool to Improve Appropriate Use Criteria for Stress Echocardiography: Long-Term Follow-Up of a Single-Center Study. J. Am. Soc. Echocardiogr. 2019, 32, 1255–1257. [Google Scholar] [CrossRef] [PubMed]
- Gibbons, R.J.; Askew, J.W.; Hodge, D.; Kaping, B.; Carryer, D.J.; Miller, T. Appropriate use criteria for stress single-photon emission computed tomography sestamibi studies: A quality improvement project. Circulation 2011, 123, 499–503. [Google Scholar] [CrossRef] [PubMed]
- McCully, R.B.; Pellikka, P.A.; Hodge, D.O.; Araoz, P.A.; Miller, T.D.; Gibbons, R.J. Applicability of appropriateness criteria for stress imaging: Similarities and differences between stress echocardiography and single-photon emission computed tomography myocardial perfusion imaging criteria. Circ. Cardiovasc. Imaging 2009, 2, 213–218. [Google Scholar] [CrossRef]
- Willens, H.J.; Nelson, K.; Hendel, R.C. Appropriate use criteria for stress echocardiography: Impact of updated criteria on appropriateness ratings, correlation with pre-authorization guidelines, and effect of temporal trends and an educational initiative on utilization. JACC Cardiovasc. Imaging 2013, 6, 297–309. [Google Scholar] [CrossRef]
- Rajeswaran, D.; Saunder, A.; Raymond, S. Post-operative risk factor control following internal carotid artery intervention. ANZ J. Surg. 2011, 81, 817–821. [Google Scholar] [CrossRef]
- Tacker, D.H.; Topardo, J.; Mahaffey, C.; Perrotta, P.L. Workflow analysis comparing manual and automated specimen processing for mass spectrometry-based vitamin D testing. Lab. Med. 2014, 45, 361–367. [Google Scholar] [CrossRef]
- Holzmüller-Laue, S.; Göde, B.; Fleischer, H.; Thurow, K. Improved compliance by BPM-driven workflow automation. J. Lab. Autom. 2014, 19, 528–545. [Google Scholar] [CrossRef] [PubMed]
- Thomas, H.; Best, M.; Mitchell, G. Whole-person care in general practice: The doctor–patient relationship. Aust. J. Gen. Pract. 2020, 49, 139–144. [Google Scholar] [CrossRef] [PubMed]
- Zayas-Cabán, T.; Haque, S.N.; Kemper, N. Identifying Opportunities for Workflow Automation in Health Care: Lessons Learned from Other Industries. Appl. Clin. Inf. 2021, 12, 686–697. [Google Scholar] [CrossRef] [PubMed]
- Pietris, J.; Bacchi, S.; Tan, Y.; Kovoor, J.; Gupta, A.; Chan, W. Safety always: The challenges of cloud computing in medical practice and ophthalmology. Eye 2023, 37, 2436–2437. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.M.; Macri, C.; Bacchi, S.; Chan, W. External generalisability in implementation studies of technological interventions. Clin. Exp. Ophthalmol. 2023, 51, 499–500. [Google Scholar] [CrossRef]
- Tso, G.J.; Tu, S.W.; Oshiro, C.; Martins, S.; Ashcraft, M.; Yuen, K.W.; Wang, D.; Robinson, A.; Heidenreich, P.A.; Goldstein, M.K. Automating Guidelines for Clinical Decision Support: Knowledge Engineering and Implementation. AMIA Annu. Symp. Proc. 2016, 2016, 1189–1198. [Google Scholar] [PubMed]
- O’Connor, S.D.; Khorasani, R.; Pochebit, S.M.; Lacson, R.; Andriole, K.P.; Dalal, A.K. Semiautomated System for Nonurgent, Clinically Significant Pathology Results. Appl. Clin. Inf. 2018, 9, 411–421. [Google Scholar] [CrossRef] [PubMed]
- Maleki Varnosfaderani, S.; Forouzanfar, M. The Role of AI in Hospitals and Clinics: Transforming Healthcare in the 21st Century. Bioengineering 2024, 11, 337. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Thurston, B.; Satheakeerthy, S.; Hains, L.; Booth, A.E.C.; Gao, C.; Bellinge, J.; Stretton, B.; Psaltis, P.; Bacchi, S. Computer-Assisted Protocol-Adherent Blood Lipid Evaluation in Vascular Outpatients (CAPABLE-Vascular). J. Clin. Med. 2025, 14, 1321. https://doi.org/10.3390/jcm14041321
Thurston B, Satheakeerthy S, Hains L, Booth AEC, Gao C, Bellinge J, Stretton B, Psaltis P, Bacchi S. Computer-Assisted Protocol-Adherent Blood Lipid Evaluation in Vascular Outpatients (CAPABLE-Vascular). Journal of Clinical Medicine. 2025; 14(4):1321. https://doi.org/10.3390/jcm14041321
Chicago/Turabian StyleThurston, Benjamin, Shrirajh Satheakeerthy, Lewis Hains, Andrew E. C. Booth, Christina Gao, Jamie Bellinge, Brandon Stretton, Peter Psaltis, and Stephen Bacchi. 2025. "Computer-Assisted Protocol-Adherent Blood Lipid Evaluation in Vascular Outpatients (CAPABLE-Vascular)" Journal of Clinical Medicine 14, no. 4: 1321. https://doi.org/10.3390/jcm14041321
APA StyleThurston, B., Satheakeerthy, S., Hains, L., Booth, A. E. C., Gao, C., Bellinge, J., Stretton, B., Psaltis, P., & Bacchi, S. (2025). Computer-Assisted Protocol-Adherent Blood Lipid Evaluation in Vascular Outpatients (CAPABLE-Vascular). Journal of Clinical Medicine, 14(4), 1321. https://doi.org/10.3390/jcm14041321







