Impact of Admission Ward on Long-Term Outcomes in Patients with Non-ST Elevation Myocardial Infarction
Abstract
1. Background
2. Methods
3. Statistical Analysis
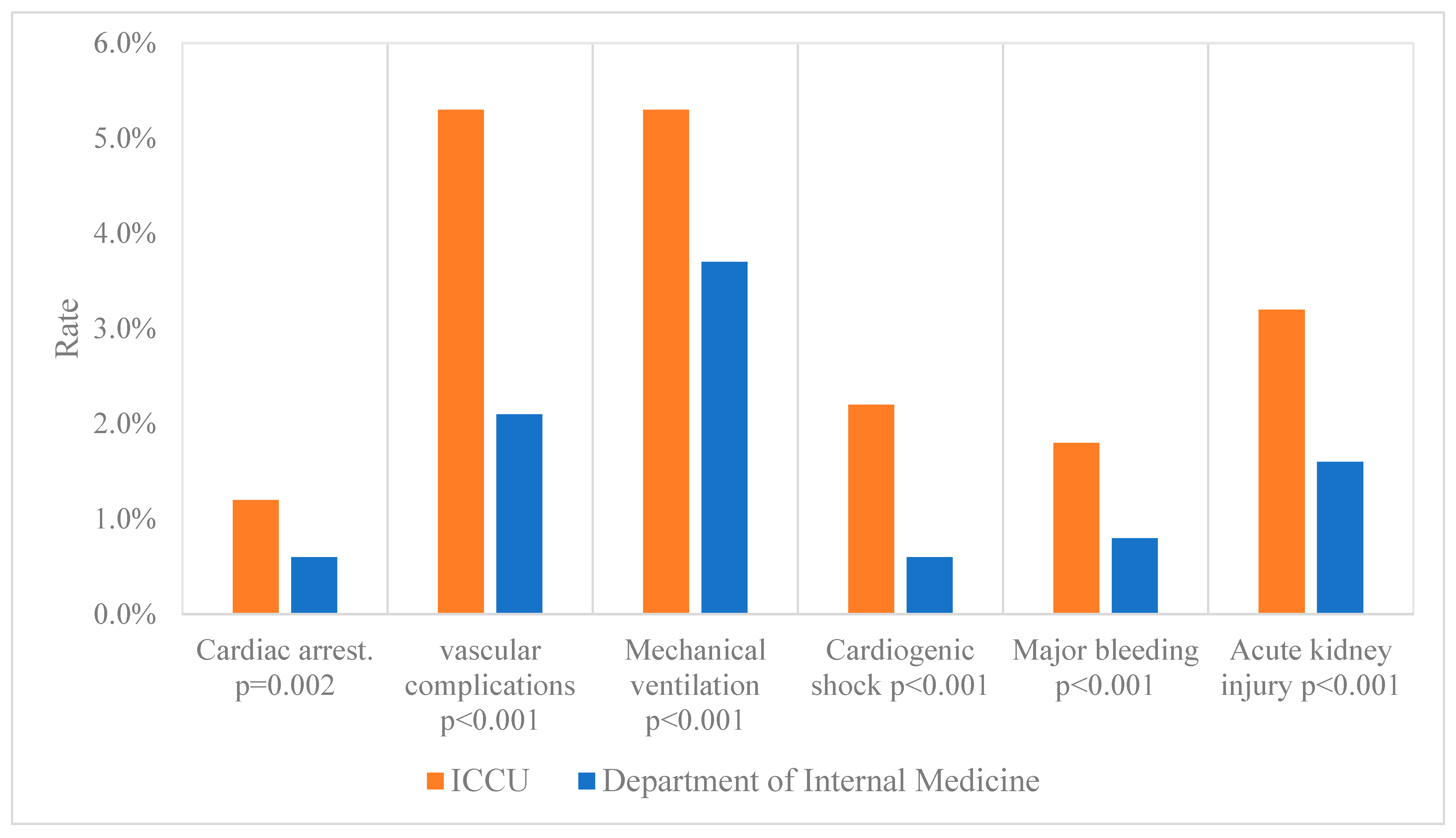
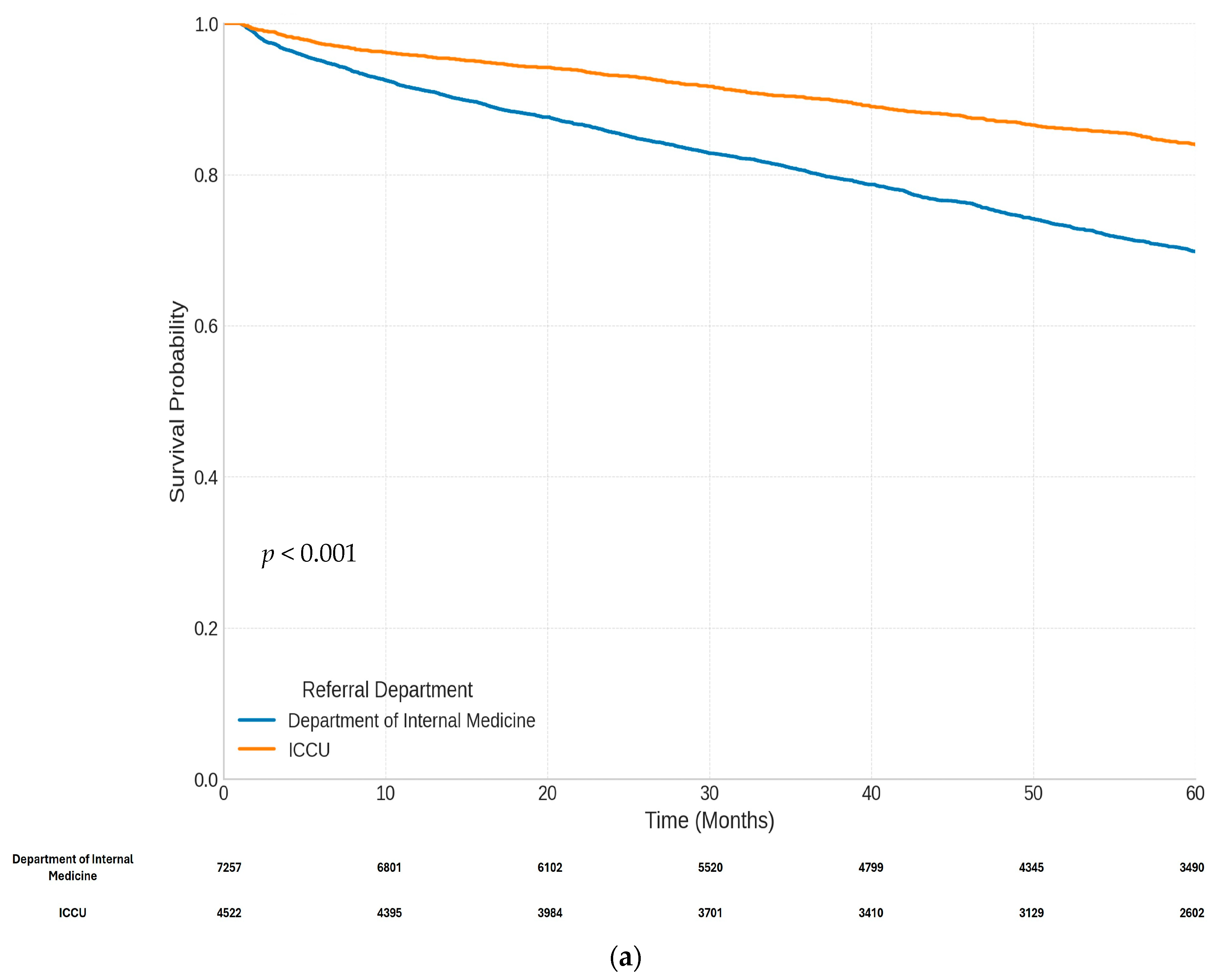
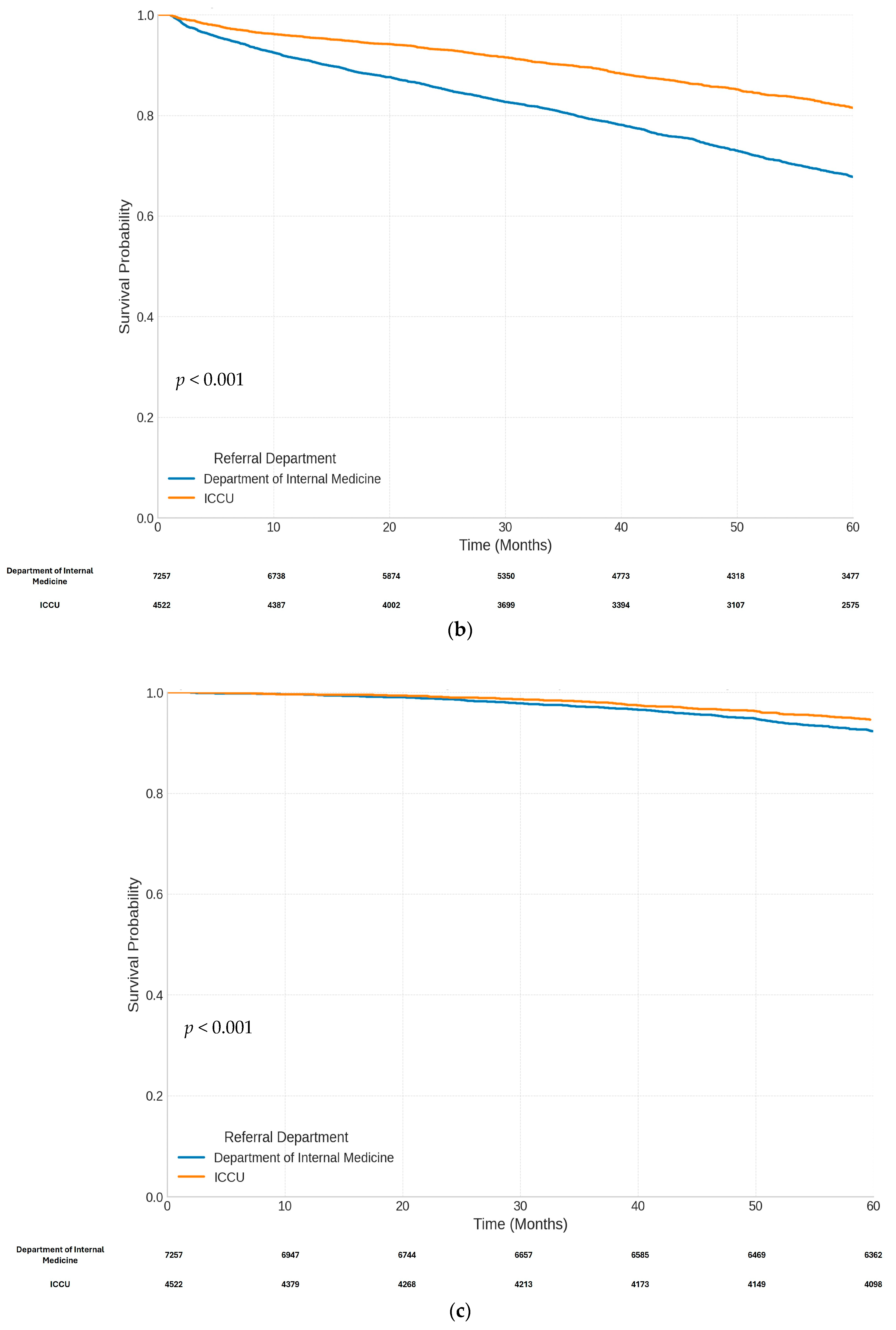
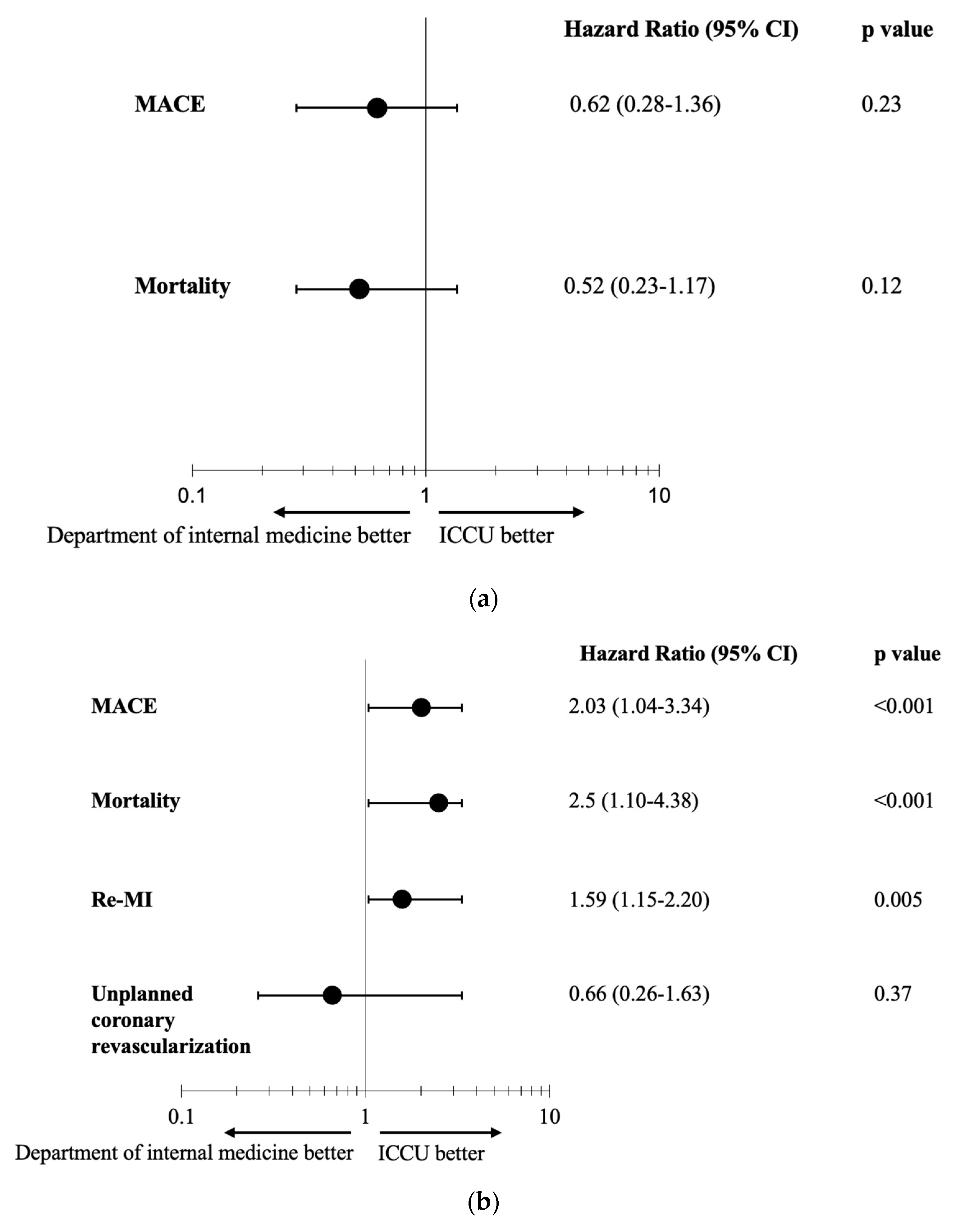
4. Results
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Montalescot, G.; Dallongeville, J.; Van Belle, E.; Rouanet, S.; Baulac, C.; Degrandsart, A.; Vicaut, E. STEMI and NSTEMI: Are they so different? 1 year outcomes in acute myocardial infarction as defined by the ESC/ACC definition (the OPERA registry). Eur. Heart J. 2007, 28, 1409–1417. [Google Scholar] [CrossRef] [PubMed]
- Byrne, R.A.; Rossello, X.; Coughlan, J.J.; Barbato, E.; Berry, C.; Chieffo, A.; Claeys, M.J.; Dan, G.A.; Dweck, M.R.; Galbraith, M.; et al. 2023 ESC Guidelines for the management of acute coronary syndromes. Eur. Heart J. 2023, 44, 3720–3826. [Google Scholar] [CrossRef] [PubMed]
- Amsterdam, E.A.; Wenger, N.K.; Brindis, R.G.; Casey, D.E.; Ganiats, T.G.; Holmes, D.R.; Jaffe, A.S.; Jneid, H.; Kelly, R.F.; Kontos, M.C.; et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J. Am. Coll. Cardiol. 2014, 64, e139–e228. [Google Scholar] [CrossRef] [PubMed]
- Cramer, H.; Hughes, J.; Johnson, R.; Evans, M.; Deaton, C.; Timmis, A.; Hemingway, H.; Feder, G.; Featherstone, K. ‘Who does this patient belong to?’ Boundary work and the re/making of (NSTEMI) heart attack patients. Sociol. Health Illn. 2018, 40, 1404–1429. [Google Scholar] [CrossRef] [PubMed]
- Goodman, D.C.; Goodman, A.A. Medical care epidemiology and unwarranted variation: The Israeli case. Isr. J. Health Policy Res. 2017, 6, 9. [Google Scholar] [CrossRef] [PubMed]
- Rosen, B.; Waitzberg, R.; Merkur, S. Israel: Health System Review. Health Syst. Transit. 2015, 17, 1–212. [Google Scholar] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D. Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth Universal Definition of Myocardial Infarction (2018). J. Am. Coll. Cardiol. 2018, 72, 2231–2264. [Google Scholar] [PubMed]
- Darling, C.E.; Fisher, K.A.; McManus, D.D.; Coles, A.H.; Spencer, F.A.; Gore, J.M.; Goldberg, R.J. Survival after hospital discharge for ST-segment elevation and non-ST-segment elevation acute myocardial infarction: A population-based study. Clin. Epidemiol. 2013, 5, 229–236. [Google Scholar] [PubMed]
- Alfredsson, J.; Sederholm-Lawesson, S.; Stenestrand, U.; Swahn, E. Although women are less likely to be admitted to coronary care units, they are treated equally to men and have better outcome. A prospective cohort study in patients with non ST-elevation acute coronary syndromes. Acute Card. Care 2009, 11, 173–180. [Google Scholar] [CrossRef] [PubMed]
- Stenestrand, U.; Wijkman, M.; Fredrikson, M.; Nystrom, F.H. Association between admission supine systolic blood pressure and 1-year mortality in patients admitted to the intensive care unit for acute chest pain. JAMA 2010, 303, 1167–1172. [Google Scholar] [CrossRef] [PubMed]
- Boersma, E.; Pieper, K.S.; Steyerberg, E.W.; Wilcox, R.G.; Chang, W.-C.; Lee, K.L.; Akkerhuis, K.M.; Harrington, R.A.; Deckers, J.W.; Armstrong, P.W.; et al. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUIT Investigators. Circulation 2000, 101, 2557–2567. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, P.W.; Fu, Y.; Chang, W.C.; Topol, E.J.; Granger, C.B.; Betriu, A.; Van de Werf, F.; Lee, K.L.; Califf, R.M. Acute coronary syndromes in the GUSTO-IIb trial: Prognostic insights and impact of recurrent ischemia. Circulation 1998, 98, 1860–1868. [Google Scholar] [CrossRef] [PubMed]
- Jollis, J.G.; DeLong, E.R.; Peterson, E.D.; Muhlbaier, L.H.; Fortin, D.F.; Califf, R.M.; Mark, D.B. Outcome of acute myocardial infarction according to the specialty of the admitting physician. N. Engl. J. Med. 1996, 335, 1880–1887. [Google Scholar] [CrossRef] [PubMed]
- Moledina, S.M.; Shoaib, A.; Graham, M.M.; Biondi-Zoccai, G.; Van Spall, H.G.C.; Kontopantelis, E.; Rashid, M.; Aktaa, S.; Gale, C.P.; Weston, C.; et al. Association of admitting physician specialty and care quality and outcomes in non-ST-segment elevation myocardial infarction (NSTEMI): Insights from a national registry. Eur. Heart J. Qual. Care Clin. Outcomes 2021, 8, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Birkhead, J.S.; Weston, C.; Lowe, D. Impact of specialty of admitting physician and type of hospital on care and outcome for myocardial infarction in England and Wales during 2004-5: Observational study. BMJ 2006, 332, 1306–1311. [Google Scholar] [CrossRef] [PubMed]
- Ayanian, J.Z.; Guadagnoli, E.; McNeil, B.J.; Cleary, P.D. Treatment and outcomes of acute myocardial infarction among patients of cardiologists and generalist physicians. Arch. Intern. Med. 1997, 157, 2570–2576. [Google Scholar] [CrossRef] [PubMed]
- Go, A.S.; Rao, R.K.; Dauterman, K.W.; Massie, B.M. A systematic review of the effects of physician specialty on the treatment of coronary disease and heart failure in the United States. Am. J. Med. 2000, 108, 259–261. [Google Scholar] [CrossRef] [PubMed]
- Moledina, S.M.; Shoaib, A.; Sun, L.Y.; Myint, P.K.; Kotronias, R.A.; Shah, B.N.; Gale, C.P.; Quan, H.; Bagur, R.; Mamas, M.A. Impact of the admitting ward on care quality and outcomes in non-ST-segment elevation myocardial infarction: Insights from a national registry. Eur. Heart J. Qual. Care Clin. Outcomes 2022, 8, 681–691. [Google Scholar] [CrossRef] [PubMed]
- Case, B.C.; Yerasi, C.; Wang, Y.; Forrestal, B.J.; Hahm, J.; Dolman, S.; Weintraub, W.S.; Waksman, R. Admissions Rate and Timing of Revascularization in the United States in Patients with Non-ST-Elevation Myocardial Infarction. Am. J. Cardiol. 2020, 134, 24–31. [Google Scholar] [CrossRef] [PubMed]
- Everett, C.C.; Fox, K.A.; Reynolds, C.; Fernandez, C.; Sharples, L.; Stocken, D.D.; Carruthers, K.; Hemingway, H.; Yan, A.T.; Goodman, S.G.; et al. Evaluation of the impact of the GRACE risk score on the management and outcome of patients hospitalised with non-ST elevation acute coronary syndrome in the UK: Protocol of the UKGRIS cluster-randomised registry-based trial. BMJ Open 2019, 9, e032165. [Google Scholar] [CrossRef] [PubMed]

| Department of Internal Medicine | ICCU | p Value | |
|---|---|---|---|
| n | 7257 | 4522 | |
| Age, years (mean) [±SD] | 67.6 (±12.1) | 62.7 (±12.9) | <0.001 |
| Gender (male) | 5013 (69.1%) | 3532 (78.1%) | <0.001 |
| BMI (kg/m2) (mean) [±SD] | 29.3 (±9.40) | 28.7 (±9.16) | <0.001 |
| Current smokers | 3265 (45.0%) | 2533 (56.0%) | <0.001 |
| Dyslipidemia | 5622 (77.5%) | 3538 (78.2%) | 0.34 |
| Hypertension | 4767 (65.7%) | 2495 (55.2%) | <0.001 |
| Diabetes mellitus | 3525 (48.6%) | 1772 (39.2%) | <0.001 |
| HBA1C (%) (mean) [±SD] | 7.04 (±1.85) | 6.68 (±1.73) | <0.001 |
| Atrial fibrillation | 1888 (26.0%) | 961 (21.3%) | <0.001 |
| PVD | 625 (8.6%) | 307 (6.8%) | <0.001 |
| Dialysis | 261 (3.6%) | 110 (2.4%) | <0.001 |
| COPD | 204 (2.8%) | 72 (1.6%) | <0.001 |
| Prior to admission | |||
| MI | 1374 (18.9%) | 666 (14.7%) | <0.001 |
| CABG | 1094 (15.1%) | 485 (10.7%) | <0.001 |
| PCI | 2663 (36.7%) | 1322 (29.2%) | <0.001 |
| Characteristics on admission | |||
| Pulse (bpm) | 71.3 (±14.9) | 72.0 (±13.8) | <0.001 |
| SBP (mmHg) | 135 (±23.7) | 127 (±22.8) | <0.001 |
| SBP < 90 (mmHg) | 94 (1.3%) | 145 (3.2%) | <0.001 |
| Creatinine (mg/dL) | 1.28 (±1.34) | 1.11 (±1.04) | <0.001 |
| Hemoglobin (g/dL) | 12.8 (±2.03) | 13.4 (±2.00) | <0.001 |
| WBC (103/uL) | 8.90 (±3.94) | 10.2 (±4.27) | <0.001 |
| Troponin (max/ULN) | 5.59 (±4.55) | 7.10 (±4.92) | <0.001 |
| Reduced LV function | 1230 (16.9%) | 841 (18.6%) | 0.024 |
| LVEF (%) | 56.1 (±16.3) | 56.7 (±15.2) | 0.608 |
| Department of Internal Medicine | ICCU | p Value | |
|---|---|---|---|
| n | 7257 | 4522 | |
| Interventional treatment characteristics | |||
| Time To PCI (hours) | <0.001 | ||
| <24 | 363 (5.0%) | 1175 (26.0%) | |
| 24–72 | 1610 (22.2%) | 2333 (51.6%) | |
| >72 | 5284 (72.8%) | 1014 (22.4%) | |
| Therapeutic PCI | 6391 (88.1%) | 3891 (86.0%) | 0.002 |
| CABG | 866 (11.9%) | 631 (14.0%) | 0.002 |
| Thrombolytic therapy | 81 (1.1%) | 298 (6.6%) | <0.001 |
| Procedural findings and modalities | |||
| Access site | <0.001 | ||
| Femoral | 1598 (22.0%) | 830 (18.4%) | |
| Radial | 5480 (75.5%) | 3571 (79.0%) | |
| Other | 179 (2.5%) | 121 (2.7%) | |
| LM stenosis > 50% | 892 (12.3%) | 507 (11.2%) | 0.083 |
| Multi vessels disease | 3000 (41.3%) | 1897 (42.0%) | 0.525 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bartal, C.; Hilu, R.; Alsana, H.; Peles, I.; Tsaban, G.; Merkin, M.; Rosenstein, G.; El-Nasasra, A.; Shmueli, H.; Abramowitz, Y.; et al. Impact of Admission Ward on Long-Term Outcomes in Patients with Non-ST Elevation Myocardial Infarction. J. Clin. Med. 2025, 14, 1284. https://doi.org/10.3390/jcm14041284
Bartal C, Hilu R, Alsana H, Peles I, Tsaban G, Merkin M, Rosenstein G, El-Nasasra A, Shmueli H, Abramowitz Y, et al. Impact of Admission Ward on Long-Term Outcomes in Patients with Non-ST Elevation Myocardial Infarction. Journal of Clinical Medicine. 2025; 14(4):1284. https://doi.org/10.3390/jcm14041284
Chicago/Turabian StyleBartal, Carmi, Ranin Hilu, Hadel Alsana, Ido Peles, Gal Tsaban, Miri Merkin, Gabriel Rosenstein, Aref El-Nasasra, Hezzy Shmueli, Yigal Abramowitz, and et al. 2025. "Impact of Admission Ward on Long-Term Outcomes in Patients with Non-ST Elevation Myocardial Infarction" Journal of Clinical Medicine 14, no. 4: 1284. https://doi.org/10.3390/jcm14041284
APA StyleBartal, C., Hilu, R., Alsana, H., Peles, I., Tsaban, G., Merkin, M., Rosenstein, G., El-Nasasra, A., Shmueli, H., Abramowitz, Y., Cafri, C., Zagher, D., & Koifman, E. (2025). Impact of Admission Ward on Long-Term Outcomes in Patients with Non-ST Elevation Myocardial Infarction. Journal of Clinical Medicine, 14(4), 1284. https://doi.org/10.3390/jcm14041284







