Preliminary Quadriceps Muscle Contraction in the Early Rehabilitation of Hip and Knee Arthroplasty
Abstract
1. Introduction
Objective
2. Materials and Methods
2.1. Study Setting
- -
- Department of Physical Medicine and Rehabilitation, University Hospital “Aleksandrovska”, Sofia, Bulgaria;
- -
- Department of Physical Medicine and Rehabilitation and Department of Orthopedics and Traumatology, University Hospital “St. Anna,” Sofia, Bulgaria.
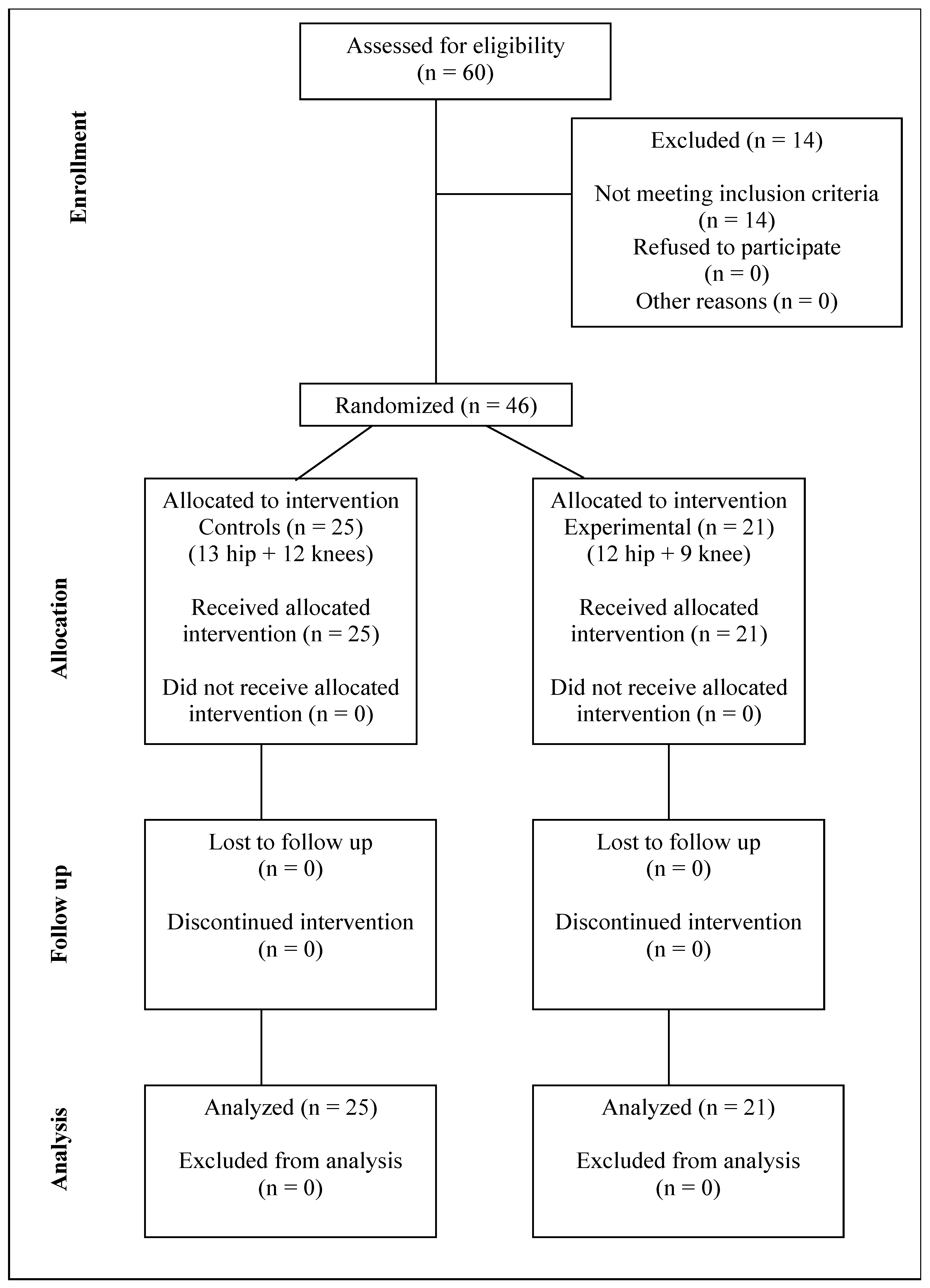
2.2. Participants
2.3. Groups
- Control group (n = 25; 13 hip, 12 knee): standard postoperative advice.
- Experimental group (n = 21; 12 hip, 9 knee): standard advice plus preliminary quadriceps contraction.
2.4. Inclusion Criteria
- Age >18 years.
- Clinically and radiographically confirmed osteoarthrosis of the hip or knee, indicated for arthroplasty.
- Ability to ambulate independently or with an assistive device.
2.5. Exclusion Criteria
- Fractures.
- Revision arthroplasty.
- Severe comorbidities (pulmonary, cardiac, metabolic) limiting physical activity.
- Postoperative complications preventing discharge after day 7.
- Advanced osteoarthritis severely limiting rehabilitation participation.
- Aphasia, dementia, or psychiatric illness impairing participation.
- Blindness or illiteracy.
2.6. Interventions
2.7. Additional Advice (Experimental Group)
2.8. Outcome Measures
2.8.1. Primary Outcome
2.8.2. Secondary Outcomes
2.9. Sample Size and Power Analysis
- ANOVA—Repeated Measures:
- α = 0.05, Power = 0.95, Groups = 4, Measurements = 4, Corr = 0.5
- Required n = 36, Achieved power = 0.951
- Linear Multiple Regression:
- α = 0.05, Power = 0.95, R2 deviation = 0.1578
- Required n = 46, Achieved power = 0.950
2.10. Follow-Up
2.11. Statistical Analysis
3. Results
4. Discussion
Study Limitations
- -
- Small sample for drawing strong generalizable conclusions;
- -
- Short follow-up (30 days);
- -
- Relatively subjective outcome measures;
- -
- Self-reported adherence;
- -
- Lack of evaluation of neuromuscular deficits such as arthrogenic muscle inhibition (AMI) [34,35,36], hyperexcitability of flexion withdrawal reflexes [7], altered hamstring-to-quadriceps ratios [37,38], impaired force control, voluntary activation deficits, changes in cortical and spinal excitability, reflex modulation, torque variability [37,38], or electromechanical delay [37,38]. Further studies are needed to assess their role, including larger cohorts, longer follow-ups, objective monitoring and adherence verification.
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| VAS | Visual analog scale |
| MMT | Manual muscle testing |
| ROM | Range of motion |
| Pre-Contr | preliminary contraction |
| BMI | body mass index |
| AMI | arthrogenic muscle inhibition |
| FWRs | hyperexcitability of flexion withdrawal reflexes |
| CI | confidence interval |
References
- Glasser, J.L.; Patel, S.A.; Li, N.Y.; Patel, R.A.; Daniels, A.H.; Antoci, V. Understanding health economics in joint replacement surgery. Orthopedics 2022, 45, e174–e182. [Google Scholar] [CrossRef]
- Marsh, M.; Newman, S. Trends and developments in hip and knee arthroplasty technology. J. Rehabil. Assist. Technol. Eng. 2021, 8, 2055668320952043. [Google Scholar] [CrossRef]
- Romanini, E.; Schettini, I.; Torre, M.; Venosa, M.; Tarantino, A.; Calvisi, V.; Zanoli, G. The rise of registry-based research: A bibliometric analysis. Acta Orthop. 2021, 92, 628–632. [Google Scholar] [CrossRef]
- Kinov, P. Quality of Life After Hip Replacement Surgery; Sofia: Paris, France, 2022; ISBN 9786197321197. [Google Scholar]
- Katz, J.N.; Arant, K.R.; Loeser, R.F. Diagnosis and treatment of hip and knee osteoarthritis: A review. Jama 2021, 325, 568–578. [Google Scholar] [CrossRef] [PubMed]
- Flick, T.R.; Ross, B.J.; Sherman, W.F. Instability after total hip arthroplasty and the role of advanced and robotic technology. Orthop. Clin. N. Am. 2021, 52, 191–200. [Google Scholar] [CrossRef] [PubMed]
- Courtney, C.A.; Lewek, M.D.; Witte, P.O.; Chmell, S.J.; Hornby, T.G. Heightened flexor withdrawal responses in subjects with knee osteoarthritis. J. Pain 2009, 10, 1242–1249. [Google Scholar] [CrossRef] [PubMed]
- Aleksiev, A. Ten-year follow-up of strengthening versus flexibility exercises with or without abdominal bracing in recurrent low back pain. Spine 2014, 39, 997–1003. [Google Scholar] [CrossRef]
- Aleksiev, A. Prognostic (Self)Treatment of Spine Pain; Amazon Publishing: Seattle, WA, USA, 2024; ISBN 9798873923458. Available online: https://www.amazon.com/dp/B0CRHS9WR3 (accessed on 1 January 2025).
- Aleksiev, A.; Matsanova-Simova, V.; Nikolova-Shopova, S.N.; Dimitrova, V. Ten-year follow-up of preliminary biceps brachial muscle contraction in rehabilitation and prophylaxis of recurrent shoulder pain due to tendon degeneration. Int. J. Adv. Res. 2021, 9, 792–802. [Google Scholar] [CrossRef]
- Aleksiev, A.; Nikolova-Shopova, S.N. Ten-year follow-up of preliminary quadriceps muscle contraction in rehabilitation and prophylaxis of recurrent knee pain due to osteoarthritis. J. Yoga Phys. Ther. Rehabil. 2021, 6, 1–8. [Google Scholar]
- Bonnet, M.; Requin, J.; Stelmach, G.E. Changes in electromyographic responses to muscle stretch, related to the programming of movement parameters. Electroencephalogr. Clin. Neurophysiol. 1991, 81, 135–151. [Google Scholar] [CrossRef]
- Cherif, A.; Zenzeri, J.; Loram, I. What is the contribution of voluntary and reflex processes to sensorimotor control of balance? Front. Bioeng. Biotechnol. 2022, 10, 973716. [Google Scholar] [CrossRef] [PubMed]
- Correa, T.A.; Crossley, K.M.; Kim, H.J.; Pandy, M.G. Contributions of individual muscles to hip joint contact force in normal walking. J. Biomech. 2010, 43, 1618–1622. [Google Scholar] [CrossRef] [PubMed]
- Song, K.; Gaffney, B.M.; Shelburne, K.B.; Pascual-Garrido, C.; Clohisy, J.C.; Harris, M.D. Dysplastic hip anatomy alters muscle moment arm lengths, lines of action, and contributions to joint reaction forces during gait. J. Biomech. 2020, 110, 109968. [Google Scholar] [CrossRef] [PubMed]
- Adouni, M.; Shirazi-Adl, A. Consideration of equilibrium equations at the hip joint alongside those at the knee and ankle joints has mixed effects on knee joint response during gait. J. Biomech. 2013, 46, 619–624. [Google Scholar] [CrossRef]
- Kumar, A.; Foster, T.C. Neurophysiology of old neurons and synapses. In Brain Aging: Models, Methods, and Mechanisms; Riddle, D.R., Ed.; Frontiers in Neuroscience; CRC Press: Boca Raton, FL, USA, 2007; ISBN 9780849338182. [Google Scholar]
- Moore, A.Z.; Caturegli, G.; Metter, E.J.; Makrogiannis, S.; Resnick, S.M.; Harris, T.B.; Ferrucci, L. Difference in muscle quality over the adult life span and biological correlates in the Baltimore Longitudinal Study of Aging. J. Am. Geriatr. Soc. 2014, 62, 230–236. [Google Scholar] [CrossRef]
- Colibazzi, V.; Coladonato, A.; Zanazzo, M.; Romanini, E. Evidence based rehabilitation after hip arthroplasty. Hip Int. 2020, 30 (Suppl. S2), 20–29. [Google Scholar] [CrossRef]
- Papalia, R.; Campi, S.; Vorini, F.; Zampogna, B.; Vasta, S.; Papalia, G.; Fossati, C.; Torre, G.; Denaro, V. The role of physical activity and rehabilitation following hip and knee arthroplasty in the elderly. J. Clin. Med. 2020, 9, 1401. [Google Scholar] [CrossRef]
- Temfemo, A.; Doutrellot, P.L.; Ahmaidi, S. Early muscular strengthening after total hip arthroplasty: Association of two models of rehabilitation. Ann. Réadapt. Méd. Phys. 2008, 51, 38–45. [Google Scholar] [CrossRef]
- Husby, V.S.; Helgerud, J.; Bjørgen, S.; Husby, O.S.; Benum, P.; Hoff, J. Early maximal strength training is an efficient treatment for patients operated with total hip arthroplasty. Arch. Phys. Med. Rehabil. 2009, 90, 1658–1667. [Google Scholar] [CrossRef]
- Bruyère, O.; Ethgen, O.; Neuprez, A.; Zégels, B.; Gillet, P.; Huskin, J.P.; Reginster, J.Y. Health-related quality of life after total knee or hip replacement for osteoarthritis: A 7-year prospective study. Arch. Orthop. Trauma Surg. 2012, 132, 1583–1587. [Google Scholar] [CrossRef]
- Layton, R.; Messenger, N.; Stewart, T. Characteristics of hip joint reaction forces during a range of activities. Med. Eng. Phys. 2022, 108, 103894. [Google Scholar] [CrossRef]
- Serbest, K.; Cilli, M.; Eldogan, O. Biomechanical effects of daily physical activities on the lower limb. Acta Orthop. Traumatol. Turc. 2015, 49, 85–90. [Google Scholar] [CrossRef]
- Yoshioka, S.; Nagano, A.; Hay, D.C.; Fukashiro, S. Peak hip and knee joint moments during a sit-to-stand movement are invariant to the change of seat height within the range of low to normal seat height. Biomed. Eng. Online 2014, 13, 27. [Google Scholar] [CrossRef] [PubMed]
- Price, D.D.; McGrath, P.A.; Rafii, A.; Buckingham, B. The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983, 17, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Wewers, M.E.; Lowe, N.K. A critical review of visual analogue scales in the measurement of clinical phenomena. Res. Nurs. Health 1990, 13, 227–236. [Google Scholar] [CrossRef] [PubMed]
- Ciesla, N.; Dinglas, V.; Fan, E.; Kho, M.; Kuramoto, J.; Needham, D. Manual muscle testing: A method of measuring extremity muscle strength applied to critically ill patients. J. Vis. Exp. JoVE 2011, 50, 2632. [Google Scholar]
- Clarkson, H. Musculoskeletal Assessment: Joint Motion and Muscle Testing, 3rd ed.; LWW: Philadelphia, PA, USA, 2012; ISBN 9781609138165. [Google Scholar]
- Hough, C.; Lieu, B.; Caldwell, E. Manual muscle strength testing of critically ill patients: Feasibility and interobserver agreement. Crit. Care 2011, 15, R43. [Google Scholar] [CrossRef]
- Medical Advisory Secretariat. Physiotherapy rehabilitation after total knee or hip replacement: An evidence-based analysis. Ont. Health Technol. Assess. Ser. 2005, 5, 1–91. [Google Scholar]
- Wright, A.A.; Ness, B.M.; Donaldson, M. Diagnostic Accuracy of Patient History in the Diagnosis of Hip-Related Pain: A Systematic Review. Arch. Phys. Med. Rehabil. 2021, 102, 2454–2463.e1. [Google Scholar] [CrossRef]
- Norte, G.; Rush, J.; Sherman, D. Arthrogenic muscle inhibition: Best evidence, mechanisms, and theory for treating the unseen in clinical rehabilitation. J. Sport Rehabil. 2022, 31, 717–735. [Google Scholar] [CrossRef]
- Sonnery-Cottet, B.; Hopper, G.P.; Gousopoulos, L.; Vieira, T.D.; Thaunat, M.; Fayard, J.M.; Freychet, B.; Ouanezar, H.; Cavaignac, E.; Saithna, A. Arthrogenic muscle inhibition following knee injury or surgery: Pathophysiology, classification, and treatment. Video J. Sports Med. 2022, 2, 26350254221086295. [Google Scholar] [CrossRef]
- Sonnery-Cottet, B.; Ripoll, T.; Cavaignac, E. Prevention of knee stiffness following ligament reconstruction: Understanding the role of arthrogenic muscle inhibition (AMI). Orthop. Traumatol. Surg. Res. 2024, 110 (Suppl. S1), 103784. [Google Scholar] [CrossRef]
- Tayfur, B.; Charuphongsa, C.; Morrissey, D.; Miller, S.C. Neuromuscular joint function in knee osteoarthritis: A systematic review and meta-analysis. Ann. Phys. Rehabil. Med. 2023, 66, 101662. [Google Scholar] [CrossRef]
- Tayfur, B.; Charuphongsa, C.; Morrissey, D.; Miller, S.C. Neuromuscular function of the knee joint following knee injuries: Does it ever get back to normal? A systematic review with meta-analyses. Sports Med. 2021, 51, 321–338. [Google Scholar] [CrossRef]
| Groups | Control with Hip Arthroplasty | Control with Knee Arthroplasty | Experimental with Hip Arthroplasty | Experimental with Knee Arthroplasty |
|---|---|---|---|---|
| Number of patients | 13 | 12 | 12 | 9 |
| Age (years) | 61.92 ± 5.18(CI) | 68.58 ± 4.11(CI) | 68.17 ± 6.34(CI) | 67.44 ± 5.57(CI) |
| Weight (kg) | 81.0 ± 12.80(CI) | 85.08 ± 15.55(CI) | 85.33 ± 11.71(CI) | 83.44 ± 13.11(CI) |
| Height (cm) | 167.31 ± 6.05(CI) | 162.67 ± 7.32(CI) | 168.83 ± 5.74(CI) | 159.89 ± 7.26(CI) |
| Body mass index | 22.29 ± 4.19(CI) | 26.71 ± 5.30(CI) | 20.76 ± 4.27(CI) | 26.69 ± 4.27(CI) |
| Groups | Control | Control | Experimental | Experimental |
|---|---|---|---|---|
| Number of patients | 25 | 25 | 21 | 21 |
| Follow-up | Before surgery | After 1 month | Before surgery | After 1 month |
| Visual analog scale | 5.28 ± 0.45(CI) | 2.6 ± 0.23(CI) | 5.81 ± 0.60(CI) | 2.08 ± 0.21(CI) |
| Manual muscle testing | 0.48 ± 0.03(CI) | 0.58 ± 0.02(CI) | 0.46 ± 0.03(CI) | 0.64 ± 0.04(CI) |
| Range of motion | 0.25 ± 0.05(CI) | 0.38 ± 0.08(CI) | 0.25 ± 0.07(CI) | 0.44 ± 0.09(CI) |
| Thigh circumference difference | 2.68 ± 0.25(CI) | 1.08 ± 0.13(CI) | 2.76 ± 0.22(CI) | 0.71 ± 0.11(CI) |
| MMT | ROM | Success Rate | Difference (cm) | |
|---|---|---|---|---|
| VAS Correlation coefficient p-value | Correlation −0.553 <0.001 | Correlation −0.255059 <0.001 | Correlation −0.1764 <0.03 | Correlation +0.22459 <0.005 |
| MMT Correlation coefficient p-value | Correlation +0.3225093 <0.001 | Correlation +0.1823 <0.02 | Correlation –0.515400 <0.001 | |
| ROM Correlation coefficient p-value | Correlation +0.49904 <0.001 | Correlation –0.5379053 <0.001 | ||
| Success rate Correlation coefficient p-value | Correlation −0.4335101521 <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aleksiev, A.; Kovacheva-Predovska, D.; Assiov, S. Preliminary Quadriceps Muscle Contraction in the Early Rehabilitation of Hip and Knee Arthroplasty. J. Clin. Med. 2025, 14, 7021. https://doi.org/10.3390/jcm14197021
Aleksiev A, Kovacheva-Predovska D, Assiov S. Preliminary Quadriceps Muscle Contraction in the Early Rehabilitation of Hip and Knee Arthroplasty. Journal of Clinical Medicine. 2025; 14(19):7021. https://doi.org/10.3390/jcm14197021
Chicago/Turabian StyleAleksiev, Assen, Daniela Kovacheva-Predovska, and Sasho Assiov. 2025. "Preliminary Quadriceps Muscle Contraction in the Early Rehabilitation of Hip and Knee Arthroplasty" Journal of Clinical Medicine 14, no. 19: 7021. https://doi.org/10.3390/jcm14197021
APA StyleAleksiev, A., Kovacheva-Predovska, D., & Assiov, S. (2025). Preliminary Quadriceps Muscle Contraction in the Early Rehabilitation of Hip and Knee Arthroplasty. Journal of Clinical Medicine, 14(19), 7021. https://doi.org/10.3390/jcm14197021








