Rescue Procedure in a Rare Case of Iatrogenic Vertebral Artery Puncture and Review of the Literature
Abstract
1. Introduction
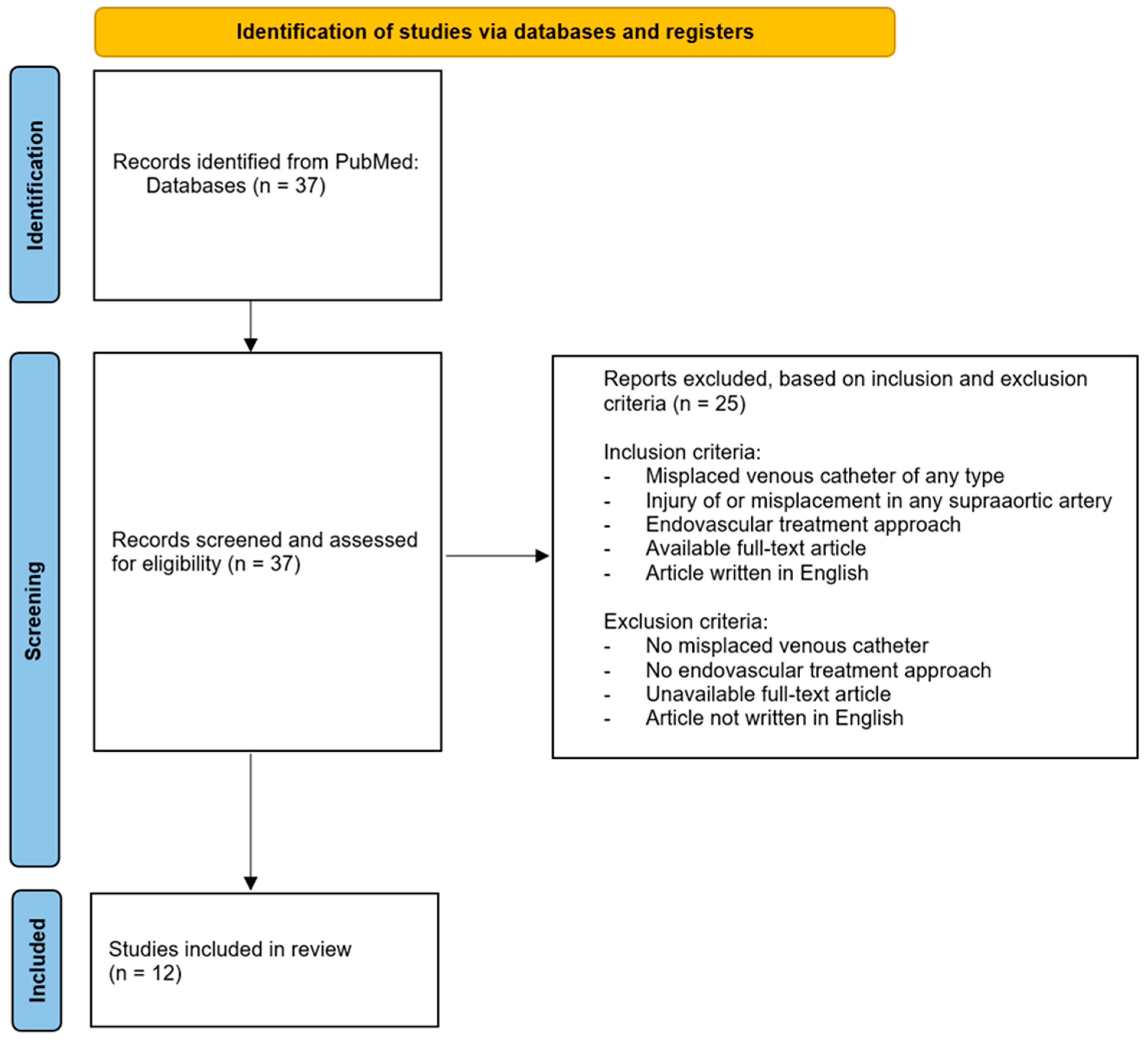
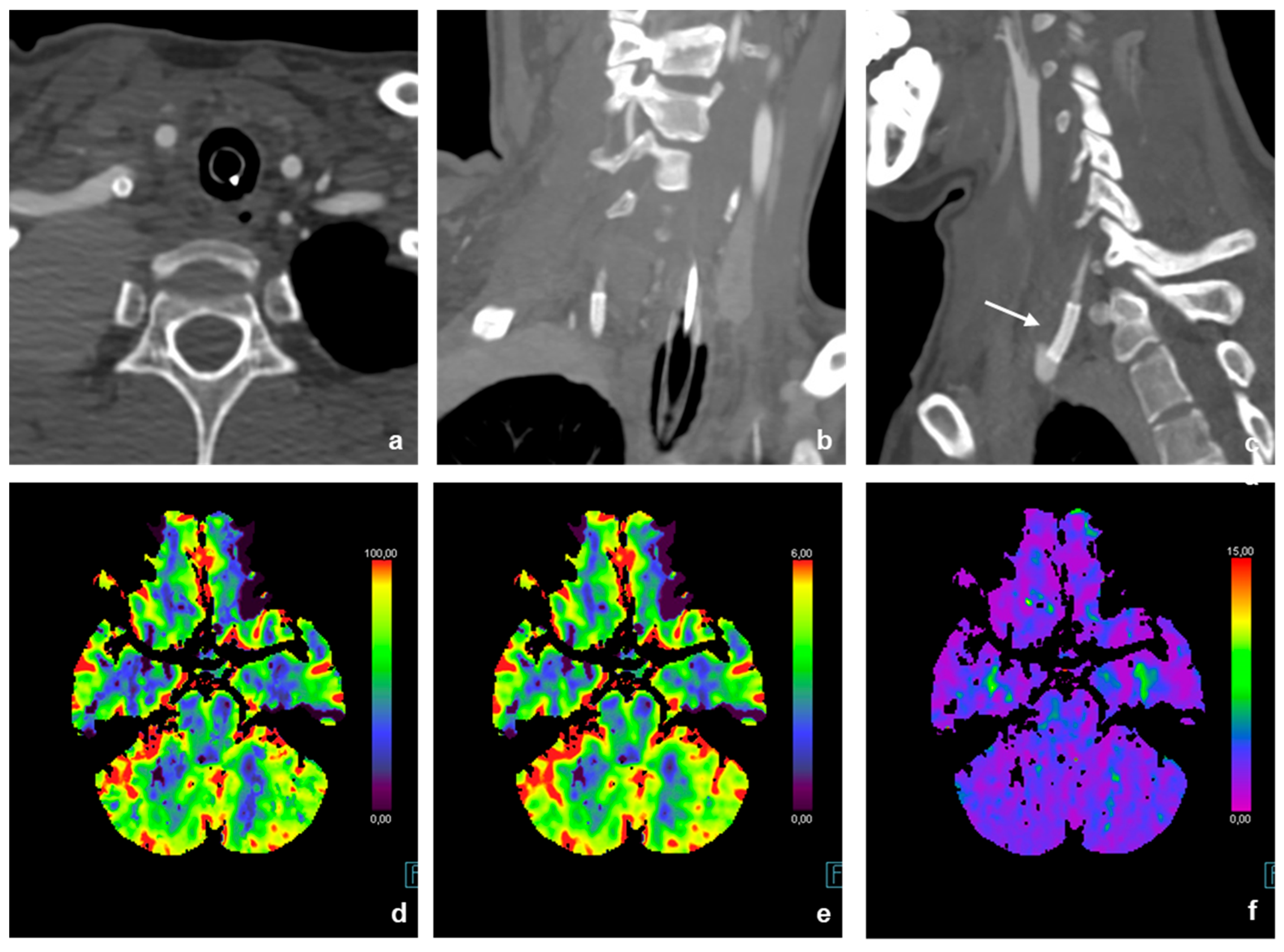
2. Systematic Review
3. Clinical Case
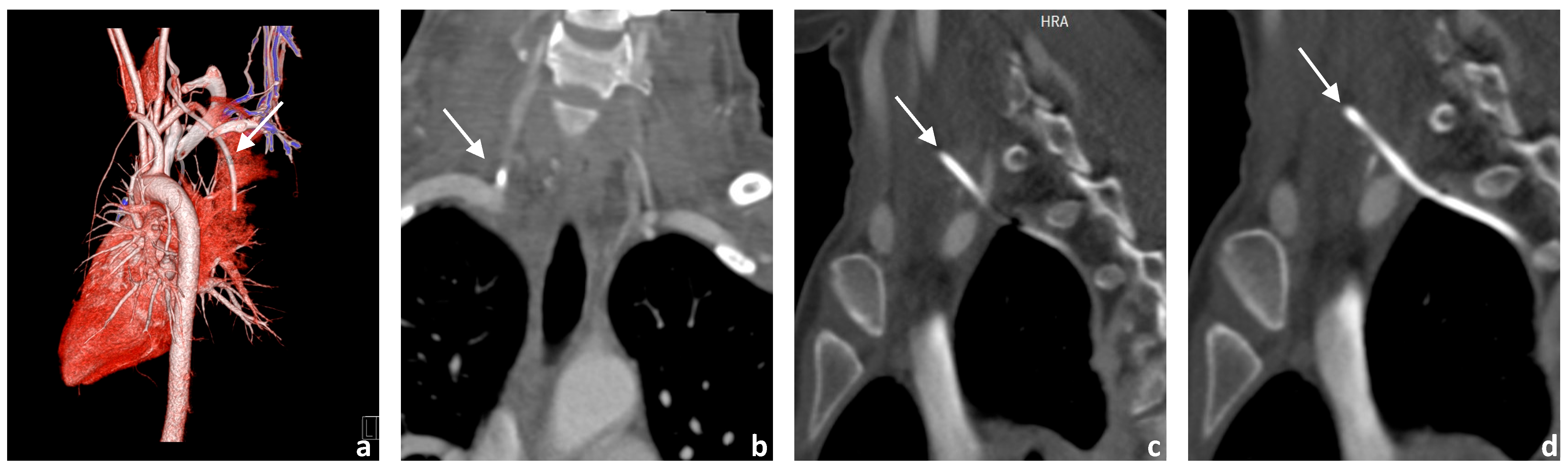
3.1. Image Acquisition
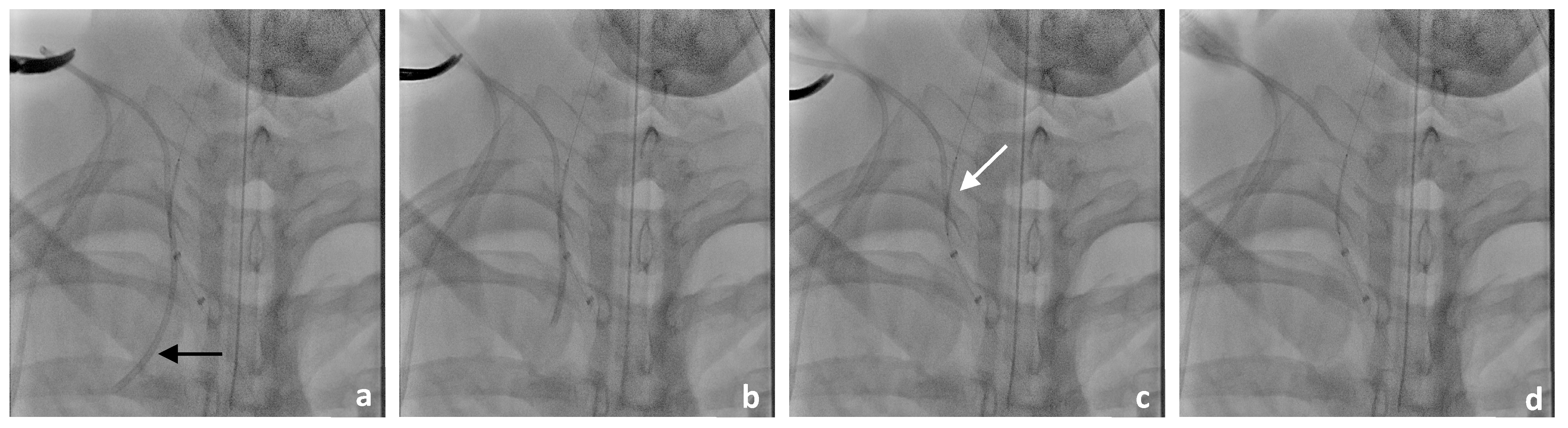
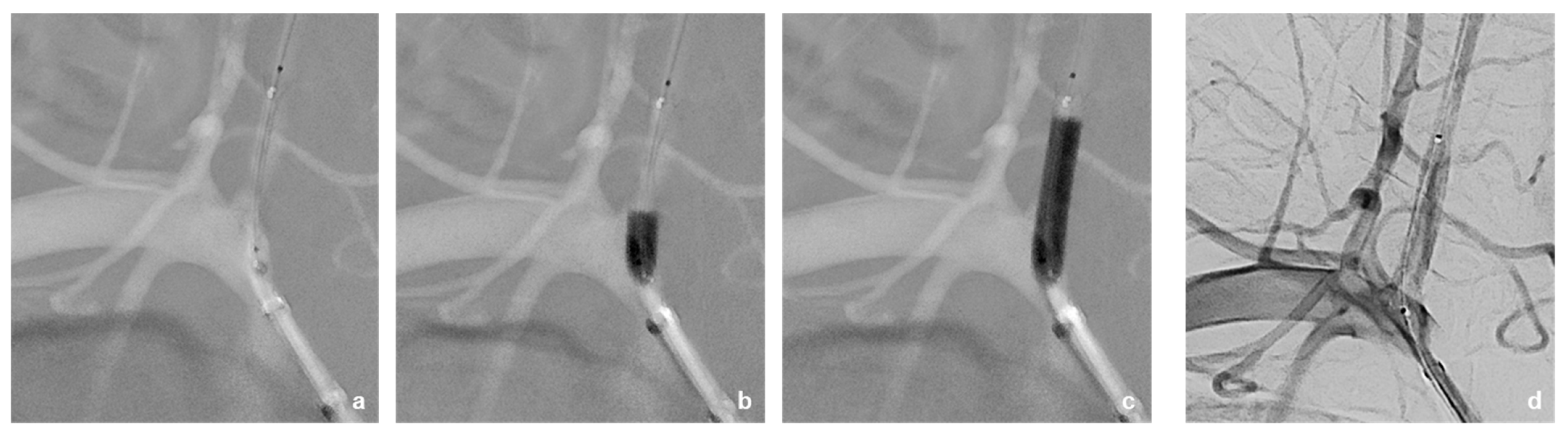
3.2. Neurointerventional Procedure
3.3. Drug Therapy During Intervention and After Stent Implantation
3.3.1. Pre-Interventional Drug Administration
3.3.2. Periinterventional Drug Administration
3.3.3. Postinterventional Drug Administration
3.4. Postinterventional Result
4. Discussion
Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lucas, S.J.; Bready, E.; Banks, C.A.; Gaillard, W.F.; Beck, A.W.; Spangler, E. Accidental Central Venous Catheter Cannulation into Aberrant Arterial Anatomy Requiring Endovascular Intervention. J. Vasc. Surg. Cases Innov. Tech. 2023, 9, 101164. [Google Scholar] [CrossRef]
- Broviac, J.W.; Cole, J.J.; Scribner, B.H. A Silicone Rubber Atrial Catheter for Prolonged Parenteral Alimentation. Surg. Gynecol. Obs. 1973, 136, 602–606. [Google Scholar]
- Fritsch, L.-M.; Le, M.; Elrod, J.; Wössmann, W.; Vincent, D.; Reinshagen, K.; Boettcher, M. Surgical Experience Affects the Outcome of Central Venous Access Catheter Implantation in Children: A Retrospective Cohort Study. J. Pediatr. Hematol. Oncol. 2023, 45, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Ladefoged, K.; Jarnum, S. Long-Term Parenteral Nutrition. Br. Med. J. 1978, 2, 262–266. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Garonzi, C.; Zeni, F.; Tridello, G.; Giacomazzi, A.; Castagna, A.; Esposto, M.P.; Caddeo, G.; Pezzella, V.; Zaccaron, A.; Bonetti, E.; et al. Results of a Long-Term, Prospective Study on Complications of Central Venous Catheter in Pediatric Patients with Hematologic-Oncologic Diseases. Pediatr. Blood Cancer 2024, 71, e30990. [Google Scholar] [CrossRef] [PubMed]
- Blotte, C.; Styers, J.; Zhu, H.; Channabasappa, N.; Piper, H.G. A Comparison of Broviac® and Peripherally Inserted Central Catheters in Children with Intestinal Failure. J. Pediatr. Surg. 2017, 52, 768–771. [Google Scholar] [CrossRef] [PubMed]
- Wicky, S.; Meuwly, J.-Y.; Doenz, F.; Uské, A.; Schnyder, P.; Denys, A. Life-Threatening Vascular Complications after Central Venous Catheter Placement. Eur. Radiol. 2002, 12, 901–907. [Google Scholar] [CrossRef] [PubMed]
- Jahromi, B.S.; Tummala, R.P.; Levy, E.I. Inadvertent Subclavian Artery Catheter Placement Complicated by Stroke: Endovascular Management and Review. Catheter. Cardiovasc. Interv. 2009, 73, 706–711. [Google Scholar] [CrossRef] [PubMed]
- Tanveer Ud Din, M.; Nasrullah, A.; Sarma, D.; Ashraf, O.; Arshad, H. Amidst COVID-19 Pandemic: The Catastrophic Sequelae of an Inadvertent Carotid Artery Insertion during Central Venous Catheter Placement—A Case Report. J. Community Hosp. Intern. Med. Perspect. 2021, 11, 689–692. [Google Scholar] [CrossRef] [PubMed]
- Ito, Y.; Kojima, T.; Yamanoi, Y.; Saito, K. Acute Endovascular Therapy for Iatrogenic Vertebral Artery Injury: A Case Report. J. Neuroendovasc. Ther. 2022, 16, 33–38. [Google Scholar] [CrossRef] [PubMed]
- Schoder, M.; Cejna, M.; Hölzenbein, T.; Bischof, G.; Lomoschitz, F.; Funovics, M.; Nöbauer-Huhmann, I.; Sulzbacher, I.; Lammer, J. Elective and Emergent Endovascular Treatment of Subclavian Artery Aneurysms and Injuries. J. Endovasc. Ther. 2003, 10, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Kohyama, T.; Fujimaki, K.; Sasamori, H.; Tokumine, J.; Moriyama, K.; Yorozu, T. Inadvertent Catheter Misplacement into the Subclavian Artery during Ultrasound-Guided Internal Jugular Venous Catheterization: A Case Report. JA Clin. Rep. 2023, 9, 58. [Google Scholar] [CrossRef] [PubMed]
- Yoshida, H.; Ikemoto, S.; Tokinaga, Y.; Ejiri, K.; Kawamata, T. Successful Removal of a Central Venous Catheter Misplaced in the Right Subclavian Artery Using an Intravascular Stent: A Case Report. JA Clin. Rep. 2021, 7, 15. [Google Scholar] [CrossRef]
- Akkan, K.; Cindil, E.; Kilic, K.; Ilgit, E.; Onal, B.; Erbas, G. Misplaced Central Venous Catheter in the Vertebral Artery: Endovascular Treatment of Foreseen Hemorrhage during Catheter Withdrawal. J. Vasc. Access 2014, 15, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Wadhwa, R.; Toms, J.; Nanda, A.; Abreo, K.; Cuellar, H. Angioplasty and Stenting of a Jugular-Carotid Fistula Resulting from the Inadvertent Placement of a Hemodialysis Catheter: Case Report and Review of Literature. Semin. Dial. 2012, 25, 460–463. [Google Scholar] [CrossRef]
- Shaw, M.; Chandrashekhara, S.H.; Sharma, A.; Kumar, S. Inadvertent Arterial Placement of Central Venous Catheter: Salvage Using Endovascular Treatment. BMJ Case Rep. 2019, 12, e231751. [Google Scholar] [CrossRef]
- Yen, C.-C.; Chiu, Y.-W.; Chen, H.-C. Remove or Not, That Is the Question: A Case Report on Carotid Artery Cannulation during Indwelling Venous Hemodialysis Catheter. Hemodial. Int. 2015, 19, E17–E20. [Google Scholar] [CrossRef]
- Guilbert, M.-C.; Elkouri, S.; Bracco, D.; Corriveau, M.M.; Beaudoin, N.; Dubois, M.J.; Bruneau, L.; Blair, J.-F. Arterial Trauma during Central Venous Catheter Insertion: Case Series, Review and Proposed Algorithm. J. Vasc. Surg. 2008, 48, 918–925. [Google Scholar] [CrossRef] [PubMed]

| Search Term | Title | Author | Year | doi | Included | Excluded | Unavailable Full Text | Language Other Than English | No Endovascular Approach | No Misplaced Catheter | Study Type | Carotid Placement | Vertebralis Placement | Subclavian Placement |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| misplaced venous catheter AND stroke | Arterial trauma during central venous catheter insertion: Case series, review and proposed algorithm | Guilbert et al. | 2008 | 10.1016/j.jvs.2008.04.046 | X | X | Review | X | X | |||||
| A rare cause of stroke: fail-implanted venous port catheter system - a case report | 2021 | X | X | Case report | ||||||||||
| Inadvertent subclavian artery catheter placement complicated by stroke: endovascular management and review | Jahromi et al. | 2009 | 10.1002/ccd.21884 | X | Case report | X | ||||||||
| Central Venous Catheter Placement Gone Awry: A Case Report of Right Internal Jugular Central Line Entering Subclavian Artery | 2022 | X | X | Case report | ||||||||||
| Misplaced peripherally inserted central catheter: an unusual cause of stroke | 2004 | X | X | Case report | ||||||||||
| Amidst COVID-19 pandemic: the catastrophic sequelae of an inadvertent carotid artery insertion during central venous catheter placement-a case report | Din et al. | 2021 | 10.1080/20009666.2021.1952015 | X | Case report | X | ||||||||
| Thrombotic, infectious, and procedural complications of the jugular bulb catheter in the intensive care unit | 1997 | X | X | Clinical study | ||||||||||
| Right vertebral artery injury as a result of misplaced internal jugular vein catheter withdrawal | 2019 | X | X | Case report | ||||||||||
| Arterial misplacement of large-caliber cannulas during jugular vein catheterization: case for surgical management | 2004 | X | X | Clinical study | ||||||||||
| Truncus bicaroticus and an aberrant right subclavian artery contributing to internal jugular venous line misplacement into the carotid artery | 2009 | X | X | Case report | ||||||||||
| Use of echocardiography to identify appropriate placement of a central venous catheter wire in the vena cava prior to cannulation | 2014 | X | X | X | Review | |||||||||
| Embolic strokes after peripherally inserted central catheter placement | 2010 | X | X | Case report | ||||||||||
| misplaced venous catheter AND cerebral angiography | Elective and emergent endovascular treatment of subclavian artery aneurysms and injuries | Schoder et al. | 2003 | 10.1177/152660280301000113 | X | Retrospective study | X | |||||||
| misplaced venous catheter AND balloon guided catheter | Acute Endovascular Therapy for Iatrogenic Vertebral Artery Injury: A Case Report | Ito et al. | 2021 | 10.5797/jnet.cr.2020-0208 | X | Case report | X | |||||||
| misplaced venous catheter AND ischemia | Inadvertent Arterial Cannulation and Norepinephrine Infusion Due to a Misplaced Central Venous Catheter | 2021 | X | Case report | ||||||||||
| Vascular anomaly diagnosis by central venous catheter misplacement: a case report | 2022 | X | Case report | |||||||||||
| Inadvertent catheter misplacement into the subclavian artery during ultrasound-guided internal jugular venous catheterization: a case report | Kohyama et al. | 2023 | 10.1186/s40981-023-00649-1 | X | Case report | X | ||||||||
| An atypical misplacement of a temporary pacing catheter diagnosed and resolved by ultrasound | 2014 | X | X | X | Case report | |||||||||
| [Right subclavian catheterization. Misplaced insertion into the subclavian artery and the ascending aorta] | 1999 | X | X | Case report | ||||||||||
| The concept of forensic emergency medicine as illustrated by an unusual complication of pulmonary artery catheterization | 2008 | X | Case report | |||||||||||
| misplaced venous catheter AND stent | Successful removal of a central venous catheter misplaced in the right subclavian artery using an intravascular stent: a case report | Yoshida et al. | 2021 | 10.1186/s40981-021-00418-y | X | Case report | X | |||||||
| Prevention and treatment of dilator injuries during central venous catheter placement | 2019 | X | X | X | Clinical study | |||||||||
| Central venous catheter misplaced in the vertebral artery | 2016 | X | X | Case report | ||||||||||
| Treatment of inadvertent cervical arterial catheterization: Single-center experience | 2022 | X | X | Clinical study | ||||||||||
| Misplaced central venous catheter in the vertebral artery: endovascular treatment of foreseen hemorrhage during catheter withdrawal | Akkan et al. | 2014 | 10.5301/jva.5000267 | X | Case report | X | ||||||||
| Erroneous placement of central venous catheters in subclavian artery: Retrieval and successful hemostasis with a femoral closure device | 2022 | X | X | Case report | ||||||||||
| Minimally invasive catheter procedures to assist complicated pacemaker lead extraction and implantation in the operating room | 2011 | X | X | Clinical study | ||||||||||
| Endovascular foreign body retrieval | 2013 | X | X | Clinical study | ||||||||||
| Intracaval misplacement of a double-J ureteral stent | 2018 | X | X | Case report | ||||||||||
| Accidental central venous catheter cannulation into aberrant arterial anatomy requiring endovascular intervention | Lucas et al. | 2023 | 10.1016/j.jvscit.2023.101164 | X | Case report | X | ||||||||
| Angioplasty and stenting of a jugular-carotid fistula resulting from the inadvertent placement of a hemodialysis catheter: case report and review of literature | Wadhwa et al. | 2016 | 10.1111/j.1525-139X.2011.01005.x | X | Case report | X | ||||||||
| Inadvertent arterial placement of central venous catheter: salvage using endovascular treatment | Shaw et al. | 2019 | 10.1136/bcr-2019-231751 | X | Case report | X | ||||||||
| Life-threatening vascular complications after central venous catheter placement | Wicky et al. | 2002 | 10.1007/s003300101018 | X | Retrospective study | X | ||||||||
| Remove or not, that is the question: A case report on carotid artery cannulation during indwelling venous hemodialysis catheter | Yen et al. | 2015 | 10.1111/hdi.12297 | X | Case report | X | ||||||||
| Misplacement or migration? Extremely rare case of cardiac migration of a ureteral j stent | 2014 | X | X | X | Case report | |||||||||
| Caval migration of a ureteral J-stent after simultaneous ureter and iliac vein perforation during its placement for obstructive pyelonephritis | 2009 | X | X | X | Case report | |||||||||
| Percutaneous retrieval of a Strecker stent misplaced during TIPS | 1995 | X | X | X | Case report | |||||||||
| misplaced venous catheter AND rescue | Percutaneous closure of accidentally subclavian artery catheterization: time to change first line approach? | 2022 | X | X | X | Clinical study | ||||||||
| misplaced broviac AND balloon guided catheter | X | |||||||||||||
| misplaced broviac AND stroke | X | |||||||||||||
| misplaced broviac AND cerebral angiography | X | |||||||||||||
| misplaced broviac AND ischemia | X | |||||||||||||
| misplaced broviac AND stent | X | |||||||||||||
| misplaced broviac AND rescue | X | |||||||||||||
| misplaced shaldon AND balloon guided catheter | X | |||||||||||||
| misplaced shaldon AND stroke | X | |||||||||||||
| misplaced shaldon AND cerebral angiography | X | |||||||||||||
| misplaced shaldon AND ischemia | X | |||||||||||||
| misplaced shaldon AND stent | X | |||||||||||||
| misplaced shaldon AND rescue | X | |||||||||||||
| misplaced central venous catheter AND balloon guided catheter | X | |||||||||||||
| misplaced central venous catheter AND stroke | X | |||||||||||||
| misplaced central venous catheter AND cerebral angiography | X | |||||||||||||
| misplaced central venous catheter AND ischemia | X | |||||||||||||
| misplaced central venous catheter AND stent | X | |||||||||||||
| misplaced central venous catheter AND rescue | X | |||||||||||||
| Treatment Approach | Technical Succes | Surgical Intervention Required | Postinterventionell Complication | Outcome | Special Points | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Vascular Territory | Manual Pressure | Percutaneous Closure | Stenting | Coiling | Balloon Occlusion | Open Surgicl Repair | Yes | No | Yes | No | Hemorrhage | Occlusion | Stroke | Pseudaneurysm | Favorable | Unfavorable | Resolution of Complications | ||||||||
| X | X | X | X | ||||||||||||||||||||||
| X | X | X | X | ||||||||||||||||||||||
| RAVT + RACP | X | X | X | X | X | X | Complete | ||||||||||||||||||
| X | X | X | X | RAVT closure without stroke after MRI-perfusion | |||||||||||||||||||||
| X | X | X | X | ||||||||||||||||||||||
| X | X | X | X | X | |||||||||||||||||||||
| ACI | X | X | X | X | Duration of misplacement of catheter = 24 days, administration of several medications | ||||||||||||||||||||
| X | X | X | X | X | |||||||||||||||||||||
| X | X | X | X | Complete posterior circulation blood supply via LAVT | |||||||||||||||||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brandt, J.; Musigmann, M.; Akkurt, B.H.; Köhler, M.; Krähling, H. Rescue Procedure in a Rare Case of Iatrogenic Vertebral Artery Puncture and Review of the Literature. J. Clin. Med. 2025, 14, 6945. https://doi.org/10.3390/jcm14196945
Brandt J, Musigmann M, Akkurt BH, Köhler M, Krähling H. Rescue Procedure in a Rare Case of Iatrogenic Vertebral Artery Puncture and Review of the Literature. Journal of Clinical Medicine. 2025; 14(19):6945. https://doi.org/10.3390/jcm14196945
Chicago/Turabian StyleBrandt, Jonas, Manfred Musigmann, Burak Han Akkurt, Michael Köhler, and Hermann Krähling. 2025. "Rescue Procedure in a Rare Case of Iatrogenic Vertebral Artery Puncture and Review of the Literature" Journal of Clinical Medicine 14, no. 19: 6945. https://doi.org/10.3390/jcm14196945
APA StyleBrandt, J., Musigmann, M., Akkurt, B. H., Köhler, M., & Krähling, H. (2025). Rescue Procedure in a Rare Case of Iatrogenic Vertebral Artery Puncture and Review of the Literature. Journal of Clinical Medicine, 14(19), 6945. https://doi.org/10.3390/jcm14196945







