Performance Asymmetry, the Risk for Ankle Sprain, and the Influence of an Intervention Program in New Male Infantry Recruits
Abstract
1. Introduction
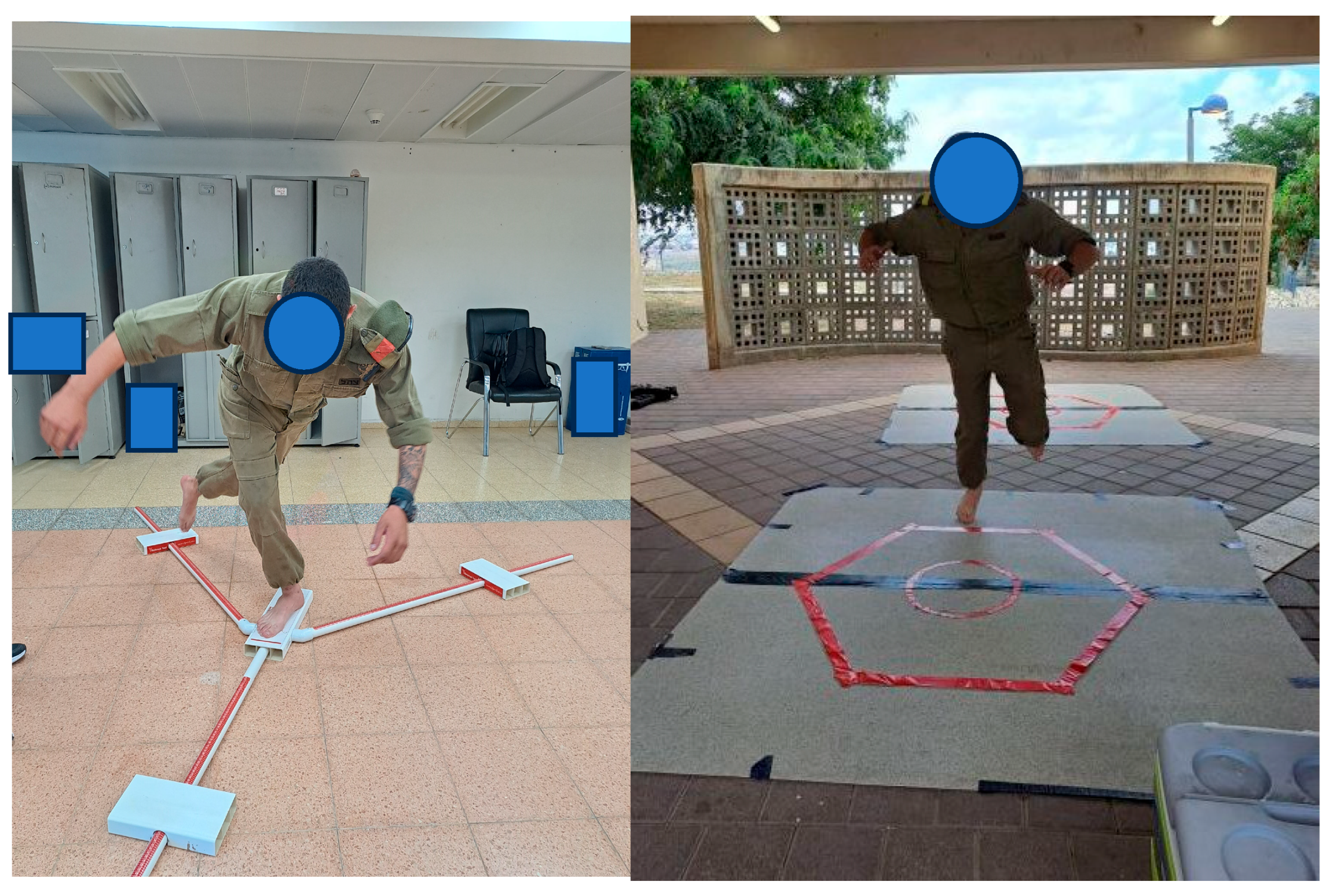
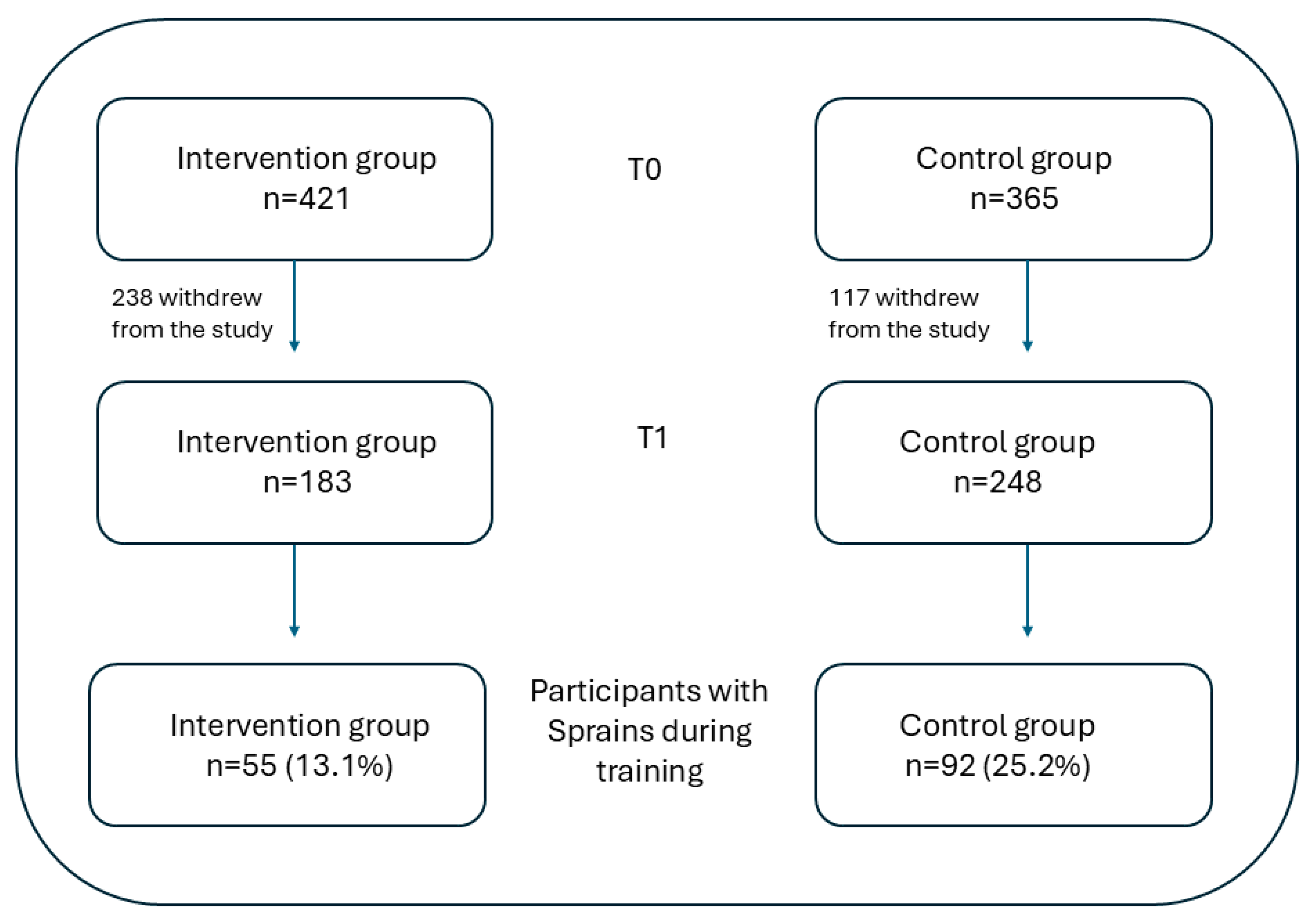
2. Materials and Methods
2.1. Assessments
2.2. Data Analysis
3. Results
4. Discussion
4.1. Limitations
4.2. Clinical Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| CAIT | Cumberland Ankle Instability Tool |
| YBT | Y-balance test |
| INT | intervention group |
| CON | control group |
| CAI | Chronic Ankle Instability |
References
- Fenn, B.P.; Song, J.; Casey, J.; Waryasz, G.R.; DiGiovanni, C.W.; Lubberts, B.; Guss, D. Worldwide epidemiology of foot and ankle injuries during military training: A systematic review. BMJ Mil. Health 2021, 167, 131–136. [Google Scholar] [CrossRef]
- Schwartz, O.; Levinson, T.; Astman, N.; Haim, L. Attrition due to orthopedic reasons during combat training: Rates, types of injuries, and comparison between infantry and noninfantry units. Mil. Med. 2014, 179, 897–900. [Google Scholar] [CrossRef]
- Herzog, M.M.; Kerr, Z.Y.; Marshall, S.W.; Wikstrom, E.A. Epidemiology of Ankle Sprains and Chronic Ankle Instability. J. Athl. Train. 2019, 54, 603–610. [Google Scholar] [CrossRef] [PubMed]
- Fraser, J.J.; MacGregor, A.J.; Ryans, C.P.; Dreyer, M.A.; Gibboney, M.D.; Rhon, D.I. Sex and occupation are salient factors associated with lateral ankle sprain risk in military tactical athletes. J. Sci. Med. Sport 2021, 24, 677–682. [Google Scholar] [CrossRef]
- Hertel, J.; Corbett, R.O. An Updated Model of Chronic Ankle Instability. J. Athl. Train. 2019, 54, 572–588. [Google Scholar] [CrossRef]
- Vuurberg, G.; Altink, N.; Rajai, M.; Blankevoort, L.; Kerkhoffs, G. Weight, BMI and stability are risk factors associated with lateral ankle sprains and chronic ankle instability: A meta-analysis. J. ISAKOS 2019, 4, 313–327. [Google Scholar] [CrossRef]
- Mason, J.; Kniewasser, C.; Hollander, K.; Zech, A. Intrinsic Risk Factors for Ankle Sprain Differ Between Male and Female Athletes: A Systematic Review and Meta-Analysis. Sports Med. Open 2022, 8, 139. [Google Scholar] [CrossRef] [PubMed]
- Steinberg, N.; Shenhar, M.; Dar, G.; Waddington, G.; Witchalls, J.; Paulman, O.; Milgrom, C.; Finestone, A. Ankle sprains in male Israeli infantry soldiers during training: Prevalence and risk factors. Inj. Prev. 2024; online first. [Google Scholar] [CrossRef] [PubMed]
- Guan, Y.; Bredin, S.S.D.; Taunton, J.; Jiang, Q.; Wu, N.; Warburton, D.E.R. Association between Inter-Limb Asymmetries in Lower-Limb Functional Performance and Sport Injury: A Systematic Review of Prospective Cohort Studies. J. Clin. Med. 2022, 11, 360. [Google Scholar] [CrossRef]
- Helme, M.; Tee, J.; Emmonds, S.; Low, C. Does lower-limb asymmetry increase injury risk in sport? A systematic review. Phys. Ther. Sport 2021, 49, 204–213. [Google Scholar] [CrossRef]
- Knapik, J.; Steelman, R. Risk Factors for Injuries During Military Static-Line Airborne Operations: A Systematic Review and Meta-Analysis. J. Athl. Train. 2016, 51, 962–980. [Google Scholar] [CrossRef]
- Hietamo, J.; Pasanen, K.; Leppänen, M.; Steffen, K.; Kannus, P.; Heinonen, A.; Mattila, V.M.; Parkkari, J. Association between lower extremity muscle strength and acute ankle injury in youth team-sports athletes. Phys. Ther. Sport 2021, 48, 188–195. [Google Scholar] [CrossRef]
- Hadzic, V.; Sattler, T.; Pori, P.; Veselko, M.; Dervisevic, E.; Sarabon, N.; Markovic, G. Quadriceps strength asymmetry as predictor of ankle sprain in male volleyball players. J. Sports Med. Phys. Fitness 2022, 62, 822–829. [Google Scholar] [CrossRef]
- MacSweeney, N.D.H.; Shaw, J.W.; Simkin, G.P.; Pedlar, C.R.; Price, P.D.B.; Mahaffey, R.; Cohen, D.D. Jumping Asymmetries and Risk of Injuries in Preprofessional Ballet. Am. J. Sports Med. 2024, 52, 492–502. [Google Scholar] [CrossRef] [PubMed]
- Yavnai, N.; Bar-Sela, S.; Pantanowitz, M.; Funk, S.; Waddington, G.; Simchas, L.; Svorai-Litvak, S.; Steinberg, N. Incidence of injuries and factors related to injuries in combat soldiers. BMJ Mil. Health 2020, 167, 418–423. [Google Scholar] [CrossRef] [PubMed]
- Yalfani, A.; Raeisi, Z. Bilateral symmetry of vertical time to stabilization in postural sway after double-leg landing in elite athletes with unilateral chronic ankle sprain. J. Foot Ankle Res. 2022, 15, 43. [Google Scholar] [CrossRef]
- Steinberg, N.; Tenenbaum, S.; Waddington, G.; Adams, R.; Zakin, G.; Zeev, A.; Siev-Ner, I. Unilateral and bilateral patellofemoral pain in young female dancers: Associated factors. J. Sports Sci. 2020, 38, 719–730. [Google Scholar] [CrossRef] [PubMed]
- Tajdini, H.; Mantashloo, Z.; Thomas, A.C.; Letafatkar, A.; Rossettini, G. Inter-limb asymmetry of kinetic and electromyographic during walking in patients with chronic ankle instability. Sci. Rep. 2022, 12, 3928. [Google Scholar] [CrossRef]
- Clark, N.C.; Campbell, S.D. Preseason weight-bearing ankle dorsiflexion in male professional football players with and without a history of severe ankle injury: A novel analysis in an English Premier League club. Phys. Ther. Sport 2021, 52, 21–29. [Google Scholar] [CrossRef]
- Steinberg, N.; Shenhar, M.; Witchalls, J.; Waddington, G.; Dar, G.; Paulman, O.; Finestone, A.R.S. Chronic Ankle Instability and Neuromuscular Performance in Prerecruitment Infantry Soldiers. J. Athl. Train. 2024, 59, 73–80. [Google Scholar] [CrossRef]
- Delahunt, E.; Bleakley, C.M.; Bossard, D.S.; Caulfield, B.M.; Docherty, C.L.; Doherty, C.; Fourchet, F.; Fong, D.T.; Hertel, J.; Hiller, C.E.; et al. Clinical assessment of acute lateral ankle sprain injuries (ROAST): 2019 consensus statement and recommendations of the International Ankle Consortium. Br. J. Sports Med. 2018, 52, 1304–1310. [Google Scholar] [CrossRef]
- Calatayud, J.; Borreani, S.; Colado, J.C.; Flandez, J.; Page, P.; Andersen, L.L. Exercise and ankle sprain injuries: A comprehensive review. Physician Sportsmed. 2014, 42, 88–93. [Google Scholar] [CrossRef] [PubMed]
- Bleakley, C.M.; Taylor, J.B.; Dischiavi, S.L.; Doherty, C.; Delahunt, E. Rehabilitation Exercises Reduce Reinjury Post Ankle Sprain, But the Content and Parameters of an Optimal Exercise Program Have Yet to Be Established: A Systematic Review and Meta-analysis. Arch. Phys. Med. Rehabil. 2019, 100, 1367–1375. [Google Scholar] [CrossRef]
- Milgrom, C.; Shlamkovitch, N.; Finestone, A.; Eldad, A.; Laor, A.; Danon, Y.L.; Lavie, O.; Wosk, J.; Simkin, A. Risk factors for lateral ankle sprain: A prospective study among military recruits. Foot Ankle 1991, 12, 26–30. [Google Scholar] [CrossRef]
- Strowbridge, N.F.; Burgess, K.R. Sports and training injuries in British soldiers: The Colchester Garrison Sports Injury and Rehabilitation Centre. J. R. Army Med. Corps 2002, 148, 236–243. [Google Scholar] [CrossRef]
- JASP, version 0.95; JASP Team: Visakhapatnam, India, 2025.
- Lisman, P.; Hildebrand, E.; Nadelen, M.; Leppert, K. Association of Functional Movement Screen and Y-Balance Test Scores With Injury in High School Athletes. J. Strength Cond. Res. 2021, 35, 1930–1938. [Google Scholar] [CrossRef] [PubMed]
- Brumitt, J.; Nelson, K.; Duey, D.; Jeppson, M.; Hammer, L. Preseason Y Balance Test Scores are not Associated with Noncontact Time-Loss Lower Quadrant Injury in Male Collegiate Basketball Players. Sports 2019, 7, 4. [Google Scholar] [CrossRef]
- Smith, C.A.; Chimera, N.J.; Warren, M. Association of y balance test reach asymmetry and injury in division I athletes. Med. Sci. Sports Exerc. 2015, 47, 136–141. [Google Scholar] [CrossRef]
- Plisky, P.J.; Rauh, M.J.; Kaminski, T.W.; Underwood, F.B. Star Excursion Balance Test as a predictor of lower extremity injury in high school basketball players. J. Orthop. Sports Phys. Ther. 2006, 36, 911–919. [Google Scholar] [CrossRef]
- Ryu, C.H.; Park, J.; Kang, M.; Oh, J.H.; Kim, Y.K.; Kim, Y.I.; Lee, H.S.; Seo, S.G. Differences in lower quarter Y-balance test with player position and ankle injuries in professional baseball players. J. Orthop. Surg. 2019, 27, 2309499019832421. [Google Scholar] [CrossRef] [PubMed]
- Vaulerin, J.; Chorin, F.; Emile, M.; d’Arripe-Longueville, F.; Colson, S.S. Ankle Sprains Risk Factors in a Sample of French Firefighters: A Preliminary Prospective Study. J. Sport Rehabil. 2020, 29, 608–615. [Google Scholar] [CrossRef] [PubMed]
- Gao, L.; Gusztáv, F.; Gao, Z. Effects of Loading Positions on Lower Limb Biomechanics During Lunge Squat in Men with Different Training Experience. Phys. Act. Health 2025, 9, 198–213. [Google Scholar]
- Basnett, C.R.; Hanish, M.J.; Wheeler, T.J.; Miriovsky, D.J.; Danielson, E.L.; Barr, J.B.; Grindstaff, T.L. Ankle dorsiflexion range of motion influences dynamic balance in individuals with chronic ankle instability. Int. J. Sports Phys. Ther. 2013, 8, 121–128. [Google Scholar] [PubMed]
- Madsen, L.P.; Hall, E.A.; Docherty, C.L. Assessing outcomes in people with chronic ankle instability: The ability of functional performance tests to measure deficits in physical function and perceived instability. J. Orthop. Sports Phys. Ther. 2018, 48, 372–380. [Google Scholar] [CrossRef]
- Rosen, A.; Ko, J.; Brown, C. A Multivariate Assessment of Clinical Contributions to the Severity of Perceived Dysfunction Measured by the Cumberland Ankle Instability Tool. Int. J. Sports Med. 2016, 37, 1154–1158. [Google Scholar] [CrossRef] [PubMed]
- Wright, C.J.; Arnold, B.L.; Ross, S.E.; Linens, S.W. Recalibration and validation of the Cumberland Ankle Instability Tool cutoff score for individuals with chronic ankle instability. Arch. Phys. Med. Rehabil. 2014, 95, 1853–1859. [Google Scholar] [CrossRef]
- Pourkazemi, F.; Hiller, C.E.; Raymond, J.; Nightingale, E.J.; Refshauge, K.M. Predictors of chronic ankle instability after an index lateral ankle sprain: A systematic review. J. Sci. Med. Sport 2014, 17, 568–573. [Google Scholar] [CrossRef]
- Kwakye, S.K.; Mostert, K.; Garnett, D.; Masenge, A. Risk factors associated with football injury among male players from a specific academy in Ghana: A pilot study. Sci. Rep. 2023, 13, 8070. [Google Scholar] [CrossRef]
- Doherty, C.; Bleakley, C.; Hertel, J.; Caulfield, B.; Ryan, J.; Delahunt, E. Recovery From a First-Time Lateral Ankle Sprain and the Predictors of Chronic Ankle Instability: A Prospective Cohort Analysis. Am. J. Sports Med. 2016, 44, 995–1003. [Google Scholar] [CrossRef]
- Svorai Band, S.; Pantanowitz, M.; Funk, S.; Waddington, G.; Steinberg, N. Factors associated with musculoskeletal injuries in an infantry commanders course. Physician Sportsmed. 2021, 49, 81–91. [Google Scholar] [CrossRef]
- Gao, Z. The effect of application of asymmetry evaluation in competitive Sports: A systematic review. Phys. Act. Health 2022, 6, 257–272. [Google Scholar] [CrossRef]
- Vasileiou, S.S.; Asimakidis, N.D.; Dalamitros, A.A.; Manou, V. Effects of an 8-Week In-Season Explosive Power Training Program on Neuromuscular Performance and Lower-Limb Asymmetries in Young Male Soccer Players. J. Strength Cond. Res. 2024, 38, 2121–2128. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Qin, Z.; Zhang, M. Association between pre-season lower limb interlimb asymmetry and non-contact lower limb injuries in elite male volleyball players. Sci. Rep. 2025, 15, 14481. [Google Scholar] [CrossRef]
- Xue, X.; Ma, T.; Li, Q.; Song, Y.; Hua, Y. Chronic ankle instability is associated with proprioception deficits: A systematic review and meta-analysis. J. Sport Health Sci. 2021, 10, 182–191. [Google Scholar] [CrossRef] [PubMed]
- Soligard, T.; Myklebust, G.; Steffen, K.; Holme, I.; Silvers, H.; Bizzini, M.; Junge, A.; Dvorak, J.; Bahr, R.; Andersen, T.E. Comprehensive warm-up programme to prevent injuries in young female footballers: Cluster randomised controlled trial. BMJ 2008, 337, a2469. [Google Scholar] [CrossRef]
- Al Attar, W.S.A.; Khaledi, E.H.; Bakhsh, J.M.; Faude, O.; Ghulam, H.; Sanders, R.H. Injury prevention programs that include balance training exercises reduce ankle injury rates among soccer players: A systematic review. J. Physiother. 2022, 68, 165–173. [Google Scholar] [CrossRef] [PubMed]
- Kaminski, T.W.; Needle, A.R.; Delahunt, E. Prevention of Lateral Ankle Sprains. J. Athl. Train. 2019, 54, 650–661. [Google Scholar] [CrossRef]
- Mohammadi, F.; Azma, K.; Naseh, I.; Emadifard, R.; Etemadi, Y. Military exercises, knee and ankle joint position sense, and injury in male conscripts: A pilot study. J. Athl. Train. 2013, 48, 790–796. [Google Scholar] [CrossRef]
- Orr, R.M.; Johnston, V.; Coyle, J.; Pope, R. Reported load carriage injuries of the Australian army soldier. J. Occup. Rehabil. 2015, 25, 316–322. [Google Scholar] [CrossRef]
| Anthropometric/Asymmetry Measure | Intervention | Control | ||
|---|---|---|---|---|
| SPRAIN n = 55 | NO-SPRAIN n = 366 | SPRAIN n = 92 | NO-SPRAIN n = 273 | |
| Height | 174.73 ± 6.4 | 175.04 ± 6.6 | 175.43 ± 7.1 | 175.55 ± 6.4 |
| Weight & | 76.34 ± 12.4 | 74.35 ± 10.5 | 77.12 ± 12.6 | 74.60 ± 12.4 |
| BMI & | 25.05 ± 3.6 | 24.28 ± 3.1 | 25.04 ± 3.7 | 24.17 ± 3.5 |
| Hexagon asymmetry $@ | 2.20 ± 1.9 | 2.09 ± 1.7 | 1.28 ± 1.2 | 1.99 ± 1.8 |
| YBT Ant asymmetry | 5.83 ± 4.2 | 5.26 ± 5.0 | 4.60 ± 4.1 | 5.71 ± 6.0 |
| YBT PL asymmetry | 8.28 ± 8.4 | 6.76 ± 6.2 | 7.09 ± 6.2 | 7.39 ± 6.7 |
| YBT PM asymmetry $ | 6.68 ± 6.1 | 7.77 ± 7.3 | 8.48 ± 6.7 | 9.11 ± 7.3 |
| YBT Comp asymmetry $@ | 9.67 ± 19.4 | 5.68 ± 7.9 | 4.72 ± 3.8 | 5.64 ± 6.1 |
| CAIT asymmetry $&@ | 2.86 ± 4.5 | 0.90 ± 2.1 | 1.26 ± 3.6 | 0.83 ± 2.4 |
| Asymmetry Measure | Intervention | Control | ||||||
|---|---|---|---|---|---|---|---|---|
| SPRAIN n = 55 | NO-SPRAIN n = 366 | SPRAIN n = 92 | NO-SPRAIN n = 273 | |||||
| T0 | T1 | T0 | T1 | T0 | T1 | T0 | T1 | |
| Hexagon $&@ | 2.30 ± 1.7 | 1.44 ± 1.1 | 2.10 ± 1.9 | 2.13 ± 2.0 | 1.29 ± 1.2 | 1.52 ± 1.8 | 1.97 ± 1.6 | 1.71 ± 1.4 |
| YBT Ant | 5.44 ± 3.5 | 4.65 ± 4.3 | 4.96 ± 4.8 | 4.67 ± 3.8 | 4.47 ± 3.7 | 5.30 ± 4.4 | 5.39 ± 4.9 | 5.57 ± 9.1 |
| YBT PL #@ | 10.30 ± 10.5 | 6.22 ± 5.5 | 6.65 ± 6.3 | 6.39 ± 5.6 | 7.20 ± 6.4 | 7.98 ± 6.5 | 7.53 ± 7.1 | 6.56 ± 5.3 |
| YBT PM | 6.52 ± 5.2 | 6.17 ± 4.7 | 7.63 ± 7.4 | 6.94 ± 6.5 | 8.65 ± 6.5 | 6.64 ± 5.4 | 8.50 ± 6.7 | 7.09 ± 5.9 |
| YBT Comp | 8.21 ± 14.3 | 6.84 ± 8.6 | 5.10 ± 5.0 | 6.19 ± 13.5 | 4.65 ± 3.5 | 5.28 ± 4.7 | 5.40 ± 6.7 | 5.08 ± 4.7 |
| CAIT #& | 1.37 ± 1.5 | 5.16 ± 5.7 | 0.89 ± 1.8 | 1.49 ± 3.9 | 1.08 ± 2.4 | 3.26 ± 5.8 | 1.09 ± 2.7 | 1.08 ± 2.7 |
| Variable | Estimate | Standard Error | Odds Ratio | Wald Statistic | p-Value |
|---|---|---|---|---|---|
| Hexagon Diff | −0.177 | 0.066 | 0.838 | 7.198 | 0.007 * |
| CAIT Diff | 0.093 | 0.033 | 1.097 | 8.159 | 0.004 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shenhar, M.; Dar, G.; Finestone, A.S.; Witchalls, J.; Waddington, G.; Shina, A.; Steinberg, N. Performance Asymmetry, the Risk for Ankle Sprain, and the Influence of an Intervention Program in New Male Infantry Recruits. J. Clin. Med. 2025, 14, 6887. https://doi.org/10.3390/jcm14196887
Shenhar M, Dar G, Finestone AS, Witchalls J, Waddington G, Shina A, Steinberg N. Performance Asymmetry, the Risk for Ankle Sprain, and the Influence of an Intervention Program in New Male Infantry Recruits. Journal of Clinical Medicine. 2025; 14(19):6887. https://doi.org/10.3390/jcm14196887
Chicago/Turabian StyleShenhar, Michal, Gali Dar, Aharon S. Finestone, Jeremy Witchalls, Gordon Waddington, Avi Shina, and Nili Steinberg. 2025. "Performance Asymmetry, the Risk for Ankle Sprain, and the Influence of an Intervention Program in New Male Infantry Recruits" Journal of Clinical Medicine 14, no. 19: 6887. https://doi.org/10.3390/jcm14196887
APA StyleShenhar, M., Dar, G., Finestone, A. S., Witchalls, J., Waddington, G., Shina, A., & Steinberg, N. (2025). Performance Asymmetry, the Risk for Ankle Sprain, and the Influence of an Intervention Program in New Male Infantry Recruits. Journal of Clinical Medicine, 14(19), 6887. https://doi.org/10.3390/jcm14196887







